Abstract
Migraine is a disabling and prevalent disorder. Migraine is most effectively treated with a stepped care approach, where patients initially receive a broad level of care (primary care) and proceed to receive increasingly specialized care throughout the course of treatment. Behavioral treatments for migraine modify behaviors of people with migraine with the intention to prevent migraine episodes and secondary consequence of migraine. Behavioral treatments can be incorporated into each level of the stepped care approach for migraine treatment. In this article, we provide a rationale for including behavioral treatment strategies in the treatment of migraine. We then describe and review the evidence for behavioral treatment strategies for migraine, including patient education, relaxation strategies, biofeedback, and cognitive behavioral treatment strategies. Finally, we describe how behavioral treatments can be integrated into a stepped care approach for migraine care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Migraine is a disabling and common neurological disorder with an estimated prevalence of approximately 18 % of adult women and 6 % of men in the USA [1, 2]. Migraine affects all areas of life, including social and occupational functioning, and The Global Burden of Disease Study from the World Health Organization rates migraine as the third most common and eighth most burdensome disease in the world [3]. Migraine can be most effectively treated with a “stepped care” approach [4], where patients initially receive the broadest level of care and, if needed, proceed to receive increasingly specialized care throughout the course of treatment. While less than half of those with migraine seek medical care, those who do most commonly present in primary care where they can be well managed through an integration of broad migraine management education and a combination of both prescription and over-the-counter medications. People may advance to more intensive “steps” of care if previous steps are not effective at adequately managing migraine (Fig. 1), including referral to specialty care (step 2), referral to a multidisciplinary care provider, potentially including a psychologist, psychiatrist, other allied health-care professional (step 3), and, when necessary and possible, referral to an interdisciplinary pain or headache clinic (step 4). “Interdisciplinary” and “multidisciplinary” are used interchangeably; however, there is an important distinction. Multidisciplinary models of care includes health-care professionals from a variety of disciplines working independently to improve patient outcomes. In interdisciplinary models of care, health-care professionals from different disciplines work together to manage the patient utilizing each provider’s expertise. In this model, health decisions are patient-centered, and effective communication between professionals is vital, Few interdisciplinary headache treatment programs currently exist, much of the shared management of migraine is of a multidisciplinary model (e.g., step 3).
Behavioral Treatments in Stepped Care
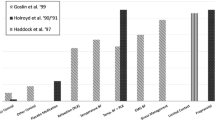
Behavioral treatments modify the behaviors of people with migraine with the intention preventing migraine episodes and secondary consequences of migraine, including diminished quality of life, headache-related disability impacting occupational, academic, and personal functioning, and psychological distress [5]. Certain evidence-based behavioral treatments, specifically relaxation training, thermal biofeedback combined with relaxation training, electromyographic biofeedback, and cognitive behavioral therapy, have grade A evidence for prevention of migraine according to the American Academy of Neurology’s evidence-based guidelines for migraine [6]. A breadth of literature on behavioral migraine treatments indicates treatment efficacy of 35–55 % for reductions in headache outcomes across trials of behavioral migraine treatment [7, 8].
Behavioral interventions can be utilized across multiple steps of care for people with migraine to enhance treatment outcomes, reduce headache-related disability, improve psychological comorbidities, and improve quality of life. At the most basic level, any intervention designed to modify the person with migraine’s behavior can be conceptualized as a behavioral intervention, ranging from patient education regarding optimal medication use in a physician’s office to intensive cognitive behavioral therapy to manage migraine provided by a psychologist or other mental health-care provider. Each health-care professional involved in the care of a person with migraine offers a specific set of skills and can provide interventions to modify the behaviors of people with migraine within this skill set (Table 1; adapted from [9]). This paper will specifically discuss behavioral interventions with the most robust evidence base, including patient education, relaxation-based therapies and biofeedback, and cognitive behavioral therapies.
Benefits of Behavioral Treatments
Incorporation of behavioral treatments into the stepped care of people with migraine has several advantages. In addition to improving treatment outcomes independently and in conjunction with medical interventions, behavioral treatments may also reduce medical expenditures, improve adherence to medical treatment strategies, and improve satisfaction for both patients and health-care professionals.
Migraine can incur a high monetary cost. Patients with migraine can have direct annual medical costs over twice as high as the general population and, most notably, prescription-drug-related costs up to four times higher [10, 11]. In one study, average prescription migraine medication costs alone were approximately $3000 per year; further, comorbid depression or anxiety among migraine patients was associated with additional elevations in medical costs [10]. Medical costs associated with migraine increase in relation to increased frequency of migraine attacks (most often measured in migraine days) [12]; therefore, individuals with frequent migraines may experience even higher medical costs. Compared to the average migraine prophylactic medications, behavioral treatments for migraine are cost effective after approximately 1 year [13]. Further, recent developments in minimal contact and home-based behavioral interventions provide even lower cost treatment options that demonstrate similar efficacy for clinical headache reductions as clinic-based behavioral treatments [13, 14].
Poor adherence with medical regimens is a challenge across medical care, but is especially problematic in chronic conditions such as migraine [15]. Treatment adherence is foundational to the optimal management of migraine. Qualitative data demonstrates that adherence with migraine treatment is a complex process which requires people with migraine to engage in behaviors every day to manage migraine, and in-the-moment to manage a specific migraine episode [16, 17]. Migraine medication adherence also has numerous barriers, ranging from forgetting to keep medication available to role conflicts (e.g., work or childcare interfering) with medication use. Reviews of empirical research suggest that people with migraine demonstrate poor adherence to all aspects of treatment, including taking preventive medication daily on a consistent basis and taking acute medication with optimal timing, type, and dosage [15, 18]. Additionally, nonadherence in the form of overconsumption of medication is implicated in medication overuse headache, which includes both medication dependence and resistance, and is associated with increased disability intractability to treatment [19, 20]. Adherence to migraine treatments can be augmented by behavioral interventions [21]. Patient education is posited to facilitate adherence by addressing the necessity of adherence and potential consequences of nonadherence [21]; further, improved self-efficacy and reduced psychiatric symptoms over the course of behavioral migraine treatments may also improve treatment adherence [22–24].
What Are Behavioral Migraine Treatments?
Patient Education
Patient education is essential to effective migraine management, as the patient makes the majority of therapeutic decisions independently and outside of the health-care professional’s office. The patient decides which attacks to treat, when to treat them, with what to treat them, to what extent to follow medical advice, whether to make healthy lifestyle changes, and many other decisions that are central to effective management. Patient education is a standard aspect of migraine treatment and ideally should be implemented in a consistent fashion by every provider in the context of migraine care.
Education alone can lead to significant improvements in pain outcomes, functional status, and quality of life, and decreased symptoms of depression, anxiety, and high health-care resource utilization [25–28]. Brief patient education has been shown to improve adherence and efficacy for pharmacological treatment alone (e.g., abortive medications) [29]. Patients who understand the mechanisms of their prescribed medications and how they fit with their treatment plan are twice as likely to fill the prescription [30]. Research on standardized patient education programs show benefits of patient education including improved self-efficacy [31, 32], improved utilization of acute medications [33, 34], improved quality of life [32], as well as reduced migraine disability and need for health-care utilization [27]. Generally, these benefits are accompanied by significant reductions in migraine attack or headache day frequency and associated disability [27, 32, 33].
Some of the most important areas to include in patient education for migraine and severe headache include provision of a basic understanding of headache pathology, education about the typical course of the chronic nature of headache, and reassurance of the benign nature of headaches, once other causes (secondary headache) have been ruled out. Also essential is to point out the pivotal importance of patient involvement in the management of migraine. This can include instruction about the proper application of acute and/or preventive medication, as indicated; instruction in how to use a headache diary; and education about lifestyle issues such as sleep, exercise, stress management, and nutrition that may influence migraine.
Provision of information is insufficient for effective patient education. Rains and colleagues [21] make the following suggestions for effective education and enhancing adherence:
-
Limit instructions to three to four major points during each discussion
-
Use simple, everyday language, especially when explaining diagnoses and treatment instructions (model or demonstrate, when possible)
-
Supplement oral instructions with written materials
-
Involve the patient’s family members or significant others
-
Ask patients to restate recommendations back to you (“I want to make sure I am being clear and that you understand what I am saying, so please tell me in your own words what we just covered”)
-
In conclusion, repeat and reinforce the concepts that were discussed.
During the course of patient education, the degree of patient understanding and agreement must be evaluated by requesting feedback and employing specific communication strategies. The “Ask–Tell–Ask” strategy has been used with great effect in the American Migraine Communication Study-2 [35]. This strategy acknowledges that effective education requires assessing what the patient already knows and believes, then building on (or correcting when necessary) this understanding. The “Ask–Tell–Ask” technique relies upon open-ended questions, active listening, and “being fully present” with the patient [36].
Further research on specific and structured patient education is pivotal to better understand what information is most pertinent to improving headache outcomes and how it is best delivered to the patient population.
Relaxation Training
Relaxation techniques focus on decreasing sympathetic arousal and retraining the stress response. Patients are typically taught various relaxation skills to induce the “relaxation response,” [37] which includes relaxation of the sympathetic nervous system and activation of the parasympathetic nervous system. Progressive muscle relaxation training (PMRT) was first introduced by Jacobson in 1938 [38]. This technique uses muscle discrimination training. Patients are instructed to systematically tense and relax discrete muscle groups while noticing the contrasting sensations. When the vigorous contractions are stopped, the muscles reflexively return to a lower state of tension through the process of homeostasis, further enhancing discrimination learning. Patients are instructed to practice this regularly and to use this strategy when they become aware of rising levels of tension or stress.
Other commonly taught relaxation techniques include guided imagery, cue-controlled relaxation, diaphragmatic breathing, hypnosis (therapist- or self-applied), meditation, or other methods that a patient finds helps to engage the “relaxation response” [37, 39, 40]. With appropriate education and training, relaxation techniques can be taught by a variety of health-care professionals. Relaxation techniques can also be self-taught by patients with print, audio, or online (e.g., apps, iTunes, YouTube) support materials. Relaxation training is a standard component of most behavioral migraine treatments provided by psychologists and other mental health-care providers. Regular practice in the patient’s day-to-day setting is required in order to gain full benefits and implement the strategies when needed [41].
It is particularly difficult to effectively isolate the efficacy of relaxation training as a behavioral intervention because relaxation training is a key component of the other behavioral migraine treatments discussed in this paper (biofeedback and CBT). In a meta-analysis of controlled behavioral trials for migraine, relaxation training demonstrated a medium effect size (d = .55) [42], which is comparable with the effect size found for more intensive CBT treatments (d = .54).
Biofeedback
Biofeedback involves monitoring physiological processes of which the patient may not be consciously aware and/or does not believe that he or she has the ability to voluntarily control. Goals include increasing awareness of and creating voluntary control over targeted physiological functions [43, 44]. Information is detected with sensors, and the information is converted into a signal, which is typically presented visually, but can also be audio or other forms of information.
Biofeedback is often a useful tool to physically demonstrate to people with migraine the physiological changes that occur during relaxation training. Many mental health-care providers, such as psychologists, are trained to provide biofeedback. During biofeedback training, patients are typically taught various relaxation skills, such as diaphragmatic breathing or visualization to induce the relaxation response. They are then instructed to practice engaging the relaxation response during biofeedback so that they can see the effect on their physiology and then modify behavior in the future to recreate this state.
Specific modalities are used for certain conditions, but often, multiple modalities are combined. Modalities with strongest efficacy for migraine management include thermal, electromyographic (EMG), or muscle tension and blood volume pulse (BVP). Additional modalities may include electroencephalography (EEG), galvanic skin response (GSR), and respiratory rate. Thermal biofeedback involves monitoring finger temperature with a sensitive thermometer. During or preceding a headache, the patient may experience activation of the sympathetic nervous system. As sympathetic activity increases, circulation to the extremities decreases and finger temperature decreases. Conversely, as parasympathetic activity increases and the relaxation response is activated, circulation and extremity temperature increase. Thus, finger temperature is viewed as providing an indirect measure of autonomic arousal.
Meta-analyses generally demonstrate overall medium effect sizes of biofeedback for migraine and average improvement rates for migraine ranging from 27 to 65 % [42, 45–48]. A recent analysis of aggregated biofeedback approaches on migraine yielded a medium-strong weighted mean effect size (d = .58). Specifically, electromyographic feedback, thermal feedback, thermal feedback plus relaxation or electromyographic feedback, and blood-volume pulse feedback (not fully discussed in this article) showed medium to large effect sizes (d = .50, .52, .60, .68, respectively) and did not significantly differ from one another [45]. Additionally, the review of several symptom categories revealed medium to large effect sizes of biofeedback on secondary outcome measures among patients with migraine including self-efficacy (d = .89), depression (d = .57), and anxiety (d = .44).
Cognitive Behavioral Therapies
Cognitive behavioral therapy (CBT) is comprised of strategies designed to modify the person with migraine’s thinking and behavior. Cognitive strategies focus on identifying and challenging maladaptive or dysfunctional beliefs, thoughts, and responses to stress [49–51]. Cognitive targets of CBT for migraine and other severe headache management include enhancing self-efficacy [52], reducing “catastrophizing” [53] (a pattern of thinking that including hopelessness, helplessness, and feeling overwhelmed and has been shown to predict poor outcome and reduced quality of life), and helping patients adopt an internal versus an external locus of control (i.e., a belief that the mechanism for change lies within oneself and not with the physician, medication, or medical procedures) [54, 55].
Behavioral strategies are designed to help patients identify and modify behaviors that may precipitate, increase, or maintain undesirable or unhealthy states. In the case of migraine or other severe headache, this may include modifying suspected triggers and promoting healthy lifestyle habits. This typically includes keeping a diary (paper or electronic) and using other behavioral techniques to identify and modify target behaviors. Having patients maintain detailed daily headache records can aid them in learning the relationship between their thoughts, behaviors, emotions, lifestyle choices, and headache characteristics. Relaxation training and/or biofeedback is often incorporated into CBT for migraine.
CBT has the added advantage of also being effective in treating depression, anxiety, panic disorder, and sleep disorders, among other conditions—all common comorbidities of migraine. Other targets of CBT for migraine or severe headache may include assertiveness training, increased coping and problem-solving skills, stress management, and other variables presumed to be related to headache onset, exacerbation, or maintenance.
CBT, by nature, combines multiple behavioral treatment components to manage migraine. Multiple meta-analyses have shown 30–55 % improvements in migraine outcomes for both relaxation training and CBT [56, 57, 43]. Clinically, CBT is often combined with pharmacological interventions. One recent study showed that the combination of preventive medication (beta-blockers) and a comprehensive CBT treatment protocol (which included relaxation, traditional CBT elements, and allowed the patient to choose either biofeedback or more intensive cognitive stress management treatment) produced large decreases in migraine days and migraine-related disability compared to either treatment alone or placebo [33]. Studies that attempt to discern additional benefit of increasing layers of complexity of relaxation, biofeedback, and CBT tend to demonstrate equal but not elevated efficacy of combined behavioral treatments, compared to single treatment approaches [42, 58, 59].
Emerging Therapies
Mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) have also been used recently for migraine and severe headache along with other chronic pain conditions [60]. MBCT is based on traditional cognitive approaches to treatment combined with mindful meditation practice [61].
Implementing Behavioral Treatments in Stepped Care of Migraine
Formal stepped care approaches, which use rule-based algorithms to refer patients onto higher steps of care based on clinical characteristics, have demonstrated efficacy in the treatment of a variety of chronic conditions, from chronic pain [62] to depression [63]. Although no formal stepped care regimen has been specifically evaluated in migraine as of this publication, stepped care approaches are common within existing randomized clinical trials for behavioral migraine treatments. For example, in an examination of behavioral treatment and preventive medication for migraine, Holroyd and colleagues [33] provided all patients with optimized acute therapy for 1 month. Optimized acute therapy included patient education and counseling around acute medication use, and optimization of the regimen of acute pharmacological therapies. Patients for whom optimized acute therapy alone was sufficient (who experienced two or fewer migraines with disability during the month of optimized acute therapy) were excluded from the remainder of the study. This approach allowed this study to retain only participants for whom optimized acute therapy alone was insufficient to manage their migraine. Similarly, stepped care approaches in clinical practice provide basic patient education and behavioral recommendations to all people with migraine and incorporate more time and resource intensive behavioral treatment strategies for patients for whom these strategies alone are insufficient.
In the first step of migraine care, at the level of primary care, people with migraine should be given patient education to optimize behaviors around migraine management (Fig. 1). An individual person’s migraine management plan will differ based on headache characteristics and patient preferences, but broad information about migraine pathophysiology, medication adherence, and common lifestyle modifications should be incorporated into the treatment of all people with migraine. At the second step of migraine care, at the level of specialty care, people with migraine should continue to receive patient education. Education topics might include specific information about the patient’s disorder, keeping a headache diary, and more individually tailored lifestyle recommendations. At the second step of migraine care, providers would recommend learning and practicing relaxation techniques. With appropriate education and training, many relaxation techniques can be incorporated into the practice of the majority of health-care providers. Further, some basic relaxation techniques can be self-taught by patients with appropriate support materials.
For a proportion of people with migraine, patient education alone is insufficient to modify behaviors necessary for migraine management. These patients might continue to have frequent severe migraine; alternately, patients may continue to have high levels of migraine-related disability even in the presence of a reduction in migraine frequency or severity. For any person with migraine for whom patient education to modify migraine management behaviors are insufficient, we recommend referral to a higher “step,” or more comprehensive, behavioral treatment for migraine (Fig. 1), typically provided by a psychologist or other mental health-care professional.
People with migraine and comorbid psychiatric conditions, particularly depression and anxiety, may find referral to comprehensive behavioral treatments for migraine particularly useful. People with migraine have elevated rates of psychiatric disorders, particularly mood and anxiety disorders [64–66]. Among people with migraine, comorbid depression and anxiety are associated with poorer quality of life and higher disability [67–69]. CBT is a standard treatment for people with depression and anxiety and may be used to treat both the migraine and psychiatric comorbidity concurrently. In one randomized controlled trial, people with depression and anxiety experienced even larger reductions in headache-related disability and migraine days with a comprehensive behavioral migraine management program, preventive medication, or both than people without depression and anxiety [70].
Ideal patients for referral to behavioral treatments are both amenable to behavioral modifications and have room for improvement in their current migraine management behaviors. Just as patients who present in physician’s offices with no intention of taking any medication prescribed are unlikely to experience large treatment effects of medical treatment, patients who present in a behavioral provider’s office with no intention of engaging in the treatment are unlikely to experience large treatment effects (or even participate in treatment). Additionally, some evidence suggests that people who believe that they can do nothing to control their migraine counterintuitively can experience large gains from behavioral migraine treatments; these people have the most to learn from behavioral migraine management and, therefore, at least have the potential to show the large treatment-related changes [23]. More research is needed to identify individual characteristics of individuals with migraine who most likely to benefit from comprehensive behavioral treatments and better understand the mechanisms through which behavioral treatments work.
Conclusion
Behavioral treatments for migraine, including biofeedback and relaxation, cognitive behavioral therapy, and patient education, have demonstrated efficacy in the treatment of migraine. Behavioral treatment strategies are cost effective, can be used in most or all stages of life where pharmacologic interventions may not be available or may be contraindicated (e.g., childhood, pregnancy), and can help improve adherence to pharmacological interventions. They can be used independently or combined with pharmacologic treatment regimens. Interventions to modify migraine management behaviors should be utilized at each step of care for people with migraine. Health-care professionals of all types are encouraged to integrate patient education strategies into the treatment of people with migraine. Certain communication strategies can enhance understanding and utilization of education, including limiting instructions to three to four major points and asking patients to restate recommendations. Patient education strategies are the key behavioral intervention utilized during “step 1” (primary care) and “step 2” (specialty care) treatment of people with migraine. For people who continue to have significant levels of migraine frequency and severity, or who continue to experience significant migraine-related disability, we recommend referral to “step 3 and 4” treatments, including relaxation training, biofeedback, and/or cognitive behavioral therapy, provided by behavioral specialists who may or may not work closely with neurologists or specialty headache professionals.
References
Lipton RB et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343–9.
Smitherman TA et al. The prevalence, impact, and treatment of migraine and severe headaches in the United States: a review of statistics from national surveillance studies. Headache. 2013;53(3):427–36. Provides a review of epidemiologic investigations of migraine and severe headaches in the United States, including information about prevalence, impact of migraine on patient’s lives, and treatment of migraine.
Murray C. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Los Angeles: Harvard University Press; 1996.
Bower P, Gilbody S. Stepped care in psychological therapies: access, effectiveness and efficiency. Narrative literature review. Br J Psychiatry. 2005;186:11–7.
Campbell J, Penzien D, Wall E. Evidence-based guidelines for migraine headache: behavioral and physical treatments: American Academy of Neurology Guidelines. 2000 Accessed February 21, 2012; Available from: www.aan.com/professionals/practice/pdfs/gl0089.pdf.
Silberstein S. Practice parameter: evidence-based guidelines for migraine headache (an evidence-based review). Neurology. 2000;55(6):754–62.
Penzien D, Rains J, Andrasik F. Behavioral management of recurrent headache: three decades of experience and empiricism. Appl Psychophysiol Biofeedback. 2002;27:163–81.
Schwartz MS, Andrasik F. Biofeedback: a practitioner’s guide. 3rd ed. New York: Guilford Press; 2003.
Buse DC. Multidisciplinary migraine management. Pain Med News. 2014;12.
Pesa J, Lage MJ. The medical costs of migraine and comorbid anxiety and depression. Head J Head Face Pain. 2004;44(6):562–70.
Hawkins K, Wang S, Rupnow M. Indirect cost burden of migraine in the United States. J Occup Environ Med. 2007;49(4):368–74.
Stokes M et al. Cost of health care among patients with chronic and episodic migraine in Canada and the USA: results from the International Burden of Migraine Study (IBMS). Headache. 2011;51(7):1058–77.
Schafer AM et al. Direct costs of preventive headache treatments: comparison of behavioral and pharmacologic approaches. Headache. 2011;51(6):985–91. Provides evidence for the cost-effectiveness of behavioral approaches for headache prevention.
Haddock CK et al. Home-based behavioral treatments for chronic benign headache: a meta-analysis of controlled trials. Cephalalgia. 1997;17(2):113–8.
Rains J, Lipchik G, Penzien D. Behavioral facilitation of medical treatment for headache. Part I: review of headache treatment compliance. Head J Head Face Pain. 2006;46(9):1387–94.
Peters M et al. Patients’ decision-making for migraine and chronic daily headache management. A qualitative study. Cephalalgia. 2003;23(8):833–41.
Seng EK, Holroyd KA. Optimal use of acute headache medication: a qualitative examination of behaviors and barriers to their performance. Headache. 2013;53(9):1438–50.
Ramsey RR et al. Treatment adherence in patients with headache: a systematic review. Headache. 2014;54(5):795–816. A thorough systematic review of all types of treatment adherence (acute medications, preventive medications, lifestyle recommendations and behavioral management strategies) for headache disorders.
Tepper SJ. Medication-overuse headache. CONTIN Life Learn Neurol. 2012;18(4, Headache):807–22. doi:10.1212/01.CON.0000418644.32032.7b.
Andrasik F et al. Disability in chronic migraine with medication overuse: treatment effects at 3 years. Headache. 2007;47(9):1277–81.
Rains JC, Penzien DB, Lipchik GL. Behavioral facilitation of medical treatment for headache—part II: theoretical models and behavioral strategies for improving adherence. Headache. 2006;46(9):1395–403.
Dunbar-Jacob J et al. Adherence in chronic disease. Annu Rev Nurs Res. 2000;18:48–90.
Seng EK, Holroyd KA. Dynamics of changes in self-efficacy and locus of control expectancies in the behavioral and drug treatment of severe migraine. Ann Behav Med. 2010;40(3):235–47.
Nestoriuc Y et al. Biofeedback treatment for headache disorders: a comprehensive efficacy review. Appl Psychophysiol Biofeedback. 2008;33(3):125–40.
Blumenfeld A, Tischio M. Center of excellence for headache care: group model at Kaiser Permanente. Headache. 2003;43(5):431–40.
Lemstra M, Stewart B, Olszynski WP. Effectiveness of multidisciplinary intervention in the treatment of migraine: a randomized clinical trial. Headache. 2002;42(9):845–54.
Rothrock JF et al. The impact of intensive patient education on clinical outcome in a clinic-based migraine population. Headache. 2006;46(5):726–31.
Harpole LH et al. Headache management program improves outcome for chronic headache. Headache. 2003;43(7):715–24.
Holroyd KA et al. Enhancing the effectiveness of abortive therapy: a controlled evaluation of self-management training. Headache. 1989;29(3):148–53.
Cameron C. Patient compliance: recognition of factors involved and suggestions for promoting compliance with therapeutic regimens. J Adv Nurs. 1996;24(2):244–50.
Cady R et al. Nurse-based education: an office-based comparative model for education of migraine patients. Headache. 2008;48(4):564–9.
Smith TR, Nicholson RA, Banks JW. Migraine education improves quality of life in a primary care setting. Headache. 2010;50(4):600–12.
Holroyd KA et al. Effect of preventive (beta blocker) treatment, behavioural migraine management, or their combination on outcomes of optimised acute treatment in frequent migraine: randomised controlled trial. BMJ. 2010;341:c4871.
Cady RK et al. Rizatriptan 10-mg ODT for early treatment of migraine and impact of migraine education on treatment response. Headache. 2009;49(5):687–96.
Hahn SR et al. Healthcare provider–patient communication and migraine assessment: results of the American Migraine Communication Study, phase II. Curr Med Res Opin. 2008;24(6):1711–8.
Boyle D, Dwinnell B, Platt F. Invite, listen, and summarize: a patient-centered communication technique. Acad Med. 2005;80(1):29–32.
Benson H, Greenwood MM, Klemchuk H. The relaxation response: psychophysiologic aspects and clinical applications. Int J Psychiatry Med. 1975;6(1–2):87–98.
Jacobson E. Progressive relaxation. Chicago: University of Chicago Press; 1938.
Hall H. Hypnosis. In: Waldman S, editor. Pain management. Philadelphia: Saunders/Elsevier; 2011. p. 963–6.
Rime C, Andrasik F. Relaxation techniques and guided imagery. In: Waldman S, editor. Pain management. Philadelphia: Saunders/Elsevier; 2011. p. 967–75.
Smith JC. Relaxation, meditation & mindfulness: a mental health practitioner’s guide to new and traditional approaches. NY: Springer; 2005.
Goslin R, Gray RR, McCrory D. Behavioral and physical treatments for migraine headache. Technical review 2.2: available from: http://www.clinpol.mc.duke.edu (1999). [cited 2003 May 15].
Buse DC, Andrasik F. Behavioral medicine for migraine. Neurol Clin. 2009;27(2):445–65.
Penzien DB, Holroyd KA. Psychosocial interventions in the management of recurrent headache disorders. 2: description of treatment techniques. Behav Med. 1994;20(2):64–73.
Nestoriuc Y, Martin A. Efficacy of biofeedback for migraine: a meta-analysis. Pain. 2007;128(1–2):111–27.
Blanchard EB et al. Migraine and tension headache: a meta-analytic review. Behav Ther. 1980;11(5):613–31.
Blanchard EB, Andrasik F. Biofeedback treatment of vascular headache. In: Hatch JGFJP, Rugh JD, editors. Biofeedback: studies in clinical efficacy. New York: Plenum Press; 1987.
Holroyd KA, Penzien DB, Holm JE, Hursey KG. Behavioral treatment of recurrent headache: what does the literature say? In: American Association for the Study of Headache. San Francisco; 1984a, June.
Beck AT et al. Cognitive therapy of depression. New York: Guilford Press; 1979. p. 425.
Holroyd KA, Andrasik F. A cognitive-behavioral approach to recurrent tension and migraine headache. In: Kendall PE, editor. Advances in cognitive-behavioral research and therapy. New York: Academic; 1982. p. 276–320.
McCarran MS, Andrasik F. Migraine and tension headaches. In: Michelson L, Ascher M, editors. Anxiety and stress disorders: cognitive-behavioral assessment and treatment. NY: Guilford; 1987. p. 465–483.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215.
Holroyd K et al. Impaired functioning and quality of life in severe migraine: the role of catastrophizing and associated symptoms. Cephalalgia. 2007;27:1156–65.
French DJ et al. Perceived self-efficacy and headache-related disability. Headache. 2000;40(8):647–56.
Heath RL et al. Locus of control moderates the relationship between headache pain and depression. J Headache Pain. 2008;9(5):301–8.
Andrasik F. What does the evidence show? Efficacy of behavioural treatments for recurrent headaches in adults. Neurol Sci. 2007;28 Suppl 2:S70–7.
Penzien DB, Rains JC, Andrasik F. Behavioral management of recurrent headache: three decades of experience and empiricism. Appl Psychophysiol Biofeedback. 2002;27(2):163–81.
Blanchard EB et al. A controlled evaluation of the addition of cognitive therapy to a home-based biofeedback and relaxation treatment of vascular headache. Headache. 1990;30(6):371–6.
Mullally WJ, Hall K, Goldstein R. Efficacy of biofeedback in the treatment of migraine and tension type headaches. Pain Physician. 2009;12(6):1005–11.
Day MA et al. Mindfulness-based cognitive therapy for the treatment of headache pain: a pilot study. Clin J Pain. 2014;30(2):152–61.
Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985;8(2):163–90.
Dorflinger L, et al. A partnered approach to opioid management, guideline concordant care and the stepped care model of pain management. J Gen Intern Med. 2014;29:870–6.
Firth N, Barkham M, Kellett S. The clinical effectiveness of stepped care systems for depression in working age adults: a systematic review. J Affect Disord. 2014;170C:119–30.
Buse DC et al. Psychiatric comorbidities of episodic and chronic migraine. J Neurol. 2013;260(8):1960–9. A review of the most recent evidence regarding common psychiatric comorbidities of both episodic and chronic migraine.
Wang SJ, Chen PK, Fuh JL. Comorbidities of migraine. Front Neurol. 2010;1:16.
Smitherman TA, Rains JC, Penzien DB. Psychiatric comorbidities and migraine chronification. Curr Pain Headache Rep. 2009;13(4):326–31.
Lanteri-Minet M et al. Anxiety and depression associated with migraine: influence on migraine subjects’ disability and quality of life, and acute migraine management. Pain. 2005;118(3):319–26.
Ashina S et al. Depression and risk of transformation of episodic to chronic migraine. J Headache Pain. 2012;13(8):615–24.
Wang SJ et al. Quality of life differs among headache diagnoses: analysis of SF-36 survey in 901 headache patients. Pain. 2001;89(2–3):285–92.
Seng EK, Holroyd KA. Psychiatric comorbidity and response to preventative therapy in the treatment of severe migraine trial. Cephalalgia. 2012;32(5):390–400. A study that demonstrates moderation of headache changes during preventive behavioral and pharmacotherapy by the presence of a depression and/or anxiety disorder.
Compliance with Ethics Guidelines
Conflict of Interest
Alexandra B. Singer declares that he has no conflict of interest.
Dawn C. Buse has received consultancy fees and paid travel accommodations from Allergan Pharmaceuticals, grants from Allergan, the National Headache Foundation, Novartis, and Teva/NuPathe, and payment for manuscript preparation from the National Headache Foundation.
Elizabeth K. Seng has received honoraria payments from the Headache Cooperative of New England and paid travel accommodations from the International Headache Academy.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding authors
Additional information
This article is part of the Topical Collection on Headache
Rights and permissions
About this article
Cite this article
Singer, A.B., Buse, D.C. & Seng, E.K. Behavioral Treatments for Migraine Management: Useful at Each Step of Migraine Care. Curr Neurol Neurosci Rep 15, 14 (2015). https://doi.org/10.1007/s11910-015-0533-5
Published:
DOI: https://doi.org/10.1007/s11910-015-0533-5