Abstract
Sedentary lifestyle after stroke is common which results in poor cardiovascular health. Aerobic exercise has the potential to reduce cardiovascular risk factors and improve functional capacity and quality of life in people after stroke. However, aerobic exercise is a therapeutic intervention that is underutilized by healthcare professionals after stroke. The purpose of this review paper is to provide information on exercise prescription using the FITT principle (frequency, intensity, time, type) for people after stroke and to guide healthcare professionals to incorporate aerobic exercise into the plan of care. This article discusses the current literature outlining the evidence base for incorporating aerobic exercise into stroke rehabilitation. Recently, high-intensity interval training has been used with people following stroke. Information is provided regarding the early but promising results for reaching higher target heart rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Exercise after stroke is an important component in the risk reduction of future cardiovascular events and recurrent stroke [1••]. Studies have demonstrated that people after stroke have poor cardiorespiratory fitness [2, 3] and can benefit from aerobic exercise training [1••]. With the continued growth of the elderly population [4] and the fact that American adults with chronic disease and disability are more likely to have cardiovascular risk factors present (physical inactivity, hypertension, obesity) [5], lifestyle interventions such as participation in exercise are extremely important. Further, when an exercise regimen is combined with pharmacologic treatment (i.e., antihypertensive medication), the risk of a second stroke is decreased by 80 % [6]. Meta-analysis suggests aerobic exercise is beneficial for improving cardiorespiratory fitness [7] and walking performance [8•]. However, despite these known benefits, most stroke rehabilitation programs lack aerobic exercise training.
Physical Inactivity After Stroke
Several studies have examined physical activity during stroke rehabilitation and report high levels of inactivity during the day [9, 10]. These observational studies have examined physical activity during inpatient stroke rehabilitation and have reported high levels of sedentary time [9, 10]. When observing activity during the daytime hours (8:00 a.m. to 5:00 p.m.), the individuals during inpatient stroke rehabilitation were seen in bed or sitting 76 % of the day and standing or walking only 23 % of the time [9]. Specifically, one study reported that more time spent in bed was associated with an unfavorable outcome on the modified Rankin Scale (mRS) at 3 months poststroke [10]. Although the majority of time is spent sedentary or in bed, we should consider whether stroke rehabilitation activities are sufficient to provide any aerobic benefit.
Previous work has suggested exercise intensity during traditional stroke rehabilitation is insufficient [11, 12]. In the longitudinal study by MacKay-Lyons and Makrides [11], they used recommendations for HR intensity from the American College of Sports Medicine [13] for an aerobic training effect. Heart rate range was defined as 60–90 % of maximum HR. They reported that less than 3 min of physical therapy was in the defined HR range, and occupational therapy was under 1 min. This finding is quite striking considering that the majority of these individuals would benefit from aerobic exercise.
A recent study by Prajapati and colleagues monitored self-selected walking activity and HR response during inpatient stroke rehabilitation [12]. The authors were interested in determining whether the time spent walking was at least 10 min in duration with a HR intensity of 40–80 % of HR reserve. The intensity chosen was more conservative than that of the study by MacKay-Lyons. Eight patients participating in inpatient stroke rehabilitation were monitored for 1 day. The authors report that only two individuals met the criteria for exercise intensity, while most had HR values below 20 % of HR reserve. No participants had bouts of walking that were at least 10 min in duration unless it occurred during a therapy session. The authors make important concluding statements that people after stroke should be encouraged to increase walking intensity and duration, and if self-selected walking is not possible, therapists should incorporate structured exercise into stroke rehabilitation.
Cardiac Rehabilitation Models for Stroke
Cardiac rehabilitation (CR) programs adapted for people after stroke appear to be feasible [14–16] and can improve cardiovascular health [17]. The CR programs offer comprehensive lifestyle management and are combined with supervised exercise sessions. However, most CR programs are not available to people after stroke [14]. This may be due to the need for a variety of equipment other than treadmills or the need for adaptive equipment for different exercise modalities for people poststroke [16, 18]. The available studies to date utilizing a CR model have been 6 months in duration. The work by Prior and colleagues reported improvements in body composition, reduced cholesterol and blood pressure, and improved behaviors for smoking cessation [15]. At enrollment in CR, the sample was considered high risk for a recurrent vascular event considering risk factors such as high cholesterol, sedentary, hypertension, and smoking. However, clinically meaningful improvements in the modification of vascular risk factors were reported. A study by Rimmer and colleagues reported improvements in cholesterol and blood pressure with a 14-week moderate-intensity exercise program [19]. This study was not conducted in a CR setting, but improvements in vascular risk factors were reported. These collective findings are extremely important considering the recurrence of stroke is high after the initial insult.
Aerobic Exercise During Inpatient Stroke Rehabilitation
Most aerobic exercise training studies during the subacute stage of recovery that have been conducted after inpatient rehabilitation has been completed [20–22]. Only a couple of studies have integrated aerobic exercise as part of inpatient stroke rehabilitation [23•, 24]. The authors highlight the importance that aerobic exercise may have on stroke recovery during the inpatient rehabilitation setting and the paucity of information guiding healthcare professionals for exercise prescription in subacute stroke [23•, 24]. Tang and colleagues discuss an important concept that “impairments in cardiorespiratory function and neuromotor control are independent, yet can mutually reinforce one another” [23•]. The take-home message from that statement is poor aerobic capacity after stroke may limit participation in therapies such as gait training or motor learning activities due to higher energy expenditure. Further, those individuals after stroke with neurologic impairments may not coordinate movement efficiently to participate in activities that challenge the cardiorespiratory system. These are important considerations when designing and implementing aerobic exercise programs poststroke.
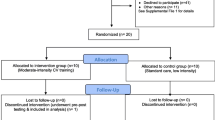
The study by Tang et al. was a randomized controlled trial where all participants received stroke rehabilitation by the treating therapists (physical, occupational, and speech). The aerobic exercise intervention was up to 30 min/day, intensity was 50–70 % of peak work rate (from the exercise test), 3 days per week using a recumbent cycle ergometer. The intervention lasted until discharge from inpatient rehabilitation. The control group only received standard therapy. While both groups improved over time in cardiorespiratory fitness and walking endurance (measured by distance during the 6-minute walk test (6MWT)), those individuals randomized to the exercise intervention had greater improvements in these specific outcome measures. It is important to note that the groups were matched for age and sex, and no between group differences were found for baseline stroke impairments measured by the National Institutes of Health Stroke Scale score, Functional Independence Measure, and the Chedoke-McMaster Stroke Assessment.
The work by Biasin and colleagues examined whether aerobic exercise could be implemented during inpatient stroke rehabilitation [24]. The primary physical therapist would refer appropriate people poststroke (based on inclusion/exclusion criteria) for study enrollment. All participants performed a submaximal exercise test prior to the commencement of the aerobic exercise intervention. The supervising physical therapist led the exercise group with assistance from trained support personnel. While the exercise program was feasible, challenges related to conflicting therapy sessions or medical treatment were noted. Further, the authors noted that not all participants reached their target exercise duration or intensity due to the conservative exercise prescription despite having information about exercise performance from the submaximal exercise test. This raises an interesting point about the possible lack of knowledge regarding exercise testing and prescription for people after stroke.
Identified Barriers for Aerobic Exercise Prescription
Despite the known benefits of aerobic exercise, many clinicians underutilize aerobic exercise during neurologic rehabilitation [25]. In a study published in 2013, 155 physical therapists in Canada responded to a survey regarding their knowledge about utilizing aerobic exercise in neurologic rehabilitation. Most of the respondents reported that aerobic exercise should be used in the treatment plan. However, only 2 % performed an exercise test that could be used to guide an appropriate exercise prescription plan, while the majority used the electronic health record for guidance.
Although recent exercise recommendations have been published [1••], there is still limited information from randomized controlled trials (RCTs) to guide healthcare professionals on aerobic exercise prescription in people following stroke specifically during stroke rehabilitation. In order to accurately prescribe exercise, we must have an understanding of the components of exercise prescription. Further, when this information and data is lacking in research trials, the interpretation of results may be insufficient for the replication of exercise prescription in clinical settings [26••].
The FITT Principle
The components of exercise prescription are frequency, intensity, time, and type (or modality), which are often referred to as the FITT principle [13]. The components of the FITT principle constitute the exercise dose or quantity needed to improve health similar to a pharmacologic intervention. According to a recent systematic review of 37 randomized controlled exercise trials conducted in people after stroke (subacute and chronic), studies appear to be devoid of reporting on all components of the FITT principle [26••]. The frequency and type of modality were reported in 94.6 % of the trials, while exercise intensity was defined in only 59 % of the RCTs. Time was described in 91.9 % of the trials. In order to successfully interpret the findings from stroke exercise trials and implement into clinical practice, more attention must be placed on including and reporting on all of the components of exercise prescription.
The purpose of this review paper is to define the components of exercise prescription and discuss current information related to the FITT principle to help guide researchers and healthcare professionals in utilizing these for exercise prescription in people following stroke.
Frequency
A recent systematic review found 16 aerobic exercise studies in stroke [27] with a frequency ranging from 2 to 5×/week for 4 weeks to 6 months, resulting in a number of total sessions ranging from 8 to 72. The most common frequency was 3×/week (13 of the 16 studies). The number of weeks varied: <8 weeks (3 studies), 8–12 weeks (7 studies), or 13–24 weeks (6 studies).
Inpatient rehab studies investigating aerobic exercise poststroke typically provide frequency from 3 to 5×/week. One study compared conventional inpatient rehabilitation (CR) plus leg cycle ergometer to CR alone [28]. Frequency was 5×/week for 3 weeks and subjects were followed for 6 weeks. As expected, both groups improved, but the cycling group improved significantly more (p < .01) relative to the control group for the Postural Assessment Scale for Stroke (specifically the ability to stand independently), Fugl–Meyer Assessment, and Functional Independence Measure Motor Subscale. A more recent inpatient rehabilitation study determined the feasibility of exercise testing and prescription and provided a group recumbent stepping program 3×/week [24], resulting in an average of 7.9 sessions over 19.5 days (every 2.5 days). The total number of visits among the 23 participants ranged from 1 to 16 sessions. All 20 patients who participated in qualitative exit interviews stated they benefited from the program including strength, endurance, and overall stroke recovery. Interestingly, 5 patients indicated they would have liked to participate in the program 5×/week. This is extremely encouraging from a clinical perspective that people after stroke would like to participate in more exercise training during rehabilitation.
A recent systematic review identified 13 aerobic exercise randomized control trials involving persons with chronic stroke [26••]. There were six studies that compared aerobic exercise with a non-aerobic exercise control. Although frequency varied, all showed significant between-group differences in VO2 peak. Summary results that were significant between groups are shown below by frequency.
Intensity
Intensity refers to the work rate, effort level, or metabolic demand of aerobic exercise and can be quantified in several ways, including HR, rate of oxygen consumption (VO2), rating of perceived exertion (RPE), watts, and/or walking speed/incline [35]. In stroke rehabilitation, aerobic intensity is commonly prescribed as a target HR, using either a raw percentage of HR max (target HR = target % × HR max) or the HR reserve method (target HR = target HR reserve% × [HR max − HR resting] + HR resting) [1••]. Heart rate max can be estimated as age-predicted maximal HR (AP max HR) using the formula 220 − age, the more accurate 206.9 − (0.67 × age) [35, 36], or a validated equation for persons taking β-blocking medication (e.g., 164 − [0.7 × age]) [37]. HR max can also be estimated by the peak HR achieved during a symptom-limited exercise test (peak HR). It is important to consider that peak HR after stroke occurs at approximately 74–86 % of AP max HR, on average [21, 38]. This means that prescription based on AP max HR may overestimate HR max, resulting in a higher intensity than expected [39]. On the other hand, if an individual exercise test is limited by cognitive or motor impairment, rather than a cardiopulmonary endpoint, exercise prescription based on peak HR may underestimate HR max, resulting in a lower intensity than expected [40]. Therefore, clinicians must consider patient performance and potential confounds that could affect exercise performance.
Low-Intensity Exercise
Low aerobic intensity is generally defined as <40 % HR reserve, <64 % HR max, or <12 RPE (6–20 scale) [35, 41]. People after stroke participating in low-intensity exercise programs do not require a baseline cardiopulmonary exercise test [1••]. Exercise prescription using low intensity (<40 % HR reserve) has not been extensively studied after stroke. However, the literature does suggest low-intensity exercise may improve motor performance, gait function, balance, and cardiovascular risk factors [28, 32, 34, 42].
Katz-Leurer and colleagues [28] found that adding a comfortable speed and lower extremity cycling program at <40 % HR reserve to inpatient stroke rehabilitation resulted in significantly greater improvement in balance (Postural Assessment Scale for Stroke) and motor impairment (lower extremity Fugl–Meyer Assessment) compared to usual care alone. Among persons with chronic stroke, two studies have used a comparison control group that performed low-intensity treadmill walking [32] or overground walking [34] at <40 % HR reserve. Although not as effective as the intervention arm, it is important to understand that engaging in low-intensity exercise can be beneficial for improving overground walking speed and gait economy [32], knee strength [34], and walking endurance [34].
Given the prevalence and negative health consequences of sedentary lifestyle in this population [3, 43] and the potential for at least modest improvements in function and cardiovascular risk factors with low-intensity exercise, stroke rehabilitation professionals should promote increased physical activity for persons with stroke. This could be done in the inpatient setting, at home, and/or as part of a community program.
Moderate-Intensity Exercise
People after stroke engaging in moderate- and high-intensity exercise should have a cardiopulmonary exercise test [1••]. Moderate intensity is generally defined as 40–59 % HR reserve, 64–76 % HR max, or 12–13 RPE (6–20 scale) [35, 41]. Among persons with chronic stroke, moderate-intensity aerobic exercise has been shown in randomized controlled studies to significantly improve VO2 peak [31, 32, 34, 44, 45], walking endurance [31, 32, 34], cardiovascular risk factors [19, 34, 42, 45, 46], brain activation [31], and cognition [29].
Randomized controlled studies conducted during inpatient rehabilitation have found that moderate intensity aerobic exercise significantly improved exercise capacity [47], walking speed and endurance [48], and resting HR [47]. However, one randomized trial demonstrated trends for better outcomes in the aerobic exercise group, but no significant between-group differences were found [23•]. The authors concluded that the duration for aerobic exercise was limited by the short length of stay but that the findings were encouraging for implementing aerobic exercise into inpatient stroke rehabilitation.
High-Intensity Exercise
Vigorous (hard) intensity is generally defined as 60–84 % HR reserve, 77–93 % HR max, or 14–16 RPE (6–20 scale) [35, 41]. Many studies report target intensities that start in the moderate range (e.g., 40–50 % peak HR reserve) and progress into the lower end of the vigorous range (e.g., 60–70 % peak HR reserve), but either do not report actual training intensity [34, 44, 45, 49, 50] or report that actual mean training intensity remained below the vigorous threshold (e.g., 58 % peak HR reserve) at the end of the intervention [23•, 32]. It may be challenging to sustain vigorous aerobic intensity for many people with stroke due to motor impairment and/or aerobic deconditioning.
Continuous exercise at vigorous intensity is especially difficult because it typically draws on anaerobic metabolism, which creates a progressively increasing disturbance to acid–base balance [41, 51]. Such anaerobic training is not sustainable for long durations and has been associated with negative affective responses among healthy adults, which may decrease exercise adherence [52]. However, one study has reported reaching vigorous intensity with continuous exercise after stroke. Globas et al. [30] progressed actual mean aerobic intensity from 49 to 77 % peak HR reserve over 3 months of treadmill exercise for persons with chronic stroke and found significantly greater improvement in VO2 peak, gait endurance, fastest gait speed, the Berg Balance Scale, mental quality of life, and self-reported mobility compared to that of a control group of usual care. A secondary analysis comparing this study to a similar protocol using moderate aerobic intensity found that the higher intensity was associated with greater improvement in aerobic capacity, and no variable other than aerobic intensity predicted aerobic fitness gains [53].
High-intensity interval training (HIT) is a method that may facilitate the attainment of higher aerobic intensities after stroke [54]. HIT involves concentrated bursts of intense exercise alternated with recovery periods, in varying combinations of burst/recovery duration and intensity. Among persons with chronic stroke, a treadmill HIT protocol using 30-s bursts at maximal safe speed and 30-s resting recovery periods was able to elicit a mean aerobic intensity of 76 % peak HR reserve in the first session [55]. Another protocol using 4-min bursts at 85–95 % peak HR and 3-min recovery periods at 70 % peak HR found that persons 3–9 months poststroke were able to achieve a median aerobic intensity of 90–93 % peak HR in the final two minutes of the last burst each session [56]. HIT appears to be promising for exercise training after stroke, but further research is needed.
While low-intensity exercise can be prescribed for most, if not all, persons with stroke, higher intensities should be prescribed whenever safe and well tolerated because they are generally more effective. Compared to lower intensity, higher intensity has been shown to elicit significantly greater improvement in aerobic fitness among healthy adults [35, 57, 58], persons with heart disease [35, 59–65], and persons with stroke [53]. Higher exercise intensity has also been shown to confer greater protection from future cardiovascular events among healthy adults and persons with heart disease [66–69] and to elicit greater improvements in motor function (e.g., walking speed and endurance) for persons with stroke [50, 53, 70–76].
Time
Time, or duration, is considered the amount of exercise in minutes per day [35]. In people after stroke, it is recommended that aerobic exercise “time” should last for 20–60 min per session or several 10-min bouts of exercise per day [1••]. In the literature, we found that most studies commence an aerobic exercise intervention between 10 and 20 min and progress to 40–60 min per session [21, 23•, 31, 32, 77–79]. The severity of stroke should also need to be considered when prescribing “time” for an exercise program. It may be more appropriate for individuals after stroke with poor endurance or those with moderate or severe deficits to begin at 10 min of continuous exercise or even have short bouts of rest until the “time” is tolerated.
Type
This component refers to the type of exercise such as aerobic exercise for endurance or resistance training for muscular strength [35]. Individuals after stroke benefit from both types of exercise, but the focus will be on aerobic exercise [1••]. Aerobic exercise can consist of overground walking, treadmill training (with or without body weight support), cycling, swimming, and recumbent stepping. In acute stroke rehabilitation, overground walking during therapy is a common form of aerobic exercise. In fact, in a study by Cumming et al., those who participated in walking activities within 24 h after stroke had better performance on walking at discharge [80]. Early mobilization activities such as walking within the first 24 h poststroke have been shown to be safe and feasible [81]. However, more research is needed to determine the best type of exercise in this early phase of stroke recovery.
Aerobic activity using a treadmill [77, 82], cycle ergometer [22, 23•, 47], and recumbent stepper [21, 83] all have been shown to improve cardiorespiratory fitness. These types of exercise could be used during inpatient rehabilitation. Task-specific training such as treadmill exercise is beneficial for improving cardiorespiratory fitness and walking outcomes [31, 84]. However, balance and safety concerns may be an issue when using a treadmill. Therefore, clinicians may consider a body weight support system to ensure patient safety. Recumbent steppers can also be used if balance is a concern, upright posture is difficult, or walking is not feasible. The recumbent stepper has a seat that swivels making transfers from wheelchair to device safe and easy [18, 21, 85]. A recent study in subacute stroke reported that after an 8-week exercise intervention using a recumbent stepper, cardiorespiratory fitness and walking distance on the 6-min walk test improved after the training period. During inpatient stroke rehabilitation, Tang and colleagues also reported similar findings using a recumbent cycle ergometer [23•].
Conclusion
Exercise training can be a valuable therapeutic intervention after stroke. However, the literature suggests exercise is underutilized by rehabilitation professionals. Physical activity and exercise recommendations suggest that exercise should be started early after stroke and carried out through the continuum of care [1••]. We know exercise is beneficial for overall cardiovascular health. However, we must be diligent about using the FITT principle to prescribe a comprehensive exercise program to our patients after stroke across the continuum of care.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Billinger SA, Arena R, Bernhardt J, et al. Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014. This scientific statement from the American Heart/American Stroke Association has been updated from the original 2004 statement. This version not only provides exercise guidelines for stroke survivors, caregivers, and health care providers but also discusses when exercise should begin for people after stroke. Physical activity and exercise are beneficial and should be incorporated into daily routine.
Mackay-Lyons MJ, Makrides L. Exercise capacity early after stroke. Arch Phys Med Rehabil. 2002;83(12):1697–702.
Billinger SA, Taylor JM, Quaney BM. Cardiopulmonary response to exercise testing in people with chronic stroke: a retrospective study. Stroke Res Treat. 2012;2012:987637.
Sandroff BM, Motl RW, Pilutti LA, et al. Accuracy of StepWatch and ActiGraph accelerometers for measuring steps taken among persons with multiple sclerosis. PLoS One. 2014;9(4):e93511.
Pharr JR, Bungum T. Health disparities experienced by people with disabilities in the United States: a Behavioral Risk Factor Surveillance System study. Glob J Health Sci. 2012;4(6):99–108.
Hackam DG, Spence JD. Combining multiple approaches for the secondary prevention of vascular events after stroke: a quantitative modeling study. Stroke. 2007;38(6):1881–5.
Pang MY, Eng JJ, Dawson AS, Gylfadottir S. The use of aerobic exercise training in improving aerobic capacity in individuals with stroke: a meta-analysis. Clin Rehabil. 2006;20(2):97–111.
Veerbeek JM, Kwakkel G, van Wegen EE, Ket JC, Heymans MW. Early prediction of outcome of activities of daily living after stroke: a systematic review. Stroke. 2011;42(5):1482–8. Articles that reviewed acute stroke activities of daily living predictive outcome measures were analyzed. At this time, the predictive value of these measures needs further research as current research is not thorough enough to draw decisive conclusions.
Bernhardt J, Chitravas N, Meslo IL, Thrift AG, Indredavik B. Not all stroke units are the same: a comparison of physical activity patterns in Melbourne, Australia, and Trondheim, Norway. Stroke. 2008;39(7):2059–65.
Askim T, Bernhardt J, Salvesen O, Indredavik B. Physical activity early after stroke and its association to functional outcome 3 months later. J Stroke Cerebrovasc Dis. 2014;23(5):e305–12.
MacKay-Lyons MJ, Makrides L. Cardiovascular stress during a contemporary stroke rehabilitation program: is the intensity adequate to induce a training effect? Arch Phys Med Rehabil. 2002;83(10):1378–83.
Prajapati SK, Mansfield A, Gage WH, Brooks D, McIlroy WE. Cardiovascular responses associated with daily walking in subacute stroke. Stroke Res Treat. 2013;2013:612458.
ACSM. Guidelines for exercise testing and prescription. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 2010.
Tang A, Marzolini S, Oh P, McIlroy WE, Brooks D. Feasibility and effects of adapted cardiac rehabilitation after stroke: a prospective trial. BMC Neurol. 2010;10:40.
Prior PL, Hachinski V, Unsworth K, et al. Comprehensive cardiac rehabilitation for secondary prevention after transient ischemic attack or mild stroke: I: feasibility and risk factors. Stroke. 2011;42(11):3207–13.
Marzolini S, Leung YM, Alter DA, Wu G, Grace SL. Outcomes associated with cardiac rehabilitation participation in patients with musculoskeletal comorbidities. Eur J Phys Rehabil Med. 2013;49(6):775–83.
Ryan AS, Ivey FM, Prior S, Li G, Hafer-Macko C. Skeletal muscle hypertrophy and muscle myostatin reduction after resistive training in stroke survivors. Stroke. 2011;42(2):416–20.
Billinger SA, Tseng BY, Kluding PM. Modified total-body recumbent stepper exercise test for assessing peak oxygen consumption in people with chronic stroke. Phys Ther. 2008;88(10):1188–95.
Rimmer JH, Rauworth AE, Wang EC, Nicola TL, Hill B. A preliminary study to examine the effects of aerobic and therapeutic (nonaerobic) exercise on cardiorespiratory fitness and coronary risk reduction in stroke survivors. Arch Phys Med Rehabil. 2009;90(3):407–12.
Duncan P, Studenski S, Richards L, et al. Randomized clinical trial of therapeutic exercise in subacute stroke. Stroke. 2003;34(9):2173–80.
Billinger SA, Mattlage AE, Ashenden AL, Lentz AA, Harter G, Rippee MA. Aerobic exercise in subacute stroke improves cardiovascular health and physical performance. J Neurol Phys Ther. 2012;36(4):159–65.
Yates JS, Studenski S, Gollub S, et al. Bicycle ergometry in subacute-stroke survivors: feasibility, safety, and exercise performance. J Aging Phys Act. 2004;12(1):64–74.
Tang A, Sibley KM, Thomas SG, et al. Effects of an aerobic exercise program on aerobic capacity, spatiotemporal gait parameters, and functional capacity in subacute stroke. Neurorehabil Neural Repair. 2009;23(4):398–406. This paper presents information regarding physical therapists’ comfort level with prescribing exercise to patients with neurologic conditions including stroke. Most therapists agree exercise is important but few utilize in clinical practice.
Biasin L, Sage MD, Brunton K, et al. Integrating aerobic training within subacute stroke rehabilitation: a feasibility study. Phys Ther. 2014.
Doyle L, Mackay-Lyons M. Utilization of aerobic exercise in adult neurological rehabilitation by physical therapists in Canada. J Neurol Phys Ther. 2013;37(1):20–6.
Ammann BC, Knols RH, Baschung P, de Bie RA, de Bruin ED. Application of principles of exercise training in sub-acute and chronic stroke survivors: a systematic review. BMC Neurol. 2014;14(1):167. This meta-analysis reviewed 28 articles that used randomized controlled trials. The authors concluded that cardiorespiratory fitness can be improved through aerobic exercise in stroke survivors.
Marsden DL, Dunn A, Callister R, Levi CR, Spratt NJ. Characteristics of exercise training interventions to improve cardiorespiratory fitness after stroke: a systematic review with meta-analysis. Neurorehabil Neural Repair. 2013;27(9):775–88.
Katz-Leurer M, Sender I, Keren O, Dvir Z. The influence of early cycling training on balance in stroke patients at the subacute stage. Results of a preliminary trial. Clin Rehabil. 2006;20(5):398–405.
Quaney BM, Boyd LA, McDowd JM, et al. Aerobic exercise improves cognition and motor function poststroke. Neurorehabil Neural Repair. 2009;23(9):879–85.
Globas C, Becker C, Cerny J, et al. Chronic stroke survivors benefit from high-intensity aerobic treadmill exercise: a randomized control trial. Neurorehabil Neural Repair. 2012;26(1):85–95.
Luft AR, Macko RF, Forrester LW, et al. Treadmill exercise activates subcortical neural networks and improves walking after stroke. A randomized controlled trial. Stroke. 2008.
Macko RF, Ivey FM, Forrester LW, et al. Treadmill exercise rehabilitation improves ambulatory function and cardiovascular fitness in patients with chronic stroke: a randomized, controlled trial. Stroke. 2005;36(10):2206–11.
Jin H, Jiang Y, Wei Q, Wang B, Ma G. Intensive aerobic cycling training with lower limb weights in Chinese patients with chronic stroke: discordance between improved cardiovascular fitness and walking ability. Disabil Rehabil. 2012;34(19):1665–71.
Jin H, Jiang Y, Wei Q, Chen L, Ma G. Effects of aerobic cycling training on cardiovascular fitness and heart rate recovery in patients with chronic stroke. NeuroRehabilitation. 2013;32(2):327–35.
American College of Sports M. ACSM’s guidelines for exercise testing and prescription. Vol 9th. Philadelphia: Lippincott Williams & Wilkins; 2014.
Gellish RL, Goslin BR, Olson RE, McDonald A, Russi GD, Moudgil VK. Longitudinal modeling of the relationship between age and maximal heart rate. Med Sci Sports Exerc. 2007;39(5):822–9.
Brawner CA, Ehrman JK, Schairer JR, Cao JJ, Keteyian SJ. Predicting maximum heart rate among patients with coronary heart disease receiving beta-adrenergic blockade therapy. Am Heart J. 2004;148(5):910–4.
MacKay-Lyons MJ, Howlett J. Exercise capacity and cardiovascular adaptations to aerobic training early after stroke. Top Stroke Rehabil. 2005;12(1):31–44.
Pang MY, Charlesworth SA, Lau RW, Chung RC. Using aerobic exercise to improve health outcomes and quality of life in stroke: evidence-based exercise prescription recommendations. Cerebrovasc Dis (Basel, Switzerland). 2013;35(1):7–22.
Tang A, Marzolini S, Oh P, McIlroy WE, Brooks D. Factors associated with change in aerobic capacity following an exercise program for individuals with stroke. J Rehabil Med. 2013;45(1):32–7.
Mezzani A, Hamm LF, Jones AM, et al. Aerobic exercise intensity assessment and prescription in cardiac rehabilitation: a joint position statement of the European Association for Cardiovascular Prevention and Rehabilitation, the American Association of Cardiovascular and Pulmonary Rehabilitation, and the Canadian Association of Cardiac Rehabilitation. J Cardiopulm Rehabil Prev. 2012;32(6):327–50.
Tang A, Eng JJ, Krassioukov AV, et al. Exercise-induced changes in cardiovascular function after stroke: a randomized controlled trial. Int J Stroke. 2014;9(7):883–9.
Manns PJ, Dunstan DW, Owen N, Healy GN. Addressing the nonexercise part of the activity continuum: a more realistic and achievable approach to activity programming for adults with mobility disability? Phys Ther. 2012;92(4):614–25.
Ivey FM, Hafer-Macko CE, Ryan AS, Macko RF. Impaired leg vasodilatory function after stroke: adaptations with treadmill exercise training. Stroke. 2010;41(12):2913–7.
Ivey FM, Ryan AS, Hafer-Macko CE, Goldberg AP, Macko RF. Treadmill aerobic training improves glucose tolerance and indices of insulin sensitivity in disabled stroke survivors: a preliminary report. Stroke. 2007;38(10):2752–8.
Lennon O, Carey A, Gaffney N, Stephenson J, Blake C. A pilot randomized controlled trial to evaluate the benefit of the cardiac rehabilitation paradigm for the non-acute ischaemic stroke population. Clin Rehabil. 2008;22(2):125–33.
Katz-Leurer M, Shochina M, Carmeli E, Friedlander Y. The influence of early aerobic training on the functional capacity in patients with cerebrovascular accident at the subacute stage. Arch Phys Med Rehabil. 2003;84(11):1609–14.
Kuys SS, Brauer SG, Ada L. Higher-intensity treadmill walking during rehabilitation after stroke in feasible and not detrimental to walking pattern or quality: a pilot randomized trial. Clin Rehabil. 2011;25(4):316–26.
Ivey FM, Ryan AS, Hafer-Macko CE, Macko RF. Improved cerebral vasomotor reactivity after exercise training in hemiparetic stroke survivors. Stroke. 2011. In press.
Outermans JC, van Peppen RP, Wittink H, Takken T, Kwakkel G. Effects of a high-intensity task-oriented training on gait performance early after stroke: a pilot study. Clin Rehabil. 2010;24(11):979–87.
Guazzi M, Adams V, Conraads V, et al. EACPR/AHA Scientific Statement. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2012;126(18):2261–74.
Ekkekakis P, Parfitt G, Petruzzello SJ. The pleasure and displeasure people feel when they exercise at different intensities: decennial update and progress towards a tripartite rationale for exercise intensity prescription. Sports Med (Auckland, NZ). 2011;41(8):641–71.
Lam JM, Globas C, Cerny J, et al. Predictors of response to treadmill exercise in stroke survivors. Neurorehabil Neural Repair. 2010;24(6):567–74.
Boyne P, Dunning K, Carl D, Gerson M, Khoury J, Kissela B. High-intensity interval training in stroke rehabilitation. Top Stroke Rehabil. 2013;20(4):317–30.
Boyne P, Dunning K, Carl D, Gerson M, Khoury J, Kissela B. Within-session responses to high-intensity interval training in chronic stroke. Med Sci Sports Exerc. 2014. In press.
Askim T, Dahl AE, Aamot IL, Hokstad A, Helbostad J, Indredavik B. High-intensity aerobic interval training for patients 3–9 months after stroke. A feasibility study. Physiother Res Int: J Res Clin Phys Ther. 2013.
Daussin FN, Ponsot E, Dufour SP, et al. Improvement of VO2max by cardiac output and oxygen extraction adaptation during intermittent versus continuous endurance training. Eur J Appl Physiol. 2007;101(3):377–83.
Helgerud J, Hoydal K, Wang E, et al. Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc. 2007;39(4):665–71.
Freyssin C, Verkindt C, Prieur F, Benaich P, Maunier S, Blanc P. Cardiac rehabilitation in chronic heart failure: effect of an 8-week, high-intensity interval training versus continuous training. Arch Phys Med Rehabil. 2012.
Fu TC, Wang CH, Lin PS, et al. Aerobic interval training improves oxygen uptake efficiency by enhancing cerebral and muscular hemodynamics in patients with heart failure. Int J Cardiol. 2011.
Moholdt T, Aamot IL, Granoien I, et al. Aerobic interval training increases peak oxygen uptake more than usual care exercise training in myocardial infarction patients: a randomized controlled study. Clin Rehabil. 2012;26(1):33–44.
Moholdt T, Aamot IL, Granoien I, et al. Long-term follow-up after cardiac rehabilitation: a randomized study of usual care exercise training versus aerobic interval training after myocardial infarction. Int J Cardiol. 2011;152(3):388–90.
Moholdt TT, Amundsen BH, Rustad LA, et al. Aerobic interval training versus continuous moderate exercise after coronary artery bypass surgery: a randomized study of cardiovascular effects and quality of life. Am Heart J. 2009;158(6):1031–7.
Rognmo O, Hetland E, Helgerud J, Hoff J, Slordahl SA. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiovasc Prev Rehabil Off J Eur Soc Cardiol Work Groups Epidemiol Prev Card Rehabil Exerc Physiol. 2004;11(3):216–22.
Wisloff U, Stoylen A, Loennechen JP, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007;115(24):3086–94.
Ciolac EG. High-intensity interval training and hypertension: maximizing the benefits of exercise? Am J Cardiovasc Dis. 2012;2(2):102–10.
Guiraud T, Nigam A, Gremeaux V, Meyer P, Juneau M, Bosquet L. High-intensity interval training in cardiac rehabilitation. Sports Med (Auckland, NZ). 2012;42(7):587–605.
Rankin AJ, Rankin AC, Macintyre P, Hillis WS. Walk or run? Is high-intensity exercise more effective than moderate-intensity exercise at reducing cardiovascular risk? Scott Med J. 2012;57(2):99–102.
Wisloff U, Nilsen TI, Droyvold WB, Morkved S, Slordahl SA, Vatten LJ. A single weekly bout of exercise may reduce cardiovascular mortality: how little pain for cardiac gain? ‘The HUNT study, Norway’. Eur J Cardiovasc Prev Rehabil Off J Eur Soc Cardiol Work Groups Epidemiol Prev Card Rehabil Exerc Physiol. 2006;13(5):798–804.
Hornby TG, Straube DS, Kinnaird CR, et al. Importance of specificity, amount, and intensity of locomotor training to improve ambulatory function in patients poststroke. Top Stroke Rehabil. 2011;18(4):293–307.
Kwakkel G, Wagenaar RC, Twisk JW, Lankhorst GJ, Koetsier JC. Intensity of leg and arm training after primary middle-cerebral-artery stroke: a randomised trial. Lancet. 1999;354(9174):191–6.
Lau KW, Mak MK. Speed-dependent treadmill training is effective to improve gait and balance performance in patients with sub-acute stroke. J Rehabil Med. 2011;43(8):709–13.
Moore JL, Roth EJ, Killian C, Hornby TG. Locomotor training improves daily stepping activity and gait efficiency in individuals poststroke who have reached a “plateau” in recovery. Stroke. 2010;41(1):129–35.
Pohl M, Mehrholz J, Ritschel C, Ruckriem S. Speed-dependent treadmill training in ambulatory hemiparetic stroke patients: a randomized controlled trial. Stroke. 2002;33(2):553–8.
Rose D, Paris T, Crews E, et al. Feasibility and effectiveness of circuit training in acute stroke rehabilitation. Neurorehabil Neural Repair. 2011;25(2):140–8.
Sullivan KJ, Knowlton BJ, Dobkin BH. Step training with body weight support: effect of treadmill speed and practice paradigms on poststroke locomotor recovery. Arch Phys Med Rehabil. 2002;83(5):683–91.
Macko RF, Smith GV, Dobrovolny CL, Sorkin JD, Goldberg AP, Silver KH. Treadmill training improves fitness reserve in chronic stroke patients. Arch Phys Med Rehabil. 2001;82(7):879–84.
Patterson SL, Rodgers MM, Macko RF, Forrester LW. Effect of treadmill exercise training on spatial and temporal gait parameters in subjects with chronic stroke: a preliminary report. J Rehabil Res Dev. 2008;45(2):221–8.
Peurala SH, Airaksinen O, Huuskonen P, et al. Effects of intensive therapy using gait trainer or floor walking exercises early after stroke. J Rehabil Med. 2009;41(3):166–73.
Cumming TB, Thrift AG, Collier JM, et al. Very early mobilization after stroke fast-tracks return to walking: further results from the phase II AVERT randomized controlled trial. Stroke. 2011;42(1):153–8.
Bernhardt J, Dewey H, Thrift A, Collier J, Donnan G. A very early rehabilitation trial for stroke (AVERT): phase II safety and feasibility. Stroke. 2008;39(2):390–6.
Mackay-Lyons M, McDonald A, Matheson J, Eskes G, Klus MA. Dual effects of body-weight supported treadmill training on cardiovascular fitness and walking ability early after stroke: a randomized controlled trial. Neurorehabil Neural Repair. 2013.
Kluding PM, Tseng BY, Billinger SA. Exercise and executive function in individuals with chronic stroke: a pilot study. J Neurol Phys Ther. 2011;35(1):11–7.
Macko RF, Ivey FM, Forrester LW. Task-oriented aerobic exercise in chronic hemiparetic stroke: training protocols and treatment effects. Top Stroke Rehabil. 2005;12(1):45–57.
Palmer-McLean K, Harbst K. ACSM’s exercise management for persons with chronic diseases and disabilities, vol. 3. Champaign: Human Kinetics; 2009.
Compliance with Ethics Guidelines
Conflict of Interest
Pierce Boyne, Eileen Coughenour, and Kari Dunning declare that they have no conflict of interest.
Sandra A Billinger has received a grant from the National Institutes of Health (K01HD067318).
Anna Mattlage has received a grant from the American Heart Association (14PRE20040026).
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Stroke
Rights and permissions
About this article
Cite this article
Billinger, S.A., Boyne, P., Coughenour, E. et al. Does Aerobic Exercise and the FITT Principle Fit into Stroke Recovery?. Curr Neurol Neurosci Rep 15, 519 (2015). https://doi.org/10.1007/s11910-014-0519-8
Published:
DOI: https://doi.org/10.1007/s11910-014-0519-8