Abstract
Cognitive impairment and dementia are significant sequelae of Parkinson disease (PD) and comprise a key feature of dementia with Lewy bodies (DLB), a disease with similar clinical and neuropathological features. Multiple independent causes have been implicated in PD dementia (PDD) and DLB, among them the accumulation of β-amyloid, a neuropathological hallmark of Alzheimer disease. Over the last decade, PET imaging has emerged as a viable method to measure amyloid burden in the human brain and relate it to neurodegenerative diseases. This article reviews what amyloid imaging has taught us about PDD and DLB. Current data suggest that brain amyloid deposition tends to be more marked in DLB, yet contributes to cognitive impairment in both DLB and PD. These results are broadly consistent with neuropathology and CSF studies. β-Amyloid may interact synergistically with other pathological processes in PD and DLB to contribute to cognitive impairment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction: A Brief History of Amyloid Imaging
Until recently, the assessment of the molecular basis of neurological disorders was largely limited to postmortem tissue. This changed with the development of amyloid radioligands such as [11C]Pittsburgh compound B (PiB) (Table 1) [1]. PiB binds fibrillar amyloid with nanomolar affinity in postmortem specimens [2–4]. As a result, it avidly stains neuritic plaques, a hallmark of Alzheimer disease (AD). In addition, it also stains many diffuse plaques, depending on their content of fibrillar amyloid [4–6]. In contrast, PiB does not appear to significantly label soluble oligomers or monomers of β-amyloid (Aβ). At brain concentrations achieved in human imaging, PiB has negligible off-target binding for Lewy bodies [7], neurofibrillary tangles (NFTs) [8], or other protein aggregates in postmortem brain tissue. However, PiB also labels vascular Aβ, the defining feature of cerebral amyloid angiopathy [4, 9, 10]. As required for a successful biomarker of Aβ, amyloid imaging in AD reliably reports significant amyloid deposition, and reliably reports its absence in young healthy control subjects (HCS) [11, 12] and in patients with other neurodegenerative diseases, including autopsy-proven Creutzfeld–Jacob disease [13] and frontotemporal dementia (FTD) on the basis of semantic dementia, albeit without autopsy confirmation [14].
Because the short half life of 11C limits the use of PiB, a number of 18F-labeled amyloid ligands have been developed as well, including [18F]florbetaben [15], [18F]florbetapir [16, 17], and [18F]flutametamol [18, 19]. White matter uptake complicates the use of the fluorinated molecules, but this disadvantage has been offset by their significantly longer half-lives compared with [11C]PiB, which permits their use at sites that lack radiochemistry facilities. Like PiB, these amyloid ligands demonstrate specific affinity for amyloid plaques in postmortem tissue and show increased retention in AD patients compared with HCS [17, 19–22] and neurodegenerative diseases not associated with Aβ accumulation, such as FTD [23•]. Head-to-head comparisons of PiB with these fluorinated ligands have demonstrated high correlations of cortical uptake of these tracers [24•]. Other amyloid ligands have also been developed, including 2-(1-{6-[(2-[18F]fluoroethyl)(methyl)amino]-2-naphthyl}ethylidene)malononitrile ([18F]FDDNP), which labels amyloid plaques, NFTs, and Lewy bodies [25, 26].
Amyloid imaging of older HCS has demonstrated a broad distribution of amyloid burden, with some HCS harboring amyloid loads well into the AD range [11, 12, 27–31]. In fact, cortical deposits of amyloid can be detected in approximately 25 % of HCS [12, 27, 28, 30, 31]. Consistent with neuropathology studies, amyloid burden measured with PiB PET increases with age [12, 29] and with the presence of the apolipoprotein ε4 haplotype [12, 29, 30, 32]. These findings have called into question the interpretation of a “positive” amyloid scan. However, even in HCS, the presence of significant amyloid burden is associated with small but significant impairments of global cognition and episodic memory [33]. Furthermore, recent longitudinal studies have consistently detected a contribution of baseline amyloid burden to the subsequent development of cognitive impairment and dementia [31, 34–37]. Thus, although amyloid burden in HCS may have only subtle repercussions for current cognitive function, it may nonetheless portend future cognitive decline.
Over the last 7 years, amyloid imaging has been applied fruitfully not just to AD but also to Parkinson disease (PD) dementia (PDD) and dementia with Lewy bodies (DLB). In this review, we will explore these efforts to relate imaged amyloid burden to clinical phenotype and to clinical course in PD and DLB.
PD Dementia and DLB
Cognitive impairment is common in PD, increasing in severity with advancing age and with progression of motor impairment [38–40]. As a result, dementia is overrepresented in PD relative to the general population, by up to a factor of 6 [41], with a prevalence of 30–80 %, depending on the motor stage and the duration of the disease [42]. A diagnosis of PDD is made when dementia develops in the setting of well-established idiopathic PD, which by consensus is taken to be at least 1 year of extrapyramidal motor symptoms [43]. PDD is clinically similar to DLB, a dementia associated with concomitant parkinsonism, visual hallucinations, and fluctuations of wakefulness and cognition [44]. In fact, these diseases share additional clinical features, including an association with REM sleep behavioral disorder, sensitivity to dopamine receptor antagonists, and response to acetylcholinesterase inhibitors. DLB and PDD share neuropathological features as well, including characteristic Lewy bodies and neurites (with involvement of cortical neurons frequent in PDD and requisite in DLB) [45]), and the loss of both nigral dopamine neurons [46] and basal forebrain cholinergic populations [47]. For these reasons, DLB and PDD are considered to be different clinical expressions of the same fundamental neuropathological processes. Their clinical differences, which consist primarily of the relative timing of dementia and parkinsonism, have been the focus of intense investigation [45].
Neuropathology Studies in PD and DLB
The biological basis for cognitive impairment in PD and DLB appears to be multifactorial. Aggregation of α-synuclein [48, 49] into oligomers, Lewy neurites and Lewy bodies and the involvement of cortical neurons contribute [50, 51], perhaps through secondary synapse dysfunction [52, 53]. Loss of monoamine neurotransmitter systems, including tegmental dopamine neurons and basal forebrain cholinergic neurons, which project to cognitive and limbic brain regions, also appears to play a role [54]. Finally, concomitant pathology characteristic of AD has been associated with both PDD and DLB [55–57].
Although Lewy-body-associated neuropathologic changes comprise the dominant findings in PD, PDD, and DLB, these need not occur in isolation. Indeed, neuropathology studies in PD report a range of concomitant neuropathological findings characteristic of AD, including Aβ-containing plaques and tau-containing NFTs. Approximately 35 % of PD cases are estimated to fulfill Consortium to Establish a Registry for Alzheimer's Disease criteria for a pathological diagnosis of AD [58, 59]. Diffuse plaques are more common than cored plaques in PD [60]. When dementia is present in PD, higher densities of cortical and striatal (cored and diffuse) plaques have been observed, compared with nondemented PD [60], although diffuse plaques remain more prevalent [61]. Several clinicopathologic studies of PDD have also found an association between higher levels of Aβ and a faster transition to dementia [60, 62, 63].
Concomitant Aβ pathologic findings are more common in DLB than in PDD [55, 64, 65]. In fact, deposition of extracellular Aβ into neuritic and diffuse plaques is present in approximately 85 % of cases of DLB [50, 66, 67]. The presence of amyloid plaques in the striatum has been reported to differentiate DLB and PDD from PD [68]. Interestingly, in that study, striatal cored plaques were much more common in DLB than in PDD. In PDD and DLB, higher levels of Aβ have also been associated with greater risk of mortality [69, 70]. The capacity for amyloid burden to accelerate cognitive decline in PDD holds when DLB and PDD are studied together [64, 65].
In addition to Aβ, the intracellular accumulation of NFTs has been linked to both PDD [49] and DLB [57]. NFTs are frequently present but rarely marked. Thus, AD pathologic changes are commonly observed in PD and DLB, most often at levels insufficient for a pathological diagnosis of AD, but their presence appears to have clinical implications.
Amyloid Imaging in PDD and DLB
Several cross-sectional imaging studies have explored amyloid deposition in PD, PDD, and DLB. One general finding is that amyloid burden tends to be modest in PD, overlapping with that in HCS [27, 71–75, 76•, 77]. Although cortical Aβ levels are often low in PD, they are not necessarily negligible. Indeed, specific cortical retention of PiB can be observed in some cases on direct visual assessment of the parametric images [27]. In addition, consistent with the broad distribution of amyloid burden in HCS described earlier, occasional PD cases demonstrate increased amyloid deposition as well, into the AD range [74, 75, 76•, 77]. Results obtained with florbetapir [23•, 78•] have been similar. Despite its capacity to label Lewy bodies, [18]FDDNP binding has also been reported to overlap in PD and HCS [79]. Together, these data demonstrate that the range of amyloid deposition in cognitively normal PD is similar to that seen in the healthy elderly population.
Amyloid burden is generally low in PD subjects with mild cognitive impairment (MCI), comparable to that in HCS [74, 76•, 80, 81•], and PiB uptake does not distinguish cognitively normal PD subjects from PD subjects with MCI. Low levels of cortical amyloid deposition have also been reported in most cases of PDD, overlapping with levels seen in HCS and frequently with levels observed in PD subjects as well [27, 71, 73–75, 76•, 77, 82]. Visual assessment of PDD patients has been notable for the frequent presence of focal cortical deposits of amyloid [27]. Because aggregate scores of global cortical ligand binding are insensitive to small foci of specific cortical retention, quantitative assessment of small foci may prove useful in relating amyloid burden to clinical phenotype and prognosis.
A minority of PDD subjects demonstrate elevated cortical amyloid deposition, in the AD range [71, 73–75, 76•, 77, 82]. The clinical characteristics of PDD patients with high and low amyloid burden appear to overlap [71, 76•, 77, 83•], although small sample sizes have limited these evaluations.
In contrast to the modest levels of amyloid observed in most PiB studies of PDD, amyloid deposition in DLB subjects is often high relative to that in HCS and PD subjects, in the AD range [23•, 27, 71, 73, 74, 76•, 78•, 84, 85, 86•, 87•, 88, 89]. Some DLB patients are clearly amyloid-negative, however. These negative scans presumably denote those with “pure” diffuse Lewy body changes without accompanying AD neuropathological changes, although one PiB-negative DLB patient proved to have substantial regional levels of Aβ despite low plaque burden at autopsy [90•]. These results are broadly consistent with the neuropathology studies described previously [55, 64, 65, 68]. Interestingly, higher cortical amyloid burden in a small cohort of DLB and PDD subjects has been associated with greater cortical and medial temporal lobe atrophy [83•], suggestive of superimposed classic AD. As observed in HCS, risk factors for higher amyloid burden in DLB and PDD subjects include age and the presence of the apolipoprotein ε4 allele [73, 76•, 84].
The clinical significance of Aβ deposits in Lewy body disorders remains a topic of active investigation. In some cross-sectional studies, global amyloid deposition has been found to relate to cognitive performance within diagnostic groups [23•, 74, 76•, 80]. In addition, in a small study, the absence of cortical amyloid deposition was associated with a better response to acetylcholine esterase inhibitors [88]. The higher amyloid burden of DLB relative to PDD has been offered as one potential explanation for the major clinical distinction between these related entities: the timing of dementia relative to parkinsonism [27, 64, 71, 84]. In this model, early and significant cortical amyloid burden may accelerate cognitive decline in patients with Lewy body disease. When this effect drives cognitive symptoms within 1 year of motor symptoms, this would result in a diagnosis of DLB.
One longitudinal study of nondemented PD subjects has been published to date. In that study, in which PD subjects were followed up for up to 5 years, those with higher amyloid burden progressed to cognitive impairment and dementia faster than those with lower amyloid burden [81•]. The hazard ratio for conversion was approximately 9 per unit PiB (distribution volume ratio). Not all individuals with positive PiB scans developed cognitive impairment, however, and some of the original cohort remained cognitively intact after 5 years of follow-up. These findings are similar to the results of longitudinal PiB studies of HCS (see earlier) [31, 34–37].
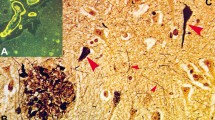
Amyloid imaging thus identifies a contribution of brain amyloid deposition to both DLB and PDD that is detectable in life (Fig. 1). Higher amyloid burden in DLB may contribute to its accelerated cognitive phenotype relative to parkinsonism, possibly as a result of synergistic Aβ–α-synuclein neurotoxicity. Cortical amyloid burden in PD, although lower than in DLB, does not appear to be harmless, however, as it has been associated with longitudinal cognitive decline.
Representative [11C]Pittsburgh compound B (PiB) scans of a healthy older subject and patients with Alzheimer disease, Parkinson disease (PD), PD with dementia, and dementia with Lewy bodies. Amyloid deposition in PD is usually mild and comparable to that seen in normal control subjects. In PDD, amyloid deposition is common, but is not usually marked. Amyloid deposition in DLB is often significant, to levels that approach those observed in AD. Note that focal cortical deposits of amyloid may not be reflected in aggregate measures of PiB binding derived over large cortical regions
Amyloid Deposition and Motor Features of Parkinsonism
PD can present with distinct motor phenotypes, including a classic asymmetric tremor extrapyramidal syndrome, a postural instability gait disorder (PIGD) syndrome, and an akinetic rigid syndrome. Although all of these presentations are associated with the presence of Lewy bodies at autopsy, presentations that deviate from the classic asymmetric tremor syndrome carry a higher risk of cognitive decline [91, 92]. A small number of neuropathology and biomarker studies have explored the relation between regional amyloid burden and motor features of parkinsonism. Higher amyloid plaque density postmortem has been associated with the PIGD phenotype [63]. One PiB imaging study on this issue has reported a positive correlation between striatal amyloid burden and PIGD motor features in PD subjects with MCI [93•]. A similar result was found using CSF [94]. This possible relation between amyloid burden and PD motor phenotype is intriguing, as it would extend the influence of Aβ to the motor domain. However, these results should be viewed as preliminary and would benefit from confirmation in larger studies.
Relation of Amyloid Imaging to CSF Biomarkers
CSF biomarkers of amyloid burden provide an independent assessment of levels of Aβ. In AD, CSF levels of Aβ-42 fall early and levels of the intracellular protein tau and its phosphorylated form phospho-tau increase [95]. The reduction in CSF levels of Aβ-42 has been attributed to its aggregation into amyloid plaques, whereas the increase in the levels of tau species has been interpreted to reflect of neuronal injury. In AD, CSF levels of Aβ-42 and amyloid imaging findings are strongly correlated [96•].
To date, amyloid imaging and CSF assessment of Aβ in PD, PDD, and DLB have generated similar results. CSF levels of Aβ and tau do not reliably differentiate PD subjects from HCS cross-sectionally [97], although some PD subjects show levels of Aβ-42 that are intermediate between those of HCS and AD subjects [98]. In PDD, the level of Aβ can fall, with relative preservation of the level of tau [99]. Two longitudinal studies of cognition in PD have found that low CSF levels of Aβ-42 are associated with a greater rate of cognitive decline [100•, 101•]. One of these studies identified a tenfold greater risk associated with low CSF levels of Aβ-42 for developing dementia in PD; in contrast, normal Aβ-42 levels were associated with a very low risk for developing dementia [101•]. In DLB subjects, CSF levels of Aβ are frequently low, relative to those in PD subjects, PDD subjects, and HCS, whereas tau levels are more variable [97, 102]. As described above, one CSF study has also explored the relation of Aβ to motor function. Consistent with PiB imaging results, that study reported that low CSF levels of Aβ-42 were associated with PIGD clinical features in PD [94]. Together, the amyloid imaging and CSF Aβ-42 reports corroborate one another.
Concordance of Amyloid Imaging and Postmortem Neuropathology in DLB and PDD
As a bulk measure of brain amyloid accumulation, amyloid PET has had remarkable success. However, it is important to keep in mind that, as described already, amyloid imaging is neither a selective marker of neuritic plaques nor a measure of total Aβ burden. Rather, amyloid imaging is a highly specific marker of fibrillar amyloid [8]. If the goal were to measure total Aβ burden, PiB would necessarily fall short, given its inability to label all Aβ species, independent of their fibrillar content [7, 90•]. In addition, because PiB stains cored and neuritic plaques reliably, but also labels those diffuse plaques that contain fibrillar amyloid in a dose-dependent manner [4–6, 103], as well as cerebral amyloid angiopathy [9, 10, 103, 104], variation in the proportions of neuritic and diffuse plaques in PD and DLB subjects could conceivably contribute to differences in their amyloid imaging characteristics. These caveats constrain interpretation of amyloid imaging, in general and in PD, PDD, and DLB. Nonetheless, the accumulating data reviewed here suggest that the amyloid species that PiB detects are detrimental, and the ability to measure them antemortem is proving valuable.
Outstanding Issues
The observation that brain amyloid burden is often high in DLB, overlapping with that in AD, along with the high frequency of elevated amyloid deposition in HCS, constrains the specificity of amyloid imaging as a marker of clinical or preclinical AD. As DLB is the second most common neurodegenerative dementia, after AD [105, 106], positive amyloid imaging in dementia may signify DLB. Similarly, it will be important to determine the extent to which positive amyloid imaging in MCI patients or in healthy patients may portend future DLB rather than AD.
In addition, the possible contribution of even modest levels of cortical amyloid deposition to cognitive decline in PD is noteworthy. Some data suggest that the cognitive repercussions of amyloid burden in PD and DLB should be more severe than in the general population. On the one hand, amyloid burden may be an independent contributor to cognitive decline in PD and DLB, and amyloid deposition may occur sporadically in PD and DLB as it does in the general population. However, a number of studies have demonstrated a synergistic relationship between α-synuclein and Aβ deposition. For example, Aβ-42 and α-synuclein increase each other’s toxicity and aggregation [107, 108•]. Aβ deposition may therefore contribute to cognitive impairment in PD both directly, as it would in the general population, and indirectly, by enhancing α-synuclein toxicity. As a result, Aβ may be more toxic in the synucleinopathies, and patients with Lewy body disease may be unable to tolerate even modest levels of Aβ. Amyloid imaging may therefore carry particularly important prognostic information in PD and DLB.
Although PiB has been used in numerous in vitro and in vivo studies, experience with the fluorinated agents is more limited. The capacity of florbetapir and its sister compounds to label different fibrillar amyloid species in PD and DLB requires further quantification. Additional studies with these new ligands will be necessary in order to understand and interpret the imaging characteristics of these ligands in PD and DLB, as they make their way into clinical practice.
Lastly, the specific molecular cascades in which amyloid participates, and the relation of those cascades to the development of cognitive and motor symptoms in PD and DLB remain to be fully elucidated.
New Directions
Amyloid imaging is one of several imaging and nonimaging biomarkers that are contributing to our understanding of PDD and DLB. For example, fluorodeoxyglucose PET, PET and single photon emission computed tomography of the dopamine system and the cholinergic system, structural and functional MRI, and meta-iodobenzylguanidine (MIBG) imaging, which assesses sympathetic cardiac denervation, are providing important insights as well [109•, 110•]. Nonimaging biomarkers of the CSF and blood are also promising [109•, 110•]. Increasingly, applying these tools together is proving informative. For example, amyloid imaging and dopamine terminal (vesicular monoamine transporter) imaging have been acquired together to differentiate DLB from AD and FTD [86•] and from AD subjects, PD subjects, and HCS [78•]. This approach may be useful for distinguishing the causes of MCI as well [111].
By expanding imaging to multimodal PET, researchers are beginning to dissect molecular cascades associated with cognition in PD and DLB. For example, brain inflammatory changes that are characteristic of AD are increasingly amenable to PET measurement. Using the PET ligand [11C]PK11195 as a marker of microglial activation, along with PiB imaging, one study has found evidence for voxel-level correlations between microglial activation and amyloid burden in PD and PDD [77]. Nonspecific and variable binding of [11C]PK11195 has complicated its use, however, and next-generation studies with more sensitive ligands such as [11C]PBR28 are under way. These tools may help to determine the relative timing of amyloid deposition and microglial activation, and their relation to cognitive impairment in PD and DLB.
Tau aggregates are also becoming an important molecular imaging target. Paired helical filaments of tau (PHF-tau) progressively accumulate in the medial temporal lobe in AD and spread to neocortex as the disease progresses [112]. Recent reports have demonstrated propagation of tau aggregates in cell culture and animal models, with trans-synaptic spread [112], raising the possibility that tau propagation may contribute to progression of disease. Interestingly, PHF-tau deposition has also been reported in PDD [49, 55] and DLB [55, 57], with greater deposition and spread than PD, reflected in higher Braak NFT stage [55]. These results suggest that the molecular processes associated with PHF-tau deposition may also contribute to cognitive impairment in PD and DLB. It is also noteworthy that NFTs are the dominant abnormality associated with the parkinsonian tauopathies—progressive supranuclear palsy and corticobasal ganglionic degeneration [112]—and that the regional distributions of NFTs in progressive supranuclear palsy and corticobasal ganglionic degeneration are distinct from those in AD, PDD, and DLB.
In this context, PET ligands for PHF-tau molecular imaging are being developed and characterized [25, 113–118]. Preliminary results for some ligands are quite promising, with greater affinity for tau than for Aβ in vitro and with a distribution of retention in human AD subjects that is reminiscent of Braak NFT staging [115–118]. If successful, PHF-tau PET will have broad applicability for the study of the parkinsonian dementias. Such ligands will be useful not only to explore the relation of PHF-tau burden to cognition and clinical course in the Lewy body diseases but also to differentiate the synucleinopathies and the parkinsonian tauopathies.
A PET ligand for α-synuclein is not yet available. The future development of such a marker will have widespread application in understanding and diagnosing PD, PDD, and DLB.
Conclusion
Amyloid imaging provides a noninvasive means to assess brain amyloid burden antemortem. To date, PD and DLB studies using amyloid imaging are broadly consistent with studies of CSF Aβ-42 and neuropathology. Together, these results suggest that Aβ deposition contributes to cognitive impairment in both PD and DLB. More work is needed to confirm these early observations, however. Notably, cortical amyloid deposition is common in DLB and is not specific to AD. Therapeutic trials in AD can now leverage amyloid imaging both to identify and to stratify subjects and as a surrogate measure of therapeutic success. The development of anti-amyloid therapeutics, if successful, would have a large impact on research in PD and DLB, as well as immediate application in the treatment of these patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Klunk WE, Engler H, Nordberg A, Wang Y, Blomqvist G, Holt DP, et al. Imaging brain amyloid in Alzheimer's disease with Pittsburgh Compound-B. Ann Neurol. 2004;55:306–19.
Mathis CA, Wang Y, Holt DP, Huang GF, Debnath ML, Klunk WE. Synthesis and evaluation of 11C-labeled 6-substituted 2-arylbenzothiazoles as amyloid imaging agents. J Med Chem. 2003;46:2740–54.
Klunk WE, Lopresti BJ, Ikonomovic MD, Lefterov IM, Koldamova RP, Abrahamson EE, et al. Binding of the positron emission tomography tracer Pittsburgh compound-B reflects the amount of amyloid-β in Alzheimer's disease brain but not in transgenic mouse brain. J Neurosci. 2005;25:10598–606.
Ikonomovic MD, Klunk WE, Abrahamson EE, Mathis CA, Price JC, Tsopelas ND, et al. Post-mortem correlates of in vivo PiB-PET amyloid imaging in a typical case of Alzheimer's disease. Brain. 2008;131:1630–45.
Burack MA, Hartlein J, Flores HP, Taylor-Reinwald L, Perlmutter JS, Cairns NJ. In vivo amyloid imaging in autopsy-confirmed Parkinson disease with dementia. Neurology. 2010;74:77–84.
Kantarci K, Yang C, Schneider JA, Senjem ML, Reyes DA, Lowe VJ, et al. Antemortem amyloid imaging and β-amyloid pathology in a case with dementia with Lewy bodies. Neurobiol Aging. 2012;33:878–85.
Fodero-Tavoletti MT, Smith DP, McLean CA, Adlard PA, Barnham KJ, Foster LE, et al. In vitro characterization of Pittsburgh compound-B binding to Lewy bodies. J Neurosci. 2007;27:10365–71.
Klunk WE, Wang Y, Huang GF, Debnath ML, Holt DP, Shao L, et al. The binding of 2-(4'-methylaminophenyl)benzothiazole to postmortem brain homogenates is dominated by the amyloid component. J Neurosci. 2003;23:2086–92.
Johnson KA, Gregas M, Becker JA, Kinnecom C, Salat DH, Moran EK, et al. Imaging of amyloid burden and distribution in cerebral amyloid angiopathy. Ann Neurol. 2007;62:229–34.
Bacskai BJ, Frosch MP, Freeman SH, Raymond SB, Augustinack JC, Johnson KA, et al. Molecular imaging with Pittsburgh compound B confirmed at autopsy: a case report. Arch Neurol. 2007;64:431–4.
Mintun MA, Larossa GN, Sheline YI, Dence CS, Lee SY, Mach RH, et al. [11C]PIB in a nondemented population: potential antecedent marker of Alzheimer disease. Neurology. 2006;67:446–52.
Morris JC, Roe CM, Xiong C, Fagan AM, Goate AM, Holtzman DM, et al. APOE predicts amyloid-beta but not tau Alzheimer pathology in cognitively normal aging. Ann Neurol. 2010;67:122–31.
Villemagne VL, McLean CA, Reardon K, Boyd A, Lewis V, Klug G, et al. 11C-PiB PET studies in typical sporadic Creutzfeldt-Jakob disease. J Neurol Neurosurg Psychiatry. 2009;80:998–1001.
Drzezga A, Grimmer T, Henriksen G, Stangier I, Perneczky R, Diehl-Schmid J, et al. Imaging of amyloid plaques and cerebral glucose metabolism in semantic dementia and Alzheimer's disease. Neuroimage. 2008;39:619–33.
Rowe CC, Ackerman U, Browne W, Mulligan R, Pike KL, O'Keefe G, et al. Imaging of amyloid β in Alzheimer's disease with 18F-BAY94-9172, a novel PET tracer: proof of mechanism. Lancet Neurol. 2008;7:129–35.
Wong DF, Rosenberg PB, Zhou Y, Kumar A, Raymont V, Ravert HT, et al. In vivo imaging of amyloid deposition in Alzheimer disease using the radioligand 18F-AV-45 (florbetapir [corrected] F 18). J Nucl Med. 2010;51:913–20.
Clark CM, Schneider JA, Bedell BJ, Beach TG, Bilker WB, Mintun MA, et al. Use of florbetapir-PET for imaging β-amyloid pathology. JAMA. 2011;305:275–83.
Nelissen N, Van Laere K, Thurfjell L, Owenius R, Vandenbulcke M, Koole M, et al. Phase 1 study of the Pittsburgh compound B derivative 18F-flutemetamol in healthy volunteers and patients with probable Alzheimer disease. J Nucl Med. 2009;50:1251–9.
Vandenberghe R, Van Laere K, Ivanoiu A, Salmon E, Bastin C, Triau E, et al. 18F-flutemetamol amyloid imaging in Alzheimer disease and mild cognitive impairment: a phase 2 trial. Ann Neurol. 2010;68:319–29.
Lister-James J, Pontecorvo MJ, Clark C, Joshi AD, Mintun MA, Zhang W, et al. Florbetapir F-18: a histopathologically validated beta-amyloid positron emission tomography imaging agent. Semin Nucl Med. 2011;41:300–4.
Clark CM, Pontecorvo MJ, Beach TG, Bedell BJ, Coleman RE, Doraiswamy PM, et al. Cerebral PET with florbetapir compared with neuropathology at autopsy for detection of neuritic amyloid-β plaques: a prospective cohort study. Lancet Neurol. 2012;11:669–78.
Wong DF, Moghekar AR, Rigamonti D, Brašić JR, Rousset O, Willis W, et al. An in vivo evaluation of cerebral cortical amyloid with [18F]flutemetamol using positron emission tomography compared with parietal biopsy samples in living normal pressure hydrocephalus patients. Mol Imaging Biol. 2013;15:230–7.
Villemagne VL, Ong K, Mulligan RS, Holl G, Pejoska S, Jones G, et al. Amyloid imaging with 18F-florbetaben in Alzheimer disease and other dementias. J Nucl Med. 2011;52:1210–7. Florbetaben was used to assess and compare amyloid burden in AD subjects, DLB subjects, PD subjects, FTD subjects, vascular dementia subjects, and HCS, and demonstrated results similar to those obtained with PiB.
Landau SM, Thomas BA, Thurfjell L, Schmidt M, Margolin R, Mintun M, et al. Alzheimer’s Disease Neuroimaging Initiative. Amyloid PET imaging in Alzheimer's disease: a comparison of three radiotracers. Eur J Nucl Med Mol Imaging. 2014. doi:10.1007/s00259-014-2753-3. This article showed high correlation in PET characteristics among PiB, florbetapir, and flutemetamol.
Small GW, Kepe V, Ercoli LM, Siddarth P, Bookheimer SY, Miller KJ, et al. PET of brain amyloid and tau in mild cognitive impairment. N Engl J Med. 2006;355:2652–63.
Smid LM, Vovko TD, Popovic M, Petric A, Kepe V, Barrio JR, et al. The 2,6-disubstituted naphthalene derivative FDDNP labeling reliably predicts Congo red birefringence of protein deposits in brain sections of selected human neurodegenerative diseases. Brain Pathol. 2006;16:124–30.
Gomperts SN, Rentz DM, Moran E, Becker JA, Locascio JJ, Klunk WE, et al. Imaging amyloid deposition in Lewy body diseases. Neurology. 2008;71:903–10.
Aizenstein HJ, Nebes RD, Saxton JA, Price JC, Mathis CA, Tsopelas ND, et al. Frequent amyloid deposition without significant cognitive impairment among the elderly. Arch Neurol. 2008;65:1509–17.
Rowe CC, Ellis KA, Rimajova M, Bourgeat P, Pike KE, Jones G, et al. Amyloid imaging results from the Australian Imaging, Biomarkers and Lifestyle (AIBL) study of aging. Neurobiol Aging. 2010;31:1275–83.
Kantarci K, Lowe V, Przybelski SA, Weigand SD, Senjem ML, Ivnik RJ, et al. APOE modifies the association between Aβ load and cognition in cognitively normal older adults. Neurology. 2012;78:232–40.
Landau SM, Mintun MA, Joshi AD, Koeppe RA, Petersen RC, Aisen PS, et al. Amyloid deposition, hypometabolism, and longitudinal cognitive decline. Ann Neurol. 2012;72:578–86.
Lim YY, Ellis KA, Ames D, Darby D, Harrington K, Martins RN, et al. Aβ amyloid, cognition, and APOE genotype in healthy older adults. Alzheimers Dement. 2013;9:538–45.
Hedden T, Oh H, Younger AP, Patel TA. Meta-analysis of amyloid-cognition relations in cognitively normal older adults. Neurology. 2013;80:1341–8.
Doraiswamy PM, Sperling RA, Coleman RE, Johnson KA, Reiman EM, Davis MD, et al. Amyloid-β assessed by florbetapir F 18 PET and 18-month cognitive decline: a multicenter study. Neurology. 2012;79:1636–44.
Doraiswamy PM, Sperling RA, Johnson K, Reiman EM, Wong TZ, Sabbagh MN, et al. AV45-A11 Study Group. Florbetapir F 18 amyloid PET and 36-month cognitive decline: a prospective multicenter study. Mol Psychiatry. 2014. doi:10.1038/mp.2014.9.
Ossenkoppele R, van der Flier WM, Verfaillie SC, Vrenken H, Versteeg A, van Schijndel RA, et al. Long-term effects of amyloid, hypometabolism, and atrophy on neuropsychological functions. Neurology. 2014;82:1768–75.
Villemagne VL, Pike KE, Chételat G, Ellis KA, Mulligan RS, Bourgeat P, et al. Longitudinal assessment of Aβ and cognition in aging and Alzheimer disease. Ann Neurol. 2011;69:181–92.
Locascio JJ, Corkin S, Growdon JH. Relation between clinical characteristics of Parkinson's disease and cognitive decline. J Clin Exp Neuropsychol. 2003;25:94–109.
Mortimer JA, Pirozzolo FJ, Hansch EC, Webster DD. Relationship of motor symptoms to intellectual deficits in Parkinson disease. Neurology. 1982;32:133–7.
Litvan I, Aarsland D, Adler CH, Goldman JG, Kulisevsky J, Mollenhauer B, et al. MDS task force on mild cognitive impairment in Parkinson’s disease: critical review of PD-MCI. Mov Disord. 2011;26:1814–24.
Mayeux R, Denaro J, Hemenegildo N, Marder K, Tang MX, Cote LJ, et al. A population-based investigation of Parkinson's disease with and without dementia. Relationship to age and gender Arch Neurol. 1992;49:492–7.
Aarsland D, Andersen K, Larsen JP, Lolk A, Kragh-Sorensen P. Prevalence and characteristics of dementia in Parkinson disease: an 8-year prospective study. Arch Neurol. 2003;60:387–92.
Emre M, Aarsland D, Brown R, Burn DJ, Duyckaerts C, Mizuno Y, et al. Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord. 2007;22:1689–707.
McKeith IG, Dickson DW, Lowe J, Emre M, O'Brien JT, Feldman H, et al. Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology. 2005;65:1863–72.
Lippa CF, Duda JE, Grossman M, Hurtig HI, Aarsland D, Boeve BF, et al. DLB and PDD boundary issues: diagnosis, treatment, molecular pathology, and biomarkers. Neurology. 2007;68:812–9.
Rinne JO, Rummukainen J, Paljarvi L, Rinne UK. Dementia in Parkinson's disease is related to neuronal loss in the medial substantia nigra. Ann Neurol. 1989;26:47–50.
Tiraboschi P, Hansen LA, Alford M, Sabbagh MN, Schoos B, Masliah E, et al. Cholinergic dysfunction in diseases with Lewy bodies. Neurology. 2000;54:407–11.
Kasten M, Klein C. The many faces of alpha-synuclein mutations. Mov Disord. 2013;28:697–701.
Horvath J, Herrmann FR, Burkhard PR, Bouras C, Kövari E. Neuropathology of dementia in a large cohort of patients with Parkinson's disease. Parkinsonism Relat Disord. 2013;19:864–8.
Harding AJ, Halliday GM. Cortical Lewy body pathology in the diagnosis of dementia. Acta Neuropathol. 2001;102:355–63.
Irwin DJ, White MT, Toledo JB, Xie SX, Robinson JL, Van Deerlin V, et al. Neuropathologic substrates of Parkinson disease dementia. Ann Neurol. 2012;72:587–98.
Nemani VM, Lu W, Berge V, Nakamura K, Onoa B, Lee MK, et al. Increased expression of alpha-synuclein reduces neurotransmitter release by inhibiting synaptic vesicle reclustering after endocytosis. Neuron. 2010;65:66–79.
Schulz-Schaeffer WJ. The synaptic pathology of alpha-synuclein aggregation in dementia with Lewy bodies, Parkinson's disease and Parkinson's disease dementia. Acta Neuropathol. 2010;120:131–43.
Halliday GM, Leverenz JB, Schneider JS, Adler CH. The neurobiological basis of cognitive impairment in Parkinson's disease. Mov Disord. 2014;29:634–50.
Jellinger KA, Attems J. Prevalence and impact of vascular and Alzheimer pathologies in Lewy body disease. Acta Neuropathol. 2008;115:427–36.
Kövari E, Horvath J, Bouras C. Neuropathology of Lewy body disorders. Brain Res Bull. 2009;80:203–10.
Colom-Cadena M, Gelpi E, Charif S, Belbin O, Blesa R, Martí MJ, et al. Confluence of α-synuclein, tau, and β-amyloid pathologies in dementia with Lewy bodies. J Neuropathol Exp Neurol. 2013;72:1203–12.
Jellinger KA, Seppi K, Wenning GK, Poewe W. Impact of coexistent Alzheimer pathology on the natural history of Parkinson's disease. J Neural Transm. 2002;109:329–39.
Mattila PM, Röyttä M, Torikka H, Dickson DW, Rinne JO. Cortical Lewy bodies and Alzheimer-type changes in patients with Parkinson's disease. Acta Neuropathol. 1998;95:576–82.
Compta Y, Parkkinen L, O'Sullivan SS, Vandrovcova J, Holton JL, Collins C, et al. Lewy- and Alzheimer-type pathologies in Parkinson's disease dementia: which is more important? Brain. 2011;134:1493–505.
Braak H, Braak E. Cognitive impairment in Parkinson's disease: amyloid plaques, neurofibrillary tangles, and neuropil threads in the cerebral cortex. J Neural Transm Park Dis Dement Sect. 1990;2:45–57.
Sabbagh MN, Adler CH, Lahti TJ, Connor DJ, Vedders L, Peterson LK, et al. Parkinson disease with dementia: comparing patients with and without Alzheimer pathology. Alzheimer Dis Assoc Disord. 2009;23:295–7.
Selikhova M, Williams DR, Kempster PA, Holton JL, Revesz T, Lees AJ. A clinico-pathological study of subtypes in Parkinson's disease. Brain. 2009;132:2947–57.
Ballard C, Ziabreva I, Perry R, Larsen JP, O'Brien J, McKeith I, et al. Differences in neuropathologic characteristics across the Lewy body dementia spectrum. Neurology. 2006;67:1931–4.
Fujishiro H, Iseki E, Higashi S, Kasanuki K, Murayama N, Togo T, et al. Distribution of cerebral amyloid deposition and its relevance to clinical phenotype in Lewy body dementia. Neurosci Lett. 2010;486:19–23.
McKeith IG, Ballard CG, Perry RH, Ince PG, O'Brien JT, Neill D, et al. Prospective validation of consensus criteria for the diagnosis of dementia with Lewy bodies. Neurology. 2000;54:1050–8.
Dickson DW. Dementia with Lewy bodies: neuropathology. J Geriatr Psychiatry Neurol. 2002;15:210–6.
Kalaitzakis ME, Walls AJ, Pearce RK, Gentleman SM. Striatal Aβ peptide deposition mirrors dementia and differentiates DLB and PDD from other parkinsonian syndromes. Neurobiol Dis. 2011;41:377–84.
Kotzbauer PT, Cairns NJ, Campbell MC, Willis AW, Racette BA, Tabbal SD, et al. Pathologic accumulation of α-synuclein and Aβ in Parkinson disease patients with dementia. Arch Neurol. 2012;69:1326–31.
Jellinger KA, Wenning GK, Seppi K. Predictors of survival in dementia with Lewy bodies and Parkinson dementia. Neurodegener Dis. 2007;4:428–30.
Edison P, Rowe CC, Rinne JO, Ng S, Ahmed I, Kemppainen N, et al. Amyloid load in Parkinson's disease dementia and Lewy body dementia measured with [11C]PIB positron emission tomography. J Neurol Neurosurg Psychiatry. 2008;79:1331–8.
Johansson A, Savitcheva I, Forsberg A, Engler H, Långström B, Nordberg A, et al. [11C]-PIB imaging in patients with Parkinson's disease: preliminary results. Parkinsonism Relat Disord. 2008;14:345–7.
Maetzler W, Liepelt I, Reimold M, Reischl G, Solbach C, Becker C, et al. Cortical PIB binding in Lewy body disease is associated with Alzheimer-like characteristics. Neurobiol Dis. 2009;34:107–12.
Foster ER, Campbell MC, Burack MA, Hartlein J, Flores HP, Cairns NJ, et al. Amyloid imaging of Lewy body-associated disorders. Mov Disord. 2010;25:2516–23.
Jokinen P, Scheinin N, Aalto S, Någren K, Savisto N, Parkkola R, et al. [11C]PIB-, [18F]FDG-PET and MRI imaging in patients with Parkinson's disease with and without dementia. Parkinsonism Relat Disord. 2010;16:666–70.
Gomperts SN, Locascio JJ, Marquie M, Santarlasci AL, Rentz DM, Maye J, et al. Brain amyloid and cognition in Lewy body diseases. Mov Disord. 2012;27:965–73. This article confirmed prior results showing greater PiB retention in DLB compared with PDD and PD and showed that age and apolipoprotein ε4 contribute to PiB burden in Lewy body diseases, as they do in HCS and AD subjects.
Edison P, Ahmed I, Fan Z, Hinz R, Gelosa G, Ray Chaudhuri K, et al. Microglia, amyloid, and glucose metabolism in Parkinson's disease with and without dementia. Neuropsychopharmacology. 2013;38:938–49.
Siderowf A, Pontecorvo MJ, Shill HA, Mintun MA, Arora A, Joshi AD, et al. PET imaging of amyloid with Florbetapir F 18 and PET imaging of dopamine degeneration with 18F-AV-133 (florbenazine) in patients with Alzheimer's disease and Lewy body disorders. BMC Neurol. 2014;14:79. Florbetapir and the vesicular monoamine transporter ligand florbenazine were used to differentiate between AD subjects, DLB subjects, PD subjects, and HCS.
Kepe V, Bordelon Y, Boxer A, Huang SC, Liu J, Thiede FC, et al. PET imaging of neuropathology in tauopathies: progressive supranuclear palsy. J Alzheimers Dis. 2013;36:145–53.
Petrou M, Bohnen NI, Müller ML, Koeppe RA, Albin RL, Frey KA. Aβ-amyloid deposition in patients with Parkinson disease at risk for development of dementia. Neurology. 2012;79:1161–7.
Gomperts SN, Locascio JJ, Rentz D, Santarlasci A, Marquie M, Johnson KA, et al. Amyloid is linked to cognitive decline in patients with Parkinson disease without dementia. Neurology. 2013;80:85–91. This article shows that baseline amyloid burden predicts cognitive decline in PD.
Maetzler W, Reimold M, Liepelt I, Solbach C, Leyhe T, Schweitzer K, et al. [11C]PIB binding in Parkinson's disease dementia. Neuroimage. 2008;39:1027–33.
Shimada H, Shinotoh H, Hirano S, Miyoshi M, Sato K, Tanaka N, et al. β-Amyloid in Lewy body disease is related to Alzheimer's disease-like atrophy. Mov Disord. 2013;28:169–75. This article associated amyloid burden in DLB and PDD with medial temporal lobe and cortical atrophy.
Rowe CC, Ng S, Ackermann U, Gong SJ, Pike K, Savage G, et al. Imaging β-amyloid burden in aging and dementia. Neurology. 2007;68:1718–25.
Claassen DO, Lowe VJ, Peller PJ, Petersen RC, Josephs KA. Amyloid and glucose imaging in dementia with Lewy bodies and multiple systems atrophy. Parkinsonism Relat Disord. 2011;17:160–5.
Burke JF, Albin RL, Koeppe RA, Giordani B, Kilbourn MR, Gilman S, et al. Assessment of mild dementia with amyloid and dopamine terminal positron emission tomography. Brain. 2011;134:1647–57. PiB and vesicular monoamine transporter imaging of the dopamine terminal were used to differentiate AD, DLB, and FTD subjects with mild dementia.
Kantarci K, Lowe VJ, Boeve BF, Weigand SD, Senjem ML, Przybelski SA, et al. Multimodality imaging characteristics of dementia with Lewy bodies. Neurobiol Aging. 2012;33:2091–105. This article compared AD and DLB patients using MRI, PiB imaging, and fluorodeoxyglucose imaging; a subset of patients underwent neuropathological evaluation. It found that a single imaging modality did not differentiate groups or individual patients well, but that using at least two modalities improved their discrimination.
Graff-Radford J, Boeve BF, Pedraza O, Ferman TJ, Przybelski S, Lesnick TG, et al. Imaging and acetylcholinesterase inhibitor response in dementia with Lewy bodies. Brain. 2012;135:2470–7.
Ossenkoppele R, Prins ND, Pijnenburg YA, Lemstra AW, van der Flier WM, Adriaanse SF, et al. Impact of molecular imaging on the diagnostic process in a memory clinic. Alzheimers Dement. 2013;9:414–21.
Ikonomovic MD, Abrahamson EE, Price JC, Hamilton RL, Mathis CA, Paljug WR, et al. Early AD pathology in a [C-11]PiB-negative case: a PiB-amyloid imaging, biochemical, and immunohistochemical study. Acta Neuropathol. 2012;123:433–47. This article explored the sensitivity of PiB and PiB imaging in a case of DLB with negative PiB imaging findings, and found that in some brain regions Aβ levels were significant, exceeding local plaque density and PiB binding.
Burn DJ, Rowan EN, Allan LM, Molloy S, O'Brien JT, McKeith IG. Motor subtype and cognitive decline in Parkinson's disease, Parkinson's disease with dementia, and dementia with Lewy bodies. J Neurol Neurosurg Psychiatry. 2006;77:585–9.
Alves G, Larsen JP, Emre M, Wentzel-Larsen T, Aarsland D. Changes in motor subtype and risk for incident dementia in Parkinson's disease. Mov Disord. 2006;21:1123–30.
Müller ML, Frey KA, Petrou M, Kotagal V, Koeppe RA, Albin RL, et al. β-Amyloid and postural instability and gait difficulty in Parkinson's disease at risk for dementia. Mov Disord. 2013;28:296–301. This article reported a relationship between amyloid burden and postural instability in PD with MCI.
Alves G, Pedersen KF, Bloem BR, Blennow K, Zetterberg H, Borm GF, et al. Cerebrospinal fluid amyloid-β and phenotypic heterogeneity in de novo Parkinson's disease. J Neurol Neurosurg Psychiatry. 2013;84:537–43.
Blennow K, Hampel H, Weiner M, Zetterberg H. Cerebrospinal fluid and plasma biomarkers in Alzheimer disease. Nat Rev Neurol. 2010;6:131–44.
Landau SM, Lu M, Joshi AD, Pontecorvo M, Mintun MA, Trojanowski JQ, et al. Alzheimer's Disease Neuroimaging Initiative. Comparing positron emission tomography imaging and cerebrospinal fluid measurements of β-amyloid. Ann Neurol. 2013;74:826–36. This study found that florbetapir PET findings and CSF levels of Aβ were highly correlated across HCS, MCI subjects, and AD subjects.
Hall S, Öhrfelt A, Constantinescu R, Andreasson U, Surova Y, Bostrom F, et al. Accuracy of a panel of 5 cerebrospinal fluid biomarkers in the differential diagnosis of patients with dementia and/or parkinsonian disorders. Arch Neurol. 2012;69:1445–52.
Shi M, Bradner J, Hancock AM, Chung KA, Quinn JF, Peskind ER, et al. Cerebrospinal fluid biomarkers for Parkinson disease diagnosis and progression. Ann Neurol. 2011;69:570–80.
Montine TJ, Shi M, Quinn JF, Peskind ER, Craft S, Ginghina C, et al. CSF Aβ(42) and tau in Parkinson’s disease with cognitive impairment. Mov Disord. 2010;25:2682–5.
Siderowf A, Xie SX, Hurtig H, Weintraub D, Duda J, Chen-Plotkin A, et al. CSF amyloid β 1-42 predicts cognitive decline in Parkinson disease. Neurology. 2010;75:1055–61. This article shows that the baseline CSF level of Aβ predicts cognitive decline in PD.
Alves G, Lange J, Blennow K, Zetterberg H, Andreasson U, Førland MG, et al. CSF Aβ42 predicts early-onset dementia in Parkinson disease. Neurology. 2014;82:1784–90. This article replicates the result in [100] showing that the baseline CSF level of Aβ predicts cognitive decline in PD.
Kanemaru K, Kameda N, Yamanouchi H. Decreased CSF amyloid β42 and normal tau levels in dementia with Lewy bodies. Neurology. 2000;54:1875–6.
Lockhart A, Lamb JR, Osredkar T, Sue LI, Joyce JN, Ye L, et al. PIB is a non-specific imaging marker of amyloid-beta (Aβ) peptide-related cerebral amyloidosis. Brain. 2007;130:2607–15.
Ly JV, Donnan GA, Villemagne VL, Zavala JA, Ma H, O'Keefe G, et al. 11C-PIB binding is increased in patients with cerebral amyloid angiopathy-related hemorrhage. Neurology. 2010;74:487–93.
McKeith I. Dementia with Lewy bodies. Dialogues Clin Neurosci. 2004;6:333–41.
Vann Jones SA, O'Brien JT. The prevalence and incidence of dementia with Lewy bodies: a systematic review of population and clinical studies. Psychol Med. 2014;44:673–83.
Masliah E, Rockenstein E, Veinbergs I, Sagara Y, Mallory M, Hashimoto M, et al. β-Amyloid peptides enhance α-synuclein accumulation and neuronal deficits in a transgenic mouse model linking Alzheimer's disease and Parkinson's disease. Proc Natl Acad Sci U S A. 2001;98:12245–50.
Jellinger KA. Interaction between pathogenic proteins in neurodegenerative disorders. J Cell Mol Med. 2012;16:1166–83. This review discusses synergistic interactions between Aβ, tau, and α-synuclein that could contribute to neurodegeneration in PD and DLB.
Sinha N, Firbank M, O'Brien JT. Biomarkers in dementia with Lewy bodies: a review. Int J Geriatr Psychiatry. 2012;27:443–53. This review focuses on biomarkers in DLB.
Mollenhauer B, Rochester L, Chen-Plotkin A, Brooks D. What can biomarkers tell us about cognition in Parkinson's disease? Mov Disord. 2014;29:622–33. This review discusses biomarkers in PD.
Albin RL, Burke JF, Koeppe RA, Giordani B, Gilman S, Frey KA. Assessing mild cognitive impairment with amyloid and dopamine terminal molecular imaging. J Nucl Med. 2013;54:887–93.
Spillantini MG, Goedert M. Tau pathology and neurodegeneration. Lancet Neurol. 2013;12:609–22.
Rojo LE, Alzate-Morales J, Saavedra IN, Davies P, Maccioni RB. Selective interaction of lansoprazole and astemizole with tau polymers: potential new clinical use in diagnosis of Alzheimer's disease. J Alzheimers Dis. 2010;19:573–89.
Zhang W, Arteaga J, Cashion DK, Chen G, Gangadharmath U, Gomez LF, et al. A highly selective and specific PET tracer for imaging of tau pathologies. J Alzheimers Dis. 2012;31:601–12.
Maruyama M, Shimada H, Suhara T, Shinotoh H, Ji B, Maeda J, et al. Imaging of tau pathology in a tauopathy mouse model and in Alzheimer patients compared to normal controls. Neuron. 2013;79:1094–108.
Chien DT, Bahri S, Szardenings AK, Walsh JC, Mu F, Su MY, et al. J Alzheimers Dis. 2013;34:457–68.
Chien DT, Szardenings AK, Bahri S, Walsh JC, Mu F, Xia C, et al. Early clinical PET imaging results with the novel PHF-tau radioligand [F18]-T808. J Alzheimers Dis. 2014;38:171–84.
Okamura N, Furumoto S, Fodero-Tavoletti MT, Mulligan RS, Harada R, Yates P, et al. Non-invasive assessment of Alzheimer's disease neurofibrillary pathology using 18F-THK5105 PET. Brain. 2014. doi:10.1093/brain/awu064.
Acknowledgments
Stephen N. Gomperts has grant support from the National Parkinson Foundation and has had grant support from the National Institute of Neurological Disorders and Stroke NINDS and the National Institute of Mental Health.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Stephen N. Gomperts declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Neuroimaging
Rights and permissions
About this article
Cite this article
Gomperts, S.N. Imaging the Role of Amyloid in PD Dementia and Dementia with Lewy Bodies. Curr Neurol Neurosci Rep 14, 472 (2014). https://doi.org/10.1007/s11910-014-0472-6
Published:
DOI: https://doi.org/10.1007/s11910-014-0472-6