Abstract
Progressive multifocal leukoencephalopathy (PML) is a severe, often fatal, opportunistic viral infection of the central nervous system that is mainly seen in the context of AIDS and certain monoclonal immune-suppressive therapies. The causative agent, a polyoma virus, named JC virus infects only humans and there is no animal model for PML. This update focuses on information gathered in recent years on the pathogenesis of the disorder, on several clinical aspects associated with diagnosis and therapy, and on the immune reconstitution inflammatory syndrome (IRIS), a complication associated with removal of immunosuppressive therapy in PML.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Progressive multifocal leukoencephalopathy (PML) is a severe, often fatal, opportunistic infection of the central nervous system (CNS). First reported in 1958 as a white matter disorder in 3 patients with lymphoproliferative disorders [1]. Subsequent studies revealed that the causative agent was a polyoma virus, named JC virus from the initials of the patient from whose brain it was initially isolated [2]. Despite previous reports [3], there is no evidence that PML is caused by either the SV40 [4] or BK virus.
The pathogen is a ubiquitous DNA virus. Subclinical infection often takes place within the first decade of life. By adulthood, 50 % [5•] to more than 80 % of the population is seropositive for the virus [6, 7]. Differences in the rates of seropositivity appear to reflect differences in methodology; however, a consistent decade by decade increase in seropositivity has been demonstrated in most studies, though at much lower rates than that observed during childhood and adolescence. Both the mechanism of infection and clinical expression of primary infection remain undefined. As the virus can be isolated from sewage worldwide, it was proposed that contaminated food and water are the mode of infection [8].
PML can be classified into several epochs [9]. The earliest epoch encompasses the times from its initial description to the early 1980s when it was predominantly associated with lymphoproliferative disorders [10]. During this time, it was regarded as a rare disorder and a comprehensive worldwide review was able to identify only 230 cases [10]. With the AIDS pandemic, PML became strikingly prevalent as it was observed in 4 % to 5 % of all patients with HIV prior to the availability of highly active anti-retroviral therapy (HAART) [11, 12]. Despite effective HAART and reductions in the incidence AIDS-associated PML, it still remains one of the 4 most common CNS opportunistic infections affecting AIDS patients [13]. The third epoch of PML was heralded by the era of monoclonal antibodies (mAbs) as therapeutic agents for immune-mediated conditions. Several mAbs have been identified as setting the stage to PML, notably natalizumab (Tysabri) and efalizumab (Raptiva), and there appears to be an increased risk with other mAbs, such as, rituximab (Maptera), as well as other therapeutic agents, such as, mycophenolate mofetil (CellCept).
The JC virus infects only humans and there is no animal model for PML. Thus, the study of the disease is limited to observation of the condition in humans or to tissue culture. The remarkable occurrence of PML with HIV and mAbs has resulted in an increased accumulation of data on the expression and pathogenesis of disorder. This update will focus on these aspects.
Monoclonal Antibodies and Putative Pathogenesis of PML
Of all mAbs, natalizumab as a predisposing agent for PML has attracted the greatest attention. Natalizumab is an α4β1 and α4β7 antagonist approved for the treatment of relapsing-remitting MS and Crohn's disease. The effect of natalizumab is attributed to its binding, among others, to integrin, inhibiting leukocyte migration and extravasation. It might also affect T and B lymphocytes differentiation [14]. Natalizumab was withdrawn from the market in 2005, after 3 cases of PML had been identified in clinical trials [15]. Two were MS patients also on β-interferon 1a therapy [16, 17] and the third was a Crohn’s disease patient [18]. No association between MS or Crohn’s had been previously noted. After the establishment of a global risk-management program, natalizumab was reintroduced to the market in 2006. As of June 6, 2012, 258 cases of PML have been observed in patients treated with natalizumab during the postmarketing phase [19]. The risk of developing PML in the context of natalizumab increases with several factors alone or in combination: previous immune-suppressive therapy, duration of therapy, and seropositivity to JC virus [20•]. The shortest duration from the time of introduction of natalizumab to the development of PML appears to be 8 months and the risk clearly significantly increases at 24 months [20•].
Efalizumab is an anti-CD11a IgG1 antibody in use for psoriasis [21]. Efalizumab inhibits T-cell activation in lymph nodes and blocks trafficking of T-cells from the circulation into the psoriatic skin [22]. It was removed from the market in 2009 following a confirmed diagnosis of PML in 3 patients and suspected PML in a fourth. All were on treatment for more than 3 years. As with natalizumab, PML had not previously been reported with psoriasis.
These 2 mAbs, natalizumab and efalizumab, appear to have a unique ability to predispose to PML and have been considered as Class I agents in this regard [9]. In addition to the fact that MS, Crohn’s, and psoriasis have not been associated with a risk for PML. In addition, there is a latency from the time of introduction of the mAb to the time of development of PML suggesting that this is not simply a stochastic event. Lastly, the incidence of PML with these 2 agents exceeds by orders of magnitude the risk with other agents that have been identified as increasing the risk of PML.
Rituximab, an anti-CD20 compound aimed at B-lymphocytes in use mainly for lymphoproliferative diseases, but also for other conditions of putative immune-mediated pathogenesis. Between 1997 and 2008, 52 patients with lymphoproliferative disorders (generally B cell malignancies), 2 with SLE, 1 with rheumatoid arthritis, and 1 with autoimmune pancytopenia have been reported with PML while under rituximab therapy [23]. However, all were also on other immunosuppressive protocols and B-cell malignancies are the second most common predisposing factor for PML, after HIV/AIDS. PML has been reported both in SLE and rheumatoid arthritis in the absence of rituximab therapy. Thus, the causative role of rituximab in inducing PML is not established. It was even argued that the use of rituximab after high dose therapy and hematopoietic stem cell transplantation delays the onset of PML [24]. Nonetheless, there does appear to be a slight increased risk. Rituximab is regarded as a Class II drug for PML since in that the conditions that it is used for, typically predisposed to PML, there is no latent period to the development of PML, and the increased risk for the disorder is low [9].
These 3 agents have different mechanisms of actions, but they all are associated with PML. What can be learned from this cause and effect relationship on the possible pathogenesis of PML in the human brain?
As PML is an isolated CNS disease and the majority of the population is JC virus infected, the healthy human nervous system most probably possesses effective means to prevent PML. Intervention and damage to these barriers is the context that leads to the ability of the virus to effectively propagate in oligodendrocytes and cause the disorder [25].
Several prerequisites have to be met at first. These include both viral and host requirements.
-
1.
Primary infection has to take place. The portal of entry and site of primary infection is probably the oropharyngeal pathway.
-
2.
Following first cycle of replication the virus has to disseminate and to establish latent or persistent infection. The sites of latent or persistent infection have not been systematically studied, but appear to be widespread and include the kidney and lymphoproliferative tissues (bone marrow, spleen, tonsils, lymph nodes) [26].
-
3.
Mutation in the JC virus genome is necessary. The virus that is ubiquitously present is referred to as the archetype virus and is the virus that likely causes primary infection. The archetype JC virus is incapable of effective replication in glial cells and must mutate into a neurotropic strain to cause disease. The mutation responsible for this has been mapped to the non-coding control region of the JC virus [27]. This mutatedvirus is found not only in PML brains but also in the tissue of healthy individuals. Gene rearrangement within the viral genome enables binding to the NF-1X binding protein found in the nuclei of glial cells, a protein shared by B-cells [28, 29]. The mechanism by which this gene rearrangement occurs remains unclear. It has been proposed that infected cells of B-cell lineage might be responsible for this genetic rearrangement using the same machinery involved in immunoglobulin synthesis [30]. Another genetic rearrangement, amino acid substitutions in the VP1 capsid protein of the virus may also play a role in virulence [31].
-
4.
Reactivation of JC virus. Like with other viruses, such as herpes simplex virus [32], the question arises whether the brain infection is the outcome of primary infection or reactivation. The preponderance of evidence indicates that PML is always or almost always the result of JC virus reactivation from latent or persistent infection. This evidence includes the following: immunoglobulins against JC virus during PML are almost always from the IgG type [33]; PML is rare in children [34]; the presence in blood [35]; or tissues [36] obtained up to 4 years earlier of JC virus with similar genetic sequences to that seen in the brain; and the detection of JC virus antibody 6 to 187 months before the development of PML in all 75 natalizumab patients with PML for whom samples were tested [19].
-
5.
Systemic immune-suppression, or the inability (present under normal immune surveillance), to keep the virus at bay. JC virus is present in peripheral blood of normal healthy controls ranging from 0 % to more than 10 %, and the likelihood of detecting circulating JC virus in PML patients increases with immunosuppression [37, 38].
-
6.
An incapacitated CNS immune response [39, 40]. An effective CNS immune surveillance can clear the virus from the brain even after established glial infection. The immune reconstitution inflammatory syndrome (IRIS) in HIV-infected individuals with PML treated with HAART and following discontinuation of natalizumab in MS patients is evidence of the importance of an effective CNS immunosurveillance in controlling the infection. JC virus-specific cytotoxic T lymphocytes appear to play a crucial role in this regard [41].
These observations lead to the following proposed course of events required to produce PML; however, the absence of an animal model makes it very difficult to be certain that this hypothesis regarding PML pathogenesis is correct and additional information may cause it to be substantially modified. Following primary infection and establishment of latent JC virus infection the virus might undergo a mutation that renders it neurotropic. In the context of chronic failed peripheral immune surveillance, JC virus will reactivate and replicate at peripheral sites including peripheral blood mononuclear cells (PBMC) and with these cells be transported to the CNS and establish productive infection in glial cells. In the absence of effective CNS immunosurveillance, PML develops. Does the risk of PML increase with prolonged exposure to immune-suppression? That PML generally occurs only after prolonged severe immunosuppression in HIV infection and that there is a latency to its development with the mAbs, natalizumab and efalizumab, certainly suggests that this is the case.
The monoclonal antibodies set the immunological stage for the development of PML both at the periphery and in the brain and maybe also have an effect, albeit indirect, on the virus as well.
-
1.
Natalizumab, by binding of the of α4β1 integrin leads to the release of lymphocytes from the bone marrow and significantly elevates circulating B cells [42]. If these cells are latently infected with JC virus, this may lead to the expression of JC virus in peripheral blood. Infection with other pathogens such as HHV-6 may transactivate the virus in the very cells that contain the genetic machinery to rearrange the virus’ transcriptional control region converting it to a neurotropic strain. Natalizumab also blocks CNS entry by lymphocytes, including JC virus-specific cytotoxic lymphocytes that correlate with PML survival [43, 44]. Moreover, dendritic cells have been demonstrated to be instrumental in the expansion of the JC virus-CTL response [45]. In 1 patient with natalizumab-associated PML, autopsy revealed a significant decrease in CD209+ dendritic cells in cerebral perivascular spaces and no CD4+ T cells were detected in the brain tissue [46]. Therefore, there appears to be multiple insults to the immune system that predispose to the development of PML under natalizumab.
-
2.
Efalizumab affects the immune system in a fashion similar to natalizumab. It inhibits T cell activation, migration, and reactivation [47, 48], and reduces the chemotactic properties of monocytes and neutrophils and downregulates VLA4 [49]. Dendritic cells in the skin are significantly decreased after efalizumab treatment [50]. Reduced transendothelial migration by peripheral T cells in vitro and peripheral and CSF T-cell spectratyping showed CD8 T-cell clonal expansion but blunted activation in 2 patients with efalizumab-associated PML [51•]. This suggests that inhibition of peripheral and intrathecal T-cell activation and suppression of CNS effector-phase migration both characterize efalizumab-associated PML.
-
3.
Rituximab causes profound B cell depletion. Many of the mechanisms operant with natalizumab that predispose to PML also appear to be present with rituximab. For example, the migration of pre-B cells into the peripheral circulation in response to B cell depletion. However, rituximab-associated PML was reported only in patients who received other immunosuppressive drugs and had, with rare exception, underlying disorders that predispose to PML [23]. Furthermore, rituximab also reduces CD3 T cells in the CSF [52], but the temporal profile and functional consequences of a reduction in T cells in patients treated with rituximab is unknown.
These 3 mAbs highlight the potential importance of B lymphocytes in the life cycle of JC virus [53]. Regulatory region sequences from JC virus DNA in peripheral blood of PML patients are not related to the archetype, but are closely related to sequences found in the PML brain [38]. In a report of 19 PML patients, over 90 % had JC virus DNA in peripheral blood lymphocytes as compared with 30 % of renal transplant recipients, and approximately 5 % of normal, healthy volunteers [54]. In relatively immunologically healthy HIV-infected persons on HAART, the likelihood of finding JC virus DNA in circulating lymphocytes appears to parallel that of the normal population [55]. Other lines of evidence pointing to the importance of the B-cell in the pathogenesis of PML are the high frequency with which the disorder is observed in B-cell malignancies, such as, chronic lymphocytic leukemia and Hodgkins disease, and therapies that affect B-cell function, such as, natalizumab, or rituximab.
Although not universally accepted, it appears that JC virus may reside in the brain in an inactive or latent form. (reviewed in White and Khalili [56]). JC virus DNA has been detected in the brain tissue of normal individuals [57], but its significance is uncertain and the full cycle of active viral replication occurs without other factors supervening.
Immune Reconstitution Inflammatory Syndrome (IRIS)
HAART has a significant beneficial impact upon the prognosis of PML in HIV patients [39]. The introduction of HAART led to the recognition of the immune reconstitution inflammatory syndrome (IRIS), an entity that is not unique to PML. IRIS is the consequence of rapid entry of immune cells into the brain at the time of immune restoration [58]. The likelihood of its appearance is increased with preexisting opportunistic infection, initiation of HAART, a low CD4 count, and a considerable decline in HIV viral load following HAART [59, 60]. Genetic factors may also contribute [61]. As many as 23 % AIDS patients with PML who recently started HAART will develop PML-IRIS [40, 62]. IRIS has also occurred in the majority of natalizumab-associated PML patients following withdrawal of the mAb and plasma exchange [63, 64]. The diagnosis of CNS-IRIS in MS patients with natalizumab-associated PML can be challenging since the deterioration might also be attributed to PML, MS or some other opportunistic infection, and there are no currently widely accepted criteria to establish the diagnosis [65•]. CNS-IRIS is defined as the paradoxical worsening of the neurological condition during immune recovery in an individual with a CNS infection. It is mainly determined by the severity of the immune suppression (in HIV-infected patients, it is the CD4 nadir [57] and the speed of immune reconstitution. IRIS may occur in 2 different settings: (1) The “paradoxical” form that takes place when an opportunistic infection initially responds to treatment but then deteriorates following HAART initiation; (2) The “unmasking” form occurs when an opportunistic infection remains undiagnosed and immune recovery following HAART initiation triggers deterioration with unusual inflammatory features. IRIS is associated with a wide spectrum of pathogens including mycobacterial diseases, leprosy, fungal infections, herpes viruses, and PML [66].
An essential feature of CNS-IRIS is the infiltration of the brain with activated T cells in an attempt to control an underlying CNS opportunistic infection. While IRIS is usually characterized by contrast-enhancing lesions on MRI imaging [65•] patients with PML may develop IRIS with only mild contrast enhancement .[67].
Treatment of MS with natalizumab prevents T cell trafficking with resultant systemic and compartmental immune suppression. Active T cells reside in the peripheral blood where there is no immune suppression. When natalizumab is withdrawn in patients with PML, the T cells transport to the site of the PML lesion in the brain with ensuing enhanced inflammation. Therefore, CNS-IRIS is a virtually universal phenomenon in this context.
Treatment of CNS-IRIS is mainly empirical. As of today there is only a single study that suggested the benefit of steroids in systemic IRIS associated with pulmonary tuberculosis [68]. and no information on CNS-IRIS. Steroids have been recommended for PML-IRIS [69], but there have been no randomized controlled trials to support their use which may have unintended consequences [70]. In any case, the prognosis of PML in natalizumab-treated patients is poor with mortality rates of about 20 % and moderate to severe disability reported in more than 80 % of survivors [19, 63].
PML: Clinical Diagnosis and Therapy
Recent reviews on the clinical aspects of PML are available. [67, 71]. Several points merit comment.
Although PML is almost always a disorder of the profoundly immune-suppressed host, it has also been diagnosed without initial apparent immunosuppression. Therefore, PML should be considered in the differential diagnosis of new-onset CNS neurological white matter-related symptoms, even without immunosuppressive risk factors.
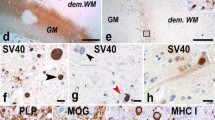
PML is mainly due to infection of oligodendrocytes and, to a lesser extent, astrocytes. Neurological deficits are therefore related to demyelination in the brain. Neuroimaging identifies affected white matter brain regions that do not correspond to vascular territories (Fig. 1). Historically, PML lesions have been described as being largely devoid of edema, mass effect, or contrast enhancement on imaging [72], but contrast enhancement has been seen in 10 % to 15 % of HIV-associated PML [73] and is frequently observed with natalizumab-associated PML [19, 63].
1.5 T MRI in patient with HIV-associated PML. a, T2 weighted image shows extensive hyperintense signal abnormality involving the white matter of the left frontal lobe with extension into the anterior limb of the internal capsule. A smaller lesion is evident in the medial right frontal lobe. b, Corresponding contrast enhanced T1 weighted shows hypointense lesion in right frontal lobe white matter extending to the gray white margin. A small area of signal hypointensity is evident in the medial right frontal lobe
The diagnosis of PML is established by detection of JC virus in the CSF by PCR in the appropriate clinical setting or by brain biopsy positive for DNA and viral antigens in the tissue combined with the typical histopathology of enlarged oligodendroglial nuclei, bizarre astrocytes, and demyelination.
There is no effective specific antiviral drug against the JC virus. Despite initial claims, no survival benefit was seen for patients who received cidofovir and cidofovir treatment did not improve PML-related residual disability by 12 months [74, 75]. Likewise, there was no improvement of survival with cytosine arabinoside by systemic or intrathecal administration [76, 77]. The finding that JC virus infects cells in culture via the 5-HT2a receptor prompted the clinical use of mirtazapine, a serotonin receptor blocker [78]. Unfortunately, the impact does not reach statistical significance in the clinical setting [79]. A screen of chemical compounds indicated that mefloquine, an antimalarial drug, could inhibit JC virus replication in a cell culture system [80]. Despite isolated case reports of the efficacy of mefloquine [81, 82] a multicenter worldwide clinical trial investigating the use of mefloquine demonstrated no effect on CSF JC viral titers.
Without an effective antiviral agent, the treatment goal in PML should be to restore the host adaptive immune response to the JC virus. In HIV-positive patients, this is accomplished by HAART. In HIV-negative patients, the main therapeutic objective is to reduce, if possible, immunosuppressive drugs, enabling the adaptive immune system to control the infection.
Conclusion
There are still many questions that are related to the biology of PML that remain unanswered or incompletely understood. For instance, is PML always the result of reactivated JC virus infection or can it happen within the context of primary infection? What are the sites of viral latency or persistence and when does it enter the brain? Is the presence of JC virus in peripheral blood or a rising JC virus antibody titer predicative of the development of PML? Would determining whether a person harbors a neurotropic strain of JC virus be a better predictor of PML? Answering these and other questions will prove enormously helpful in addressing the risks for PML following treatment with the expanding array of newer immunomodulatory drugs. It will also provide possible strategies for prevention and treatment of PML.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Astrom KE, Mancall EL, Richardson Jr EP. Progressive multifocal leuko-encephalopathy; a hitherto unrecognized complication of chronic lymphatic leukaemia and Hodgkin's disease. Brain. 1958;81:93–111.
Padgett BL, et al. Cultivation of papova-like virus from human brain with progressive multifocal leucoencephalopathy. Lancet. 1971;1:1257–60.
Weiner LP, et al. Isolation of virus related to SV40 from patients with progressive multifocal leukoencephalopathy. N Engl J Med. 1972;286:385–90.
Stoner G, Ryschkewitsch C. Evidence of JC virus in two progressive multifocal leukoencephalopathy (PML) brains previously reported to be infected with SC40. J Neuropathol Exp Neurol. 1991;50:342.
• Gorelik L, et al. Anti-JC virus antibodies: implications for PML risk stratification. Ann Neurol. 2010;68:295–303. A study from a leading group in the field that deals with reducing the risk of PML in patients about to receive immuno-suppressive therapies.
Stolt A, et al. Seroepidemiology of the human polyomaviruses. J Gen Virol. 2003;84:1499–504.
Walker D, Padgett B. The epidemiology of human polyomaviruses. In: Sever J, Madden D, editors. Polyomaviruses and human neurological disease. New York: Alan R. Liss, Inc; 1983. p. 99–106.
Bofill-Mas S, Girones R. Excretion and transmission of JCV in human populations. J Neuroviro. 2001;7:345–9.
Zaheer F, Berger JR. Treatment related progressive multifocal leukoencephalopathy: current understanding and future steps. Ther Advances Drug Safety. 2012 (in press).
Brooks BR, Walker DL. Progressive multifocal leukoencephalopathy. Neurol Clin. 1984;2:299–313.
Berger JR, et al. Progressive multifocal leukoencephalopathy associated with human immunodeficiency virus infection. A review of the literature with a report of sixteen cases. Ann Intern Med. 1987;107:78–87.
Kure K, et al. Human immunodeficiency virus-1 infection of the nervous system: an autopsy study of 268 adult, pediatric, and fetal brains. Hum Pathol. 1991;22:700–10.
Collazos J. Opportunistic infections of the CNS in patients with AIDS: diagnosis and management. CNS Drugs. 2003;17:869–87.
Polman CH, et al. A randomized, placebo-controlled trial of natalizumab for relapsing multiple sclerosis. N Engl J Med. 2006;354:899–910.
Berger JR, Koralnik IJ. Progressive multifocal leukoencephalopathy and natalizumab–unforeseen consequences. N Engl J Med. 2005;353:414–6.
Kleinschmidt-DeMasters BK, Tyler KL. Progressive multifocal leukoencephalopathy complicating treatment with natalizumab and interferon beta-1a for multiple sclerosis. N Engl J Med. 2005;353:369–74.
Langer-Gould A, et al. Progressive multifocal leukoencephalopathy in a patient treated with natalizumab. N Engl J Med. 2005;353:375–81.
Van Assche G, et al. Progressive multifocal leukoencephalopathy after natalizumab therapy for Crohn's disease. N Engl J Med. 2005;353:362–8.
BiogenIdec. PML incidence in patients receiving TYSABRI. 2012 [cited July 2, 2012]; Available at: https://medinfo.biogenidec.com/medinfo/secure/pmlresource.do?resource=TYSABRIPMLSafetyUpdate. Accessed 10 July 2012.
• Bloomgren G, et al. Risk of natalizumab-associated progressive multifocal leukoencephalopathy. N Eng J Med. 2012;366:1870–80. A recent study that assesses who is at risk to develop PML under natalizumab therapy.
Gordon KB, et al. Efalizumab for patients with moderate to severe plaque psoriasis: a randomized controlled trial. JAMA. 2003;290:3073–80.
Lebwohl M, et al. A novel targeted T-cell modulator, efalizumab, for plaque psoriasis. N Engl J Med. 2003;349:2004–13.
Carson KR, et al. Progressive multifocal leukoencephalopathy after rituximab therapy in HIV-negative patients: a report of 57 cases from the Research on adverse drug events and reports project. Blood. 2009;113:4834–40.
Garcia-Suarez J, et al. Changes in the natural history of progressive multifocal leukoencephalopathy in HIV-negative lymphoproliferative disorders: impact of novel therapies. Am J Hematol. 2005;80:271–81.
Berger JR. Progressive multifocal leukoencephalopathy in acquired immunodeficiency syndrome: explaining the high incidence and disproportionate frequency of the illness relative to other immunosuppressive conditions. J Neuroviro. 2003;9 Suppl 1:38–41.
Caldarelli-Stefano R, et al. Detection and typing of JC virus in autopsy brains and extraneural organs of AIDS patients and non-immunocompromised individuals. J Neuroviro. 1999;5:125–33.
Jensen PN, Major EO. A classification scheme for human polyomavirus JCV variants based on the nucleotide sequence of the noncoding regulatory region. J Neuroviro. 2001;7:280–7.
Major EO, et al. Glial cells of the human developing brain and B cells of the immune system share a common DNA binding factor for recognition of the regulatory sequences of the human polyomavirus, JCV. J Neurosci Res. 1990;27:461–71.
Monaco MC, et al. JC virus infection of hematopoietic progenitor cells, primary B lymphocytes, and tonsillar stromal cells: implications for viral latency. J Virol. 1996;70:7004–12.
Houff SA, Berger JR. The bone marrow, B cells, and JC virus. J Neuroviro. 2008;14:341–3.
Sunyaev SR, et al. Adaptive mutations in the JC virus protein capsid are associated with progressive multifocal leukoencephalopathy (PML). PLoS Genet. 2009;5:e1000368.
Steiner I. Herpes simplex virus encephalitis: new infection or reactivation? Curr Opin Neurol. 2011;24:268–74.
Weber F, et al. Cellular and humoral immune response in progressive multifocal leukoencephalopathy. Ann Neurol. 2001;49:636–42.
Berger JR, et al. Progressive multifocal leukoencephalopathy in HIV-1-infected children. AIDS. 1992;6:837–41.
Fedele CG, et al. Identical rearranged forms of JC polyomavirus transcriptional control region in plasma and cerebrospinal fluid of acquired immunodeficiency syndrome patients with progressive multifocal leukoencephalopathy. J Neuroviro. 2003;9:551–8.
Katz DA, et al. Progressive multifocal leukoencephalopathy complicating Wiskott-Aldrich syndrome. Report of a case and review of the literature of progressive multifocal leukoencephalopathy with other inherited immunodeficiency states. Arch Neurol. 1994;51:422–6.
Andreoletti L, et al. Semiquantitative detection of JCV-DNA in peripheral blood leukocytes from HIV-1-infected patients with or without progressive multifocal leukoencephalopathy. J Med Virol. 2002;66:1–7.
Tornatore C, et al. Detection of JC viral genome in the lymphocytes of non-PML HIV positive patients: association with B cell lymphopenia. Neurology. 1992;42 Suppl 3:211.
Berenguer J, et al. Clinical course and prognostic factors of progressive multifocal leukoencephalopathy in patients treated with highly active antiretroviral therapy. Clin Infect Dis. 2003;36:1047–52.
Cinque P, et al. The good and evil of HAART in HIV-related progressive multifocal leukoencephalopathy. J Neuroviro. 2001;7:358–63.
Koralnik IJ, Du Pasquier RA, Letvin NL. JC virus-specific cytotoxic T lymphocytes in individuals with progressive multifocal leukoencephalopathy. J Virol. 2001;75:3483–7.
Krumbholz M, et al. Natalizumab disproportionately increases circulating pre-B and B cells in multiple sclerosis. Neurology. 2008;71:1350–4.
Du Pasquier RA, et al. JCV-specific cellular immune response correlates with a favorable clinical outcome in HIV-infected individuals with progressive multifocal leukoencephalopathy. J Neuroviro. 2001;7:318–22.
Du Pasquier RA, et al. A prospective study demonstrates an association between JC virus-specific cytotoxic T lymphocytes and the early control of progressive multifocal leukoencephalopathy. Brain. 2004;127:1970–8.
Marzocchetti A, et al. Efficient in vitro expansion of JC virus-specific CD8(+) T-cell responses by JCV peptide-stimulated dendritic cells from patients with progressive multifocal leukoencephalopathy. Virology. 2009;383:173–7.
del Pilar Martin M, et al. Decrease in the numbers of dendritic cells and CD4+ T cells in cerebral perivascular spaces due to natalizumab. Arch Neurol. 2008;65:1596–603.
Jullien D, et al. T-cell modulation for the treatment of chronic plaque psoriasis with efalizumab (Raptiva): mechanisms of action. Dermatology. 2004;208:297–306.
Papp KA. Efalizumab: advancing psoriasis management with a novel, targeted T-cell modulator. Drugs Today (Barc). 2004;40:889–99.
Capsoni F, et al. Effect of Efalizumab on neutrophil and monocyte functions in patients with psoriasis. Int J Immunopathol Pharmacol. 2008;21:437–45.
Lowes MA, et al. Increase in TNF-alpha and inducible nitric oxide synthase-expressing dendritic cells in psoriasis and reduction with efalizumab (anti-CD11a). Proc Natl Acad Sci U S A. 2005;102:19057–62.
• Schwab N, et al. Fatal PML associated with efalizumab therapy: insights into integrin alphaLbeta2 in JC virus control. Neurology. 2012;78:458–67. discussion 465. A recent observation on the possible pathogenesis of PML under monoclonal antibody therapy.
Cross AH, et al. Rituximab reduces B cells and T cells in cerebrospinal fluid of multiple sclerosis patients. J Neuroimmunol. 2006;180:63–70.
Marshall LJ, Major EO. Molecular regulation of JC virus tropism: insights into potential therapeutic targets for progressive multifocal leukoencephalopathy. J Neuroimmune Pharmacol. 2010;5:404–17.
Tornatore C, et al. Detection of JC virus DNA in peripheral lymphocytes from patients with and without progressive multifocal leukoencephalopathy. Ann Neurol. 1992;31:454–62.
Berger JR, et al. Are saliva and oropharyngeal secretions a source of JCV infection? J Neuroviro. 2005;11 Suppl 2:83.
White MK, Khalili K. Pathogenesis of progressive multifocal leukoencephalopathy–revisited. J Infect Dis. 2011;203:578–86.
Bayliss J, et al. Immunosuppression increases latent infection of brain by JC polyomavirus. Pathology. 2011;43:362–7.
Rushing EJ, et al. Immune reconstitution inflammatory syndrome of the brain: case illustrations of a challenging entity. J Neuropathol Exp Neurol. 2008;67:819–27.
Manabe YC, et al. Immune reconstitution inflammatory syndrome: risk factors and treatment implications. J Acquir Immune Defic Syndr. 2007;46:456–62.
Shelburne SA, et al. Incidence and risk factors for immune reconstitution inflammatory syndrome during highly active antiretroviral therapy. AIDS. 2005;19:399–406.
Price P, et al. Polymorphisms in cytokine genes define subpopulations of HIV-1 patients who experienced immune restoration diseases. AIDS. 2002;16:2043–7.
Falco V, et al. Influence of HAART on the clinical course of HIV-1-infected patients with progressive multifocal leukoencephalopathy: results of an observational multicenter study. J Acquir Immune Defic Syndr. 2008;49:26–31.
Clifford DB, et al. Natalizumab-associated progressive multifocal leukoencephalopathy in patients with multiple sclerosis: lessons from 28 cases. Lancet Neurol. 2010;9:438–46.
Miravalle A, Jensen R, Kinkel RP. Immune reconstitution inflammatory syndrome in patients with multiple sclerosis following cessation of natalizumab therapy. Arch Neurol. 2010;68:186–91.
• Johnson T, Nath A. Immune reconstitution inflammatory syndrome and the central nervous system. Curr Opin Neurol. 2011;24:284–90. A recent comprahensive review on IRIS.
Lawn SD, Meintjes G. Pathogenesis and prevention of immune reconstitution disease during antiretroviral therapy. Expert Rev Anti Infect Ther. 2011;9:415–30.
Tan CS, Koralnik IJ. Progressive multifocal leukoencephalopathy and other disorders caused by JC virus: clinical features and pathogenesis. Lancet Neurol. 2010;9:425–37.
Meintjes G, et al. Randomized placebo-controlled trial of prednisone for paradoxical tuberculosis-associated immune reconstitution inflammatory syndrome. AIDS. 2010;24:2381–90.
Hartung HP. et al [Therapie der Multiplen Sklerose mit monokonalen Antikorpen: aktualisierte Empfelungen im Rahmen eines Expert meetings]. Actuelle Neurol. 2011;38:2–11.
Berger JR. Steroids for PML-IRIS: a double-edged sword? Neurology. 2009;72:1454–5.
Berger JR. The clinical features of PML. Cleve Clin J Med. 2011;78 Suppl 2:S8–12.
Whiteman ML, et al. Progressive multifocal leukoencephalopathy in 47 HIV-seropositive patients: neuroimaging with clinical and pathologic correlation. Radiology. 1993;187:233–40.
Berger JR, et al. Progressive multifocal leukoencephalopathy in patients with HIV infection. J Neuroviro. 1998;4:59–68.
De Luca A, et al. Cidofovir in addition to antiretroviral treatment is not effective for AIDS-associated progressive multifocal leukoencephalopathy: a multicohort analysis. AIDS. 2008;22:1759–67.
Marra CM, et al. A pilot study of cidofovir for progressive multifocal leukoencephalopathy in AIDS. AIDS. 2002;16:1791–7.
De Luca A, et al. Clinical and virological monitoring during treatment with intrathecal cytarabine in patients with AIDS-associated progressive multifocal leukoencephalopathy. Clin Infect Dis. 1999;28:624–8.
Hall CD, et al. Failure of cytarabine in progressive multifocal leukoencephalopathy associated with human immunodeficiency virus infection. AIDS Clinical Trials Group 243 Team [see comments]. N Engl J Med. 1998;338:1345–51.
Elphick GF, et al. The human polyomavirus, JCV, uses serotonin receptors to infect cells. Science. 2004;306:1380–3.
Marzocchetti A, et al. Determinants of survival in progressive multifocal leukoencephalopathy. Neurology. 2009;73:1551–8.
Brickelmaier M, et al. Identification and characterization of mefloquine efficacy against Jc virus in vitro. Antimicrob Agents Chemother. 2009.
Beppu M, et al. Mefloquine improved progressive multifocal leukoencephalopathy in a patient with systemic lupus erythematosus. Intern Med. 2012;51(10):1245–7.
Moenster RP, Jett RA. Mirtazapine and mefloquine therapy for progressive multifocal leukoencephalopathy in a patient infected with human immunodeficiency virus. Am J Health Syst Pharm. 2012;69(6):496–8.
Disclosure
I. Steiner: none; J. R. Berger: consultant (Amgen, Bayer, Millenium, Genentech, and Novartis) and speakers’ bureaus (Novartis, Bayer, and Biogen Idec).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Steiner, I., Berger, J.R. Update on Progressive Multifocal Leukoencephalopathy. Curr Neurol Neurosci Rep 12, 680–686 (2012). https://doi.org/10.1007/s11910-012-0313-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-012-0313-4