Abstract
Purpose of review
A new syndrome responding to gluten-free diet and defined non-celiac gluten sensitivity entered the spectrum of gluten-related disorders, together with celiac disease and wheat allergy. However, its definition, prevalence, diagnosis, pathogenesis, treatment, and follow up are still controversial. The purpose of the review is to summarize the evidence and problems emerging from the current literature.
Recent findings
Direct implication of gluten in the onset of symptoms is often unproved as a low fermentable oligo-, di- and mono-saccharides and polyols diet or other components of cereals as wheat amylase trypsin inhibitor could be similarly involved. To date, no specific biomarkers or histological abnormalities confirm diagnosis, and only the self-reported response to gluten-free diet as well as a positive double blind placebo-gluten challenge characterizes these non-celiac, non-wheat allergic patients.
Summary
Critical revision of published studies can offer practical indications in approaching this clinical topic and useful suggestions to standardize scientific researches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although celiac disease (CD) was clinically known since 1888 [1], only in 1950s, a group of cereals (namely wheat, barley, and rye) was identified as responsible for the villous atrophy of the intestinal mucosa. Initially, starch was considered the toxic fraction, but later a mixture of proteins known as “gluten” was discovered and characterized the disease, arousing following researches about CD pathogenesis [2, 3].
Gluten induces, in genetically predisposed subjects carrying HLA-DQ2 and/or HLA DQ8 genotype, an immunological T-cell mediated reaction with production of autoantibodies and release of inflammatory cytokines inducing different levels of villous atrophy, increased intraepithelial lymphocytes, and altered intestinal permeability [4, 5]. These histological alterations, along with increased levels of high sensitive and specific anti-endomysial and anti-transglutaminase antibodies, confirm the diagnosis [6, 7]. At the moment, gluten-free diet (GFD) remains the unique therapy leading to progressive normalization of antibodies levels and intestinal mucosa, warranting good health and prognosis in the majority of cases. As the CD prevalence is 1–2 % in the general population and a long-life strict GFD is difficult to maintain, researches are in progress to offer alternative therapies [8].
GFD is the gold-standard also for 0.2–4 % of general population affected by wheat allergy (WA). The pathogenesis can be IgE mediated or non-IgE mediated [9, 10]. Different peptides of wheat and others than those involved in CD are implicated, but from the practical point of view, these patients should follow GFD, as strictly as celiac patients do [11]. In the classic form of WA, cross-linking between gluten peptides and IgE stimulates the release of histamine and other chemical mediators, triggering symptoms related to skin, respiratory, circulatory, or gastrointestinal systems. Diagnosis is based on clinical history, skin prick test, specific IgE dosage, and oral challenge. Again, GFD improves or eliminates symptoms. Non-IgE-mediated allergy, as other non-IgE-mediated food hypersensitivities often associated, has a wide range of systemic or gastrointestinal symptoms and can be diagnosed by a double-blind placebo-controlled challenge. There are no biochemical or serologic markers and intestinal mucosa shows architectural normality except for an increased number of eosinophils. Pathogenic mechanisms are not known, and clinical response to the GFD is essential to confirm diagnosis.
In recent years, in the spectrum of gluten-related disorders, a new syndrome at the moment defined by a group of experts “non-celiac gluten sensitivity” (NCGS) has gained interest and wide visibility on both scientific and non-scientific literature [12]. NCGS is characterized by gastrointestinal and extra-intestinal symptoms responding to gluten withdrawal, although no reliable biomarkers or histological abnormalities are available and discussion on definition, epidemiology, pathogenesis, diagnosis, and follow up inflames the scientific debates [13].
The purpose of this review is to critically examine published studies on NCGS focusing on open problems and doubts.
Brief History
Case reports on subjects complaining symptoms suggestive of CD and responding to GFD in the absence of serological or histological alterations have been published in the past [14, 15]: cases were sporadic and aroused little attention. On the contrary, in recent years, increasing numbers of subjects adopted a GFD to improve their gastrointestinal and/or extra-intestinal symptoms or simply to achieve better health and performances. Although in a large proportion of patients, a correct diagnostic process excluded CD and WA, GFD often is a personal choice based on a self-diagnosis. It is reported that in 2015 about 25 % of Americans adopted GFD and the market of gluten-free products reached 11.6 billion of dollars and continues to increase [12, 16]. It is quite unexpected that this phenomenon involved a country where in a recent past CD was even not considered a problem being underestimated for many years.
In any case, the hypothesis that dietary exclusion (in particular wheat) in non-celiac subjects with irritable bowel syndrome (IBS) was beneficial and was supported by some authors without a scientific demonstration that gluten itself was the causative factor [17–20]. Then, in 2011, an Australian group conducted a randomized, double-blind, placebo-controlled challenge study in IBS patients who had CD excluded and concluded with the existence of “non celiac gluten intolerance” [21]. This study has been criticized for the small number of participants, the limited statistical power, and for the choice of challenge (muffins and bread with and without carbohydrate-free gluten, 16 g/day) tested for blindness in only 10 subjects but it was considered important to confirm the involvement of wheat in determining symptoms in these patients. However, in 2013 through a placebo-controlled, cross-over challenge study, the same group concluded that there was no specific or dose-dependent effect of gluten in 37 subjects with NCGS following diets low in fermentable oligo-, di- and mono-saccharides and polyols (FODMAPs). In fact, in only 8 % of participants, gluten-specific effects were observed and food containing FODMAPs was considered the major responsible for symptoms as already suggested for some IBS patients [22•]. Similar results were obtained by other authors: Di Sabatino et al. [23••] performed a randomized, double-blind, placebo-controlled, cross-over trial with 4.375 g/day of gluten (capsules) in 59 suspected NCGS (without CD and WA) and identified only three subjects as “true gluten sensitive” according to the criteria adopted. A slightly higher percentage (14 %) was obtained by Elli et al. [24••] in a multicenter Italian randomized double-blind placebo-controlled trial (5.6 g/day gluten, capsules) in 98 subjects complaining functional symptoms. It is interesting to note that in both these studies, the response to the GFD was positive in a relevant percentage of cases while the blind administration of gluten elicited symptoms in only a minority of subjects responding to GFD. Therefore, it is possible that factors other than gluten were implicated in NCGS, as FODMAPs, antitrypsin amylase inhibitors (ATIs), or other proteins present in cereals.
As the true etiologic factor is not clearly identified, some panelists in the group of experts met in Munich in 2012 to evaluate the published information on this new syndrome, discussed the possibility to use, at this stage, the term “wheat sensitivity” or “people who avoid gluten” instead of NCGS [13]. Therefore, also the nomenclature of the syndrome is debatable and in some way confusing.
Strengths and Weaknesses about NCGS
-
(a)
Some non-celiac, non-allergic subjects claim symptoms responding to GFD.
Significant differences in design, setting, recruitment, and diagnostic criteria make difficult to compare the results in different studies [20, 21, 25, 26].
CD and WA are not always adequately excluded. Exclusion of CD is usually based on the presence of negative specific antibodies, non-compatible HLA status, and normal histology but some authors report in NCGS a mild increased number of intraepithelial lymphocytes in intestinal mucosa, presence of IgG anti-gliadin antibodies (IgG AGA) in serum, HLA status compatible with CD, C- associated antibodies in duodenal aspirate, or in supernatant of biopsy culture suggesting a potential CD [27–29].
WA is usually diagnosed by skin prick test and specific IgE assays (even if a low predictive value is reported). Open oral food challenge and double-blind placebo-controlled challenge are recommended for correct diagnosis of IgE- and non-IgE-mediated allergy.
The subjects involved in scientific studies are often self-reported NCGS diagnosis [30–32] or IBS patients [21, 22•, 24••] and less frequently suspected gluten sensitive patients [26, 33] making diagnostic work-up and evaluation rather confuse.
Objective assessment of the response is not simple and usually based on visual analogic scales (VAS) or numerical rating scale (NRS) [22•, 24••, 25, 34].
-
(b)
Suspected NCGS subjects complain gastrointestinal and/or extra-intestinal symptoms usually indistinguishable from CD and IBS patients.
According to an Italian prospective multicenter survey [26], as previously published in other studies [35], the main gastrointestinal symptoms are bloating (87 %), abdominal pain (83 %), diarrhea (>50 %), alternating bowel habits (27 %), constipation (24 %), and epigastric pain (52 %). Nausea, acid reflux, aerophagia, and aphthous stomatitis are less frequent.
Among extra-intestinal symptoms, tiredness (64 %) and lack of well-being (68 %) are common, followed by foggy mind (38 %), headache (54 %), muscle or joint pain (31 %), arm/leg numbness (32 %), anxiety (39 %), or depression (18 %). Finally, weight loss (25 %), dermatitis (18 %) or skin rash (29 %), and anemia (22 %) are also complained.
Symptoms are scarcely indicative of diagnosis, often more than two or three symptoms are present making evaluation of improvement difficult (How many symptoms have to be considered and which are the most important in establishing the effect of the diet? How much should be the symptomatic improvement in order to define a true response?).
Symptoms disappear after starting a GFD and recur after challenge within few hours or 1–2 days [12, 13, 21, 26].
Although quick response is usually elicited in WA, a delayed response (2 h–5 days after allergen exposure) is possible. Symptoms can appear at different times, and no international consensus on this topic has been reached (36); moreover, it is important to notice that non-IgE-mediated allergy shows strict similarities with NCGS and differential diagnosis results often difficult.
In respect to CD, a proportion of patients claim symptoms rapidly after ingestion of minimal doses of gluten or contaminations, while others remain asymptomatic also after a long-time exposure to high doses of gluten [36, 37]. Consequently, time of recurrence of symptoms is not a strong data supporting diagnosis of NCGS.
All studies report a prevalence of NCGS among adult females [12, 25, 26].
In contrast to CD, no major complications or comorbidities has been reported [13].
-
(c)
In NCGS, major biochemical tests are usually normal. Negative specific CD-related serum antibodies (IgA anti-endomysium, IgA anti-transglutaminase, and IgG anti-deaminated gliadin) and negative specific wheat IgE and skin prick test are necessary to afford diagnosis of NCGS.
Some studies report a variable prevalence (25–50 %) of IgG anti gliadin antibodies which are known to be not specific and present in different autoimmune disorders [13, 38].
Mild alterations in biochemical tests as low serum iron and ferritin, folate, vitamin B12, and vitamin D levels are present, although these all are not specific and usually related to other forms of malabsorption [26, 30, 31].
-
(d)
To date, no genetic pattern has been found to be specific of NCGS.
It is well-known that positive HLA-DQ2/DQ8 haplotypes are necessary, even if not sufficient, to develop CD and their absence excludes diagnosis of CD [6]. About 30–40 % of the general population is HLA-DQ2/DQ8 positive.
In NCGS, the reported prevalence of positive HLA-DQ2/DQ8 haplotypes varies from 24 to 100 % but not all studied subjects had CD correctly excluded and NCGS diagnosis confirmed; moreover, genetic test was often not fully described and related to histology [35]. Other haplotypes, not CD-related, should be investigated.
-
(e)
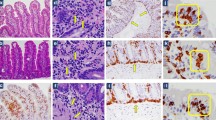
Histology of the intestinal mucosa does not show significant modifications. The absence of villous atrophy is specifically requested to diagnose NCGS.
Histology is not always reported in NCGS studies, and exclusion of CD has been frequently achieved through negative serology and/or genetic typing. In some studies, NCGS patients show increased duodenal intraepithelial lymphocytes (IELs) count (25 IELs/100 enterocytes), corresponding to Marsh I (Marsh Oberhuber) or grade A (Corazza Villanacci) lesions of CD histological classification [25, 26, 39]. Lymphocytic duodenitis is common and often but not exclusively associated with celiac disease [40].
Thus, a better understanding of the natural history of seronegative duodenitis or other diagnostic techniques as antiendomysium antibodies levels in culture medium of biopsies are necessary to exclude potential CD.
According to the review by Molina-Infante, it is clear that a consistent proportion of subjects considered affected by NCGS could be reclassified as celiacs [35].
-
(f)
In absence of serologic markers and histological abnormalities, double-blind placebo-controlled gluten challenge is the unique way to positively diagnose NCGS, and a standardized diagnostic protocol is mandatory to compare results of different studies. Searching for an agreement in 2014, some experts met in Salerno (Italy) and published their recommendations to achieve a correct diagnosis of NCGS [34].
However, the suggested diagnostic protocol (as shown in Fig. 1 ) is cumbersome and difficult to be introduced in the daily routine, being its application more suitable to a research setting than clinical practice. Dose of gluten, type, and vehicle for gluten administration, length of challenge and wash out, and assessment of the response are all parameters which need standardization yet.
Fig. 1 The diagnostic algorithm of NCGS proposed by Catassi et al. [34]. GFD gluten-free diet, A product A (gluten or placebo), B product B (placebo or gluten), E evaluation (questionnaire). The evaluation was performed weekly during step 1 and daily during step 2. Improvement evaluation: responders were defined as patients who fulfilled the response criteria (>30 % reduction of one to three main symptoms or at least 1 symptom with no worsening of others) for at least 50 % of the observation time. Adapted from Catassi et al., Nutrients. 2015
-
g)
True prevalence is not known, varying from 0.6 to 7 % according to different settings examined and design of the studies. The major bias concerns NCGS diagnosis and enrolled subjects.
In UK, a questionnaire was used to screen population for self-reported gluten sensitivity [30]. In 1002 adults, the prevalence of gluten sensitivity was 13 % with 3.7 % on GFD whereas the prevalence of diagnosed CD as 0.8 %. In a secondary care, 200 investigated gluten sensitive subjects had CD in 7 % of cases and NCGS in 93 %.
A cross-sectional population survey was conducted in Australia on adults selected at random from the Electoral Roll [41•]. Wheat avoidance was reported in 10.6 % of the 1184 selected subjects: 1.2 % had CD, 7.3 % presented symptoms responding to GFD whereas 2.1 % followed GFD for reasons other than health.
A survey was also conducted in parents of 916 New Zealand children with a median age of 10 years through a questionnaire specifically devoted to gluten-related issues [42]. Overall, 1 % of children were affected by CD whereas 5 % avoid gluten even if 67 % of them had not excluded CD.
A multicenter prospective study was carried out in 38 Italian centers for diagnosis of gluten-related disorders. In this setting, the prevalence of NCGS was only slightly more common than that of CD [26].
-
(h)
In NCGS patients, GFD resolves symptoms but a well-defined pathogenic pathway is still to be identified, differently from the other two gluten-related disorders (CD and WA) where autoimmune and allergic mechanisms have been demonstrated.
In 2011, Sapone et al. [43] studied the intestinal innate and adaptive immune response comparing CD and NCGS patients and showed some differences between the two disorders. Compared to CD and control patients, an increased expression of Toll-like receptor (TLR) 1, 2, and 4 was demonstrated, while the levels of adaptive immune response actors (IL-6, IL-21, and INF-gamma) did not differ significantly [25, 39]. It is important to underline that diagnosis of NCGS was based on negativity for CD and WA and positive response to GFD but not confirmed by a double-blind placebo-controlled challenge test and patients were examined after a 4-month gluten challenge. On the contrary, Brottveit et al. reported that after 3-day gluten challenge NCGS patients showed only an increase of IFN-γ levels and intraepithelial CD3+ T-cells at baseline whereas CD patients had a concomitant innate and adaptive immune response, suggesting that the adaptive immune response might play a role in the NCGS pathogenesis [44]. A recent study by Di Sabatino et al. investigated a complete pattern of innate and adaptive markers in CD and self-reported NCGS (negative for CD and WA and tested with double-blind placebo-controlled gluten challenge in 11/14 cases) supernatant of duodenal. The authors concluded that there was no difference in the immune response of intestinal mucosa of NCGS and treated CD patients and controls.
Studies on intestinal permeability are not conclusive: Sapone et al. showed a normal baseline intestinal permeability and tight junctions markers evaluated by the in vivo lactulose/mannitol test (LA/MA) in NCGS patients, whereas gliadin exposure induces increased intestinal permeability assessed by measuring transepithelial electrical resistance (TEER) of biopsy explants in a following study by Fasano et al. [45].
Finally, recent clinical and experimental studies enquired the potential pathogenic role of other wheat components besides gluten. As aforementioned, FODMAPs are now a well-defined trigger of symptoms in IBS patients and a proinflammatory effect of both FODMAPs, and other non-gluten proteins such as ATIs, wheat germ agglutinin (WGA), and exorphin, has been proved in [46]. Although “in vitro” and “in vivo” studies demonstrated that ATIs react as an adjuvant in innate response of monocytes, macrophages, and dendritic cells activation through TLR4 complex [47, 48•], it remains to be established the role of ATIs in NCGS pathogenesis. WGA, which has epithelial-damaging and immune effects at very low doses at least in vitro [49, 50], might also contribute to both intestinal and extraintestinal manifestations of NCGS but “in vivo” effects are still questioned.
The actual evidence on the possible pathogenesis of NCGS is conflicting chiefly because of the different design of published papers [51]. Hence, further comparable and standardized studies are necessary.
-
(i)
GFD, self-prescribed or suggested after exclusion of CD and WA, resolves intestinal and extraintestinal symptoms.
First of all, duration of treatment and strictness of the GFD are not established: how long has the GFD to be followed? A long-life strict GFD is requested as in CD or an “on demand” approach is possible? What are the effects off contaminations?
Thus, many questions remain unsolved mainly because our knowledge about the natural history of this condition is still scarce: currently, no data about long-term complications, a late onset of CD or a transient sensitivity, are available.
Personal Considerations and Future Prospectives
The main questions we need to study and solve are:
-
Is gluten the only cause of symptoms or other components of the diet are involved?
-
Which is the pathogenic mechanism underlying this condition?
-
Who are the subjects possibly more involved?
-
Is the condition irreversible or transient?
To obtain acceptable scientific responses:
-
Studies have to be comparable (similar criteria for enrollment of patients, diagnostic protocols, and evaluation of results)
-
For comparison, it is necessary to define subgroups of patients with uniform characteristics (CD patients with classic intestinal symptoms versus patients with extra-intestinal symptoms versus asymptomatic patients versus patients with other associated autoimmune diseases as well as subjects showing only a mild intestinal inflammation should not be gathered together with patients showing villous atrophy on histology).
-
WA exclusion should be better evaluated
-
The relationship with subjects affected by irritable bowel syndrome should be further considered
-
Advancements in knowledge of different cereals could be helpful, thus researches on protein structure and genetic typing are advisable.
Conclusion
In this chaotic scenario without strong evidence about gluten involvement and utility of GFD in patients with NCGS and in the absence of simpler diagnostic tools, it is recommended that subjects avoid self-diagnosis and self-treatment and that non-expert doctors refer suspected NCGS patients to tertiary referral center for proper management and follow-up.
In this respect, if it will be confirmed a causative effect of gluten in triggering symptoms as well as unhealthy consequences in up to 10 % of the general population (1 % CD, 0.2–4 % WA, and 5–7 % NCGS), then deep changes in dietary habits and a different agricultural and economic policy could become indispensable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gee SJ. On the coeliac affection. St Bartholomews Hospital Reports 1888. p. 17-20.
DICKE WK, WEIJERS HA, VAN DE KAMER JH. Coeliac disease. II. The presence in wheat of a factor having a deleterious effect in cases of coeliac disease. Acta Paediatr. 1953;42(1):34–42.
ANDERSON CM, FRENCH JM, SAMMONS HG, FRAZER AC, GERRARD JW, SMELLIE JM. Coeliac disease: gastrointestinal studies and the effect of dietary wheat flour. Lancet. 1952;1(6713):836–42.
Abadie V, Jabri B. IL-15: a central regulator of celiac disease immunopathology. Immunol Rev. 2014;260(1):221–34. doi:10.1111/imr.12191.
Rostom A, Murray JA, Kagnoff MF. American Gastroenterological Association (AGA) Institute technical review on the diagnosis and management of celiac disease. Gastroenterology. 2006;131(6):1981–2002. doi:10.1053/j.gastro.2006.10.004.
Rubio-Tapia A, Hill ID, Kelly CP, Calderwood AH, Murray JA. Gastroenterology ACo. ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol. 2013;108(5):656–76. doi:10.1038/ajg.2013.79. quiz 77.
Pallav K, Leffler DA, Tariq S, Kabbani T, Hansen J, Peer A, et al. Noncoeliac enteropathy: the differential diagnosis of villous atrophy in contemporary clinical practice. Aliment Pharmacol Ther. 2012;35(3):380–90. doi:10.1111/j.1365-2036.2011.04938.x.
Leffler D, Kupfer SS, Lebwohl B, Bugin K, Griebel D, Lathrop JT, et al. Development of celiac disease therapeutics: report of the third gastroenterology regulatory endpoints and advancement of therapeutics workshop. Gastroenterology. 2016. doi:10.1053/j.gastro.2016.07.025.
Keet CA, Matsui EC, Dhillon G, Lenehan P, Paterakis M, Wood RA. The natural history of wheat allergy. Ann Allergy Asthma Immunol. 2009;102(5):410–5. doi:10.1016/S1081-1206(10)60513-3.
Cianferoni A. Wheat allergy: diagnosis and management. J Asthma Allergy. 2016;9:13–25. doi:10.2147/JAA.S81550.
Pastorello EA, Farioli L, Conti A, Pravettoni V, Bonomi S, Iametti S, et al. Wheat IgE-mediated food allergy in European patients: alpha-amylase inhibitors, lipid transfer proteins and low-molecular-weight glutenins. Allergenic molecules recognized by double-blind, placebo-controlled food challenge. Int Arch Allergy Immunol. 2007;144(1):10–22. doi:10.1159/000102609.
Sapone A, Bai JC, Ciacci C, Dolinsek J, Green PH, Hadjivassiliou M, et al. Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Med. 2012;10:13.
Catassi C, Bai JC, Bonaz B, Bouma G, Calabro A, Carroccio A, et al. Non-Celiac Gluten sensitivity: the new frontier of gluten related disorders. Nutrients. 2013;5(10):3839–53.
Ellis A, Linaker BD. Non-coeliac gluten sensitivity? Lancet. 1978;1(8078):1358–9.
Cooper BT, Holmes GK, Ferguson R, Thompson RA, Allan RN, Cooke WT. Gluten-sensitive diarrhea without evidence of celiac disease. Gastroenterology. 1980;79(5 Pt 1):801–6.
Reilly NR. The gluten-free diet: recognizing fact, fiction, and fad. J Pediatr. 2016;175:206–10. doi:10.1016/j.jpeds.2016.04.014.
Wahnschaffe U, Stockmann M, Daum S, Ullrich R, Riecken EO, Schulzke JD. Intestinal antibodies against gliadin, tissue-transglutaminase, beta-lactoglobulin, and ovalbumin in patients with irritable bowel syndrome. Ann N Y Acad Sci. 1998;859:280–4.
Wahnschaffe U, Schulzke JD, Zeitz M, Ullrich R. Predictors of clinical response to gluten-free diet in patients diagnosed with diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol. 2007;5(7):844–50. doi:10.1016/j.cgh.2007.03.021. quiz 769.
Fan X, Sellin JH. Review article: small intestinal bacterial overgrowth, bile acid malabsorption and gluten intolerance as possible causes of chronic watery diarrhoea. Aliment Pharmacol Ther. 2009;29(10):1069–77. doi:10.1111/j.1365-2036.2009.03970.x.
Verdu EF, Armstrong D, Murray JA. Between celiac disease and irritable bowel syndrome: the "no man’s land" of gluten sensitivity. Am J Gastroenterol. 2009;104(6):1587–94. doi:10.1038/ajg.2009.188.
Biesiekierski JR, Newnham ED, Irving PM, Barrett JS, Haines M, Doecke JD, et al. Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am J Gastroenterol. 2011;106(3):508–14. doi:10.1038/ajg.2010.487. quiz 15.
Biesiekierski JR, Peters SL, Newnham ED, Rosella O, Muir JG, Gibson PR. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology. 2013;145(2):320-8 e1-3. A DBPC challenge trial showing that patients with self-reported NCGS improved on a low-FODMAP diet with no specific gluten-related effects.
Di Sabatino A, Volta U, Salvatore C, Biancheri P, Caio G, De Giorgio R, et al. Small amounts of gluten in subjects with suspected nonceliac gluten sensitivity: a randomized, double-blind, placebo-controlled, cross-over trial. Clin Gastroenterol Hepatol. 2015. doi:10.1016/j.cgh.2015.01.029. A recent DBPC trial showing the effects of purified wheat gluten on patients with self-reported NCGS.
Elli L, Tomba C, Branchi F, Roncoroni L, Lombardo V, Bardella MT, et al. Evidence for the presence of Non-celiac gluten sensitivity in patients with functional gastrointestinal symptoms: results from a multicenter randomized double-blind placebo-controlled gluten challenge. Nutrients. 2016;8(2):84. doi:10.3390/nu8020084. A recent multicentric DBPC trial showing that around 15% patients with funtional gastorintestinal symptoms might have NCGS.
Carroccio A, Mansueto P, Iacono G, Soresi M, D’Alcamo A, Cavataio F, et al. Non-celiac wheat sensitivity diagnosed by double-blind placebo-controlled challenge: exploring a new clinical entity. Am J Gastroenterol. 2012;107(12):1898–906. doi:10.1038/ajg.2012.236. quiz 907.
Volta U, Bardella MT, Calabro A, Troncone R, Corazza GR. An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med. 2014;12:85.
Carroccio A, Mansueto P, D’Alcamo A, Iacono G. Non-celiac wheat sensitivity as an allergic condition: personal experience and narrative review. Am J Gastroenterol. 2013;108(12):1845–52. doi:10.1038/ajg.2013.353. quiz 53.
Molina-Infante J, Santolaria S, Montoro M, Esteve M, Fernández-Bañares F. Non-celiac gluten sensitivity: a critical review of current evidence. Gastroenterol Hepatol. 2014;37(6):362–71. doi:10.1016/j.gastrohep.2014.01.005.
Biesiekierski JR, Newnham ED, Shepherd SJ, Muir JG, Gibson PR. Characterization of adults with a self-diagnosis of nonceliac gluten sensitivity. Nutr Clin Pract. 2014;29(4):504–9. doi:10.1177/0884533614529163.
Aziz I, Lewis NR, Hadjivassiliou M, Winfield SN, Rugg N, Kelsall A, et al. A UK study assessing the population prevalence of self-reported gluten sensitivity and referral characteristics to secondary care. Eur J Gastroenterol Hepatol. 2014;26(1):33–9. doi:10.1097/01.meg.0000435546.87251.f7.
Kabbani TA, Vanga RR, Leffler DA, Villafuerte-Galvez J, Pallav K, Hansen J, et al. Celiac disease or non-celiac gluten sensitivity? An approach to clinical differential diagnosis. Am J Gastroenterol. 2014;109(5):741–6. doi:10.1038/ajg.2014.41. quiz 7.
Coburn JA, Vande Voort JL, Lahr BD, Van Dyke CT, Kroning CM, Wu TT, et al. Human leukocyte antigen genetics and clinical features of self-treated patients on a gluten-free diet. J Clin Gastroenterol. 2013;47(10):828–33. doi:10.1097/MCG.0b013e31828f531c.
Di Sabatino A, Corazza GR. Nonceliac gluten sensitivity: sense or sensibility? Ann Intern Med. 2012;156(4):309–11.
Catassi C, Elli L, Bonaz B, Bouma G, Carroccio A, Castillejo G, et al. Diagnosis of non-celiac gluten sensitivity (NCGS): the Salerno experts’ criteria. Nutrients. 2015;7(6):4966–77. doi:10.3390/nu7064966.
Molina-Infante J, Santolaria S, Sanders DS, Fernández-Bañares F. Systematic review: noncoeliac gluten sensitivity. Aliment Pharmacol Ther. 2015;41(9):807–20. doi:10.1111/apt.13155.
Bardella MT, Fredella C, Trovato C, Ermacora E, Cavalli R, Saladino V, et al. Long-term remission in patients with dermatitis herpetiformis on a normal diet. Br J Dermatol. 2003;149(5):968–71.
Bruins MJ. The clinical response to gluten challenge: a review of the literature. Nutrients. 2013;5(11):4614–41. doi:10.3390/nu5114614.
Volta U, Tovoli F, Cicola R, Parisi C, Fabbri A, Piscaglia M, et al. Serological tests in gluten sensitivity (nonceliac gluten intolerance). J Clin Gastroenterol. 2012;46(8):680–5. doi:10.1097/MCG.0b013e3182372541.
Sapone A, Lammers KM, Mazzarella G, Mikhailenko I, Cartenì M, Casolaro V, et al. Differential mucosal IL-17 expression in two gliadin-induced disorders: gluten sensitivity and the autoimmune enteropathy celiac disease. Int Arch Allergy Immunol. 2010;152(1):75–80. doi:10.1159/000260087.
Walker MM, Murray JA, Ronkainen J, Aro P, Storskrubb T, D’Amato M, et al. Detection of celiac disease and lymphocytic enteropathy by parallel serology and histopathology in a population-based study. Gastroenterology. 2010;139(1):112–9. doi:10.1053/j.gastro.2010.04.007.
Golley S, Corsini N, Topping D, Morell M, Mohr P. Motivations for avoiding wheat consumption in Australia: results from a population survey. Public Health Nutr. 2015;18(3):490–9. doi:10.1017/S1368980014000652. This study investigates the prevalence of gluten avoidance in the general population and the reasons for this dietary choice beyond celiac disease.
Tanpowpong P, Ingham TR, Lampshire PK, Kirchberg FF, Epton MJ, Crane J, et al. Coeliac disease and gluten avoidance in New Zealand children. Arch Dis Child. 2012;97(1):12–6. doi:10.1136/archdischild-2011-300248.
Sapone A, Lammers KM, Casolaro V, Cammarota M, Giuliano MT, De Rosa M, et al. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity. BMC Med. 2011;9:23. doi:10.1186/1741-7015-9-23.
Brottveit M, Beitnes AC, Tollefsen S, Bratlie JE, Jahnsen FL, Johansen FE, et al. Mucosal cytokine response after short-term gluten challenge in celiac disease and non-celiac gluten sensitivity. Am J Gastroenterol. 2013;108(5):842–50. doi:10.1038/ajg.2013.91.
Hollon J, Puppa EL, Greenwald B, Goldberg E, Guerrerio A, Fasano A. Effect of gliadin on permeability of intestinal biopsy explants from celiac disease patients and patients with non-celiac gluten sensitivity. Nutrients. 2015;7(3):1565–76. doi:10.3390/nu7031565.
Gibson PR, Shepherd SJ. Food choice as a key management strategy for functional gastrointestinal symptoms. Am J Gastroenterol. 2012;107(5):657–66. doi:10.1038/ajg.2012.49. quiz 67.
Junker Y, Zeissig S, Kim SJ, Barisani D, Wieser H, Leffler DA, et al. Wheat amylase trypsin inhibitors drive intestinal inflammation via activation of toll-like receptor 4. J Exp Med. 2012;209(13):2395–408. doi:10.1084/jem.20102660.
Schuppan D, Zevallos V. Wheat amylase trypsin inhibitors as nutritional activators of innate immunity. Dig Dis. 2015;33(2):260–3. doi:10.1159/000371476. The study demonstrates the promoting effects of ATIs on innate immune cells through suggesting a primary role in severe forms of wheat sensitivity.
Haas H, Falcone FH, Schramm G, Haisch K, Gibbs BF, Klaucke J, et al. Dietary lectins can induce in vitro release of IL-4 and IL-13 from human basophils. Eur J Immunol. 1999;29(3):918–27. doi:10.1002/(SICI)1521-4141(199903)29:03<918::AID-IMMU918>3.0.CO;2-T.
Dalla Pellegrina C, Perbellini O, Scupoli MT, Tomelleri C, Zanetti C, Zoccatelli G, et al. Effects of wheat germ agglutinin on human gastrointestinal epithelium: insights from an experimental model of immune/epithelial cell interaction. Toxicol Appl Pharmacol. 2009;237(2):146–53. doi:10.1016/j.taap.2009.03.012.
Czaja-Bulsa G. Non coeliac gluten sensitivity—a new disease with gluten intolerance. Clin Nutr. 2015;34(2):189–94. doi:10.1016/j.clnu.2014.08.012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs Bardella and Ferretti have no conflict of interest to declare.
Dr. Elli reports personal fees from Schär Institute, outside the submitted work
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical Collection on Small Intestine
Rights and permissions
About this article
Cite this article
Bardella, M.T., Elli, L. & Ferretti, F. Non Celiac Gluten Sensitivity. Curr Gastroenterol Rep 18, 63 (2016). https://doi.org/10.1007/s11894-016-0536-7
Published:
DOI: https://doi.org/10.1007/s11894-016-0536-7