Abstract
Purpose of Review
This review seeks to address knowledge gaps around the economic burden of diabetes in Africa. Africa is home to numerous endemic infections and also prevalent non-communicable diseases including diabetes. It is projected that the greatest increases in diabetes prevalence will occur in Africa. The importance of this review therefore lies in providing adequate knowledge on the economic challenges that diabetes poses to the continent and describe the way forward in tackling this epidemic.
Recent Findings
Diabetes contributes to a huge amount of the global health expenditure in the world. There is a dearth of information on the economic burden of diabetes in Africa with very limited number of studies in the area. Predictions do show that Africa has the greatest predicted increase in both the burden of diabetes and associated diabetic complications but yet contributes the lowest in the global annual healthcare expenses with regard to diabetes care. In 2017, the International Diabetes Federation (IDF) estimated the total health expenditure due to diabetes at $3.3 billion. In Nigeria, the national annual direct costs of diabetes was estimated in the range of $1.071 billion to $1.639 billion per year while the estimated monthly direct medical costs per individual in Cameroon stands at $148. In Sudan, the direct cost of type 2 diabetes control was $175 per year which only included the cost of medications and ambulatory care. People with diabetes are likely to experience one or more chronic illness and a significant portion of the costs associated with these complications are attributed to the underlying diabetes.
Summary
The growing epidemics of diabetes and associated diabetic complications worldwide poses catastrophic financial costs, especially in Africa where most of the expenses are paid by patients and families. The most common method used for the estimation of the economic burden of a public health problem like diabetes is the cost-of-illness approach. Cost-of-illness studies traditionally divide costs into three categories: direct, indirect, and intangible. The IDF estimated the total health expenditure due to diabetes at $3.3 billion worldwide in 2017. Most of the existing studies in Africa estimated only the direct costs. The medical direct cost of type 1 diabetes was higher than type 2. However, the estimations of costs of diabetes in many countries in Africa may be underestimated due to absence of data on the relative contribution of cost of diabetes complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is compounding evidence that the prevalence of diabetes has reached epidemic proportion in most parts of the globe including Africa [1]. Rapid demographic growth, nutritional and socioeconomic transitions are pointedly suggested to be responsible for the rising surge of diabetes in Africa [2•]. Diabetes has three main types: type 1 diabetes, type 2 diabetes, and gestational diabetes. Type 2 diabetes represents by far the most prevalent form of the affection (70–90%) [3•]. The growing epidemics of diabetes and associated diabetic complications worldwide poses a catastrophic financial cost, especially in Africa where most of the expenses are paid by patients and families [4, 5].
The mechanisms for diabetes healthcare finances in the continent range from direct to intangible costs with no clear-specific country data. Africa as a continent houses both rapidly growing and stagnant economies but their relative contribution to diabetes healthcare expenditure is sparsely known. This review therefore seeks to address the underlying mechanisms and knowledge gaps about the economic burden of diabetes in Africa.
The Epidemiological Burden of Diabetes
Type 1 diabetes which mainly affects children and adolescents is increasing every year. It is estimated that the incidence of type 1 diabetes is growing exponentially especially in children below 15 years of age with the overall yearly increment estimated to around 3% varying with regard to the different geographical regions of the world [6, 7]. A total of about 1 million children and adolescents aged below 20 years are estimated to have type 1 diabetes worldwide with Europe, North America, and the Caribbean having the largest proportions of these [3•]. Africa however is not exempt from the rising type 1 diabetes phenomenon. The African region currently has an estimated 50,600 children and adolescents below 20 years affected with type 1 diabetes [3•]. Further compounding the problem is that in many countries in Africa there is limited access to insulin and inadequate health service provision; thus, children and adolescents with type 1 diabetes suffer from high rates of diabetes-related complications and early mortality [8].
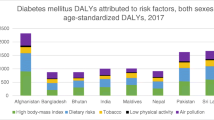
Type 2 diabetes has equally seen a global increase in prevalence of epidemic proportions over the past decades [2•]. According to the International Diabetes Federation (IDF) estimates, type 2 diabetes has known a tremendous rise in numbers over the past 20 years from a global prevalence of 151 million adults (20–79 years) in 2000 to a staggering 425 million adults in 2017 [3•, 9]. If nothing is done, this number is expected to rise to an estimated 625 million adults by the year 2045 with the largest proportions being in low and middle income countries including many countries in Africa [3•] (see Fig. 1). About 15.5 million adults live with type 2 diabetes in Africa with the highest proportions in persons aged between 55 and 64 years. In Africa, a large number (69.2%) of people have undiagnosed diabetes and more than half (55.3%) of people with diabetes live in an urban setting, even though the overall population in the region is grossly (60.3%) rural. As urbanization increases and populations age, type 2 diabetes will pose an ever-growing threat. It is expected that by 2045 there will be 40.7 million adults aged 20–79 years in this region living with diabetes, more than double the number in 2017.
Global prevalence of diabetes. (Adapted with permission from: International Diabetes Federation. IDF Diabetes Atlas, 8th edn. Brussels, Belgium: International Diabetes Federation, 2017. http://www.diabetesatlas.org) [3•]
Hyperglycemia in pregnancy also poses a threat in many parts of the world with regard to the life-threatening complications for the mother and offspring. Africa has the lowest raw prevalence of about 9.5% [3•] compared to 26.6% in the South-East Asia region which represents the highest prevalence in the world.
In 2017, according to IDF estimates, more than 298,160 deaths (6% of all mortality) in Africa were attributed to diabetes with the highest percentage of all-cause mortality due to diabetes in age group 30–39. Furthermore, 77.0% of all deaths attributable to diabetes occurred in people under 60 years, the highest proportion in the world. This data highlights how investment, research, and health systems are too slow to respond to the diabetes burden in Africa and remain focused primarily on infectious disease [3•].
Table 1 shows data on diabetes prevalence and mortality and health expenditure in some sub-Saharan African countries. The prevalence of diabetes in 2017 varied from 1% in Benin to 10.4% in South Soudan and deaths due to diabetes from 536.5 in Equatorial Guinea to 42,621.4 in South Africa [3•].
Generally, people with diabetes have an increased risk of developing a number of serious life-threatening health problems and complications thus increasing medical care costs and lowering quality of life. These complications span from cardiovascular diseases, diabetic eye disease, diabetic nephropathy, diabetic polyneuropathy which may be present in people with type 2 diabetes at the moment of diagnosis and early (around 5 years) after onset of type 1 diabetes. These complications compound the burden of diabetes but are also responsible for significant healthcare expenditure [12].
The Economic Impact of Diabetes in Africa
The most common method used for the estimation of the economic burden of a public health problem like diabetes is the cost-of-illness approach. Cost-of-illness studies are descriptive studies that value in dollar terms the costs of a particular health problem, which allows the economic burden of the problem to be estimated [13,14,15]. Cost-of-illness studies traditionally divide costs into three categories: direct, indirect, and intangible. Diabetes and its complications are responsible for a substantial societal financial burden. Diabetes care incur substantial costs to patients, families, and society, not only for direct costs of medical care for diabetes but also for indirect costs and intangible costs [16, 17].
Direct cost may be classified into two: direct medical cost and direct non-medical cost on one hand, or household expenses (which includes out pocket expenses borne by the patient and their families) and cost of organizing and operating hospital services on the other hand. The indirect costs usually refer to the resources lost as a result of illness, and they represent the opportunity cost of time lost as a result of workdays missed due to ill health (absenteeism), reduced productivity while at work due to ill health (presentism), reduced workforce participation due to disability, and productivity losses due to premature retirement and mortality [18]. Intangible costs are costs associated with changes in the quality of life of individuals and relatives as a result of the illness (cost of pain, grief, and suffering on individuals and their families). The calculation of diabetes costs can be done following different epidemiological approaches, study perspectives, sources of data, and resources quantification [19]. Limited information is currently available on the cost associated with diabetes in Africa. In addition, the few existing studies used divergent approaches.
Costs of Diabetes
Few studies have investigated diabetes health expenditure in Africa. In 2017, the IDF Diabetes Atlas estimated that 3.3 billion was spent on health care by people with diabetes; less than 1% of the total amount spent worldwide [3•]. Table 2 presents costs associated with diabetes in some African countries. Although Africa has the greatest predicted increase in both the burden of diabetes and associated diabetic complications, it contributes the lowest in the global annual healthcare expenses with regard to diabetes care.
In 2009, Kirigia et al., for the estimation of diabetes cost in Africa, classified the 46 member states in the WHO African Region into three groups (Region 1: Botswana, Equatorial Guinea, Gabon, Mauritius, Seychelles, South Africa; Region 2: Algeria, Angola, Cape Verde, Congo, Namibia, Swaziland; and the Region 3: Benin, Burkina Faso, Burundi, Cameroon, Central African Republic, Chad, Comoros, Democratic Republic of Congo, Cote d’Ivoire, Eritrea, Ethiopia, Gambia, Ghana, Guinea, Guinea-Bissau, Kenya, Lesotho, Liberia, Madagascar, Malawi, Mali, Mauritania, Mozambique, Niger, Nigeria, Rwanda, Sao Tome and Principe, Senegal, Sierra Leone, Tanzania, Togo, Uganda, Zambia, Zimbabwe) using gross national income (GNI) per capita expressed in purchasing power parity for 2005 (Region 1 with GNI per capita of > Int$8000; Region 2 with GNI between Int$2000 and Int$8000, and Region 3 with GNI < Int$2000). Considering the 7.02 million cases of diabetes recorded by countries of the WHO African Region in 2000, they estimated a total economic loss of Int$25.51 billion, or Int$11,431.6, $4770.6, and or Int$2144.3 per patient with diabetes per year for Region 1, Region 2, and Region 3, respectively. The grand total indirect cost was about Int$8.1 billion (32%) in the Region. The direct cost incurred in treating diabetes was Int$853.2 million in group 1, Int$523.3 million in group 2, and Int$6.7 billion in group 3 [22•]. We found two studies done in countries which quantified both direct and indirect cost of diabetes [20, 21]. In Mali (2009), the total annual cost per patient was estimated at $1127.7 with an average direct cost of $365.48 and an indirect cost of $762.20 [21]. In Morocco (2013), the total direct cost was estimated in a range of $0.47 billion and $1.5 billion and the average per capita direct cost of diabetes between $259 and $830. The indirect cost was estimated to be around $2 billion and the average per capita indirect cost to be $1113 [20].
Most of the studies investigated only direct cost of diabetes. In Nigeria, the national annual direct costs of diabetes was estimated in the range of $1.071 billion to $1.639 billion per year [23, 26, 28]. Alouki et al. (2015) estimated that medical costs per individual per year for uncomplicated diabetes in the four countries ranged from $126 to 1093 in Guinea, $137 to 869 in Mali, $212 to 828 in Benin, and $224 to 859 in Burkina Faso [24]. In Nigeria, the monthly direct medical cost of type 2 diabetes varied from $262.22 to $400.52 [23, 28, 33, 34], and was estimated at $148 in Cameroon (2009–2011) [27]. In Ghana (2010), the mean direct cost per diabetic patient per year (type 1 and type 2 diabetes) was estimated at $422.98 and the financial cost of medical services and medical supplies [29]. In Sudan (2005), the direct cost of type 2 diabetes control was $175 per year and this cost included only cost of drugs and ambulatory care [30]. Other studies only evaluated cost in people with type 1 diabetes. In a study done in Tanzania (1992), the mean annual direct cost was $287 (in a clinic of adults and some children), with the insulin component of $156 [32]. In Sudan (1995), the median annual direct cost in children with type 1 diabetes was $283 with insulin accounting for 36% of this amount [31]. Ogle et al. (2013–2015) calculated the annual cost of direct supplies expensed by families of children with type 1 diabetes, in some lower income countries in Africa (Benin, Burkina Faso, Central African Republic, Ivory Coast, Malawi, Mauritania, and Somalia) using cost data collected from IDF Life for a Child program centers; this annual cost ranged from $357 (Somalia) to $1185 (Burkina Faso) [25]. In general, the medical direct cost of type 1 diabetes was higher than type 2 diabetes [23, 26, 29]. Also, medical care in the public sector was less costly when compared to the private sector [24, 30].
Costs of Diabetes Complications
People with diabetes are likely to experience one or more chronic illness and a significant portion of the costs associated with these complications are attributed to the underlying diabetes [3•]. In this review, we found four studies which estimated the costs of diabetic complications. In Nigeria, the estimation of the successfully treatment of patients with diabetes foot ulcers (DFU) ranged from $488 to $1808 according to DFU stage [35, 36]. In Tanzania (2012), this cost of DFU ranged from Int$102 for uncomplicated DFU to Int$3060 for complicated DFU [37]. Alouki et al. (2009–2014) found that the cost of treatment of diabetes with retinopathy (the complication which entails the lowest incremental cost) ranged from $176 to 1002 in Mali, $320–987 in Benin, $305–983 in Burkina Faso, and $187–1243 in Guinea. The treatment for diabetes with nephropathy (complication with the highest additional cost) ranged from $490 to 4068 in Mali, $850–3197 in Benin, $782–3411 in Burkina Faso, and $808–4256 in Guinea [24]. In Nigeria (2012) where about 80% of patients with type 2 diabetes also have high blood pressure, an annual national cost implication in these patients would be in the range of $1.7 billion, an increment in 4.5% therapy cost relative to type 2 diabetes alone [26].
According to IDF estimates in 2017, diabetes expenses in Africa (AFR) was lowest from all seven IDF regions, representing less than 1% (Int$6.7 billion) of the total spent worldwide, despite the fact that 3% of person with diabetes live in the AFR regions [3•]. The mean diabetes-related expenditure per person (20–79) ranged from Int$46 in Central African Republic to Int$2087 in Equatorial Guinea [3•]. This situation is alarming considering the fact that an important part of these expenses was out of pocket expenditures incurred by patients [38]. In general, health investment in AFR countries is insufficient and underestimated by governments [39]. As presented in Table 1, the gross domestic product per capita varied from $661 in Central African Republic to $29,341.5 in Equatorial Guinea, with the capital health expenditure ranging from Int$0.0049 in Malawi to Int$559.59 in Equatorial Guinea [10, 11]. Moreover, diabetes expenditure per patient was high compared to allocated per capita health expenditure in many African countries. In most of sub-Saharan countries where there are no specific health resources allocated to the management of diabetes and its complications, this situation can be seen as a result of the inadequate provision of diabetes health services, and the relative poverty of these countries constrains their attempts to improve health care indicators [39].
Knowledge Gaps and Perspective for Change
As noted in Mbanya et al. in 2003 [39], it is clear that national estimates on the economic impact of diabetes in African countries are lacking. We found some studies which provide a fragmented picture of the situation in Africa; however, there are several knowledge gaps.
In most of the countries, no study was done at the national level. The studies were done at the level of the hospital and enrolled a limited number of patients. Most of these estimates were done in type 2 diabetes or in diabetes in general. Little information is available on costs specific to type 1 diabetes, type 2 diabetes, or gestational diabetes. Most of the studies aimed to estimate the direct medical cost of diabetes paid by the patients and did not take into account government and societal perspectives. In addition, few studies have been conducted to estimate the indirect costs of diabetes that are much higher than indirect costs. Another issue is that the estimation made on diabetes cost did not take into account undiagnosed diabetes and diabetes complications and therefore, the aggregate costs associated with diabetes have been severely under estimated. Furthermore, there are wide differences observed across countries in estimated diabetes direct and indirect costs and, due to this, the usefulness of the results presented in cost of illness studies often raises serious questions [40, 41]. It is well known that cost of illness estimates can be used to support policy and budgetary decisions [14, 19] and therefore there is a need for well-targeted studies on the economic burden of diabetes in Africa.
Conclusion
Diabetes imposes a considerable economic burden on patients and societies, and given that the prevalence of diabetes is expected to increase, the economic burden on individuals will also continue to rise. With limited resources and where every decision should be evidence-based, an estimation of the costs associated with diabetes in Africa gives an insight into the benefits of disease prevention and can facilitate the design and adoption of cost effective treatment options.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Atun R, Gale EAM. The challenge of diabetes in sub-Saharan Africa. Lancet Diabetes Endocrinol. 2015;3:675–7.
• Atun R, Davies JI, Gale EAM, Bärnighausen T, Beran D, Kengne AP, et al. Diabetes in sub-Saharan Africa: from clinical care to health policy. Lancet Diabetes Endocrinol. 2017;5:622–67 This article provides an up-to-date situational analysis with regards to the diabetes challenges and perspectives for transforming the diabetes landscape in the continent. It further identifies current gaps in economic policies which may serve as landmarks for action.
• IDF. IDF Diabetes Atlas, 8th edition. Brussels, Belgium: International Diabetes Federation; 2017. The IDF Diabetes Atlas provides a gross estimate of total health expenditure worldwide. It stands as a useful reference point for global estimates since the data is pooled from the numerous participating countries in the federation.
Nikolic IA, Stanciole AE, Zaydman M. Chronic emergency: why NCDS matter—Health Nutrition and Population (HPN) discussion paper [Internet]. 2011 [cited 2018 Sep 7]. Available from: http://siteresources.worldbank.org/HEALTHNUTRITIONANDPOPULATION/Resources/281627-1095698140167/ChronicEmergencyWhyNCDsMatter.pdf.Accessed 7 Sept 2018.
Smith-Spangler C, Bhattacharya J, Goldhaber-Fiebert J. Diabetes, its treatment, and catastrophic medical spending in 35 developing countries. Diabetes Care. 2012;35:319–26.
Stipančić G, La Grasta Sabolić L, Požgaj Šepec M, Radica A, Skrabić V, Severinski S, et al. Regional differences in incidence and clinical presentation of type 1 diabetes in children aged under 15 years in Croatia. Croat Med J. 2012;53:141–8.
Patterson CC, Dahlquist GG, Gyürüs E, Green A, Soltész G, EURODIAB Study Group. Incidence trends for childhood type 1 diabetes in Europe during 1989-2003 and predicted new cases 2005-20: a multicentre prospective registration study. Lancet Lond Engl. 2009;373:2027–33.
Bahendeka SK. Diabetes in sub-Saharan Africa: let us not forget type 1. Lancet Diabetes Endocrinol. 2017;5:575–7.
IDF. IDF Diabetes Atlas, 1st edition [Internet]. Brussels, Belgium: International Diabetes Federation; 2000 [cited 2015 Jan 6]. Available from: www.idf.org/diabetesatlas. Accessed 6 Sept 2018.
The World Bank. Data indicators [Internet]. 2017 [cited 2018 Oct 1]. Available from: https://data.worldbank.org/indicator/NY.GDP.PCAP.PP.CD?view=chart
World Health Organization. Global health expenditure database [Internet]. 2015. Available from: http://apps.who.int/nha/database/ViewData/Indicators/en
Chawla A, Chawla R, Jaggi S. Microvasular and macrovascular complications in diabetes mellitus: distinct or continuum? Indian J Endocrinol Metab. 2016;20:546–51.
Hodgson TA, Meiners MR. Cost-of-illness methodology: a guide to current practices and procedures. Milbank Mem Fund Q Health Soc. 1982;60:429–62.
Jo C. Cost-of-illness studies: concepts, scopes, and methods. Clin Mol Hepatol. 2014;20:327–37.
Byford S, Torgerson DJ, Raftery J. Cost of illness studies. BMJ. 2000;320:1335.
WHO. Global status report on noncommunicable diseases, vol. 2010. Geneva: World Health Organization; 2010.
WHO. Global status report on noncommunicable diseases, vol. 2014. Geneva: World Health Organisation; 2014.
Kengne AP, June-Rose McHiza Z, Amoah AGB, Mbanya J-C. Cardiovascular diseases and diabetes as economic and developmental challenges in Africa. Prog Cardiovasc Dis. 2013;56:302–13.
Songer TJ, Ettaro L. The economics of diabetes project panel. Studies on the cost of diabetes [Internet]. Centers for Disease Control and Prevention; 1998 [cited 2016 Dec 11]. Available from: http://www.pitt.edu/~tjs/coi/Costofillness.PDF. Accessed 7 Sept 2018.
Boutayeb W, Lamlili MEN, Boutayeb A, Boutayeb S. Estimation of direct and indirect cost of diabetes in Morocco. J Biomed Sci Eng. 2013;6:732–8.
Bermudez-Tamayo C, Besançon S, Johri M, Assa S, Brown JB, Ramaiya K. Direct and indirect costs of diabetes mellitus in Mali: a case-control study. PLoS One. 2017;12:e0176128.
•• Kirigia JM, Sambo HB, Sambo LG, Barry SP. Economic burden of diabetes mellitus in the WHO African region. BMC Int Health Hum Rights. 2009;9(6) This article presents a direct view of the cost of diabetes on more than half of the countries in Africa. It is therefore a cardinal picture as to the economic burden of diabetes in the African continent. It further shows the estimated cost of illness (diabetes) per region (country)/year.
Suleiman IA, Fadeke OF, Okubanjo OO. Pharmacoeconomic evaluation of anti-diabetic therapy in a Nigerian tertiary health institution. Annals of African Medicine. 2006;5:132–137.
Alouki K, Delisle H, Besançon S, Baldé N, Sidibé-Traoré A, Drabo J, et al. Simple calculator to estimate the medical cost of diabetes in sub-Saharan Africa. World J Diabetes. 2015;6:1312–22.
Ogle GD, Kim H, Middlehurst AC, Silink M, Jenkins AJ. Financial costs for families of children with type 1 diabetes in lower-income countries. Diabet Med. 2015;33:820–6.
Suleiman IA, Festus JA. Cost of illness among diabetes mellitus patients in Niger Delta, Nigeria. J Pharm Health Serv Res. 2015;6:53–60.
Ngassam E, Nguewa J-L, Ongnessek S, Foutko A, Mendane F, Balla V, et al. Cout de la prise en charge du diabète de type 2 a l’hopital central de yaounde. Diabetes Metab. 2012;38:A105.
Abdulganiyu G, Tayo F. What is the cost of illness of type II diabetes mellitus in a developing economy? Int J Pharm Pharm Sci. 2014;6:929–31.
Quaye EA, Amporful EO, Akweongo P, Aikins MK. Analysis of the financial cost of diabetes mellitus in four cocoa clinics of Ghana. Value Health Reg Issues. 2015;7:49–53.
Elrayah-Eliadarous H, Yassin K, Eltom M, Abdelrahman S, Wahlström R, Östenson C-G. Direct costs for care and glycaemic control in patients with type 2 diabetes in Sudan. Exp Clin Endocrinol Diabetes. 2010;118:220–5.
Elrayah H, Eltom M, Bedri A, Belal A, Rosling H, Ostenson C-G. Economic burden on families of childhood type 1 diabetes in urban Sudan. Diabetes Res Clin Pract. 2005;70:159–65.
Chale S, Swai A, Mujinja P, McLarty D. Must diabetes be a fatal disease in Africa? Study of costs of treatment. BMJ. 1992;304:1215–8.
Ipingbemi AE, Erhun WO. Cost implications of treatment of diabetes mellitus in a secondary healthcare facility in Ibadan. Afr J Med Med Sci. 2015;44:79–87.
Okoronkwo IL, Ekpemiro JN, Okwor EU, Okpala PU, Adeyemo FO. Economic burden and catastrophic cost among people living with type 2 diabetes mellitus attending a tertiary health institution in south-east zone, Nigeria. BMC Res Notes. 2015;8.
Danmusa UM, Terhile I, Nasir IA, Ahmad AA, Muhammad HY. Prevalence and healthcare costs associated with the management of diabetic foot ulcer in patients attending Ahmadu Bello University Teaching Hospital, Nigeria. Int J Health Sci. 2016;10:219–28.
Ogbera AO, Fasanmade O, Ohwovoriole AE, Adediran O. An assessment of the disease burden of foot ulcers in patients with diabetes mellitus attending a teaching hospital in Lagos, Nigeria. Int J Low Extrem Wounds. 2006;5:244–9.
Cavanagh P, Attinger C, Abbas Z, Bal A, Rojas N, Xu Z-R. Cost of treating diabetic foot ulcers in five different countries. Diabetes Metab Res Rev. 2012;28(Suppl 1):107–11.
Mutyambizi C, Pavlova M, Chola L, Hongoro C, Groot W. Cost of diabetes mellitus in Africa: a systematic review of existing literature. Glob Health. 2018;14:3.
Mbanya J-C, Mbanya D. Diabetes cost in sub-Saharan Africa. J Cardiovasc Risk. 2003;10:191–3.
Bloom BS, Bruno DJ, Maman DY, Jayadevappa R. Usefulness of US cost-of-illness studies in healthcare decision making. PharmacoEconomics. 2001;19:207–13.
Tarricone R. Cost-of-illness analysis. What room in health economics? Health Policy Amst Neth. 2006;77:51–63.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Clarisse Mapa Tassou, Jean-Claude Katte, Camille Mba Maadjhou, and Jean Claude Mbanya declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Economics and Policy in Diabetes