Abstract
Diabetes imposes a huge financial burden on affected individuals, their families, society, and country. Undesirable changes in lifestyle coupled with inadequate health care systems are some of the major drivers of diabetes burden in sub-Saharan Africa (SSA), where there will be the greatest increase of diabetes in the world of 143%, within the next 25 years. Only 5.5% of the GDP in SSA was spent on health in 2016 compared to the global estimate of 10%. Although SSA has witnessed a recent increase in diabetes incidence, the current diabetes-related expenditure of US$9.5 billion represents only 1% of the overall global expenditure on this disease. These include the direct costs associated with medical care, and the indirect costs resulting from cessation or reduced productivity because of disease-related disability/premature mortality. Indirect cost per patient with diabetes in SSA is higher than direct expenditures, contributing over 60% of the total cost.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Nearly 80% of noncommunicable disease (NCDs) related deaths including diabetes, occur in low- and middle- income countries, which constitute the majority of countries in sub-Saharan Africa (SSA) (WHO 2019a). Available estimates show that 7.1% of adults living in Africa or 33 million people suffer from diabetes, although in 2019 the International Diabetes Federation estimated that diabetes affected over 19 million people in the region, while an additional 45 million adults had impaired glucose tolerance (IGT) (IDF Diabetes Federation 2019a). Nigeria is among the top ten countries in the world with the highest number of people with IGT (8.2 million people). If current trends persist, both the number of people with type 2 diabetes (T2D) and IGT in SSA will increase by 143% by 2045; the highest global predicted increase. However, the true number could be much higher, given that as many as two thirds of those with the disease remain undiagnosed (IDF Diabetes Federation 2019a).
This rising burden of diabetes in SSA has been triggered by increasing obesity and changing lifestyles in both rural and urban communities (Mbanya et al. 2014). As in other parts of the world, more than 90% of patients have type 2 diabetes with diagnosis often made late in the course of disease progression, or at the time of complications. Also, approximately 10,300 children and adolescents are diagnosed each year with type 1 diabetes (T1D) which carries a high mortality rate (IDF Diabetes Federation 2019a).
Social and Financial Burden
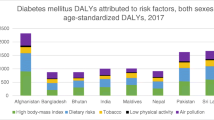
Delayed diagnosis and poor metabolic control contribute to the high morbidity and premature mortality in the region (Dalal et al. 2011). The mortality rate is increasing and occurring at younger ages in SSA compared with the other regions; three of four deaths due to diabetes occur in the active age group less than 60 years old (IDF Diabetes Federation 2019a; Miranda et al. 2019). Total disability adjusted life-years (DALYs) due to diabetes increased by 126.4% between 1990 and 2017, and the Lancet Diabetes and Endocrinology Commission estimated that in 2015, the overall cost of diabetes in sub-Saharan Africa was US$19.45 billion, or 1.2% of cumulative gross domestic product (GDP) (Gouda et al. 2019; Atun et al. 2017).
Despite progress in health coverage, access to medications especially insulin and quality healthcare facilities remain a challenge, with wide disparities between African countries (Mutyambizi et al. 2018). Poor access to insulin is the major cause of mortality in children with T1D (Atun and Gale 2015; Choukem et al. 2019). This has a huge financial implication for the economy of households and the already overburdened healthcare systems.
Few African countries have a national diabetes plan and there is a lack of access to full coverage for essential health services (IDF Diabetes Federation 2019a). Due to the lack of primary data and the high proportion of undiagnosed diabetes to estimate the real-world cost of diabetes in the SSA, public health interventions have relied on results from modeling methods (Afroz et al. 2018). Africa’s health service delivery capacity has improved, yet this is still insufficient to meet current and future needs of the care of diabetes (WHO 2019b).
Challenges to Diabetes Management in Africa
These challenges are of two magnitudes: the increase in diabetes growth and those related to the implementation of effective diabetes care in Africa (Fig. 3.1).
Epidemiological transitions:
In the 1980s, diabetes was still uncommon in Africa, but today it has exploded in many communities. This trend in T2D has been strongly linked to obesity, suboptimal diet, and physical inactivity, resulting from the rapid epidemiologic shifts involving urbanization and changing lifestyles in both the rural and urban communities of SSA (Mbanya et al. 2014). The age-standardized diabetes prevalence increased in parallel with body mass index from 3.4 to 8.5% in men, and 4.1 to 8.9% in women between 1980 and 2014 (NCD Risk Factor Collaboration (NCD-RisC)—Africa Working Group 2017). Global rise in BMI is usually linked to the increase in BMI in rural communities, except in SSA where BMI rose faster among urban women, and at a similar rate among urban and rural men (NCD Risk Factor Collaboration (NCD-RisC) 2019). The expansion of supermarkets with access to highly processed food and sweetened beverages as well as reduced physical activity could be driving the rural-urban differences (Pastakia et al. 2017; Assah et al. 2011).
Access to Health Care
Many African countries are not prepared to effectively manage diabetes and they provide only suboptimal care to patients. Early identification, management, and control are important determinants for the reduction of diabetes complications, thus leading to a substantial reduction of the economic burden (Atun and Gale 2015; Kapwata and Manda 2018).
Timely diagnosis and prevention rely mostly on the availability of health care practitioners, regular screening, and management of comorbidities (Pastakia et al. 2017). The proximity of healthcare facilities has been strongly linked to increasing utilization of these services in developing countries, especially in rural communities (Feikin et al. 2009). Financial availability and accessibility of health services, transportation facilities, and cost, as well as the receptiveness of the healthcare professionals to the cultural and social norms of the community are equally relevant (Huerta Munoz and Källestål 2012). Poor access to insulin is the leading cause of mortality in patients with T1D (Gale 2006). Among the 400 million people globally who do not have access to basic healthcare services, the majority live in SSA (Sanogo et al. 2019).
Knowledge, Beliefs, and Health Seeking Behaviors in Africa
Obesity which is a major risk factor for T2D is still perceived by some people as a sign of wealth and good living, while physical activity like regularly walking is a sign of poverty. Although most patients recognize that health care facilities are the ideal places to turn to, it is not unusual for patients to seek solely or as complementary care, the traditional healers (Choukem et al. 2019). Diverse knowledge, beliefs, and perceptions in addition to finances are key factors that influence a patient’s decision to seek medical advice during an illness. Moreover, misconceptions associated with hospital facilities contribute to increasing the total cost associated with diabetes, as some patients tend to be managed at home or seek traditional healers, thereby presenting to health facilities mostly at the time of complications (Choukem et al. 2019).
Lack of Political Will
There is still a lack of appropriate action taken by key decision leaders in SSA, in order to halt the progression of diabetes (Atun and Gale 2015). The misconception that diabetes is a disease of the rich and the elderly, hampers commitments to mobilize adequate resources for the management of diabetes and its complications. In fact, less than 30% of African countries have operational integrated policies for diabetes care (Kengne et al. 2013).
Under-Allocation of Resources
Inadequate financing of NCDs like diabetes constitutes a major barrier to the early diagnosis and management of diabetes complications (Atun and Gale 2015). Although infections, maternal and perinatal mortality continue to threaten African healthcare systems, the idea that infectious diseases should be controlled before tackling NCDs is mostly misleading. According to WHO estimates in 2015 infectious diseases, maternal, perinatal, and nutritional conditions accounted for 59.1% of all age total DALYs, while NCDs were responsible for 30.7% (WHO 2019a). In addition, NCDs are responsible for up to 37% of total loss of productivity in SSA, compared to only 27% for infectious diseases (WHO 2019b).
Complications and Mortality Attributable to Diabetes
Noncommunicable diseases like diabetes and cardiovascular account for 41 million deaths each year; the leading cause of mortality globally. Over 85% of these deaths occur in low- and middle-income countries (WHO 2019a), and the acute and chronic complications associated with the disease make it very costly to manage (Kengne et al. 2013). Diabetes is a major cause of non-traumatic lower limb amputation, blindness, kidney failure, heart attacks, and stroke (IDF Diabetes Federation 2019a).
Prevalence and Incidence of Diabetes Complications
Chronic complications of diabetes may be present at the time of diagnosis especially in patients with T2D, but can also appear soon after the diagnosis in patients with T1D (IDF Diabetes Federation 2019a). In early 2000, macrovascular complications of diabetes were considered rare in Africa, with coronary heart disease affecting 5–8% of type 2 diabetic patients (Mbanya and Sobngwi 2003). However, there is increasing evidence suggesting an increase in the burden of cardiovascular disease in SSA (Kengne et al. 2013), as a result of poor glycemic control in addition to other cardiovascular risk factors such as high blood pressure and dyslipidemia (Kengne et al. 2005).
Five percent of patients with diabetes have cerebrovascular accidents at diagnosis, and up to 9.5% and 25% of patients with type 1 and 2 diabetes respectively also have retinopathy at diagnosis. Depending on the glycemic control and duration of diabetes the prevalence of diabetic retinopathy varies between 13 and 55 %, with severe retinopathy representing 15% of all cases (Mbanya and Sobngwi 2003; Kengne et al. 2005). Eight to 49% of patients with diabetes exhibit nephropathy and neuropathy is present in 11–66% depending on the diagnostic method used (Dalal et al. 2011). Long-standing complications in patients with T1D do not differ greatly from those with T2D (Motala et al. 2001).
Lower extremity amputation varies from 1.5 to 7% (Mbanya and Sobngwi 2003). Diabetes complications in Africa are increasing as the prevalence and incidence of diabetes continue to rise. In Ghana, the incidence of diabetes-related lower limb amputations increased from 0.6 per 1000 follow up years in 2010 to 10.9 in 2015 (Sarfo-Kantanka et al. 2019). This is in contrast to industrialized countries where the complication rates are reducing (IDF Diabetes Federation 2019a). The coexistence of multiple chronic complications of diabetes is common, like in Nigeria where 51.7% of patients with diabetes and renal complications also had the peripheral vascular disease (Agaba 2004). Interactions between peripheral damaged organs and infection occur in up to 53% of patients with diabetes (Dalal et al. 2011). Heavy investment in the health care system like dialysis units and coronary care units are necessary to take care of these diabetes-related complications.
Disability and Mortality
In 2017, NCDs accounted for 80% of disabilities globally with diabetes being the fourth leading cause (Mbanya et al. 2014). The age-standardized DALY rates for diabetes are higher amongst men than women (Gouda et al. 2019). Disability and the premature mortality caused by diabetes occur at a younger age in SSA compared to other regions. Globally in 2019, diabetes was responsible for 366,200 deaths with 3 of 4 deaths occurring before 60 years whereas, in 2009, diabetes-related mortality was highest in the age group of 30–39 years (IDF Diabetes Federation 2019a, b). High blood pressure which is common in blacks, was found to be about twice more common in people with diabetes compared to age-matched controls, while dyslipidemia ranged from 16 to 89% and overweight 50–83%. Cardiovascular complications are amongst the leading cause of mortality from chronic complications in patients with T2D (Kengne et al. 2005).
Although there is poor documentation on the causes of deaths in Africa, available estimates suggest that diabetes-related mortality ranges between 8 and 41% of all-cause mortality, and this is primarily due to acute complications and infections (Peer et al. 2014). In Cameroon, acute complications were the leading cause of mortality (22.2%) followed by cardiovascular complications (16.7%) and nephropathy (14.8%) (Foryoung et al. 2018). The life expectancy in children with T1D could be as low as 1% in Africa (Beran and Yudkin 2006). In South Africa, the predominant cause of mortality in patients with T1D is nephropathy, accounting for over 40% of all deaths (Gill et al. 2005). Table 3.1 shows the number of deaths in adults aged 20–79 years for some SSA countries.
Economic Burden of Diabetes Mellitus
Three alternative approaches exist to estimate the economic burden of public health problems like diabetes including the willingness to pay approach, the macroeconomic/production function approach, and the cost of illness approach (COI). The last one is the most commonly employed and takes into account the direct cost, indirect cost, and intangible cost (Fig. 3.2).
Measurements approaches to the economic burden of diabetes (Adapted from Kirigia et al. (2009))
Costs Attributable to Diabetes Mellitus in Africa
Since 2001, there has been a steady rise in the gross domestic product (GDP) of many sub-Saharan African countries, reaching its peak in 2014. In 2016, the mean GDP per capita spent by SSA countries was equivalent to US$1511.3 with a wide range from US$282.1 in Burundi to US$15,077.8 in Seychelles (The World Bank 2019). Overall, less than 5.6% of the GDP was spent on healthcare in the low- and middle-income countries of SSA. The World Health Organization (WHO) estimates that up to 11 million Africans fall into poverty each year, due to high out of pocket payments for healthcare (WHO 2019b). Few studies have quantified the economic burden of diabetes at the regional level. A major difficulty in collating data for the cost of illness studies is that authors report on only one type of cost; mostly the direct cost (Afroz et al. 2018). In South Africa, where the diabetes age-adjusted prevalence is 12.7%, mean diabetes-related expenditure was US$1245.0 per patient (Table 3.1), while in Benin, the age-adjusted diabetes prevalence was 1% and mean expenditure was US$163.8 pp.
Diabetes costs have increased from 1.4 billion in 2010 to 9.5 billion in 2019. This is due to both an increase in the prevalence of diabetes by 57%, and an increase in the cost of persons living with diabetes from US$222.6 to US$509 (IDF Diabetes Federation 2019a, b). According to current reports, the cost of care for people with diabetes in Africa accounts for 12.5% of healthcare expenses, with the highest percentage in South Africa (23.0%) (IDF Diabetes Federation 2019a).
Purchasing Power Parity Calculations
Nineteen million adults with diabetes recorded in Africa in 2019 resulted in a total economic cost of US$9.5 billion. Using the 2005 purchasing power parity (PPP), Kirigia and colleagues estimated the cost of diabetes per patient at Int$3633, giving a total burden of Int$25.51 billion, with indirect cost contributing 68% of it (Kirigia et al. 2009). Consistent with this, other reviews have reported the indirect costs of diabetes per patient to be higher than the direct costs (Mutyambizi et al. 2018). Nevertheless, Bommer and colleagues found a lower contribution of indirect cost (44.4%) (Bommer et al. 2017).
Cost of medication and hospitalization are the major causes of direct expenses (Afroz et al. 2018). A review reported the cost of medication to contribute as high as 50% of the total cost (Mutyambizi et al. 2018).
Direct Cost
The direct cost of a disease refers to resources used for the treatment of the disease regardless of whether they are born by patients themselves, by private or public payers, or by the government (IDF Diabetes Federation 2019a). This is usually divided into the direct medical cost which are expenses, borne as a result of direct medical treatment like medications, outpatient visits, laboratory tests, and hospitalizations. The second is the direct nonmedical cost which are expenses incurred as a result of transportation, food, lodgment. In COI studies, cost of medications, diagnostic cost, cost of the consultation, and inpatient cost is the most commonly reported (Mutyambizi et al. 2018).
Profile of African Countries
The direct cost of diabetes differs greatly between African countries with reported costs estimated from Int$3.5 billion to Int$4.5 billion and over US$10.8 billion per annum (Mutyambizi et al. 2018; Bommer et al. 2017) (Table 3.2). There are inconsistent findings of the major contributors, with some reviews reporting the cost of hospitalization as predominant, and other medication costs (Mutyambizi et al. 2018; Afroz et al. 2018). For outpatients in Nigeria, the cost of medication varied between Int$420.63 to Int$1025.00 per patient per annum for type 1 and 2 diabetes respectively, thus contributing as high as 90% of all treatment cost. For hospitalized patients, the cost of medication ranged from Int$553 to 1438 per admission in Nigeria and Int$80 to 461 in South Africa. In Cameroon, the cost of medication was estimated at I$3.9 per patient per month (Mutyambizi et al. 2018). The greatest expense incurred for diabetes medications comes from insulin. Indeed, the annual treatment for diabetes with insulin is US$104.4 compared to US$26.9 with metformin (Atun et al. 2017).
Several factors are associated with the direct cost of diabetes include socioeconomic factors like age, level of education and income class, factors related to diabetes like duration of diabetes, number of complications, mode of treatment, hospitalizations, and surgery (Afroz et al. 2018). As shown in Table 3.2, the cost of T1D is consistently higher than for type 2 diabetes across the studies.
Indirect Cost
The indirect cost is the opportunity cost resulting from reduced or loss of productivity at work by patients and their accompanying persons, because of the disease-related disability or premature mortality (Afroz et al. 2018). This includes the productive time lost for medical reasons like traveling for medical consultations and waiting to be admitted, hospital admissions for complications, absence from work for disease-related disability, and years of work lost due to premature deaths. Depending on the approach used to calculate the indirect cost of diabetes, the economic burden might be overstated. Some methods estimate the indirect cost for the unemployed while others use a more conservative approach like the friction-cost approach (Van den Hout 2010).
The COI study in 2015 used four sources of indirect costs: labor-force drop out; mortality; absenteeism; and presenteeism (Bommer et al. 2017). Globally, the first two contribute 48.5% and 45.5% respectively of indirect cost, however, this is different in LMICs where mortality dominates, contributing 63.6% of the indirect cost in middle-income countries and 90.6% in low-income countries. As shown in Table 3.2, the annual indirect cost of diabetes per patient was estimated at US$762.20 in Mali, for an annual total cost per patient of US$365.48, while in Morocco, the indirect cost per patient per month was US$1113 (Bermudez-Tamayo et al. 2017; Boutayeb et al. 2013). Because most studies report only on the direct cost, there is a dearth of information on the indirect cost of diabetes in Africa. Nonetheless, its contribution to total cost could contribute to over 60% of the total cost (Kirigia et al. 2009; Mapa-Tassou et al. 2019).
Intangible Cost
Intangible cost relates to the reduced quality of life as a result of the physical, psychological, and social handicap of disease. The quality of life can be severely affected by chronic diseases and examples include pain, worry, anxiety, loss of independence, and lack of participation in social events (Afroz et al. 2018).
Intangible costs are the most difficult to assess given that they are related to emotions. Because the quality of life is difficult to express in terms of money, many studies do not report on the intangible cost. Intangible cost of diabetes may range between US$30.8 per month if the patient had no complications, to US$143.9 if four or more complications were present. If patients had blood glucose levels within targets, the intangible cost was estimated at 10.3 per month, compared to US$41.1, if poorly controlled, with an annual estimate of US$496.7 (Afroz et al. 2018).
Cost of Diabetes Complications
The major contributor to direct costs for diabetes-related complications is hospitalization, and for indirect cost are absenteeism, disability, and premature mortality. There is a linear relationship between expenditures and the number of complications present. According to the International Diabetes Federation estimates, the treatment of diabetes-related complications accounts for over 50% of the direct cost attributable to diabetes, and this expenditure is highest in the 60–70 years age group (IDF Diabetes Federation 2019a).
Nephropathy, diabetic foot, and stroke are the complications associated with the highest expenses in Africa (Mutyambizi et al. 2018). Patients with diabetes are likely to spend up to four times more if they have diabetes-related complications compared to those with no complication, and this varies greatly by countries. In Mali, up to Int$1346.5 per patient was spent on nephropathy while only Int$33.03 was spent in Guinea. For acute complications like diabetic ketoacidosis, the cost of management differs in those with and without chronic complications. In Guinea, the cost of treatment for diabetic ketoacidosis ranged from Int$22.1 to Int$39.2, and in Burkina Faso from Int$628.27 to Int$1085.4 (Mutyambizi et al. 2018).
Mean annual health expenditures for people with four or more complications are expected to be about 20 times more than in people without complications (IDF Diabetes Federation 2019a). Consistent with this, the presence of one or more complications increased the cost ratio by 1.1 for retinopathy and up to 4.3 for an infected diabetes foot in another study. This is because, in Africa, foot complications in patients with diabetes often progress to infection or gangrene, resulting in longer hospitalizations and higher mortality rates (Mutyambizi et al. 2018).
Comparative Health Care Expenditures in Africa
In 2016, 5.5% of the GDP in Africa was spent on health against 10% at the global level, with SSA having the highest out of pocket expenses (36.7%) (WHO 2019b; The World Bank 2019). In SSA, the GDP percent spent on health is not related to the national expenditure. For example, Sierra Leone with GDP per capita of US$501.4 spent 16.53% of its budget on healthcare, while others like Equatorial Guinea and Nigeria having a GDP of US$9738.4 and 1968.6 spent only 3.38% and 3.35% respectively. Similarly, out of pocket expenses on health care were highest in Equatorial Guinee and Nigeria (72.83% and 75.21% respectively) (WHO 2019c).
Globally, at least US$760 billion is expected to be spent on diabetes annually, and it could reach US$845 billion by 2045 (IDF Diabetes Federation 2019a). The expenditure per person in high-income countries (US$5339) was over 30-folds and almost sevenfold higher than in low- and middle-income countries respectively in 2019. Reduced or missed production opportunities due to diabetes contribute an additional 35% to the annual global health expenditures. Overall, direct expenses on diabetes have increased by 4.5% over the last 2 years, and it is predicted to increase by 11.2% over the next 25 years (IDF Diabetes Federation 2019a). It is possible that the real estimates are more important as actual projections are conservative, and based on the assumption that diabetes prevalence and expenditures are not changing. One can find substantially higher estimates for the global economic burden of diabetes at US$1.31 trillion, equivalent to 1.8% of the world GDP, with indirect cost contributing 34.7% of the overall burden in a COI study of 2015 (Bommer et al. 2017).
In 2015, North America had the highest economic burden at US$499.40 billion (2.6% of its total GDP), while Africa had the lowest diabetes-related expenditure; US$9.45 billion (1.2% of its total GDP). The contribution of the indirect cost was more important in high-income countries compared to LMICs (40.0% versus 33.5%) (Bommer et al. 2017). While the cost of medication is the major contributor to direct cost in Africa, there are conflicting reports between the cost medication or cost of hospitalization at the global level (Ng et al. 2014). Indirect cost contributed as high as 44.6% in SSA and 57.4% in South Asia as opposed to only 21.9% in Latin America and the Caribbean, although there is a report of a higher contribution of the indirect cost of 68% to the total cost in SSA (Bommer et al. 2017). (Kirigia et al. 2009).
The lowest annual expenditure per person spent in SSA was in the Central African Republic, with similar estimates in Bangladesh (US$64), and Nepal (US$80). Overall, slightly higher expenditure was spent in 2019 in women than men across all the regions (US$382.6 billion versus US$377.6 billion) and this difference is predicted to be maintained over the years (IDF Diabetes Federation 2019a).
Perspectives
Countries with the lowest GDP have the highest burden of NCDs in terms of DALYs, therefore if nothing is done, the rapid increase in diabetes will badly affect the African region. The potential strategies to address the economic burden of diabetes are listed below.
National Diabetes Programs (NDPs)
Early management and lifestyle changes can delay or prevent T2D in 80% of individuals (IDF Diabetes Federation 2019a). Therefore, the development and implementation of diabetes programs may reduce the incidence of diabetes and mortality. Unfortunately, less than one-third of SSA countries have a national diabetes plan (IDF Diabetes Federation 2019a). Important areas for the focus of NDPs are conducting community cost-effective interventions, aiming at raising awareness on diabetes and its risk factors, increasing physical activity, losing weight, eating healthily, along with routine screening and clinical care, and access to essential medication and supplies.
Sustainable Development Goals
The third UN summit in New York in September 2018 recognized the challenges posed by diabetes and other NCDs on the socioeconomic development. To achieve the 2030 targets related to sustainable development goal 3, especially item 3.4 which aims at reducing premature mortality from NCDs by at least 33%, there is a need for governments, leaders, and stakeholders in SSA to urgently react to the threat imposed by diabetes and other NCDs. SSA healthcare systems continue to prioritize infectious diseases and currently, less than 30% of ministries in SSA have integrated policies for the management of diabetes and other NCDs (Kengne et al. 2013). Given that over 70% of deaths globally are due to NCDs, there is value in investing in strengthening the health care system and undertake more translational research to reduce the burden of diabetes (WHO 2019a). Furthermore, because diabetes mortality is highest in low-income countries, prioritization of the limited resources using cost-effective strategies, like the WHO Best Buys interventions (e.g., taxation on alcohol and tobacco products) to change behaviors may improve health outcomes (Atun et al. 2017; Kengne et al. 2013).
Universal Health Coverage (UHC)
Most countries in SSA do not have a national health care insurance coverage, and therefore out of pocket payment of care limits access for individuals with low income. Such an objective could be achieved by ensuring an equitable tax payment system, and compulsory health insurance (Sanogo et al. 2019).
References
Abdulganiyu G, Fola T (2014) What is the cost of illness of type II diabetes mellitus in a developing economy? Int J Pharm Pharm Sci 6:5
Afroz A, Alramadan MJ, Hossain MN, Romero L, Alam K, Magliano DJ et al (2018) Cost-of-illness of type 2 diabetes mellitus in low and lower-middle income countries: a systematic review. BMC Health Serv Res 18(1):972
Agaba EI (2004) Characteristics of type 2 diabetics presenting with end stage renal disease at the Jos University Teaching Hospital, Nigeria. West Afr J Med 23(2):142–145
Alouki K, Delisle H, Besançon S, Baldé N, Sidibé-Traoré A, Drabo J et al (2015) Simple calculator to estimate the medical cost of diabetes in sub-Saharan Africa. World J Diabetes 6(16):1312–1322
Assah FK, Ekelund U, Brage S, Mbanya JC, Wareham NJ (2011) Urbanization, physical activity, and metabolic health in sub-Saharan Africa. Diabetes Care 34(2):491–496
Atun R, Gale EAM (2015) The challenge of diabetes in sub-Saharan Africa. Lancet Diabetes Endocrinol 3(9):675–677
Atun R, Davies JI, Gale EAM, Bärnighausen T, Beran D, Kengne AP et al (2017) Diabetes in sub-Saharan Africa: from clinical care to health policy. Lancet Diabetes Endocrinol 5(8):622–667
Beran D, Yudkin JS (2006) Diabetes care in sub-Saharan Africa. Lancet 368(9548):1689–1695
Bermudez-Tamayo C, Besançon S, Johri M, Assa S, Brown JB, Ramaiya K (2017) Direct and indirect costs of diabetes mellitus in Mali: a case-control study. PLoS One 12(5):e0176128
Bommer C, Heesemann E, Sagalova V, Manne-Goehler J, Atun R, Bärnighausen T et al (2017) The global economic burden of diabetes in adults aged 20-79 years: a cost-of-illness study. Lancet Diabetes Endocrinol 5(6):423–430
Boutayeb W, Lamlili MEN, Boutayeb A, Boutayeb S (2013) Estimation of direct and indirect cost of diabetes in Morocco. J Biomed Sci Eng 06(07):732–738
Choukem SP, Dimala CA, Maadjhou C, Mbanya JC (2019) Diabetes management in Africa. In: Rodriguez-Saldana J (ed) The diabetes textbook. Springer, Cham, pp 273–288
Dalal S, Beunza JJ, Volmink J, Adebamowo C, Bajunirwe F, Njelekela M et al (2011) Non-communicable diseases in sub-Saharan Africa: what we know now. Int J Epidemiol 40(4):885–901
Elrayah H, Eltom M, Bedri A, Belal A, Rosling H, Östenson C-G (2005) Economic burden on families of childhood type 1 diabetes in urban Sudan. Diabetes Res Clin Pract 70(2):159–165
Elrayah-Eliadarous H, Yassin K, Eltom M, Abdelrahman S, Wahlström R, Ostenson C-G (2010) Direct costs for care and glycaemic control in patients with type 2 diabetes in Sudan. Exp Clin Endocrinol Diabetes 118(4):220–225
Feikin DR, Nguyen LM, Adazu K, Ombok M, Audi A, Slutsker L et al (2009) The impact of distance of residence from a peripheral health facility on pediatric health utilisation in rural western Kenya. Trop Med Int Health 14(1):54–61
Foryoung JB, Ditah C, Fon PN, Mboue-Djieka Y, Nebongo DN, Mbango ND et al (2018) Long-term mortality in outpatients with type 2 diabetes in a reference hospital in Cameroon: a retrospective cohort study. BMJ Open 8(2):e019086
Gale EAM (2006) Dying of diabetes. Lancet 368(9548):1626–1628
Gill GV, Huddle KRL, Monkoe G (2005) Long-term (20 years) outcome and mortality of Type 1 diabetic patients in Soweto, South Africa. Diabetes Med 22(12):1642–1646
Gouda HN, Charlson F, Sorsdahl K, Ahmadzada S, Ferrari AJ, Erskine H et al (2019) Burden of non-communicable diseases in sub-Saharan Africa, 1990–2017: results from the Global Burden of Disease Study 2017. Lancet Glob Health 7(10):e1375–e1387
Huerta Munoz U, Källestål C (2012) Geographical accessibility and spatial coverage modeling of the primary health care network in the Western Province of Rwanda. Int J Health Geogr 11:40
IDF Diabetes Federation (2019a) IDF Diabetes Atlas, 9th ed. International Diabetes Federation, Brussels (cited 2019 Dec 19). http://www.diabetesatlas.org/
IDF Diabetes Federation (2019b) International diabetes atlas, 4th ed. International Diabetes Federation, Brussels, Belgium 2009 (cited 2019 Dec 19). https://www.idf.org/e-library/epidemiology-research/diabetes-atlas/21-atlas-4th-edition.html
Kapwata T, Manda S (2018) Geographic assessment of access to health care in patients with cardiovascular disease in South Africa. BMC Health Serv Res 18(1):197
Kengne AP, Amoah AGB, Mbanya J-C (2005) Cardiovascular complications of diabetes mellitus in sub-Saharan Africa. Circulation 112(23):3592–3601
Kengne AP, June-Rose Mchiza Z, Amoah AGB, Mbanya J-C (2013) Cardiovascular diseases and diabetes as economic and developmental challenges in Africa. Prog Cardiovasc Dis 56(3):302–313
Kirigia JM, Sambo HB, Sambo LG, Barry SP (2009) Economic burden of diabetes mellitus in the WHO African region. BMC Int Health Hum Rights 9:6
Mapa-Tassou C, Katte J-C, Mba Maadjhou C, Mbanya JC (2019) Economic impact of diabetes in Africa. Curr Diabetes Rep 19(2):5
Mbanya J-C, Sobngwi E (2003) Diabetes in Africa. Diabetes microvascular and macrovascular disease in Africa. J Cardiovasc Risk 10(2):97–102
Mbanya JC, Assah F, Saji J, Atanga EN (2014) Obesity and type 2 diabetes in Sub-Sahara Africa. Curr Diabetes Rep 14:1–8
Miranda JJ, Barrientos-Gutiérrez T, Corvalan C, Hyder AA, Lazo-Porras M, Oni T et al (2019) Understanding the rise of cardiometabolic diseases in low- and middle-income countries. Nat Med 25(11):1667–1679
Motala AA, Pirie FJ, Gouws E, Amod A, Omar MAK (2001) Microvascular complications in South African patients with long-duration diabetes mellitus. S Afr Med J 91(11):987–992
Mutyambizi C, Pavlova M, Chola L, Hongoro C, Groot W (2018) Cost of diabetes mellitus in Africa: a systematic review of existing literature. Glob Health 14(1):3
NCD Risk Factor Collaboration (NCD-RisC) (2019) Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature 569(7755):260–264
NCD Risk Factor Collaboration (NCD-RisC)—Africa Working Group (2017) Trends in obesity and diabetes across Africa from 1980 to 2014: an analysis of pooled population-based studies. Int J Epidemiol 46(5):1421–1432
Ng CS, Lee JYC, Toh MP, Ko Y (2014) Cost-of-illness studies of diabetes mellitus: a systematic review. Diabetes Res Clin Pract 105(2):151–163
Ngassam E, Nguewa J-L, Ongnessek S, Foutko A, Mendane F, Balla V et al (2012) P318 Cout de la prise en charge du diabète de type 2 a l’hopital central de yaounde. Diabetes Metab 38:A105
Ogle GD, Kim H, Middlehurst AC, Silink M, Jenkins AJ (2016) Financial costs for families of children with Type 1 diabetes in lower-income countries. Diabetes Med 33(6):820–826
Pastakia SD, Pekny CR, Manyara SM, Fischer L (2017) Diabetes in sub-Saharan Africa—from policy to practice to progress: targeting the existing gaps for future care for diabetes. Diabetes Metab Syndr Obes 10:247–263
Peer N, Kengne A-P, Motala AA, Mbanya JC (2014) Diabetes in the Africa Region: an update. Diabetes Res Clin Pract 103(2):197–205
Quaye EA, Amporful EO, Akweongo P, Aikins MK (2015) Analysis of the financial cost of diabetes mellitus in four cocoa clinics of Ghana. Value Health Reg Issues 7:49–53
Sanogo NA, Fantaye AW, Yaya S (2019) Universal health coverage and facilitation of equitable access to care in Africa. Front Public Health 7:102
Sarfo-Kantanka O, Sarfo FS, Kyei I, Agyemang C, Mbanya JC (2019) Incidence and determinants of diabetes-related lower limb amputations in Ghana, 2010–2015—a retrospective cohort study. BMC Endocr Disord 19(1):27
Suleiman IA, Festus JA (2015) Cost of illness among diabetes mellitus patients in Niger Delta, Nigeria. J Pharm Health Serv Res 6:53–60
Suleiman IA, Fadeke OF, Okubanjo OO (2006) Pharmacoeconomic evaluation of anti-diabetic therapy in a Nigerian Tertiary Health Institution. Ann Afr Med 5:132–137
The World Bank (2019) Data indicators (cited 2019 Dec 19). https://data.worldbank.org/indicator
Van den Hout WB (2010) The value of productivity: human-capital versus friction-cost method. Ann Rheum Dis 69(1):89–91
WHO (2019a) NCD mortality and morbidity (cited 2019 Dec 19). http://www.who.int/gho/ncd/mortality_morbidity/en/
WHO (2019b) A heavy burden: the productivity cost of illness in Africa. WHO, Regional Office for Africa (cited 2019 Dec 19). https://www.afro.who.int/publications/heavy-burden-productivity-cost-illness-africa
WHO (2019c) Global health expenditure database 2017 (cited 2019 Dec 19). Available from: https://apps.who.int/nha/database/Select/Indicators/en
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Mba, C.M., Mbanya, J.C. (2020). Challenges and Economic Burden of Diabetes in Africa. In: Faintuch, J., Faintuch, S. (eds) Obesity and Diabetes. Springer, Cham. https://doi.org/10.1007/978-3-030-53370-0_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-53370-0_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-53369-4
Online ISBN: 978-3-030-53370-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)