Abstract
Purpose of Review
Insulin resistance is an early complication of chronic kidney disease (CKD) associated with worsening cardiovascular outcomes. This review will evaluate mechanisms responsible for CKD-induced insulin resistance and therapies currently available.
Recent Findings
Recent mechanisms have been identified including SIRPα and specific E3 ubiquitin ligases causing insulin resistance in CKD. The hallmark finding in these mechanisms is degradation of the insulin receptor substrate 1 (IRS1) which impairs intracellular insulin signaling and ultimately metabolism. The mechanisms responsible for insulin resistance in CKD include inflammation, oxidative stress, elevations in aldosterone, angiotensin II, uremic toxins, and metabolic acidosis. Potential treatments currently available for CKD-induced insulin resistance include lifestyle modification and metformin. Potential future treatments may include glucagon-like peptide agonists, SGLT2 inhibitors, and thiazolidinediones.
Summary
Investigations into molecular mechanisms responsible for insulin resistance in CKD may provide new therapeutic targets while current therapies may prevent the catabolic sequelae of CKD and ameliorate its cardiovascular consequences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic kidney disease (CKD) is associated with an increase in mortality which increases with the stage of disease. Results from a NIH-supported, multi-center, clinical trial carried out over 2.5 years revealed that end-stage kidney disease increased mortality by greater than 46% [1]. One of the factors contributing to this increased mortality is insulin resistance. Insulin resistance is an independent predictor of cardiovascular mortality [2, 3] and has long been associated with CKD even in the absence of diabetes and with mild loss of kidney function [4, 5]. Fliser et al. found patients with early stages of CKD with near normal creatinine had defects in insulin-mediated metabolism of glucose [5]. Jia et al. used a modified oral glucose tolerance test and reported insulin resistance in CKD patients with a median GFR of 46 ml/min per 1.73 m2 [6]. Furthermore, insulin resistance is not limited to specific etiologies of kidney disease, e.g., diabetes, IgA nephropathy, or polycystic kidney disease [5]. Several factors have been identified as causal in CKD-induced insulin resistance, including the accumulation of toxins such as indoxyl sulfate or urea. How these compounds impair intracellular insulin signaling is unclear [7,8,9]. Other evidence provides a link between glucose intolerance in CKD and defects in intracellular signaling that occur as a result of CKD complications (e.g., metabolic acidosis, increased glucocorticoid production, excess angiotensin II, and inflammation) (Fig. 1). For example, changes in tyrosine phosphorylation may impair insulin signaling, decreasing phosphatidylinositol 3-kinase (PI3K) and p-Akt activation, leading to protein degradation and muscle wasting [11••, 12, 13].
A scheme representing CKD associated metabolic derangements inducing insulin resistance while impairing intracellular insulin signaling leading to metabolic consequences. Adapted from Kidney International (2015) 88, 1233–1239. Insulin receptor substrate-1 (IRS-1), Phosphoinositide 3 kinase (PI3K), protein kinase B also known as AKT. (Reprinted from: Thomas SS, et al. Kidney Int 2015; 88(6): 1233–9, with permission from Elsevier) [10]
There is a general dearth of information about therapies that can routinely prevent insulin resistance in animal models or people with CKD. However, antidiabetic agents which improve cardiorenal outcomes in people with diabetes and CKD, such as SGLT2 inhibitors [14••, 15•], may also prove effective in treatment of insulin resistance in people with nondiabetic CKD. For example, recent data suggests that SGLT2 inhibitors may improve insulin resistance as well as cardiorenal complications of CKD [14••, 15•, 16]. In this review, we will examine recent advances in identifying molecular mechanisms that cause insulin resistance; we will also describe CKD-specific metabolic derangements that are responsible for contributing to insulin resistance. Finally, we will discuss recent trials that highlight potentially promising novel treatments for insulin resistance in CKD.
Diagnostic Testing
Diagnostic testing for insulin sensitivity is largely confined to research settings because the available methods are time-consuming and invasive and require frequent monitoring and trained personnel. The current “gold standard” for measuring insulin resistance is the euglycemic clamp test. Patients simultaneously receive intravenous infusions of insulin and glucose to maintain a constant level of blood glucose. At equilibrium, the rate of glucose administration is equal to the rate of its uptake into the cells, which reflects insulin sensitivity in the overall body. As such, a high rate of glucose infusion signifies total body insulin sensitivity while a low rate shows resistance to insulin [4]. Simpler and less invasive tests have been used to estimate insulin resistance. These assays evaluate insulin sensitivity in either static (i.e., fasting) or dynamic (infusion of glucose or insulin) states, reflecting more largely hepatic vs. skeletal muscle insulin sensitivity, respectively [17]. The homeostatic model assessment of insulin resistance (HOMA-IR) is a commonly used mathematical equation which estimates static insulin sensitivity in fasting state [18]. The oral or intravenous glucose tolerance tests (OGTT or IVGTT) are examples of dynamic tests based on the changes in insulin and glucose in response to a challenge with oral or intravenous glucose. In OGTT, after an overnight fast, blood samples for determinations of glucose and insulin concentrations are taken at 0, 30, 60, and 120 min following a standard oral glucose load. Specific indexes including Matsuda index, Stumvoll index, Avignon index, oral glucose insulin sensitivity index (OGSI), Gutt index, and Belfiore index use particular sampling protocols during the OGTT or the meal [19,20,21,22,23,24].
Molecular Mechanism of Insulin Resistance
Intracellular Insulin Signaling
Identifying the mediators of intracellular insulin signaling may be key to determining potential targets for therapy of insulin resistance. Normal insulin signaling is initiated when insulin binds to its receptor causing auto-phosphorylation of tyrosines of insulin receptor substrate1 (IRS1). This is followed by phosphorylation of phosphatidylinositol 3-kinase (PI3K) and Akt kinase (pAkt). Akt phosphorylation triggers several downstream responses in peripheral tissues, leading to GLUT4 translocation to the membrane, as well as promoting glycogen and protein synthesis and inhibiting lipid and protein degradation. Abnormal intracellular signaling in CKD results in low levels of pAkt in peripheral tissues, leading to alterations in metabolism of glucose and lipids as well as accelerated protein degradation in muscle [10]. Specifically, CKD activates the ubiquitin proteasome system (UPS) which leads to degradation of IRS1, reduced phosphorylation of Akt, and eventually impaired protein, lipid, and glycogen synthesis, as well as increased muscle protein degradation and lipolysis (Fig. 1).
Signal Regulatory Protein Alpha
Signal regulatory protein alpha (SIRPα) impairs insulin signaling by dephosphorylating the tyrosines on the insulin receptor and IRS1 [11••]. It is expressed highly in the skeletal muscles in a mouse model of CKD. When SIRPα is suppressed, intracellular insulin signaling improves, leading to suppression of protein degradation. Conversely, overexpression of SIRPα impairs insulin signaling and exacerbates abnormal muscle metabolism. Identification of Nf-kB binding sites in SIRPα promoter suggests that inflammation may promote SIRPα overexpression in CKD. As such, reducing SIRPα expression, for example by ameliorating inflammation, may serve as a therapeutic target for preventing insulin resistance in CKD.
Ubiquitin Proteasome System
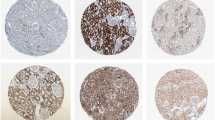
The UPS is responsible for targeted protein degradation [10]. The proteolytic process begins when a ubiquitin-activating enzyme (E1) forms a thioester bond with ubiquitin. Ubiquitin is then transferred to a ubiquitin-conjugating enzyme (E2). In the third step, the ubiquitin ligase (E3) catalyzes formation of an isopeptide bond between ubiquitin and a lysine residue on the targeted protein. This process is repeated until a chain of five ubiquitins is formed on the targeted proteins, which are then sent for degradation by the 26S proteasome. This proteasome recognizes the chain of ubiquitins and removes them to dissemble and degrade the protein into peptides, which are later degraded by cytoplasmic peptidases. E3 ligases are single- or multi-subunit enzymes with separate domains for binding to ubiquitin and substrate proteins. The selectivity of the UPS system comes from the large number of E3 ligases, each of which binds a specific set of protein targets. Specifically, IRS1 degradation by the UPS leads to impaired insulin signaling (Fig. 2). CKD and its associated complications stimulate the expression of different E3 ubiquitin ligases, thus altering the specific proteins targeted for degradation by the UPS [10].
IRS1 degradation is characterized by activation of disease-specific E3 ubiquitin ligases. Adapted from Kidney International (2015) 88, 1233–1239. Insulin receptor substrate-1 (IRS-1), insulin growth factor-1 (IGF-1), Casitas B-lineage lymphoma B (Cblb), Cullin 7 (Cul7). (Reprinted from: Thomas SS, et al. Kidney Int 2015; 88(6): 1233–9, with permission from Elsevier) [10]
Suppressor of Cytokine Signaling/Elongin BC
An increase in interleukin (IL)-6 is associated with induction of SOCS3 or SOCS1 expression. These proteins promote insulin resistance by enhancing UPS-mediated degradation of IRS-1 and subsequent reduction in p-Akt. This increase in UPS activity requires SOCS1-mediated induction of E3 ubiquitin ligases that contain Elongin BC-Cullin proteins because when these proteins are mutated, SOCS1-induced ubiquitination of IRS1 is prevented, hence suppressing IRS1 degradation [25, 26]. Expression of SOCS3 and Stat3, a transcription factor in the IL6 signaling cascade, was increased in muscle biopsies from obese patients with type 2 diabetes, suggesting these mechanisms can be relevant in patients with insulin resistance [27].
Casitas B-Lineage Lymphoma B/MG53
In mice, a high-sucrose and/or a high-fat diet (HFD) increases levels of carbohydrate-responsive element-binding protein (ChREBP) and binding of the sterol regulatory element protein 1c (SREBP1c) which stimulate myostatin expression. Myostatin production leads to IRS1 degradation via up-regulation of the Casitas B-lineage lymphoma B (Cb1b) protein which in mice exhibits properties of an E3 ubiquitin ligase [28]. MG53 is another E3 ubiquitin ligase, and it is up-regulated in animal models of obesity, hypertension, and metabolic syndrome or while on a HFD. Mice lacking the ability to express Cb1b or MG53 ameliorated insulin resistance even while on HFD or high-sucrose diet [29,30,31].
Metabolic Abnormalities in CKD-Induced Insulin Resistance
Inflammation and Oxidative Stress
The state of heightened inflammation in CKD can promote insulin resistance by several mechanisms. Inflammatory conditions, which are characterized by activation of NFκB, regulate expression of SIRPα which decreases Akt phosphorylation and in turn leads to insulin resistance [11••]. CKD is associated with elevated levels of pro-inflammatory cytokines (e.g., tumor necrosis factor alpha (TNF-α), IL-6, and IFN-gamma), which are associated with an increase in insulin resistance and higher rates of cardiovascular disease and mortality, even with near normal serum creatinine in early CKD [5, 32, 33]. In vitro studies support these findings. In human skeletal muscle cells, TNF-α induced insulin resistance [34] and indirectly generated free fatty acids (FFA) suggesting enhanced lipolysis, while inhibiting IRS1 via increased intracellular diacylglycerol (DAG) and long-chain acyl-coenzyme A (LCA-CoA) [35]. IL-6 promoted insulin resistance by inducing expression of SOCS-3 or SOCS-1, either of which can inhibit IRS-1binding to the insulin receptor via STAT3 signaling [36] as well as enhanced ubiquitin-mediated degradation of IRS-1 [37]. Oxidative stress can contribute to the development of insulin resistance in CKD in presence of increased circulating fibrinogen, C-reactive protein (CRP), TNF-α, and IL-6 [38,39,40]. High levels of reactive oxygen species (ROS) can reduce tyrosine phosphorylation of IRS1, resulting in decreased insulin signaling [41].
Aldosterone and Angiotensin II
Excessive aldosterone and angiotensin II are commonly observed in CKD and can lead to insulin resistance by several mechanisms. For example, mineralocorticoid receptor activation increases asymmetric dimethyl arginine (ADMA), which impairs insulin signaling in adipocytes of rodents with CKD. Angiotensin II stimulates the expression of IL-6 and serum Amyloid A [42, 43], which increase SOCS3 resulting in reduced IRS1 and impaired insulin signaling. Consistently, angiotensin receptor blockers decrease the expression of inflammatory cytokines and reduce insulin resistance in patients with CKD [44].
Uremic Toxins
Accumulation of urea and uremic toxins may promote insulin resistance. For example, high urea concentrations encourage production of ROS, which in turn promotes modification of intracellular proteins by O-linked beta-N-acetylglucosamine (O-GlcNAc). Increased modification of the mediators in insulin signaling pathway by O-GlcNAcs blunt insulin signaling. Treating uremic mice with antioxidants prevented insulin resistance [8]. Administering p-cresyl sulfate, a uremic solute, to mice with normal kidney function led to insulin resistance, including redistribution of body fat to muscle and liver, and altered insulin signaling in muscle [45]. Furthermore, in animal models of CKD, reducing serum p-cresyl sulfate (by treatment with a prebiotic which reduced its intestinal production) prevented insulin resistance and the resulting dyslipidemia [45].
Metabolic Acidosis
Metabolic acidosis, another common complication of CKD, can also lead to development of insulin resistance. Acidosis promotes detachment of insulin from its receptor, thereby reducing insulin-stimulated intracellular signaling [46]. Treatment with supplemental bicarbonate, or changing the diet to include vegetable and fruit instead of meat, can correct the acidosis and preserve muscle mass and insulin sensitivity while slowing CKD progression [47,48,49].
Potential Treatments for Insulin Resistance in CKD
Lifestyle Modification
Intensive lifestyle modifications reduced progression to diabetes (58% reduction in 2.8 years) in people with impaired glucose tolerance in the Diabetes Prevention Program (DPP) [50]. These modifications consisted of intentional loss of at least 7% of original body weight using a healthy, low-calorie and low-fat diet and moderate physical activity for at least 150 min per week [50]. This impressive improvement even exceeded that observed by treatment with metformin and lasted in long-term follow-up of this cohort (27% reduction after 15 years of follow-up) [51••].
Metformin
Metformin is a known insulin sensitizer with its main site of action in the liver. It has been associated with improved body composition and stabilization of body mass index (BMI) [52]. Treatment with metformin reduced progression to diabetes in the DPP study (31 and 18% reduction after 2.8 and 15 years of follow-up) [50, 51••]. In addition, a recent systematic review found metformin use in patients with moderate CKD, congestive heart failure, and chronic liver disease conferred a 33% reduction in all-cause mortality [53]. The US Food and Drug Administration (FDA) recently relaxed its restriction for use of metformin in patients with CKD [54]. Thus, randomized trials maybe warranted to examine the impact of metformin on renal and cardiovascular outcomes as well as mortality in patients with CKD.
Glucagon-Like Peptide-1 Receptor Agonists
Glucagon-like peptide (GLP) agonists, or the incretin mimetics, enhance glucose-dependent insulin secretion, slow gastric emptying, and reduce postprandial glucagon and food intake. Liraglutide improves cardiovascular and microvascular outcomes, including kidney disease, in people with diabetes [55•]. Glucagon-like peptide-1 receptor (GLP1) agonists improve insulin resistance in animal models [56]. However, their impact on insulin resistance and its contribution to improved renal and cardiovascular outcomes have been not examined in human trials.
SGLT2 Inhibitor
Sodium-glucose cotransporter 2 (SGLT2) inhibitors are a novel class of oral diabetic agents which function by reducing renal glucose reabsorption. The SGLT2 inhibitors empagliflozin and canagliflozin slowed CKD progression and improved cardiovascular outcomes in people with diabetes and kidney disease [14••, 57••, 58••]. Interestingly canagliflozin improves muscle-specific insulin sensitivity in Zucker diabetic rats [15•]. Furthermore, in small trials, SGLT2 inhibitors enhance insulin sensitivity in people with diabetes, [59•, 60] an observation which is physiologically consistent with the calorie deficit and the resulting weight loss caused by this class of medications. However, the effect of SGLT2 inhibitors on insulin resistance has not been examined in patients with nondiabetic CKD.
Thiazolidinediones
The thiazolidinediones (TZDs) improve glucose tolerance by enhancing insulin sensitivity. Use of rosiglitazone has been complicated with an increase in heart failure. However, pioglitazone use is associated with significant protection from micro- and macrovascular complications. Specifically, the Insulin Resistance Intervention after Stroke (IRIS) trial examined the use of pioglitazone in nondiabetic, high-risk patients after an ischemic stroke or TIA [61••]. In patients with insulin resistance, defined as a HOMA-IR score of > 3.0, treatment with pioglitazone reduced subsequent stroke and acute coronary syndrome [62••]. Finally, in the PROspective pioglitAzone Clinical Trial In macroVascular Events (PROactive) trial pioglitazone-treated CKD patients were less likely to reach a composite end points of all-cause mortality, MI, and stroke, independent of the severity of renal impairment [63]. Future trials are required to assess the impact of pioglitazone on insulin resistance and renal outcomes.
Conclusions
Many CKD complications (e.g., inflammation/oxidative stress, renin angiotensin aldosterone pathway activation, uremic toxins, and metabolic acidosis) can lead to insulin resistance. Several of these anomalies may stimulate insulin resistance via similar mechanisms, for example overexpression of SIRPα, a mediator of insulin signaling in skeletal muscles. Results of recent clinical trials have shown evidence that insulin resistance can be modified and that this may lead to improvements in adverse outcomes of CKD. Promising avenues of treatment include intensive lifestyle modification, metformin, and TZDs as well as the newer diabetes agents such as GLP1 agonists and SGLT2 inhibitors. Future studies are needed to identify optimal approaches for diagnosis and treatment of insulin resistance in CKD, even in absence of diabetes.
References
Papers of particular interest, published recently, have been highlighted as: •Of importance ••Of major importance
Huang CX, Tighiouart H, Beddhu S, Cheung AK, Dwyer JT, Eknoyan G, et al. Both low muscle mass and low fat are associated with higher all-cause mortality in hemodialysis patients. Kidney Int. 2010;77(7):624–9.
Shinohara K, Shoji T, Emoto M, Tahara H, Koyama H, Ishimura E, et al. Insulin resistance as an independent predictor of cardiovascular mortality in patients with end-stage renal disease. J Am Soc Nephrol. 2002;13(7):1894–900.
Becker B, Kronenberg F, Kielstein JT, Haller H, Morath C, Ritz E, et al. Renal insulin resistance syndrome, adiponectin and cardiovascular events in patients with kidney disease: the mild and moderate kidney disease study. J Am Soc Nephrol. 2005;16(4):1091–8.
DeFronzo RA, Alvestrand A, Smith D, Hendler R, Hendler E, Wahren J. Insulin resistance in uremia. J Clin Invest. 1981;67(2):563–8.
Fliser D, Pacini G, Engelleiter R, Kautzky-Willer A, Prager R, Franek E, et al. Insulin resistance and hyperinsulinemia are already present in patients with incipient renal disease. Kidney Int. 1998;53(5):1343–7.
Jia T, Huang X, Qureshi AR, Xu H, Ärnlöv J, Lindholm B, et al. Validation of insulin sensitivity surrogate indices and prediction of clinical outcomes in individuals with and without impaired renal function. Kidney Int. 2014;86(2):383–91.
Niwa T, Tsukushi S, Ise M, Miyazaki T, Tsubakihara Y, Owada A, et al. Indoxyl sulfate and progression of renal failure: effects of a low-protein diet and oral sorbent on indoxyl sulfate production in uremic rats and undialyzed uremic patients. Miner Electrolyte Metab. 1997;23(3–6):179–84.
D'Apolito M, Du X, Zong H, et al. Urea-induced ROS generation causes insulin resistance in mice with chronic renal failure. J Clin Invest. 2010;120(1):203–13.
Rigalleau V, Blanchetier V, Combe C, Guillot C, Deleris G, Aubertin J, et al. A low-protein diet improves insulin sensitivity of endogenous glucose production in predialytic uremic patients. Am J Clin Nutr. 1997;65(5):1512–6.
Thomas SS, Zhang L, Mitch WE. Molecular mechanisms of insulin resistance in chronic kidney disease. Kidney Int. 2015;88(6):1233–9.
•• Thomas SS, Dong Y, Zhang L, Mitch WE. Signal regulatory protein-alpha interacts with the insulin receptor contributing to muscle wasting in chronic kidney disease. Kidney Int. 2013;84(2):308–16. This study evaluates how SIRPα causes impaired insulin signaling by tyrosine dephosphorylating insulin receptor and IRS1.
Bailey JL, Wang X, England BK, Price SR, Ding X, Mitch WE. The acidosis of chronic renal failure activates muscle proteolysis in rats by augmenting transcription of genes encoding proteins of the ATP-dependent ubiquitin-proteasome pathway. J Clin Invest. 1996;97(6):1447–53.
Ding H, Gao XL, Hirschberg R, Vadgama JV, Kopple JD. Impaired actions of insulin-like growth factor 1 on protein synthesis and degradation in skeletal muscle of rats with chronic renal failure. Evidence for a postreceptor defect. J Clin Invest. 1996;97(4):1064–75.
•• Zinman B, Lachin JM, Inzucchi SE. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2016;374(11):1094. Patients with type 2 diabetes at high risk for cardiovascular events who received empagliflozin, as compared with placebo, had a lower rate of the primary composite cardiovascular outcome and of death from any cause when the study drug was added to standard care.
• O'Brien TP, Jenkins EC, Estes SK, et al. Correcting postprandial hyperglycemia in Zucker diabetic fatty rats with an SGLT2 inhibitor restores glucose effectiveness in the liver and reduces insulin resistance in skeletal muscle. Diabetes. 2017;66(5):1172–84. SGLT2-I treatment improves impaired glucose effectiveness in the liver and insulin sensitivity in muscle.
Kaku K, Watada H, Iwamoto Y, et al. Efficacy and safety of monotherapy with the novel sodium/glucose cotransporter-2 inhibitor tofogliflozin in Japanese patients with type 2 diabetes mellitus: a combined phase 2 and 3 randomized, placebo-controlled, double-blind, parallel-group comparative study. Cardiovasc Diabetol. 2014;13:65.
Goodarzi MO, Cui J, Chen YD, Hsueh WA, Guo X, Rotter JI. Fasting insulin reflects heterogeneous physiological processes: role of insulin clearance. Am J Physiol Endocrinol Metab. 2011;301(2):E402–8.
Pham H, Utzschneider KM, de Boer IH. Measurement of insulin resistance in chronic kidney disease. Curr Opin Nephrol Hypertens. 2011;20(6):640–6.
Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22(9):1462–70.
Stumvoll M, Mitrakou A, Pimenta W, Jenssen T, Yki-Jarvinen H, van Haeften T, et al. Use of the oral glucose tolerance test to assess insulin release and insulin sensitivity. Diabetes Care. 2000;23(3):295–301.
Avignon A, Boegner C, Mariano-Goulart D, Colette C, Monnier L. Assessment of insulin sensitivity from plasma insulin and glucose in the fasting or post oral glucose-load state. Int J Obes Relat Metab Disord. 1999;23(5):512–7.
Mari A, Pacini G, Murphy E, Ludvik B, Nolan JJ. A model-based method for assessing insulin sensitivity from the oral glucose tolerance test. Diabetes Care. 2001;24(3):539–48.
Gutt M, Davis CL, Spitzer SB, Llabre MM, Kumar M, Czarnecki EM, et al. Validation of the insulin sensitivity index (ISI(0,120)): comparison with other measures. Diabetes Res Clin Pract. 2000;47(3):177–84.
Belfiore F, Iannello S, Volpicelli G. Insulin sensitivity indices calculated from basal and OGTT-induced insulin, glucose, and FFA levels. Mol Genet Metab. 1998;63(2):134–41.
Rui L, Fisher TL, Thomas J, White MF. Regulation of insulin/insulin-like growth factor-1 signaling by proteasome-mediated degradation of insulin receptor substrate-2. J Biol Chem. 2001;276(43):40362–7.
Rui L, Yuan M, Frantz D, Shoelson S, White MF. SOCS-1 and SOCS-3 block insulin signaling by ubiquitin-mediated degradation of IRS1 and IRS2. J Biol Chem. 2002;277(44):42394–8.
Mashili F, Chibalin AV, Krook A, Zierath JR. Constitutive STAT3 phosphorylation contributes to skeletal muscle insulin resistance in type 2 diabetes. Diabetes. 2013;62(2):457–65.
Bonala S, Lokireddy S, McFarlane C, Patnam S, Sharma M, Kambadur R. Myostatin induces insulin resistance via Casitas B-lineage lymphoma b (Cblb)-mediated degradation of insulin receptor substrate 1 (IRS1) protein in response to high calorie diet intake. J Biol Chem. 2014;289(11):7654–70.
Molero JC, Jensen TE, Withers PC, Couzens M, Herzog H, Thien CBF, et al. c-Cbl-deficient mice have reduced adiposity, higher energy expenditure, and improved peripheral insulin action. J Clin Invest. 2004;114(9):1326–33.
Molero JC, Waring SG, Cooper A, Turner N, Laybutt R, Cooney GJ, et al. Casitas b-lineage lymphoma-deficient mice are protected against high-fat diet-induced obesity and insulin resistance. Diabetes. 2006;55(3):708–15.
Yi JS, Park JS, Ham YM, et al. MG53-induced IRS-1 ubiquitination negatively regulates skeletal myogenesis and insulin signalling. Nat Commun. 2013;4:2354.
Shoelson SE, Lee J, Goldfine AB. Inflammation and insulin resistance. J Clin Invest. 2006;116(7):1793–801.
Meuwese CL, Snaedal S, Halbesma N, Stenvinkel P, Dekker FW, Qureshi AR, et al. Trimestral variations of C-reactive protein, interleukin-6 and tumour necrosis factor-alpha are similarly associated with survival in haemodialysis patients. Nephrol Dial Transplant. 2011;26(4):1313–8.
Kanety H, Feinstein R, Papa MZ, Hemi R, Karasik A. Tumor necrosis factor alpha-induced phosphorylation of insulin receptor substrate-1 (IRS-1). Possible mechanism for suppression of insulin-stimulated tyrosine phosphorylation of IRS-1. J Biol Chem. 1995;270(40):23780–4.
Plomgaard P, Fischer CP, Ibfelt T, Pedersen BK, van Hall G. Tumor necrosis factor-alpha modulates human in vivo lipolysis. J Clin Endocrinol Metab. 2008;93(2):543–9.
Rieusset J, Bouzakri K, Chevillotte E, Ricard N, Jacquet D, Bastard JP, et al. Suppressor of cytokine signaling 3 expression and insulin resistance in skeletal muscle of obese and type 2 diabetic patients. Diabetes. 2004;53(9):2232–41.
Rudich A, Tirosh A, Potashnik R, Hemi R, Kanety H, Bashan N. Prolonged oxidative stress impairs insulin-induced GLUT4 translocation in 3T3-L1 adipocytes. Diabetes. 1998;47(10):1562–9.
Borazan A, Binici DN. Relationship between insulin resistance and inflammation markers in hemodialysis patients. Ren Fail. 2010;32(2):198–202.
Kursat S, Colak HB, Toraman A, Tekce H, Ulman C, Bayturan O. Relationship of insulin resistance in chronic haemodialysis patients with inflammatory indicators, malnutrition, echocardiographic parameters and 24 hour ambulatory blood pressure monitoring. Scand J Urol Nephrol. 2010;44(4):257–64.
Martins C, Mazza do Nascimento M, Pecoits-Filho R, et al. Insulin resistance is associated with circulating fibrinogen levels in nondiabetic patients receiving peritoneal dialysis. J Ren Nutr. 2007;17(2):132–7.
Wright VP, Reiser PJ, Clanton TL. Redox modulation of global phosphatase activity and protein phosphorylation in intact skeletal muscle. J Physiol. 2009;587(Pt 23):5767–81.
Zhang L, Du J, Hu Z, et al. IL-6 and serum amyloid A synergy mediates angiotensin II-induced muscle wasting. J Am Soc Nephrol. 2009;20(3):604–12.
Song YH, Li Y, Du J, Mitch WE, Rosenthal N, Delafontaine P. Muscle-specific expression of IGF-1 blocks angiotensin II-induced skeletal muscle wasting. J Clin Invest. 2005;115(2):451–8.
de Vinuesa SG, Goicoechea M, Kanter J, Puerta M, Cachofeiro V, Lahera V, et al. Insulin resistance, inflammatory biomarkers, and adipokines in patients with chronic kidney disease: effects of angiotensin II blockade. J Am Soc Nephrol. 2006;17(12 Suppl 3):S206–12.
Koppe L, Pillon NJ, Vella RE, Croze ML, Pelletier CC, Chambert S, et al. p-Cresyl sulfate promotes insulin resistance associated with CKD. J Am Soc Nephrol. 2013;24(1):88–99.
Marshall S, Podlecki DA, Olefsky JM. Low pH accelerates dissociation of receptor-bound insulin. Endocrinology. 1983;113(1):37–42.
de Brito-Ashurst I, Varagunam M, Raftery MJ, Yaqoob MM. Bicarbonate supplementation slows progression of CKD and improves nutritional status. J Am Soc Nephrol. 2009;20(9):2075–84.
Phisitkul S, Khanna A, Simoni J, Broglio K, Sheather S, Hasan Rajab M, et al. Amelioration of metabolic acidosis in patients with low GFR reduced kidney endothelin production and kidney injury, and better preserved GFR. Kidney Int. 2010;77(7):617–23.
Mahajan A, Simoni J, Sheather SJ, Broglio KR, Rajab MH, Wesson DE. Daily oral sodium bicarbonate preserves glomerular filtration rate by slowing its decline in early hypertensive nephropathy. Kidney Int. 2010;78(3):303–9.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403.
•• Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol. 2015;3(11):866–75. The DPP trial determined that lifestyle intervention or metformin significantly reduced diabetes development over 15 years without an overall difference in the aggregate microvascular outcomes among treatment groups.
van der Aa MP, Elst MA, van de Garde EM, van Mil EG, Knibbe CA, van der Vorst MM. Long-term treatment with metformin in obese, insulin-resistant adolescents: results of a randomized double-blinded placebo-controlled trial. Nutr Diabetes. 2016;6(8):e228.
Crowley MJ, Diamantidis CJ, McDuffie JR, et al. Clinical outcomes of metformin use in populations with chronic kidney disease, congestive heart failure, or chronic liver disease: a systematic review. Ann Intern Med. 2017;166(3):191–200.
Imam TH. Changes in metformin use in chronic kidney disease. Clin Kidney J. 2017;10(3):301–4.
• Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–22. The rate of the first occurrence of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke among patients with type 2 diabetes mellitus was lower with liraglutide than with placebo.
Yamazaki S, Satoh H, Watanabe T. Liraglutide enhances insulin sensitivity by activating AMP-activated protein kinase in male Wistar rats. Endocrinology. 2014;155(9):3288–301.
•• Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375(4):323–34. In patients with type 2 diabetes at high cardiovascular risk, empagliflozin was associated with slower progression of kidney disease and lower rates of clinically relevant renal events than was placebo when added to standard care.
•• Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57. Canagliflozin had a lower risk of cardiovascular events than those who received placebo but a greater risk of amputation, primarily at the level of the toe or metatarsal.
• Ferrannini E, Muscelli E, Frascerra S, Baldi S, Mari A, Heise T, et al. Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. J Clin Invest. 2014;124(2):499–508. Empagliflozin-induced glycosuria with improved β cell function and insulin sensitivity thereby lowering fasting and postprandial glycemia.
Merovci A, Solis-Herrera C, Daniele G, Eldor R, Fiorentino TV, Tripathy D, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest. 2014;124(2):509–14.
•• Kernan WN, Viscoli CM, Furie KL, Young LH, Inzucchi SE, Gorman M, et al. Pioglitazone after ischemic stroke or transient ischemic attack. N Engl J Med. 2016;374(14):1321–31. In patients with insulin resistance without diabetes plus recent history of stroke or TIA, the risk of stroke or myocardial infarction was lower among patients who received pioglitazone than among those who received placebo. Pioglitazone was also associated with a lower risk of diabetes.
•• Young LH, Viscoli CM, Curtis JP, Inzucchi SE, Schwartz GG, Lovejoy AM, et al. Cardiac outcomes after ischemic stroke or transient ischemic attack: effects of pioglitazone in patients with insulin resistance without diabetes mellitus. Circulation. 2017;135(20):1882–93. Among patients with insulin resistance without diabetes mellitus, pioglitazone reduced the risk for acute coronary syndromes after a recent cerebrovascular event.
Dormandy JA, Charbonnel B, Eckland DJ, et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet. 2005;366(9493):1279–89.
Funding
This review was supported in part by the VA Career Development Award 1IK2 BX002492 to SST from the United States Department of Veterans Affairs, Biomedical Laboratory Research and Development Program. We acknowledge the generous support of Dr. and Mrs. Harold Selzman.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Natasha Dave, Jiao Wu, and Sandhya Thomas declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclosures
Contents of this review do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Additional information
This article is part of the Topical Collection on Microvascular Complications—Nephropathy
Rights and permissions
About this article
Cite this article
Dave, N., Wu, J. & Thomas, S. Chronic Kidney Disease-Induced Insulin Resistance: Current State of the Field. Curr Diab Rep 18, 44 (2018). https://doi.org/10.1007/s11892-018-1010-8
Published:
DOI: https://doi.org/10.1007/s11892-018-1010-8