Abstract
Purpose of Review
This study aims to examine the operationalisation of ‘psychological insulin resistance’ (PIR) among people with type 2 diabetes and to identify and critique relevant measures.
Recent Findings
PIR has been operationalised as (1) the assessment of attitudes or beliefs about insulin therapy and (2) hypothetical or actual resistance, or unwillingness, to use to insulin. Five validated PIR questionnaires were identified. None was fully comprehensive of all aspects of PIR, and the rigour and reporting of questionnaire development and psychometric validation varied considerably between measures.
Summary
Assessment of PIR should focus on the identification of negative and positive attitudes towards insulin use. Actual or hypothetical insulin refusal may be better conceptualised as a potential consequence of PIR, as its assessment overlooks the attitudes that may prevent insulin use. This paper provides guidance on the selection of questionnaires for clinical or research purpose and the development of new, or improvement of existing, questionnaires.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
International guidelines emphasise the early consideration and initiation of insulin therapy among people with type 2 diabetes (T2D) for whom target glycaemic outcomes are not achieved with maximum oral hypoglycaemic agents and/or non-insulin injectables [1, 2]. However, research suggests that both initiation and intensification of insulin are commonly delayed beyond clinical need [3•, 4, 5, 6•, 7,8,9,10]. Causes of delay are multi-faceted, including, for example, healthcare systemic barriers [11, 12] and clinical inertia among healthcare professionals (HCPs) (i.e. delaying recommendation/prescription beyond clinical need) [3•, 13]. Delay may also be due to the person with T2D experiencing a phenomenon known as ‘psychological insulin resistance’ (PIR). Systematic reviews of PIR have synthesised relevant qualitative and quantitative literature over the past two decades, providing an overview of commonly reported barriers to insulin use among people with T2D and known correlates and determinants of PIR [14, 15, 16••, 17]. PIR has been operationalised in various ways, and several tools developed to measure PIR, but no comprehensive review of measurement has been conducted to date. Therefore, we aim to clarify the operationalisation of PIR and to identify and evaluate measures of PIR, in terms of questionnaire design, conceptual focus and psychometric properties, as well as provide recommendations for future research.
Operationalising Psychological Insulin Resistance
In the context of T2D, PIR is commonly defined as a reluctance to use insulin therapy due to negative attitudes (i.e. concerns or fears) about the therapy [14, 15, 18]. PIR has been operationalised in terms resistance to using insulin therapy (1) and attitudes towards insulin therapy (2). The implications of this are discussed in the subsequent sections. In contrast to the vast literature exploring PIR, it has been suggested that ‘receptiveness’ to insulin therapy is a common experience and that the phenomenon of PIR may have been overstated [19]. This poses the question of whether receptiveness to insulin is best conceptualised as acceptance of insulin use, the absence of negative attitudes and/or the presence of positive attitudes towards insulin therapy. These issues are discussed further below.
PIR research has most commonly focused on adults with non-insulin-treated T2D with reference to insulin uptake. However, PIR is not limited to this treatment group and may have explanatory value in relation to ongoing use and resistance to further treatment intensification. For example, among those with insulin-treated T2D, psychological barriers to insulin use have been cited as reasons for self-reported insulin omission [20,21,22] and qualitative research has highlighted negative attitudes towards insulin intensification [19, 23•] and self-titration [24••]. In this review, the measurement of PIR is considered across all stages of treatment progression.
Resistance to Insulin Therapy
The limited data available suggest that 20–43% of people with T2D for whom insulin is recommended refuse it, depending on the support received, the study setting (i.e. clinical trial, real-world cohort study) and population [25,26,27]. Studies investigating insulin refusal typically do so using a proxy measure, i.e. the proportion of people who report being hypothetically (un)willing to initiate insulin, generally assessed using a single-item measure [28,29,30,31,32,33,34,35,36,37]. For example, ‘If your doctor recommended that you start insulin, how willing would you be to take it?’ [30]. Rates of hypothetical ‘unwillingness’ vary considerably across samples, for example, an international study reported 6% of participants in Spain were ‘not at all’ willing to initiate insulin compared to 37% in Italy [30]. For those already using insulin, similar single items have been used to measure willingness to “titrate insulin treatment, if advised” [36] or administer additional injections per day [38].
Utility of a Single-Item Measure
Within a clinical context, a single-item measure may be a practical, quick and easy screening tool to identify people with T2D who face barriers to insulin initiation and may need additional support to promote timely treatment intensification. Indeed, a recent prospective study has demonstrated the predictive validity of this single item in terms of actual insulin uptake: adults with T2D requiring treatment intensification who were hypothetically ‘very willing’ to commence insulin at baseline were six times more likely to be using insulin at follow-up compared to those who were ‘not at all’ [39••]. However, single items have clear psychometric limitations: there is typically no information on their origin or development history, internal consistency reliability cannot be computed for a single item, they are more vulnerable to random measurement errors and there is greater scope than with multi-item measures for ambiguity of interpretation of the meaning of the item.
Furthermore, a single item focused on ‘willingness’ provides no insight into the reasoning behind any resistance and, therefore, no direction for intervention. For clinical and research purposes, identifying and addressing barriers may be equally as important among those who report being willing to use insulin therapy as for those reporting unwillingness. Indeed, receptiveness may be a consequence of several factors (e.g. influence of family and friends [40••], the clinician/patient relationship and decision-making dynamic [41]) and does not necessarily equate to the absence of concerns about insulin, which may impact on treatment transition. Recent research suggests that the ‘necessity-concerns framework’ may have value in explaining acceptance of insulin therapy [40••]. In this framework, people with T2D can concurrently hold both negative and positive attitudes towards insulin, and the decision to use insulin therapy is a negotiation between these attitudes. A focus on resistance or receptiveness alone is not, in itself, a clinically useful operationalisation of PIR. To understand the individual’s reasoning, attitudes to insulin therapy must be investigated.
Attitudes to Insulin Therapy
Qualitative research [15,16,17] has identified numerous psychological barriers to insulin therapy among adults with T2D, including, for example, injection-related anxieties, low self-efficacy, concerns about side-effects (i.e. hypoglycaemia, weight gain), inaccurate health beliefs (e.g. insulin being a cause of long-term diabetes-complications), concern about financial burden of treatment, doubts about the effectiveness or necessity of insulin, concern over apparent diabetes progression and feelings of personal failure, concerns about the impact of treatment on social relationships and freedom and flexibility and perceived diabetes stigma. Studies have also identified more general barriers related to religious and cultural norms and values. For example, a distrust of Western medicine [42, 43], a strong sense of fatalism or stronger reliance on faith than medicine [27, 44] and influence of community and family values in decision-making [45].
Over the past decade, there has been a considerable research focus on developing quantitative measures of these attitudes. Three measures of PIR were published in 2007: the 14-item ‘Barriers to Insulin Treatment’ (BIT) [46], the 20-item ‘Insulin Treatment Appraisal Scale’ (ITAS) [47] and the 14-item ‘Study the Hurdles of Insulin Prescription’ (SHIP) [38]. The ITAS, BIT and SHIP were designed for Western populations, and aspects of PIR assessed may lack cross-cultural relevance. For this reason, the 13-item ‘Chinese Attitudes to Starting Insulin Questionnaire’ (Ch-ASIQ) [48] and the 18-item ‘Korean Psychological Insulin Resistance scale’ (K-PIR) [49] were developed with the aim of producing measures of PIR both culturally and linguistically appropriate to those populations. The development and validation of the K-PIR was published in Korean only, and therefore, a full critical review of this questionnaire is not provided here [49]. Finally, the 22-item ‘Beliefs about Insulin Scale’ (BIS) was published most recently [50••]. Table 1 summarises the development history and psychometrics properties of the five PIR questionnaires published in English-language journals (i.e. BIT, ITAS, SHIP, Ch-ASIQ, BIS), as well as the questionnaire characteristics, e.g. length, subscales, scoring, language availability and subsequent uptake.
In addition, several studies have employed study-specific items or scales to measure attitudes to insulin therapy (e.g. [26•, 29, 30, 34, 63]). These are typically unvalidated with little description of item wording, development process or psychometric properties and are therefore excluded from this review. Finally, a number of other questionnaires are relevant to PIR but either focus too specifically on a single aspect, or domain of, PIR (e.g. fear of self-injecting [64], concerns about hypoglycaemia [24••]), or assess satisfaction with insulin without identifying factors influencing satisfaction (e.g. [65]). These measures are not discussed further.
Conceptual Focus and Content Validity
The process undertaken to develop PIR questionnaires varies considerably (see Table 1). As reported, the development of the ITAS and BIT was informed by literature review and clinical experience. The iterative development and refinement of the SHIP involved a three-phase process including qualitative research with the target groups, subsequent cognitive debriefing of items and a review by an HCP expert panel. In contrast to other measures, the development of the BIS was theoretically driven and the item pool was developed and reviewed by experts to reflect the adopted cognitive-behavioural theoretical framework [50••].
Appendix 1 illustrates the specific aspects of PIR measured by each questionnaire and the conceptual overlap between questionnaires. The themes and sub-themes used to group questionnaire items is based upon the current authors’ subjective interpretation of the published questionnaire wording and informed by recent systematic reviews, which have synthesised qualitative research examining attitudes towards insulin [15,16,17].
The questionnaires have considerable overlap but none are identical in item content, and no single questionnaire assesses all themes, or sub-themes, of PIR identified across the measures. All questionnaires include both positively and negatively worded items, although they are generally imbalanced by a strong negative focus. Typically, positive items refer specifically to the positive consequences of insulin therapy (i.e. treatment efficacy) or facilitators of insulin use (i.e. self-efficacy). In contrast, the positively worded items in the BIS (forming the ‘functional beliefs’ subscale) focus on the acceptance of insulin despite negative perceptions of insulin or include double-negative statements stating that insulin would not have a negative impact on the individual. Therefore, the BIS does not assess positive beliefs about insulin therapy. Furthermore, the BIS appears to be conceptually distinct from other PIR questionnaires. Ten BIS items refer to general negative emotional reactions to insulin use, while no other questionnaire includes negatively worded items that cannot otherwise be categorised to a specific concern about insulin use.
Relevance Across Treatment Groups
The ITAS, SHIP and BIS were designed to be suitable for completion regardless of insulin treatment status. To assess differences in PIR between groups, or changes over time, a balance must be struck between the specificity of items (to a treatment type) and applicability (across treatment types). Items that require knowledge or experience of actual insulin therapy may be of limited relevance to those not yet using insulin. This is evidenced by the ITAS item ‘insulin causes weight gain’, which is one of the only negative items more likely to be endorsed among the those using insulin therapy, compared to those not using insulin [47, 54]. It may be that many people with non-insulin-treated T2D are unaware of the association between insulin therapy and weight gain, and therefore, this issue may not contribute to PIR for them. Similarly, prior to insulin initiation, people with T2D may be unaware of the heightened risk of hypoglycaemia. The BIT two-item fear of hypoglycaemia subscale is preceded by a statement indicating that insulin can lead to ‘extremely low blood glucose levels’, thus allowing for measurement of concern rather than knowledge. However, such ‘scene-setting’ does not feature elsewhere in the BIT, or other questionnaires, and likely increases endorsement of these items among those with T2D who may be otherwise unaware of the possibility of experiencing hypoglycaemia as a side effect of insulin. Indeed, this BIT subscale is typically the most highly endorsed negative subscale [46, 56, 66], while, in ITAS studies, several other negative insulin appraisals are more commonly endorsed than concern about hypoglycaemia among people with non-insulin-treated T2D [47, 54].
Qualitative studies suggest people with insulin-treated T2D perceive multiple daily injections (i.e. >3) and quick-acting insulins as less convenient and indicating worse health than less intensive insulin regimens [23•], potentially contributing to resistance to further treatment intensification. Concerns about self-titrating insulin doses are discussed elsewhere [24••]. However, negative attitudes to specific insulin regimens, insulin intensification or self-titration are not incorporated in the ITAS or BIS, and therefore, these measures may have limited sensitivity in differentiating negative attitudes to insulin intensification, or types of insulin therapy. In contrast, the SHIP includes an item referring specifically to concern that insulin treatment may become more complicated over time and refers specifically to either insulin ‘initiation’ or ‘intensification’ depending on the respondents’ current treatment regimen. However, due to the SHIP’s focus on attitudes towards treatment progression, this measure cannot be used to assess change in attitudes towards insulin in general.
Psychometric Properties
Table 1 details the psychometric validation process employed for each questionnaire, the number of items and subscales in the final questionnaire as well as the reliability, validity and responsiveness of each questionnaire.
All questionnaires were subject to exploratory factor analysis (EFA) to assess scale structure and identify potential items for removal. The SHIP and BIT were subject to the most robust psychometric testing process, including initial factor analysis and item reduction in one dataset, followed by further factor analysis of the final questionnaire and validation testing in a second dataset. Only the BIT was subject to confirmatory factor analysis following questionnaire finalisation. Despite the relatively rigorous approach taken to develop the Ch-ASIQ item pool (see Table 1), less attention was paid to item reduction and examination of scale structure. Following an unforced factor analysis, items were dropped based on single-factor loadings, factors were then manually collapsed (not informed EFA), and dropped where internal consistency was deemed inadequate (α < 0.6). Inspection of eigenvalues suggests a forced three-factor structure warrants investigation (based on the knick-criterion). Further psychometric testing of the Ch-ASIQ should include an iterative item reduction and factor analysis approach.
Multi-dimensional scale structures were reported of all questionnaires (see Table 1). The BIT and the Ch-ASIQ subscales each relate to a specific aspect of PIR (or facilitator of insulin use), such as injection-related anxieties). In contrast, the ITAS and the BIS each encompass just two dimensions including either positive or negative statements about insulin therapy. The SHIP includes one dimension focused around positive expectations and facilitators of insulin use, but concerns about insulin are split across two dimensions. An underlying single-factor structure was investigated for the BIT and ITAS, and total scores have been recommended for use. More recent research has replicated the two-factor structure of the ITAS, but discouraged the use of the total score [54].
For questionnaires suitable for use regardless of insulin treatment, psychometric properties need to be considered separately by treatment group (insulin-treated and non-insulin-treated). Separate EFA was undertaken by treatment group for the SHIP, but was not reported for the BIS. Original validation of the ITAS did not include separate EFA by treatment group [47] but this has been conducted subsequently and found to be satisfactory [54]. It is of note, however, that the entire ITAS scale was more commonly skipped by participants not using insulin compared to those insulin treated (7 vs. 0%) [54], suggesting this group may have questioned the relevance of the ITAS to their experience. Future researchers using the ITAS with non-insulin-treated populations might consider modifying the instructions to emphasise the questionnaire’s relevance and maximise completion rates.
Known-Groups Validity
It is expected that the experience of PIR differs (qualitatively and quantitatively) between those with insulin and non-insulin-treated T2D, and therefore, PIR questionnaire scores should differ between groups. ITAS total and subscale scores were found to differ significantly by treatment group, whereby greater, more negative, scores were reported among those not using insulin therapy [47]. In subsequent research, inconsistent results have been demonstrated for the ITAS positive score [54, 56,57,58]. BIS dysfunctional beliefs scores were significantly higher among those with non-insulin-treated T2D who had refused insulin treatment compared to those who were currently using insulin. Despite not being developed for use beyond insulin initiation, BIT total and subscale scores differentiated treatment groups (insulin versus non-insulin), with the exception of the ‘positive insulin-related outcomes’ and ‘fear of hypoglycaemia’ subscales [56]. Post-insulin initiation, the SHIP measures attitudes towards insulin intensification, not insulin in general, and therefore, direct comparisons have not be made between treatment groups.
Predictive and Concurrent Validity
PIR is not a clinical diagnosis and thus defining a cut-point on PIR questionnaires is neither necessary nor appropriate. However, given the clinical importance of timely treatment intensification, it is important to establish the utility of PIR questionnaires in predicting actual insulin uptake or intensification (predictive validity) or discriminating between those hypothetically willing and unwilling to commence insulin therapy (concurrent validity). A significant association between hypothetical willingness to begin insulin and attitudes towards insulin was demonstrated in the original validation of the BIT and SHIP [38, 46], and more recently for the BIT [59] and the ITAS [31]. Furthermore, two SHIP domain scores (‘acceptance and motivation’ and ‘constraints and fears’) were found to predict willingness to intensify insulin among people with insulin-treated diabetes.
The predictive validity of the SHIP was examined with regard to actual insulin initiation and intensification. Two of the three domains (‘acceptance and motivation’ and ‘constraints and fears’) adequately predicted insulin initiation, but none were predictive of intensification of insulin. Recently, prospective research has demonstrated that ITAS negative and positive scores contribute significantly to the prediction of insulin uptake [39••], and more negative BIT total scores among adults with newly diagnosed T2D are associated with a longer time to insulin initiation [60].
Sensitivity to Change
Longitudinal research has demonstrated significant improvements in ITAS total and negative scores following insulin initiation, but inconsistent change in ITAS positive scores [39••, 58, 62]. No prospective research has examined change in BIS or SHIP scores following insulin initiation or intensification. The responsiveness of the ITAS and BIT to change in insulin administration (from insulin injections to novel patch-on insulin delivery) was examined in a small (N = 18), 2-week single-arm study [61•]. Strong significant change in BIT total scores was observed and non-significant changes, with a moderate effect size, were observed for ITAS scores. Given the apparent responsiveness of the BIT among those using insulin therapy, further research may be warranted in this population.
Practical Considerations
In addition to the conceptual focus, development rigour and psychometric properties, researchers/clinicians need also to consider questionnaire characteristics that affect access and use, e.g. length, language availability, readability and ease of scoring (see Table 1). All five PIR questionnaires discussed here are relatively brief (range 13 to 22 items) and may be completed in a few minutes. Questionnaire scoring is not onerous, involving either computing a sum or mean of item responses. The ITAS is the most widely translated questionnaire, having been developed in English [47] and subsequently translated for use in Turkish [53], Romanian [32] and Chinese [51, 52] populations. However, translations may not have been subject to linguistic or psychometric validation, and the ITAS two-dimensional scale structure was not supported within a Hong Kong sample [51]. English translations (involving forward/backward translation and review) are available for the BIT [46], originally developed in German, and the Ch-ASIQ [48]. A direct English translation of the Romanian BIS and an English summary version of the French SHIP are published, but full cultural and linguistic validation has not been conducted. Beyond translation, the cultural appropriateness of a scale needs also to be considered. Thus, while the ITAS has a strong development and validation history and is recommended for most applications, the attitudes towards insulin assessed may not comprehensively represent the experience of PIR in non-western countries or cultural groups [48].
Choice of measure may also be influenced by the frequency of prior use, which may provide a context for research extension and cross-study comparisons. The ITAS is the most commonly used PIR questionnaire in published empirical research to date, followed by the BIT (see Table 1). Despite being published in the same year as the ITAS and BIT, the SHIP has not been used subsequently in published research to our knowledge.
Directions for Future Research
Following critical review of the available validated PIR measures, directions for future research and scale improvement are apparent. Positive attitudes towards insulin use are associated with intention to begin insulin therapy [38, 46], independent of negative attitudes [31]. This is consistent with the recent proposition of the utility of the ‘necessity-concerns framework’ in understanding the decision-making process to initiate insulin therapy [40••]. However, across PIR questionnaires, few items assess positive perceptions of insulin therapy, relative to negative attitudes. For example, the ITAS includes four positive items, compared to 16 negative items. Furthermore, positive items commonly refer to knowledge of physiological benefits (e.g. ITAS: ‘maintain good control of blood glucose’, BIT: ‘prevent long-term complications’), which could be applied to any pharmacological treatment of diabetes, rather than to the consequences of insulin specifically. Qualitative studies have identified other, more specific, benefits of insulin therapy, including increased dietary flexibility due to the ability to adjust insulin (assessed in the SHIP), feeling more positive about health in general, relief over the ease of using insulin devices/injecting and insulin use fostering personal control over diabetes [23•, 67, 68]. PIR questionnaires may benefit from revision, with the development and testing of new positive items referring to additional, and perhaps more immediately salient, benefits. Additional items may also improve the ability of positive subscales to discriminate between treatment groups [54, 56, 58] and the responsiveness of positive subscales [39••, 58, 61•].
The impact of PIR beyond insulin initiation has received little research attention. No research has examined the association between PIR and insulin omission using validated questionnaires and a recent review article called for further research to examine the relationship between PIR and intensification of insulin [69]. The SHIP was designed specifically to assess barriers to insulin intensification (in addition to initiation), but the predictive validity of this measure with regard to insulin intensification was not supported, and little research has since examined the relationship between PIR and insulin intensification. PIR questionnaires may not adequately assess concerns about specific insulin regimens and types of insulin, which have been identified in qualitative literature [23•, 41]. Research is warranted to investigate, and optimise, the predictive validity of PIR measures in relation to optimal insulin-taking behaviours and insulin intensification.
Finally, the responsiveness of BIT and ITAS has been demonstrated following change in diabetes treatment [39••, 58, 61•]. However, the sensitivity of scales in response to intervention aimed to reduce PIR or clinical counselling is unknown, as few interventions have been designed to reduce PIR [70, 71], and their impact has not been evaluated using validated PIR measures. Furthermore, PIR questionnaires may provide a foundation for the future development of tailored PIR interventions. This is an area for future research.
Implications for Clinical Practice
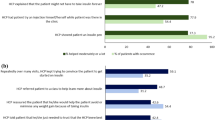
Research suggests that HCPs have pre-conceived ideas about the willingness of people with non-insulin-treated T2D to begin insulin therapy and anticipate negative emotional reactions [12, 72, 73]. In clinical practice, the question of willingness to begin insulin may be perceived as confrontational and blunt by the person with T2D, whose negative response may then discourage the HCP in the timely initiation of insulin therapy. In contrast, exploring attitudes towards insulin use may assist HCPs in providing practical support to increase receptiveness to insulin therapy (i.e. education, problem-solving, practical skills) and assist the person with T2D to make an informed treatment decision. A practical guide on how to have such an open-ended discussion about PIR has been described elsewhere [74•].
The completion of a relatively brief PIR questionnaire within or prior to the consultation may help to identify the most salient barriers and guide discussion. Alternatively, where the possibility of questionnaire completion is limited by consultation times, language availability or literacy skills, HCPs might choose to use PIR questionnaires as a checklist to guide clinical discussions around insulin therapy. The BIS was designed specifically, but not yet tested, to identify beliefs that may be addressed clinically using empirically validated cognitive-behavioural strategies. Other PIR measures identify practical barriers to insulin use, which would be more easily addressed within clinical care, rather than requiring psychological intervention. The ITAS has a strong development and validation history and is widely used and has the advantage over many other PIR measures of being suitable for use before and after insulin initiation. However, HCPs should be mindful that the use of any single PIR questionnaire within care may limit discussion to the barriers included in that specific measure. As shown in Appendix 1, no questionnaire is inclusive of all identified aspects of PIR across questionnaires, and still other barriers to insulin use may exist.
Conclusion
PIR has been defined and operationalised in terms of psychological barriers to insulin use among people with T2D, which may lead to refusal of insulin initiation or intensification. The measurement of actual or hypothetical insulin refusal offers insight into the extent of one potential impact of PIR, but ignores factors that may prevent or encourage insulin use. Furthermore, focusing on willingness to initiate/intensity insulin overlooks the potential impact of ongoing concerns about insulin therapy on daily self-care behaviours. For this reason, it is recommended that PIR measurement focuses on exploring attitudes to insulin therapy rather than simply on insulin refusal. In this review, six validated measures of PIR were identified, five of which are published in English-language, peer-reviewed journals. Choice of measures needs to be guided by the clinical or research aim, taking into consideration the sample (i.e. linguistic and cultural validity), clinical time point (i.e. identifying barriers to insulin initiation, ongoing use, or intensification) and the contextual face validity of PIR questionnaires relative to clinical/research interest, in addition to the psychometric strengths and limitations described above. For most clinical and research applications in Western countries, the ITAS appears to have the strongest basis for recommendation. As well as barriers, perceived benefits or facilitators of insulin therapy are associated independently with intention to begin/intensify insulin therapy and may warrant more comprehensive assessment (for example, only 4/20 ITAS items are positive). The development and testing of additional positive items is indicated by qualitative research findings. Further research is needed to assess the clinical utility of PIR questionnaires to assist HCPs in identifying and addressing perceived barriers of insulin therapy, as well as the responsiveness of these questionnaires to clinical intervention.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance ••Of major importance
Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38(1):140–9.
Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2009;32(1):193–203.
• Khunti S, Davies MJ, Khunti K. Clinical inertia in the management of type 2 diabetes mellitus: a focused literature review. British Journal of Diabetes & Vascular Disease. 2015;15(2):65–9. Recent literature review providing useful overview of the problem of clinical inertia in type 2 diabetes.
Harris SB, Kapor J, Lank CN, Willan AR, Houston T. Clinical inertia in patients with T2DM requiring insulin in family practice. Can Fam Physician. 2010;56(12):e418–e24.
Blak BT, Smith HT, Hards M, Maguire A, Gimeno V. A retrospective database study of insulin initiation in patients with type 2 diabetes in UK primary care. Diabet Med. 2012;29(8):e191–e8. doi:10.1111/j.1464-5491.2012.03694.x.
• Khunti K, Nikolajsen A, Thorsted BL, Andersen M, Davies MJ, Paul SK. Clinical inertia with regard to intensifying therapy in people with type 2 diabetes treated with basal insulin. Diabetes Obesity Metab. 2016;18(4):401–9. doi:10.1111/dom.1 26. Large-scale retrospecitve study highlighting the clinical delay of insulin intensification among people with insulin-treated type 2 diabetes.
Khunti K, Wolden ML, Thorsted BL, Andersen M, Davies MJ. Clinical inertia in people with type 2 diabetes: a retrospective cohort study of more than 80,000 people. Diabetes Care. 2013;36(11):3411. doi:10.2337/dc13-0331.
Khunti K, Damci T, Meneghini L, Pan CY, Yale JF. Study of once daily Levemir (SOLVE™): insights into the timing of insulin initiation in people with poorly controlled type 2 diabetes in routine clinical practice. Diabetes Obes Metab. 2012;14(7):654–61.
Fulcher G, Roberts A, Sinha A, Proietto J. What happens when patients require intensification from basal insulin? A retrospective audit of clinical practice for the treatment of type 2 diabetes from four Australian centres. Diabetes Res Clin Pract. 2015;108(3):405–13.
Grant RW, Buse JB, Meigs JB. Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change. Diabetes Care. 2005;28(2):337–442.
Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract. 2011;93(1):1–9.
Furler J, Spitzer O, Young D, Best J. Insulin in general practice: barriers and enablers for timely initiation. Aust Fam Physician. 2011;40(8):617–21.
Shaefer CF Jr. Clinical inertia: overcoming a major barrier to diabetes management. Insulin. 2006;1(2):61–4.
Gherman A, Veresiu I, Sassu R, Schnur J, Scheckner B, Montgomery G. Psychological insulin resistance: a critical review of the literature. Practical Diabetes International. 2011;28(3):125–8d.
Brod M, Kongsø JH, Lessard S, Christensen TL. Psychological insulin resistance: patient beliefs and implications for diabetes management. Qual Life Res. 2009;18(1):23–32. doi:10.1007/s11136-008-9419-1.
•• Ng CJ, Lai PSM, Lee YK, Azmi SA, Teo CH. Barriers and facilitators to starting insulin in patients with type 2 diabetes: a systematic review. Int J Clin Pract. 2015;69(10):1050–70. doi:10.1111/ijcp.12691. Recent mixed-methods systematic review of barriers and facilitators of insulin initiation among people with type 2 diabetes.
Wang HF, Yeh MC. Psychological resistance to insulin therapy in adults with type 2 diabetes: mixed-method systematic review. J Adv Nurs. 2012;68(4):743–57.
Leslie CA, Satin-Rapaport W, Matheson D, Stone R, Enfield G. Psychological insulin resistance: a missed diagnosis. Diabetes Spectrum. 1994;7(1):52–7.
Jenkins N, Hallowell N, Farmer AJ, Holman RR, Lawton J. Initiating insulin as part of the treating to target in type 2 diabetes (4-T) trial: an interview study of patients’ and health professionals’ experiences. Diabetes Care. 2010;33(10):2178–80.
Peyrot M, Rubin RR, Kruger DF, Travis LB. Correlates of insulin injection omission. Diabetes Care. 2010;33(2):240–5.
Davies MJ, Gagliardino JJ, Gray LJ, Khunti K, Mohan V, Hughes R. Real-world factors affecting adherence to insulin therapy in patients with type 1 or type 2 diabetes mellitus: a systematic review. Diabet Med. 2013;30(5):512–24. doi:10.1111/dme.12128.
Peyrot M, Barnett AH, Meneghini LF, Schumm-Draeger PM. Insulin adherence behaviours and barriers in the multinational global attitudes of patients and physicians in insulin therapy study. Diabet Med. 2012;29(5):682–9.
• Holmes-Truscott E, Browne JL, Speight J. The impact of insulin therapy and attitudes towards insulin intensification among adults with type 2 diabetes: a qualitative study. J Diabetes Complicat. 2016;30(6):1151–7. doi:10.1016/j.jdiacomp.2016.03.027. One of the first real-world qualitative studies examining attitudes to insulin intensification among people with type 2 diabetes.
•• McBain H, Begum S, Rahman S, Mulligan K. Barriers to and enablers of insulin self-titration in adults with type 2 diabetes: a qualitative study. Diabet Med. 2016; doi:10.1111/dme.13196. First in-depth qualitative exploration of perceived barriers to and enablers of self-titration among people with type 2 diabetes.
UKPDS. Relative efficacy of randomly allocated diet, sulphonylurea, insulin, or metformin in patients with newly diagnosed non-insulin dependent diabetes followed for three years (UKPDS 13). BMJ. 1995;310(6972):83–8.
• Odawara M, Ishii H, Tajima N, Iwamoto Y. Impact of patient attitudes and beliefs to insulin therapy upon initiation, and their attitudinal changes after initiation: the DAWN JAPAN study. Curr Med Res Opin. 2016;32(4):681–6. This articles describes, for the first time, the prospective association between attitudes towards insulin and actual insulin uptake in type 2 diabetes.
Khan H, Lasker SS, Chowdhury TA. Prevalence and reasons for insulin refusal in Bangladeshi patients with poorly controlled type 2 diabetes in East London. Diabet Med. 2008;25(9):1108–11.
Polonsky WH, Fisher L, Dowe S, Edelman SV. Why do patients resist insulin therapy? [Abstract]. Diabetes. 2003;52(SUPPLEMENT(1)):A417.
Polonsky WH, Fisher L, Guzman S, Villa-Caballero L, Edelman SV. Psychological insulin resistance in patients with type 2 diabetes: the scope of the problem. Diabetes Care. 2005;28(10):2543–5.
Polonsky WH, TRS H, Dain MP, Snoek FJ. Are patients with type 2 diabetes reluctant to start insulin therapy? An examination of the scope and underpinnings of psychological insulin resistance in a large, international population. Curr Med Res Opin. 2011;27(6):1169–74.
Holmes-Truscott E, Blackberry I, O’Neal DN, Furler J, Speight J. Willingness to initiate insulin among adults with type 2 diabetes in Australian primary care: results from the Stepping Up Study. Diabetes Res Clin Pract. 2016;114:126–35.
Gherman A, Alionescu A. Depression and Dysfunctional beliefs. Predictors of negative appraisal of insulin treatment. Journal of Evidence-Based Psychotherapies. 2015;15(2):207.
Larkin ME, Capasso VA, Chen CL, Mahoney EK, Hazard B, Cagliero E, et al. Measuring psychological insulin resistance: barriers to insulin use. Diabetes Educ. 2008;34(3):511–7.
Wong S, Lee J, Ko Y, Chong MF, Lam CK, Tang WE. Perceptions of insulin therapy amongst Asian patients with diabetes in Singapore. Diabet Med. 2011;28(2):206–11.
Nur Azmiah Z, Zulkarnain AK, Tahir A. Psychological insulin resistance (PIR) among type 2 diabetes patients at public health clinics in federal territory of Malaysia. Int Med J Malaysia. 2011;10(2):7–12.
Lee KP. Psychological factors associated with psychosocial insulin resistance in primary care patients in Hong Kong. Journal of Clinical and Translational Endocrinology. 2015;2(4):157–62.
Woudenberg YJC, Lucas C, Latour C, Scholte op Reimer WJM. Acceptance of insulin therapy: a long shot? Psychological insulin resistance in primary care. Diabet Med. 2012;29(6):796–802. doi:10.1111/j.1464-5491.2011.03552.x.
Martinez L, Consoli SM, Monnier L, Simon D, Wong O, Yomtov B et al. Studying the Hurdles of Insulin Prescription (SHIP©): development, scoring and initial validation of a new self-administered questionnaire. Health Qual Life Outcomes. 2007;5(53). doi: 10.1186/1477-7525-5-53.
•• Holmes-Truscott E, Furler J, Blackberry I, O’Neal D, Speight J. Predictors of insulin uptake among adults with type 2 diabetes in the Stepping Up Study. Diabetes Res Clin Pract. 2017; doi:10.1016/j.diabres.2017.01.002. Assesses the predictive validity of both the Insulin Treatment Appraisal Scale and hypothetical willingness responses in terms of actual insulin uptake.
•• Patel N, Stone MA, McDonough C, Davies MJ, Khunti K, Eborall H. Concerns and perceptions about necessity in relation to insulin therapy in an ethnically diverse UK population with type 2 diabetes: a qualitative study focusing mainly on people of South Asian origin. Diabet Med. 2014;32(5):635–44. doi:10.1111/dme.12648. Purposes the utility of the necessity-concerns framework in understanding the acceptance of insulin iniation among people with type 2 diabetes.
Jenkins N, Hallowell N, Farmer AJ, Holman RR, Lawton J. Participants’ experiences of intensifying insulin therapy during the treating to target in type 2 diabetes (4-T) trial: qualitative interview study. Diabet Med. 2011;28(5):543–8.
Ho EY, James J. Cultural barriers to initiating insulin therapy in Chinese people with type 2 diabetes living in Canada. Can J Diabetes. 2006;30(4):390–6.
Hunt LM, Arar NH, Akana LL. Herbs, prayer, and insulin: use of medical and alternative treatments by a group of Mexican American diabetes patients. J Fam Pract. 2000;49(3):216–23.
Noakes H. Perceptions of black African and African-Caribbean people regarding insulin. J Diabetes Nurs. 2010;14(4):148–56.
Patel N, Stone MA, Chauhan A, Davies MJ, Khunti K. Insulin initiation and management in people with type 2 diabetes in an ethnically diverse population: the healthcare provider perspective. Diabet Med. 2012;29(10):1311–6. doi:10.1111/j.1464-5491.2012.03669.x.
Petrak F, Stridde E, Leverkus F, Crispin AA, Forst T, Pfützner A. Development and validation of a new measure to evaluate psychological resistance to insulin treatment. Diabetes Care. 2007;30(9):2199–204.
Snoek FJ, Skovlund SE, Pouwer F. Development and validation of the insulin treatment appraisal scale (ITAS) in patients with type 2 diabetes. Health Qual Life Outcomes. 2007;5:69. doi:10.1186/1477-7525-5-69.
Fu SN, Chin WY, Wong CKH, Yeung VTF, Yiu MP, Tsui HY, et al. Development and validation of the Chinese Attitudes to Starting Insulin Questionnaire (Ch-ASIQ) for primary care patients with type 2 diabetes. PLoS One. 2013;8(11):e78933.
Song Y, Jeon Y, Cho J, Kim B. Development of a psychological insulin resistance scale for Korean patients with diabetes. J Korean Acad Nurs. 2016;46(6):813–23.
•• Gherman A. Measuring psychological insulin resistance from the rational emotive and behavioral therapy perspective: development of the beliefs about insulin scale. Journal of Evidence-Based Psychotherapies. 2016;16(2):177. This articles describes the development and validation of the Romanian Beliefs about Insulin Scale.
Lee K. Validity and reliability of the Chinese version of the insulin treatment appraisal scale among primary care patients in Hong Kong. Hong Kong Med J. 2016;22(4):306–13.
Chang M, Huang C, Li T, Liao L, Chen C. Validation of the Chinese-version of the insulin treatment appraisal scale. Journal of Diabetes Investigation. 2010;1(suppl 1):88.
Huis In T, EMJ V, Makine C, Nouwen A, Karşda C, Kadioǧlu P, Karşda K, et al. Validation of the Turkish version of the problem areas in diabetes scale. Cardiovascular Psychiatry and Neurology. 2011; doi:10.1155/2011/315068.
Holmes-Truscott E, Pouwer F, Speight J. Further investigation of the psychometric properties of the insulin treatment appraisal scale among insulin-using and non-insulin-using adults with type 2 diabetes: results from diabetes MILES-Australia. Health Qual Life Outcomes. 2014;12:87. doi:10.1186/1477-7525-12-87.
Fu SN, Wong CKH, Chin WY, Luk W. Association of more negative attitude towards commencing insulin with lower glycosylated hemoglobin (HbA1c) level: a survey on insulin-naïve type 2 diabetes mellitus Chinese patients. J Diabetes Metab Disord. 2016;15(1):3.
Bahrmann A, Abel A, Zeyfang A, Petrak F, Kubiak T, Hummel J, et al. Psychological insulin resistance in geriatric patients with diabetes mellitus. Patient Educ Couns. 2014;94(3):417–22. doi:10.1016/j.pec.2013.11.010.
Chen CC, Chang MP, Hsieh MH, Huang CY, Liao LN, Li TC. Evaluation of perception of insulin therapy among Chinese patients with type 2 diabetes mellitus. Diabetes and Metab. 2011;37(5):389–94.
Hermanns N, Mahr M, Kulzer B, Skovlund SE, Haak T. Barriers towards insulin therapy in type 2 diabetic patients: results of an observational longitudinal study. Health Qual Life Outcomes. 2010;8:113. doi:10.1186/1477-7525-8-113.
Petrak F, Herpertz S, Stridde E, Pfützner A. Psychological insulin resistance in type 2 diabetes patients regarding oral antidiabetes treatment, subcutaneous insulin injections, or inhaled insulin. Diabetes Technol Ther. 2013;15(8):702–10.
Keij SM, Ismail K, Winkley K. The association between psychological distress and starting insulin therapy in people with type 2 diabetes: a prospective cohort study. Diabetic UK Professional Conference Gasglow: Diabetic Medicine; 2016. p. 170–5.
• Hermanns N, Lilly LC, Mader JK, Aberer F, Ribitsch A, Kojzar H, et al. Novel simple insulin delivery device reduces barriers to insulin therapy in type 2 diabetes results from a pilot study. J Diabetes Sci Technol. 2015;9(3):581–7. The first study to examine change in PIR questionnaire scores following insulin administration device change among people with type 2 diabetes.
Liebl A, Andersen H, Svendsen AL, Vora J, Yale JF. The SSG. Resource utilisation and quality of life following initiation of insulin detemir in patients with type 2 diabetes mellitus. Int J Clin Pract. 2013;67(8):740–9. doi:10.1111/ijcp.12133.
Peyrot M, Rubin RR, Lauritzen T, Skovlund SE, Snoek FJ, Matthews DR, et al. Resistance to insulin therapy among patients and providers: results of the cross-national Diabetes Attitudes, Wishes, and Needs (DAWN) study. Diabetes Care. 2005;28(11):2673–9.
Snoek FJ, Mollema ED, Heine RJ, Bouter LM, Van Der Ploeg HM. Development and validation of the diabetes fear of injecting and self- testing questionnaire (D-FISQ): first findings. Diabet Med. 1997;14(10):871–6.
Anderson RT, Skovlund SE, Marrero D, Levine DW, Meadows K, Brod M, et al. Development and validation of the insulin treatment satisfaction questionnaire. Clin Ther. 2004;26(4):565–78.
Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Factors associated with psychological insulin resistance in individuals with type 2 diabetes. Diabetes Care. 2010;33(8):1747–9.
Morris JE, Povey RC, Street CG. Experiences of people with type 2 diabetes who have changed from oral medication to self-administered insulin injections. A qualitative study. Practical Diabetes International. 2005;22(7):239–43.
Phillips A. Experiences of patients with type 2 diabetes starting insulin therapy. Nurs Stand. 2007;21(23):35.
Polinski JM, Smith BF, Curtis BH, Seeger JD, Choudhry NK, Connolly JG, et al. Barriers to insulin progression among patients with type 2 diabetes: a systematic review. Diabetes Educ. 2012;39(1):53–65. doi:10.1177/0145721712467696.
Brod M, Alolga SL, Meneghini L. Barriers to initiating insulin in type 2 diabetes patients: development of a new patient education tool to address myths. Misconceptions and Clinical Realities Patient. 2014;7(4):437–50.
Patel N, Stone MA, Hadjiconstantinou M, Hiles S, Troughton J, Martin-Stacey L, et al. Using an interactive DVD about type 2 diabetes and insulin therapy in a UK South Asian community and in patient education and healthcare provider training. Patient Educ Couns. 2015;98(9):1123–30. doi:10.1016/j.pec.2015.04.018.
Lee YK, Lee PY, Ng CJ. A qualitative study on healthcare professionals’ perceived barriers to insulin initiation in a multi-ethnic population. BMC Fam Pract. 2012;13:28. doi:10.1186/1471-2296-13-28.
Phillips A. Starting patients on insulin therapy: diabetes nurse specialist views. Nurs Stand. 2007;21(30):35–40.
• Hendrieckx C, Halliday JA, Beeney LJ, Speight J. Diabetes and emotional health: a handbook for health professionals supporting adults with type 1 or type 2 diabetes. Canberra: National Diabetes Services Scheme; 2016. Available from: www.ndss.org.au. An evidence-based, clinically infromed, practical resource to support health professionals to meet the emotional and mental health needs of adults with diabetes. Chapter 5 is focused on the psychological barriers to insulin use.
Acknowledgments
EHT and JS are supported by the funding provided to The Australian Centre for Behavioural Research in Diabetes by Diabetes Victoria and Deakin University. FP is supported by the University of Southern Denmark.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare no external support for any aspect of the submitted work.
EHT has undertaken research funded by an unrestricted educational grant from Abbott Diabetes Care to The Australian Centre for Behavioural Research in Diabetes (ACBRD) and has served on an AstraZeneca advisory board.
FP has received travel grants and funding from Novo Nordisk to his research group. FP co-developed the Insulin Treatment Appraisal Scale (ITAS).
JS has served as an advisory board member for Roche Diabetes Care, Sanofi ANZ and Janssen Pharmaceuticals. Her research group (ACBRD) has received unrestricted educational grants from Abbott Diabetes Care and Sanofi ANZ and consultancy income from Roche Diabetes Care, AstraZeneca and Sanofi ANZ.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Psychosocial Aspects
Electronic Supplementary Material
ESM 1
(DOCX 25 kb)
Rights and permissions
About this article
Cite this article
Holmes-Truscott, E., Pouwer, F. & Speight, J. Assessing Psychological Insulin Resistance in Type 2 Diabetes: a Critical Comparison of Measures. Curr Diab Rep 17, 46 (2017). https://doi.org/10.1007/s11892-017-0873-4
Published:
DOI: https://doi.org/10.1007/s11892-017-0873-4