Abstract
Purpose of Review
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a heritable form of cardiomyopathy, typically with autosomal dominant transmission, shown to be a defect in the cardiac desmosomes, with distinct regional and histopathological features. Clinically, this can ultimately result in bi-ventricular failure and/or malignant ventricular tachycardia (VT) via reentrant circuits created by patchy scar formation. We sought to review the current treatment for ventricular arrhythmias in the setting of ARVC, with particular attention to radiofrequency (RF) ablation and its varied techniques, along with potential therapies in the ablation spectrum.
Recent Findings
There is underwhelming data on the effectiveness of medical therapy for ARVC-related VT, including beta-blockers and antiarrhythmic medication. Primary and secondary prophylactic implantable-cardioverter defibrillator (ICD) implantation in higher-risk patients is recommended. More recently, RF ablation has been used for ARVC-related VT. Endocardial VT ablation in this setting can produce acute success, though recurrence rate is quite high, which may be explained by the more epicardial and patchy nature of the disease. Combined endocardial-epicardial ablation has since been shown to be feasible, safe, and with significantly better acute and long-term success, particularly when combined with scar dechanneling or homogenization of the scar. However, recurrence rates are not insignificant, and ablation does not eliminate the need for ICD placement.
Summary
Medical therapy for ARVC-related VT is suboptimal. RF ablation techniques including endocardial and epicardial approaches appear to have the highest success rates for ARVC-related VT. Catheter ablation of VT in ARVC patients should be considered a potentially effective strategy for eliminating frequent VT episodes and ICD shocks rather than a curative therapeutic approach, until long-term efficacy has been consistently documented. Research into the optimal mapping and ablation techniques are promising and ongoing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a heritable form of cardiomyopathy, genetically determined predominantly via an autosomal dominant pattern. The prevalence of ARVC is approximately 1:5000, affecting men more frequently than women with a ratio of 3:1. ARVC predominantly affects the right ventricle (RV), but may also involve the left ventricle (LV) and results in heart failure and ventricular tachycardia (VT) [1]. In 1982, Marcus et al. initially described the disease, when he reported 24 cases of VT with left bundle branch block (LBBB) morphology, RV wall motion abnormalities, and replacement of the RV myocardium by adipose and fibrous tissue [2]. Later, in 1984, the electrocardiographic characteristics of ARVC were described, including the pathognomonic epsilon wave [3]. Pathologically, ARVC is characterized by fibro-fatty replacement, myocardial atrophy, fibrosis, and eventually thinning of the RV wall with RV dilatation and formation of small aneurysms in this chamber [4]. These alterations subsequently cause electrical instability often precipitating VT [5]. Several genes have been associated with this entity, and more than 13 mutations have been identified to date [6]. ARVC is frequently a devastating disease given the fact that the first symptom is often sudden cardiac death (SCD). Implantable cardioverter-defibrillator (ICD) implantation decreases the risk of SCD from VT. Nonetheless, ARVC is a progressive entity, and usually progresses to refractory VT or a ventricular fibrillation (VF) storm despite ICD therapies. ARVC should be considered in a young patient with palpitations, symptoms consistent with arrhythmogenic syncope, or aborted SCD. VT in ARVC mostly has a left bundle branch (LBBB) morphology, although VT with a RBBB morphology may also be present if the LV is involved. VT is often exercise-related, due largely to activation of the sympathetic nervous system, which leads to premature ventricular contractions (PVCs) and reentrant circuits. Other electrocardiographic anomalies such as inverted T waves in the right precordial leads (V1–V3) and frequent PVCs, even in asymptomatic patients, should arouse suspicion for this disease [6].
In this review, we will focus on the fundamental electrocardiographic and electrophysiologic characteristics and findings of VT in ARVC and therapeutic approaches of this disorder with an emphasis on endocardial and epicardial radiofrequency (RF) ablation. Details regarding the pathogenesis, clinical manifestations, diagnostic criteria, and the approach to risk stratification have already been described elsewhere [6, 7].
Diagnosis
Consensus diagnostic criteria have been developed, first in 1994 and updated in 2010. The diagnosis is based on six categories, each divided into major and minor criteria. These six categories include imaging [including both cardiovascular magnetic resonance imaging (CMR) and/or transthoracic echo], tissue characterization by RV biopsy or autopsy, repolarization abnormalities, depolarization abnormalities, evidence of arrhythmias, and family history [4]. The diagnosis of ARVC is made in the presence of two major or one major plus two minor criteria or four minor criteria taken from different groups [4]. Additionally, with the arrival of the molecular genetics, remarkable diagnostic improvements have been made [8].
Electrocardiogram
Almost 90% of patients with ARVC have some electrocardiograms (ECG) abnormality. The primary depolarization abnormality included in the revised criteria is the epsilon wave, described as reproducible low-amplitude signals between end of QRS complex to the onset of the T wave in the right precordial leads (V1 to V3), probably secondary to slowed intraventricular conduction. This may be found in up to 33% of patients with ARVC. Inverted T waves in the right precordial leads are the primary repolarization abnormality described in the 2010 Revised Task Force Criteria, and both these ECG findings constitute a major criterion (the T inversion in the absence of complete RBBB). One of the commonest ECG findings is a prolonged S wave upstroke [55 ms in V1–V3 (90–95%)], followed by an inverted T wave in those right precordial leads, that occurs in 50% of cases presenting with VT. If PVCs are evident, the origin is usually from one of the three regions of fibro-fatty replacement in the “triangle of dysplasia” (i.e., right ventricular outflow tract, apex, and infundibulum).
Signal Average Electrocardiogram
Three criteria have been described using signal average electrocardiogram (SAECG): (a) the filtered QRS duration >114 ms, (b) low-amplitude signal <38 ms, and (c) root-mean-square amplitude of the last 40 ms of the QRS >20 μV. An abnormal SAECG (defined by one of three criteria) has been associated with a dilated and impaired RV on CMR [9].
Differential Diagnoses
Right ventricular outflow tract (RVOT) tachycardia is one of the main differential diagnoses of ARVC. Although in the revised criteria of 2010 cited above, the more specific VT morphology for ARVC is a LBBB morphology with a superior axis, the clinical presentation and electrocardiographic findings of VT are similar to idiopathic RVOT VT (VT with LBBB with an inferior axis). Nonetheless, unlike ARVC, RVOT tachycardia is contemplated to be a primary electrical disease in the absence of structural heart disease. Idiopathic RVOT VT is considerably more common than ARVC. Hoffmayer et al. have developed an electrocardiographic scoring system for distinguishing RVOT arrhythmias in patients with ARVC from idiopathic VT [10]. The scoring system includes ECG findings in sinus rhythm and during VT; it provides three points for anterior T wave inversions in leads V1–V3 during sinus rhythm, and in the setting of ventricular arrhythmias (VA); two points for QRS duration in lead I > 120 ms, two points for QRS notching, and one point for precordial transition in lead V5 or later. A score of 5 or greater was able to correctly distinguish ARVC from idiopathic VT 93% of the time, with a sensitivity of 84%, specificity of 100%, positive predictive value of 100%, and negative predictive value of 91% [10].
Sarcoidosis is also a condition that should be distinguished due to its overlapping VT morphologies. Dechering et al. identified the electrophysiological characteristics of VA in cardiac sarcoidosis versus ARVC [11]. Clinical and electrophysiological parameters that were more characteristic of cardiac sarcoidosis in their patients included reduced left ventricular ejection fraction, a significantly wider QRS during VT, right-sided apical VT, and more inducible forms of monomorphic VT [11]. Preexcited AV reentry tachycardia, Brugada syndrome, and other congenital heart diseases such as Uhl’s anomaly (apoptotic dysplasia with complete absence of the myocardium) may also show similar appearing arrhythmias [12].
Treatment Strategies
Because the clinical presentation of ARVC patients may be varied from asymptomatic to SCD, the therapeutic strategy must be customized to each patient, based on clinical presentation, risk stratification, and patient preference. Avoiding serious adverse events and identifying patients at high risk for malignant arrhythmias and SCD is the ultimate goal of therapy [13]. Several studies have assessed the efficacy and safety of pharmacological and non-pharmacological therapies in patients with ARVC, yet large prospective randomized controlled trials are lacking.
Pharmacological Therapy
Antiarrhythmic drugs (AADs) have been used as adjunctive therapy to reduce frequent ICD discharges due to recurrent VT [14]. Beta-blockers have shown to be effective in reducing adrenergically stimulated arrhythmias [15]. However, the available evidence for ARVC patients is from observational studies, which have shown conflicting results. Amiodarone and sotalol have been proposed as effective treatments of sustained monomorphic VT in patients with ARVC. In 1992, Wichter et al. reported in patients with ARVC that sotalol was the most effective medication in the treatment of both inducible and non-inducible VT with efficacy rates of 68.4 and 82.8%, respectively [16]. ARVC patients who did not respond to sotalol were non-responders to other AAD including amiodarone [16]. Conversely, Marcus et al. reported that neither beta-blockers nor sotalol seemed to be protective against clinically relevant VT. Additionally, patients on sotalol were found to have an increased risk for significant VT. On the other hand, amiodarone, although only received by a relatively small number of patients, had the greatest efficacy in preventing VT in this study [17]. These inconsistent data need to eventually be addressed in the future with randomized clinical trials. The addition of flecainide in combination with sotalol/metoprolol may be an effective antiarrhythmic strategy for the control of ventricular arrhythmias in patients with ARVC refractory to single-agent therapy and/or catheter ablation (CA) [18].
Non-Pharmacologic Treatment
Implantable-Cardioverted Defibrillator
When assessing the need for primary prevention ICD placement, predictive markers of higher risk for SCD would ideally be clearly defined. However, these high-risk markers for SCD have not been well defined by large prospective trials for ARVC. As per the 2008 ACC/HRS device guidelines (and unchanged in the 2012 update), NSVT on non-invasive monitoring, severe RV dilation, extensive RV involvement, LV involvement, unexplained syncope, and male sex may serve as markers of higher risk. As such, these patients are potential candidates for a prophylactic ICD even in the absence of prior VA [13]. Additionally, patients with genotypes of ARVC associated with a high risk for SCD (e.g., ARVC/D 5-TMEM43) should be considered as possible candidates for primary prevention ICD therapy [19]. In 2005, Hodgkinson et al. identified 11 families from Canada who were affected by autosomal-dominant ARVC 5 TMEM43, which is related to mutation at chromosome 3-3p25 and is associated with early SCD, especially in men [19]. There are no specific prospective randomized trials for secondary prevention of SCD in an ARVC population, or comparing medical therapy versus ICD. However, observational studies from different centers consistently show a high rate of appropriate ICD firings for VA and a low rate of arrhythmic death in the ARVC patients who have received an ICD. Corrado et al. determined the impact of ICD therapy on SCD prevention in patients with ARVC [20]. The authors followed 132 patients after successful ICD implantation due to cardiac arrest, sustained VT, unexplained syncope, and/or family history of SCD due to ARVC. After a follow-up of 3.3 years, 48% of the patients received appropriate ICD intervention for episodes of VT. The total patient survival rate at 3.3 years was 96% in patients with an ICD compared with 72% of the projected SCD-free survival rates without the device (P < 0.001). Significant predictors of malignant VT were identified and included young age, history of cardiac arrest or VT with hemodynamic compromise, unexplained syncope, and involvement of the left ventricle. Bhonsale et al. also reported important predictors of appropriate ICD intervention in ARVC patients in whom ICD were implanted for primary prevention of SCD. These factors included the presence of non-sustained VT and inducibility at EPS [21].
Although there is clear evidence for secondary prophylaxis ICD implantation in ARVC, short- and long-term complications are frequently observed with these devices. The fibro-fatty infiltration of the RV causes problems in ICD lead placement including aneurysmal rupture. ARVC patients are usually younger compared to patients with ICD indications due to other diseases. This situation leads to an increased lifetime risk of device-related complications [22]. Developments in ICD technology may further improve the outcomes and decrease the risk of adverse events in patients with ARVC. Despite the growing use of newer technology such as the subcutaneous ICD system, to date, there are limited data on the use of such technology for ARVC patients; hence, the transvenous system remains as the preferred device modality.
Radiofrequency Ablation
RF ablation of VA in ARVC has traditionally been reserved for patients with recurrent VT despite treatment with AADs [23, 24]. In the past, there has been a high rate of recurrence after endocardial ablation due to the characteristic diffuse, patchy involvement of the myocardium, including the epicardium, and progressive nature of this disease [23, 24]. More recently, several publications suggest that simultaneous epicardial and endocardial mapping and ablation for VT are feasible and might even result in permanent elimination of this arrhythmia [25•].
VT in ARVC is the result of scar-related macro-reentry circuits, similar to that observed in the post-myocardial infarction setting, which is suitable for mapping and interruption by CA. To this end, CA may be guided by either conventional electrophysiological or substrate-based mapping during sinus rhythm. In the first studies of VA interruption in ARVC dating back to 1989, Fontaine et al. [26], using direct current fulguration (160 to 280 J) in 13 ARVC patients with refractory VA, demonstrated the feasibility of VT ablation in this entity. However, given the high mortality rate with this technique, it was not widely performed [26]. Subsequently, several RF current endocardial ARVC VT ablation studies have reported on acute and long-term ablation results. Acute success has been obtained in 60 to 80% of patients, whereas the long-term recurrence rate at follow-up of 3 to 5 years was lower (50 to 70%). More recently, studies have suggested that many of the VT reentry circuits in ARVC either originate from or partially or primarily use the epicardium, which may partly explain the failure of conventional endocardial mapping/CA.
Endocardial RF Ablation
Ellison et al. attempted to extrapolate ischemic VT entrainment mapping techniques and predictors of successful ablation sites to VT in ARVC patients [27]. The authors identified exit, central/proximal, inner loop, outer loop, remote bystander, and adjacent bystander sites by entrainment criteria. The reentrant circuit sites were found predominantly around the tricuspid annulus and in the RVOT. RF ablation acutely terminated VT in 22% of the cases, and only 42% of the patients were rendered non-inducible after CA [27]. However, in a study by Marchlinski et al., using detailed RV bipolar electrogram voltage mapping in 21 patients with ARVC (Fig. 1) [24], VT was ablated in 19 patients by use of focal and/or linear lesions with irrigated-tip catheters with long-term success rates of 84% during 27-month follow-up. Consistent with prior studies, the electrogram abnormalities in the RV were always perivalvular and tended to extend toward the apex, often in a cone-like manner involving both the free wall and, to a lesser extent, the septum. Activation and entrainment mapping followed by focal ablation was used in only three patients with hemodynamically tolerated VT. In the remaining 16 patients with non-mappable VT, linear lesions of 2.0 to 8.6 cm were also deployed, with the site of ablation guided primarily by pace mapping. These linear lesions typically extended from the most abnormal myocardium, with a signal amplitude <0.5 mV, through abnormal endocardium with a good pace map match to annular/valvular structures as previously described. In patients with less extensive perivalvular bipolar voltage abnormalities, the linear lesion extended across the entire segment of abnormal myocardium. Of note, more than one ablation procedure was required in 13 patients [24]. Delal et al. sought to evaluate the outcomes of RF CA of VT in ARVC patients focusing on defining the single-procedure efficacy over long-term follow-up [23]. Of these procedures, 46% resulted in elimination of all inducible VTs, although 85% of the procedures were followed by recurrence. The cumulative VT recurrence-free survival was 75, 50, and 25% after 1.5, 5, and 14 months, respectively [23].
Characteristic patterns of endocardial bipolar voltage abnormalities in RV cardiomyopathy and VT. Anterior (above) and posterior (below) views. Peritricuspid (pattern 1), peripulmonic/RVOT (pattern 2), or more extensive involvement extending from both valvular regions (pattern 3) toward the RV apex are shown. Distribution of abnormal electrograms is predominantly on the free wall. RV apex is spared, and septal involvement is frequently identified (arrows). With permission from Marchlinski et al. Circulation. 2004;110:2293–8 [24]
Epicardial RF Ablation
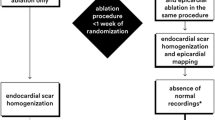
Garcia et al., given the poor long-term outcomes in endocardial-only VT ablation in ARVC, and the propensity for ARVC VT circuits to originate or involve the epicardial myocardium, first reported the feasibility and efficacy of epicardial CA in ARVC patients who underwent an epicardial approach after previously failed endocardial VT mapping/ablation procedures [25•]. Using bipolar voltage mapping, the magnitude of the electroanatomical scar (<1.0 mV for epicardium and <1.5 mV for endocardium) was significantly larger on the epicardium compared to the endocardium (95 ± 47 versus 38 ± 32 cm2; P < 0.001, respectively), and was uniformly marked by multicomponent and late electrograms (Fig. 2a–c). VTs were targeted on the endocardium and epicardium with the use of activation, entrainment, or pace mapping with focal/linear ablation and targeting of late potentials. Complete success was achieved in 85% of cases (partial success in 92%), and 77% of patients were free of VT during 18 months of follow-up [25•]. This study demonstrated the feasibility and improved efficacy of a simultaneous endocardial/epicardial substrate-based ablation approach versus an endocardial ablation alone, and suggests this approach be given strong consideration [25•]. Given the fact that obtaining epicardial access has several potential complications, the same group of investigators tested the hypothesis that endocardial unipolar voltage mapping in patients with ARVC VT and preserved endocardial bipolar voltage might identify the extent of epicardial bipolar voltage substrate [28]. Using a cutoff of <5.5 mV for normal endocardial unipolar voltage derived from 8 control patients without structural heart disease, 10 patients with known ARVC and 13 patients with RV VT with modest or no endocardial bipolar voltage abnormalities underwent detailed endocardial and epicardial mapping. The area of epicardial unipolar voltage abnormality in most patients was on average three times more extensive than the endocardial bipolar abnormality and correlated (r = 0.63, P < 0.05 and r = 0.81, P < 0.008, respectively) with the larger area epicardial bipolar abnormality with respect to size (Fig. 3) [28].
a Endocardial versus epicardial bipolar voltage map (anterior view) in a patient with ARVC and VT unresponsive to endocardial ablation. The white broken lines on the right image show the approximated mapped endocardial surface on the combined RV-LV epicardial voltage map shown. Note that only a small basal RV region of low voltage was present on the endocardium in proximity to the tricuspid valve annulus (yellow arrows). Low voltage covered the entire epicardial free wall surface of the RV, and signals were of low amplitude, multicomponent, fractionated, and late. With permission from Garcia et al. Circulation. 2009;120:366–75 [25•]. b Anterior view of the epicardial bipolar voltage map showing a diffuse area of low-amplitude signals <0.5 mV. To define area of abnormal epicardial voltage for comparison with endocardial voltage map, the majority of signals in low-voltage area were also multicomponent, wide, and/or late (arrows). With permission from Garcia et al. Circulation. 2009;120:366–75 [25•]. c Ablation targets identified during epicardial mapping included late potentials (blue arrows) recorded from distal and proximal electrodes of the ablation catheter and pace map match of VT (yellow arrow) with long stimulus to QRS interval. With permission from Garcia et al. Circulation. 2009;120:366–75 [25•]
Unipolar endocardial electrograms defining the location and greater extent of epicardial bipolar electrogram abnormalities. left endocardial bipolar voltage showing small patches of low voltage in a patient with ARVC. center Endocardial unipolar voltage map demonstrates a more extensive area of abnormal endocardium (<5.5 mV). right Epicardial bipolar voltage mapping confirms the extent of abnormal epicardium predicted by the unipolar mapping. Black dots represent wide, split, and/or late electrograms consistent with scar versus fat. Reprinted from Polin et al. Heart Rhythm. 2011;8:76–83, with permission from Elsevier [28]
Pokushalov et al. corroborated these epicardial concepts in the pediatric population with ARVC-related VA [29]. After ablation, 94.1% of the patients had no inducible VT. During a mean follow-up of 26 months, 70.6% patients remained free of any episodes of VT [29]. Coronary angiography was performed selecting a safer area for RF applications and keeping the ablation catheter in the target site position during ablation [29]. Although it is safe to deliver RF applications in the anterolateral RV wall, it is desirable to routinely perform coronary angiogram to precisely localize the right coronary artery and its major branches.
In a prospective international study in 49 patients with ARVC-related VA, Bai et al. compared the long-term freedom from recurrent VA via endocardial-alone ablation versus endo-epicardial substrate-based ablation [30]. All patients had prior monomorphic VT with LBBB pattern documented by ECG or Holter, with or without syncope, and all had received an ICD. Subsequently, they developed recurrent VTs or multiple ICD therapies despite taking antiarrhythmic drugs AAD, including sotalol, amiodarone, dofetilide, and beta-blockers. After a follow-up of at least 3 years post-ablation, freedom from VAs or ICD therapy was 52.2% in the endocardial group and 84.6% in the endocardial/epicardial group (P = 0.029), with 21.7 and 69.2% patients off AAD (P < 0.001), respectively. The presence of >10 PVCs per minute after CA was associated with more VA recurrence [30]. Based on this data, it is prudent to consider an endo-epicardial approach to ARVC-related VA.
Ablation Strategies
Scar Dechanneling
In a single-center prospective study of 11 patients with ARVC-related VA, Berruezo et al. reported that in addition to an endocardial and/or epicardial approach for ablation of the clinical ARVC VT, complete scar dechanneling with elimination of either endocardial and/or epicardial scar-conducting channels (i.e., intrascar, interscar, or between scar and valvular annuli) is a promising approach to improve long-term success rate of CA [31••]. In fact, the combined endocardial and epicardial VT ablation eliminated all clinical and induced VTs, and the addition of scar dechanneling resulted in non-inducibility in all cases, significantly improved from earlier studies. Seven patients continued on sotalol. During a median follow-up of 11 months, only one patient (9%) had a VT recurrence. To identify these channels, an endocardial high-density substrate voltage map of the RV was obtained during stable sinus rhythm using the CARTO system. Image integration between a preacquired contrast-enhanced cardiac CT or contrast-enhanced CMRI was performed using CartoMerge software. Substrate mapping was performed to identify scar and conducting channels (CCs) inside the scar, between the scars, or between a scar and the tricuspid annulus. The CCs have been defined as pathways of orthodromically activated sites inside the scar. Scar CCs were identified by (1) a color-coded voltage map adjustment of the lower and upper thresholds (voltage channels) and (2) the presence of >2 tagged recordings of electrograms with a duration >70 ms and/or isolated, delayed components (E-IDCs), with the delayed component showing sequential orthodromic activation (late potential channels) (Fig. 4). Those CCs between two confluent scar areas or between a scar and the tricuspid annulus were considered in addition to intrascar CCs. After CC identification, the entrance of each CC in the scar was tagged during sinus rhythm. The CC entrance was defined as the E-IDC with the shortest delay between the far-field component of healthy muscle (usually low frequency, high voltage) and the local component (delayed activation, usually with fractionation and low voltage) corresponding to the activation of myocardial tissue in the scar.
Epicardial substrate voltage map of a patient with familial ARVC and VT storm. A wide inferolateral and apical dense scar was identified. A conducting channel (CC) was identified at the base of the scar by tagging the E-IDCs (blue dots) but not with a voltage adjustment. Electrograms on the left correspond to the CC at the right ventricular outflow tract (blue dots). The entrance of this CC during sinus rhythm was identified on the basis of the activation time of the delayed components of the E-IDCs. The activation sequence was from inferior to superior, as shown on the sequential electrogram activation time measurement (M1–M2). In this case, voltage mapping was also able to show this CC. Two additional rows of tagged E-IDCs identified two CCs parallel to the tricuspid annulus, with an activation sequence from superior to inferior. RF applications at the CC entrance eliminated both channels with a low number of applications. In this patient, both intrascar and interscar CCs (due to the presence of confluent patchy scars) were eliminated. With permission from Berruezo et al. Circ Arrhythm Electrophysiol. 2012;5:111–21 [31••]
The initial step was RF catheter ablation of the clinical VT. Activation mapping and entrainment mapping were used for sustained, well-tolerated VT, and substrate-based ablation guided by pace mapping was used for non-sustained or non-tolerated VT. In addition to the clinical VT ablation, elimination of all CCs identified during substrate mapping was attempted by means of combined endocardial and epicardial scar dechanneling. It has been reported that the higher the scar heterogeneity in patients with ischemia is, the higher the arrhythmogenic potential of scars is. Scar heterogeneity can be recognized during substrate voltage mapping and permits identifying CCs of consecutive electrograms with higher voltage amplitude than the surrounding area, which have been demonstrated to be responsible for VT reentrant circuits; their elimination renders VTs non-inducible. Therefore, to reduce possible VT relapses using different CCs than those participating in the clinical VT, the substrate-based ablation strategy employed endocardial and epicardial scar CC elimination on top of clinical VT ablation (Fig. 5) [31••]. The same group a few years later published a second study, which confirmed that the scar and the CCs responsible for VTs in patients with ARVC are mostly epicardial and have a typical distribution, with a preferential location in the subtricuspid area. The CCs can be identified during substrate mapping in SR by using both techniques: bipolar voltage adjustment of the upper and lower thresholds and tagging the E-IDCs with sequential activation inside the scar. However, the latter should always be used for a substrate-guided ablation, as this technique identifies a higher proportion of CCs and, more importantly, most CCs that serve as the substrate for VTs. Using only the bipolar voltage adjustment, more than 70% of the CCs and 60% of the VT isthmuses would not be identified [32].
Epicardial substrate voltage map with CCs identified by tagging electrograms with isolated, delayed components. CC entrance is marked with black dots. The amplitude of the far-field component decreases and the delay of the local component of the electrogram registered at the border zone increases with the distance from the edge of the scar. b 3D anatomic map with red dots at locations where radiofrequency was delivered (mainly at the CC entrance). c A new map after radiofrequency ablation was obtained. Of note, a few applications eliminated all isolated, delayed components and increased the epicardial scar area. d RV electrogram registry from the distal dipole of the ablation catheter and electrogram registered at the proximal dipole of the ablation catheter during radiofrequency application in a CC entrance in this patient. The electrogram has two components. The first represents the far field of the normal myocardium, and the second (black arrows) represents the local activation at the CC entrance. During radiofrequency application, a delay precedes the CC entrance block (asterisk). With permission from Berruezo et al. Circ Arrhythm Electrophysiol. 2012;5:111–21 [31••]
In a single-center study in 2015, Phillips et al. evaluated procedural strategy, safety, and efficacy of epicardial RFA with a focus on the substrate characteristics and recurrent VT [33]. The majority of critical VT circuits (69%) were on the epicardial surface, mostly in the subtricuspid region. VT-free survival was 83, 76, and 70% at 6, 12, and 24 months, respectively. A significant reduction of VT burden was observed (P < 0.001), even among those with VT recurrence. The only complication noted was one post-procedural pericarditis. The features of the recurrent VT suggested a possible catecholamine-mediated mechanism with an origin in a region not targeted for ablation (during exercise, with fast cycle lengths) [33]. Santangeli et al. later published similar results. VT-free survival was 71% with a mean follow-up of 56 months, with an additional 15% experiencing only a single VT recurrent episode, and with no patient receiving long-term amiodarone therapy [34].
Left Ventricular Involvement
Biventricular involvement with LV fibro-fatty replacement has been found in up to 70% of the cases of ARVC. It is usually age dependent and associated with a more severe cardiomyopathy [35]. Berte et al. defined the imaging and electrophysiological characteristics of the left-sided ARVC substrate [36]. Their main findings was that LV intramyocardial fat is present on imaging in the majority of patients with ARVC fulfilling the modified Task Force criteria, mostly on lateral, inferior, and apical LV segments, and with a lower burden than the RV and that LV fat hosts the same density of LAVA as RV fat, but is less efficiently detected by voltage mapping [36].
Recommendations for RF ablation of ARVC VT according to the International Task Force Consensus Statement have been recently published (Table 1) [37••].
Perspective and Conclusions
Although VT ablation of for ARVC does not eliminate the need for an ICD, given a considerable recurrence rate, it does result in lower arrhythmia burden, lower medication dependence, and increased quality of life. Future studies on a larger scale of patients should compare traditional mapping and ablation to different substrate modification techniques. For refractory cases, autonomic modulation by performing cervicothoracic bilateral sympathectomy has shown promising results [38]. RF catheter ablation of VT in ARVC patients is considered an effective strategy management for eliminating frequent VT and ICD shocks. However, RF ablation should not be seen as a curative therapeutic approach, until long-term studies have been conducted. Therefore, RF ablation is not an alternative to ICD therapy in patients with ARVC and VT, with the rare exception of cases of hemodynamically stable, single-morphology VT [37••].
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Manyari DE, Klein GJ, Gulamhusein S, Boughner D, Guiraudon GM, Wyse G, et al. Arrhythmogenic right ventricular dysplasia: a generalized cardiomyopathy? Circulation. 1983;68:251–7.
Marcus FI, Fontaine GH, Guiraudon G, Frank R, Laurenceau JL, Malergue C, et al. Right ventricular dysplasia: a report of 24 adult cases. Circulation. 1982;65:384–98.
Fontaine G, Frank R, Guiraudon G, Pavie A, Tereau Y, Chomette G, et al. Significance of intraventricular conduction disorders observed in arrhythmogenic right ventricular dysplasia. Arch Mal Coeur Vaiss. 1984;77:872–9.
Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Circulation. 2010;121:1533–41.
Lemery R, Brugada P, Janssen J, Cheriex E, Dugernier T, Wellens HJ. Nonischemic sustained ventricular tachycardia: clinical outcome in 12 patients with arrhythmogenic right ventricular dysplasia. J Am Coll Cardiol. 1989;14:96–105.
Romero J, Mejia-Lopez E, Manrique C, Lucariello R. Arrhythmogenic right ventricular cardiomyopathy (ARVC/D): a systematic literature review. Clin Med Insights Cardiol. 2013;7:97–114.
Corrado D, Link MS, Calkins H. Arrhythmogenic right ventricular cardiomyopathy. N Engl J Med. 2017;376:61–72.
Corrado D, Thiene G. Arrhythmogenic right ventricular cardiomyopathy/dysplasia: clinical impact of molecular genetic studies. Circulation. 2006;113:1634–7.
Kamath GS, Zareba W, Delaney J, Koneru JN, McKenna W, Gear K, et al. Value of the signal-averaged electrocardiogram in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Heart Rhythm. 2011;8:256–62.
Hoffmayer KS, Bhave PD, Marcus GM, James CA, Tichnell C, Chopra N, et al. An electrocardiographic scoring system for distinguishing right ventricular outflow tract arrhythmias in patients with arrhythmogenic right ventricular cardiomyopathy from idiopathic ventricular tachycardia. Heart Rhythm. 2013;10:477–82.
Dechering DG, Kochhauser S, Wasmer K, Zellerhoff S, Pott C, Kobe J, et al. Electrophysiological characteristics of ventricular tachyarrhythmias in cardiac sarcoidosis versus arrhythmogenic right ventricular cardiomyopathy. Heart Rhythm. 2013;10:158–64.
Gerlis LM, Schmidt-Ott SC, Ho SY, Anderson RH. Dysplastic conditions of the right ventricular myocardium: Uhl’s anomaly vs arrhythmogenic right ventricular dysplasia. Br Heart J. 1993;69:142–50.
Wichter T, Breithardt G. Implantable cardioverter-defibrillator therapy in arrhythmogenic right ventricular cardiomyopathy: a role for genotyping in decision-making? J Am Coll Cardiol. 2005;45:409–11.
European Heart Rhythm A, Heart Rhythm S, Zipes DP, Camm AJ, Borggrefe M, Buxton AE, et al. American College of C, American Heart Association Task F and European Society of Cardiology Committee for Practice G. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death). J Am Coll Cardiol. 2006;48:e247–346.
Leclercq JF, Coumel P. Characteristics, prognosis and treatment of the ventricular arrhythmias of right ventricular dysplasia. Eur Heart J. 1989;10(Suppl D):61–7.
Wichter T, Borggrefe M, Haverkamp W, Chen X, Breithardt G. Efficacy of antiarrhythmic drugs in patients with arrhythmogenic right ventricular disease. Results in patients with inducible and noninducible ventricular tachycardia. Circulation. 1992;86:29–37.
Marcus GM, Glidden DV, Polonsky B, Zareba W, Smith LM, Cannom DS, et al. Multidisciplinary study of right ventricular dysplasia I. Efficacy of antiarrhythmic drugs in arrhythmogenic right ventricular cardiomyopathy: a report from the North American ARVC Registry. J Am Coll Cardiol. 2009;54:609–15.
Ermakov S, Gerstenfeld EP, Svetlichnaya Y and Scheinman MM. Use of flecainide in combination antiarrhythmic therapy in patients with arrhythmogenic right ventricular cardiomyopathy. Heart Rhythm. 2016.
Hodgkinson KA, Parfrey PS, Bassett AS, Kupprion C, Drenckhahn J, Norman MW, et al. The impact of implantable cardioverter-defibrillator therapy on survival in autosomal-dominant arrhythmogenic right ventricular cardiomyopathy (ARVD5). J Am Coll Cardiol. 2005;45:400–8.
Corrado D, Leoni L, Link MS, Della Bella P, Gaita F, Curnis A, et al. Implantable cardioverter-defibrillator therapy for prevention of sudden death in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation. 2003;108:3084–91.
Bhonsale A, James CA, Tichnell C, Murray B, Gagarin D, Philips B, et al. Incidence and predictors of implantable cardioverter-defibrillator therapy in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy undergoing implantable cardioverter-defibrillator implantation for primary prevention. J Am Coll Cardiol. 2011;58:1485–96.
Epstein AE, JP DM, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. American College of Cardiology/American Heart Association Task Force on Practice G, American Association for Thoracic S and Society of Thoracic S. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Circulation. 2008;117:e350–408.
Dalal D, Jain R, Tandri H, Dong J, Eid SM, Prakasa K, et al. Long-term efficacy of catheter ablation of ventricular tachycardia in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy. J Am Coll Cardiol. 2007;50:432–40.
Marchlinski FE, Zado E, Dixit S, Gerstenfeld E, Callans DJ, Hsia H, et al. Electroanatomic substrate and outcome of catheter ablative therapy for ventricular tachycardia in setting of right ventricular cardiomyopathy. Circulation. 2004;110:2293–8.
• Garcia FC, Bazan V, Zado ES, Ren JF, Marchlinski FE. Epicardial substrate and outcome with epicardial ablation of ventricular tachycardia in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation. 2009;120:366–75. This is the first study that demontrate the benefit of epicaridal ablation for ARVD patients.
Fontaine G, Frank R, Rougier I, Tonet JL, Gallais Y, Farenq G, et al. Electrode catheter ablation of resistant ventricular tachycardia in arrhythmogenic right ventricular dysplasia: experience of 13 patients with a mean follow-up of 45 months. Eur Heart J. 1989;10(Suppl D):74–81.
Ellison KE, Friedman PL, Ganz LI, Stevenson WG. Entrainment mapping and radiofrequency catheter ablation of ventricular tachycardia in right ventricular dysplasia. J Am Coll Cardiol. 1998;32:724–8.
Polin GM, Haqqani H, Tzou W, Hutchinson MD, Garcia FC, Callans DJ, et al. Endocardial unipolar voltage mapping to identify epicardial substrate in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Heart Rhythm. 2011;8:76–83.
Pokushalov E, Romanov A, Turov A, Artyomenko S, Shirokova N, Karaskov A. Percutaneous epicardial ablation of ventricular tachycardia after failure of endocardial approach in the pediatric population with arrhythmogenic right ventricular dysplasia. Heart Rhythm. 2010;7:1406–10.
Bai R, Di Biase L, Shivkumar K, Mohanty P, Tung R, Santangeli P, et al. Ablation of ventricular arrhythmias in arrhythmogenic right ventricular dysplasia/cardiomyopathy: arrhythmia-free survival after endo-epicardial substrate based mapping and ablation. Circ Arrhythm Electrophysiol. 2011;4:478–85.
•• Berruezo A, Fernandez-Armenta J, Mont L, Zeljko H, Andreu D, Herczku C, et al. Combined endocardial and epicardial catheter ablation in arrhythmogenic right ventricular dysplasia incorporating scar dechanneling technique. Circ Arrhythm Electrophysiol. 2012;5:111–21. In this study a detailed description of how to perform scar dechannelling in ARVD patients is given.
Fernandez-Armenta J, Andreu D, Penela D, Trucco E, Cipolletta L, Arbelo E, et al. Sinus rhythm detection of conducting channels and ventricular tachycardia isthmus in arrhythmogenic right ventricular cardiomyopathy. Heart Rhythm. 2014;11:747–54.
Philips B, te Riele AS, Sawant A, Kareddy V, James CA, Murray B, et al. Outcomes and ventricular tachycardia recurrence characteristics after epicardial ablation of ventricular tachycardia in arrhythmogenic right ventricular dysplasia/cardiomyopathy. Heart Rhythm. 2015;12:716–25.
Santangeli P, Zado ES, Supple GE, Haqqani HM, Garcia FC, Tschabrunn CM, et al. Long-term outcome with catheter ablation of ventricular tachycardia in patients with arrhythmogenic right ventricular cardiomyopathy. Circ Arrhythm Electrophysiol. 2015;8:1413–21.
Corrado D, Basso C, Thiene G, McKenna WJ, Davies MJ, Fontaliran F, et al. Spectrum of clinicopathologic manifestations of arrhythmogenic right ventricular cardiomyopathy/dysplasia: a multicenter study. J Am Coll Cardiol. 1997;30:1512–20.
Berte B, Denis A, Amraoui S, Yamashita S, Komatsu Y, Pillois X, et al. Characterization of the left-sided substrate in arrhythmogenic right ventricular cardiomyopathy. Circ Arrhythm Electrophysiol. 2015;8:1403–12.
•• Corrado D, Wichter T, Link MS, Hauer RN, Marchlinski FE, Anastasakis A, et al. Treatment of arrhythmogenic right ventricular cardiomyopathy/dysplasia: an international task force consensus statement. Circulation. 2015;132:441–53. This is the most updated consensus statement with precise recommendations for RF ablation in ARVD patients.
Te Riele AS, Ajijola OA, Shivkumar K, Tandri H. Role of bilateral sympathectomy in the treatment of refractory ventricular arrhythmias in arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circ Arrhythm Electrophysiol. 2016;9:e003713.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Di Biase is a consultant for Stereotaxis, Biosense Webster, Boston Scientific, and St. Jude Medical and has received speaker honoraria/travel from Medtronic, Janssen, Pfizer, EPiEP, and Biotronik.
Dr. Natale has received speaker honoraria from Boston Scientific, Biosense Webster, St. Jude Medical, Biotronik, and Medtronic and is a consultant for Biosense Webster, St. Jude Medical, and Janssen.
Dr. Romero, Dr. Briceño, and Dr. Grushko declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Myocardial Disease
Rights and permissions
About this article
Cite this article
Romero, J., Grushko, M., Briceño, D.F. et al. Radiofrequency Ablation in Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC). Curr Cardiol Rep 19, 82 (2017). https://doi.org/10.1007/s11886-017-0893-3
Published:
DOI: https://doi.org/10.1007/s11886-017-0893-3