Abstract
Cardiovascular disease is the leading cause of morbidity and mortality globally, with diabetes being an independent risk factor. Adequate diabetes management has proven to be resource-intensive, requiring frequent lab work, primary care and specialist visits, and time-consuming record-keeping by the patient and care team. New mobile health (mHealth) technologies have enhanced how diabetes is managed and care is delivered. While more recent work has investigated mHealth devices as complementary tools in behavioral interventions for diabetes prevention and management, little is still known about the effectiveness of mHealth technology as stand-alone intervention tools for reducing diabetes risk. In addition, more work is needed to identify the role of mHealth technology in treating vulnerable populations to ameliorate cardiovascular health disparities. With advances in mobile health technology development for diabetes prevention and management, these modalities will likely play an increasingly prominent role in reducing cardiometabolic risk for the US population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2014, the World Health Organization (WHO) recognized cardiovascular disease (CVD) as the leading cause of morbidity and mortality globally. With diabetes independently and markedly increasing CVD risk, the implementation of improved risk reduction strategies and diabetes interventions deserves prioritization [1]. Adequate management of diabetes has proven to be resource-intensive [2], demanding a concerted and dedicated effort by the patient and a team of health care providers [3]. Historically, this has required frequent primary care and specialist visits and time-consuming record-keeping by the patient and the clinician [4]. Barriers to accessing and affording this level of care restrict many from achieving adequate blood glucose control, and ultimately place patients at greater risk for cardiovascular complications [5]. New mobile health (mHealth) technologies have enhanced how diabetes is managed and care is delivered.
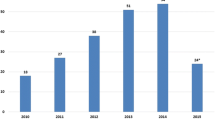
As mHealth technologies expand in capacity and capability, so too are the ways they are integrated into diabetes care. Fifteen years ago, innovative technology-based diabetes prevention and intervention efforts primarily consisted of short message service (SMS) text messaging and internet-based patient portals. SMS messaging tended to be used for medication adherence and appointment reminders, and to deliver motivational messaging [6]. Internet-based interventions had more sophistication allowing for transmission of data between patients and providers, distribution of educational content via an online platform, and delivery of lifestyle interventions [7]. With the advent and widespread uptake of smartphones, wearable devices, and mobile applications (apps), opportunities for real-time health data tracking, tailored feedback, motivational support, and personalized coaching are expanding and improving the ways diabetes is managed, both at home and in clinical settings. As depicted in Fig. 1, mHealth technologies have a place in both diabetes prevention and management, often targeting modifiable health behaviors to ultimately reduce cardiometabolic risk.
The use of mHealth technology in public health interventions and medical care is pervasive in diabetes prevention and management, with several thousand diabetes-related apps available across the Apple iTunes store and Android Market and numerous devices available for tracking cardiovascular health factors (e.g., body weight/body mass index (BMI), dietary intake, physical activity, blood pressure, blood glucose). The purpose of this review is to describe current mHealth technologies being used in diabetes prevention and management and to identify less explored areas where mHealth tools show promise. With the American Heart Association (AHA) recently calling for improved cardiovascular health and risk factor management in youth with diabetes mellitus and among racial/ethnic minority groups, this review places a special focus on these vulnerable populations [8].
Mobile Health Technology in Diabetes Prevention
The emergence of various mHealth offerings has exposed new channels for delivering and complementing existing interventions that target lifestyle factors associated with increased cardiometabolic risk (e.g., physical activity, sedentary time, sleep, dietary intake). The two most prominent mHealth technologies used in type-2 diabetes prevention, to date, include wearable activity trackers and mobile applications, as defined in Table 1. While we will highlight how activity trackers and mobile apps are currently being used in type-2 diabetes prevention, we will also describe key studies demonstrating their use in prevention of disease progression among those diagnosed with diabetes. Key interventions using mHealth technology for diabetes prevention are provided in Table 2.
Wearable Devices for Diabetes Prevention
Wearable activity monitors are among the most prevalent type of wearable device used in technology-based interventions targeting diabetes risk factors, likely due to their accessibility, cost-effectiveness, and their ability to incorporate effective, evidence-based behavior change techniques (e.g., self-monitoring, feedback, goal-setting) [9]. These devices provide real-time measures of physical activity and daily/weekly feedback via a monitor display, accompanying application, e-mail message, or text message.
While no existing wearable activity monitor studies have assessed the association between device use and diabetes outcomes, some activity monitors have been evaluated as an intervention tool for facilitating weight management, increasing physical activity, and decreasing sedentary time [10–12]. One study targeted sedentary time among overweight women by providing a Fitbit® activity monitor and issuing an alert via the device when sedentary time lasted longer than a specified period [13]. Preliminary evidence from this study and others [14•] suggests that wearable activity monitors may increase physical activity, decrease sedentary time, and facilitate short-term weight loss when used in behavioral interventions, particularly in interventions grounded in behavior change theory [8]. However, limited data exists to support wearable activity monitors as an independent intervention modality to reduce diabetes risk [8]. Furthermore, data on user engagement are limited despite participant engagement being a critical factor for physical activity and weight loss intervention success [8].
Despite high uptake of commercially available wearable activity monitors among the public, most of these monitors lack an empirical foundation, thus contributing to limitations in diabetes prevention. Many have yet to be tested for efficacy, with most studies reporting on usability, acceptability, and feasibility [15–17]. Furthermore, most have only gauged usability at the stage of implementation, rather than engaging the users at each step from intervention development to implementation as demonstrated by Yingling and colleagues in a community-based setting [15].
Mobile Applications for Diabetes Prevention
The ubiquity of smartphones and devices has extended diabetes prevention from clinical settings to an individual’s daily environment. In 2014, the Pew Research Center reported that 81 % of households with an annual income above $75,000/year and 47 % of households with an income below $30,000/year owned a smartphone [18]. For those at risk for diabetes, smartphone devices offer a platform for health tracking and monitoring. Health tracking is often recommended in lifestyle interventions, as it has been shown to raise awareness of behavior trends and improve health outcomes [19]. A 2013 report by the Pew Research Center found that 69 % of US adults track at least one health indicator such as weight, diet, or exercise routine, highlighting the potential impact of mobile apps for self-monitoring [20]. In this section, we outline key studies of existing mobile applications targeting weight loss, dietary intake, or physical activity/sedentary behavior for preventing the onset or worsening of diabetes.
Mobile Applications Targeting Weight Loss
Prior studies suggest that technology-delivered interventions, including e-mail-, SMS-, or Internet-based interventions can provide comparable weight reductions to in-person weight loss interventions [8, 21], despite in-person sessions being touted as a necessary intervention component to maximize weight loss [22, 23]. Consequently, the 2013 American Heart Association/American College of Cardiology/The Obesity Society (AHA/ACC/TOS) obesity treatment guidelines endorsed technology-delivered weight loss interventions as an acceptable alternative to in-person interventions [24]. These technology-based interventions appear to be most effective when they include similar components to traditional weight loss interventions, including use of a structured program, self-monitoring, feedback and communication with a qualified interventionist, social support, and individual tailoring [25]. However, a 2013 review found that few evidence-based behavior change strategies were actually present in existing weight loss mobile apps, with strategies that help to improve motivation, reduce stress, and assist with problem solving, often missing [26].
Weight loss interventions combining in-person and remote delivery have produced clinically significant reductions in weight [27•, 28•]. One randomized controlled trial (RCT) converted the 16 in-person sessions from the evidence-based Diabetes Prevention Program (DPP) to 6 in-person sessions supplemented with a mobile app and pedometer [27•]. This intervention led to significant weight reductions, lowered blood pressure, increased physical activity, and reduced saturated fat intake, potentially reducing cardiometabolic risk [27•]. There have been mixed results for weight loss interventions delivered solely by smartphone or mobile application. Block and colleagues reported on an algorithm-driven diabetes prevention intervention that was delivered 100 % remotely via the Internet and mobile phone [28•]. Though this intervention improved glycemic control, body weight, BMI, and waist circumference, it is unknown what feature(s) may have contributed to improved health outcomes, a common finding among multi-factorial, technology-delivered interventions. While this 100 % device-delivered intervention showed promise in producing clinically significant weight reduction, a recent RCT suggests otherwise. Despite high intervention engagement and study retention, the smartphone-delivered weight loss intervention for at-risk young adults did not lead to weight loss relative to a control group given written material on healthy lifestyles [29•]. These mixed results suggest that interventionists may need to couple the enhanced smartphone function, such as location and sensing capabilities, with social support and human interaction components of in-person coaching to produce significant diabetes risk reduction.
Mobile Applications Targeting Dietary Intake
A number of mobile apps are available for managing the diet of an individual at risk for or managing diabetes. As demonstrated in the DPP, maintaining a log of foods (type and amount) consumed daily may lead to reduction of diabetes risk, when coupled with an intensive behavioral intervention [22]. Mobile apps are one tool for making everyday diet logging easier and more convenient [30, 31].
Among users with type 2 diabetes, diet logging on a mobile app appears easier and less time-consuming than a paper-based system [32]. Use of an app-based food log has also been shown to improve both diet quality and hemoglobin A1c (HbA1c) in patients with type 2 diabetes [33, 34, 35••, 36]. Most app-based food logs offer various ways to input foods consumed and, after entry, often populate the app with calculated micro- and macronutrient composition of entered foods. With advanced cameras available on most smartphones, manual entry of foods can potentially be replaced with photographs. In comparisons of text-based and image-based entry methods, users report being more likely to continue using the image-based tool than the text-based tool, which tend to be more accurate than the patient’s recollection of foods consumed [37, 38]. Photo-based diet tracking apps have been found to include few evidence-based strategies to improve dietary intake despite showing promise to increase self-efficacy and empowerment among users [39]. Hales and colleagues recently highlighted the need for photo diet tracking apps to incorporate known effective behavior strategies, such as self-regulation, for healthy eating interventions [40].
Advances in image recognition show potential for estimating food quantity, volume, and type; however, these features remain in development and have yet to be studied broadly. At present, no recommendations can be made on the effectiveness of a mobile app as a stand-alone intervention tool for improving dietary intake and reducing diabetes risk; however, these apps may act as a complementary tool to improve self-monitoring among patients at risk for or managing diabetes.
Mobile Applications Targeting Physical Activity
Little is known about the use of mobile apps for content delivery in physical activity interventions [8, 41], particularly with regards to the feasibility and acceptability of apps promoting active lifestyles in individuals with type 2 diabetes [42]. For those physical activity-related apps that have been studied, few are based on health behavior change theories, and evidence-based physical activity recommendations are rarely considered [42, 43]. Among physical activity interventions that have used mobile apps, most have reported increases in physical activity levels with the use of technology, although these studies have been limited by small sample sizes [41, 44]. A 2014 review of smartphones and their viability for measuring and influencing physical activity called for future studies to “utilize randomized controlled trial research designs, larger sample sizes, and longer study periods to better explore the physical activity measurement and intervention capabilities of smartphones,” yet data remain limited on mobile app use for improving physical activity levels among those at risk for or with diabetes [41].
Mobile Health Technology in Type-2 Diabetes Management
Due to its complex and chronic nature, diabetes management requires continuous medical care and ongoing patient self-management to reduce the risk of short-term and long-term cardiovascular complications. For the patient, self-care is multidimensional, requiring a range of activities, including tracking blood glucose levels, adhering to medications, and receiving routine diabetes education and medical attention. As outlined in Table 1, mHealth technologies are prominent in diabetes management as non-invasive and invasive diabetes medical devices (e.g., blood glucose meters, insulin pumps), self-management mobile apps, and apps for bidirectional data sharing between patients and providers. Key interventions incorporating mHealth technology for diabetes management are described in Table 2.
Wearable Devices for Diabetes Management
Non-invasive Medical Devices
Self-monitoring of blood glucose plays an important role in improving glycemic control, as it guides long-term treatment and allows for necessary insulin dose changes between physician visits [45]. Non-invasive glucose monitoring (i.e., requiring no finger-pricking or subcutaneous needle insertion) aims at making self-monitoring less painful and inconvenient. Several non-invasive technologies have been investigated (e.g., near-infrared spectroscopy, reverse iontophoresis). Although non-invasive devices have been FDA-approved since 2001, no non-invasive glucose-sensing devices are commercially available due to problems with unreliable readings, skin irritation, and significant lag times between measured values and “true” blood glucose levels [46]. For example, contact lenses have recently been explored as a medium for glucose-sensing. These devices use fluorescence to measure glucose levels in tears, but have yet to overcome problems of varying glucose levels between eyes, irritation, inaccurate representations of serum glucose, and unreliable energy sources [46, 47].
Invasive Medical Devices
Invasive technology for continuous glucose monitoring (CGM) offers several commercially available options. This technology was introduced in 1999, and in 2015, devices were available from Animas, Dexcom, and Medtronics Diabetes. These devices couple a blood glucose sensor (placed in the subcutaneous fat) with a device that displays and stores the measurements. The sensor measures glucose levels in the interstitial fluid several times per minute and transmits an average of the readings to the receiving device every few minutes. In several short-term studies in patients with type 2 diabetes, CGM was associated with reduced HbA1c levels, increased time in normal glycemic range, and reduced hypoglycemic episodes [48–54]. An RCT comparing the effects of real-time CGM and an internet blood glucose monitoring system among insulin-treated patients with type 2 diabetes found that CGM improved HbA1c in the first 6 months, but the effect did not persist over the next 6 months [52]. Although standard of care guidelines are beginning to consider which patients would benefit most from CGM, the frequency of calibration, short sensor lifespan, and monitor invasiveness have limited CGM’s appeal [55].
Mobile Applications for Diabetes Management
Physical activity, healthy eating, medication adherence, monitoring, self-management problem solving, risk reduction, and healthy coping were recently cited as the seven “essential behaviors for improving diabetes mellitus self-management” [56]. Thousands of mobile applications exist today that offer options for supporting these behaviors and encouraging improved diabetes self-management, with the options growing daily [57]. The available apps typically include options for blood glucose tracking, insulin dosing, diabetes education and training, or transmission of data to a health care professional. While most diabetes management apps are available at no cost, some charge a flat fee or subscription fee. Despite numerous mobile health-tracking options for patients managing diabetes, a clinical study found that only few adults with type 2 diabetes used apps, though many reported self-monitoring with other methods [58].
Mobile Applications for Blood Glucose Tracking
Glucose monitoring is one of the most common components of apps designed for patients with diabetes [59]. Most blood glucose monitoring apps present blood glucose levels and blood glucose trends over time. Most apps require manual entry of information, while others receive transmitted data from an external device (e.g., glucometers or accelerometers) through a USB connection or low-energy Bluetooth. Some apps also offer a data upload feature that allows for direct sharing.
A few studies found improvements in HbA1c in those who used a glucose monitoring app in conjunction with receiving weekly text messages [60, 61] or real-time communication from health professionals [34]. However, to date, most studies on glucose monitoring apps do not report glucose or HbA1c values at baseline or as an outcome. Regarding acceptability, patients are generally in favor of using an app to aid with blood glucose self-monitoring, especially when data is automatically synchronized with a glucometer [62, 63]. One review found that most glucose monitoring apps, regardless of endorsement or certification from an accrediting body, receive good scores from reviewers [57]. App use does not appear to be dependent on age, sex, or education, as all groups report similar likelihood of using the app [64], but new apps are being developed to address potential age-specific usability issues among older populations [65].
Mobile Applications for Diabetes Education
Receiving continuous diabetes-specific education is a priority in diabetes self-management recommendations [4]. Apps that provide educational material on diabetes-related topics may provide relatively basic lessons on diabetes care and self-management [66]. Unfortunately, a recent review found that the educational component in most diabetes-related apps is not evidence-based. For instance, only 5 % of the applications surveyed provided personalized education on interpretation of the data entered by the user in regards to important characteristics such as age and gender. This is in contrast to the 2016 guidelines, which recommend that education be tailored for a patient based on the patient’s preferences, needs, and values [67, 68]. Furthermore, data are limited on the effectiveness of educational apps for diabetes and their cost-effectiveness [69].
Mobile Applications for Data Sharing
Although most of the mobile apps are designed only for the patient’s perspective (also known as “patient facing”), several apps exist that enable data sharing between the patient and physician, allowing for the physician’s involvement in treatment decision-making. These apps allow users to e-mail or export logged or objectively measured data into a file that can be shared with health care professionals, family members, or caregivers. This allows physicians to visualize trends in blood glucose and make necessary adjustments to treatment in real-time. A 2016 RCT of a diabetes self-management app with bidirectional data sharing demonstrated that older adults with type 2 diabetes experienced significant improvements in HbA1c over 1 year when compared to those receiving usual care [70••]. Physicians also tend to find data sharing favorable, as seen in one study of a device that shared patients’ glucose trends with a physician [71]. When sharing data with the patient, providers should be considerate of the usefulness and complexity of the data shared, as to not confuse patients and resultantly overburden the provider [72]. The effect of electronic health record-connected mobile applications on diabetes management will likely remain unknown until key privacy, regulation, and security issues are addressed.
Mobile Health in Type 2 Diabetes Among Vulnerable Populations
Children/Adolescents
With the prevalence of type 2 diabetes significantly increased in the pediatric population, children and adolescents are a vulnerable population in need of early lifestyle interventions to reduce diabetes risk. Mobile health tools present an opportunity to intervene, as mobile devices are already readily accessible to most children and adolescents [73], and studies show that younger patients with diabetes are more likely to use mHealth tools [74]. Mobile apps are one of the more frequently used mHealth technologies by children and adolescents, with studies suggesting that children are willing to use diabetes apps and use them frequently [75]. The frequent use of diabetes apps may be attributed to the fact that many children find them beneficial [75, 76], with many including games for increased engagement [77]. For example, a small study investigating the use of a glucometer and synchronized mobile app in children and adolescents with diabetes found that those who experienced decreases in HbA1c levels directly attributed the improvement to use of the mHealth tools as part of the study [78]. Another study demonstrated that adolescents who used a glucometer connected to the mobile app bant (2010–2012 University Health Network) increased the frequency of glucose monitoring compared to their baseline monitoring [79, 80]. In addition to demonstrated improvements in self-monitoring, improvements in child-parent relationships around diabetes management have been attributed to use of mHealth tools in interventions [81, 82]. While mHealth tools show promise for improving diabetes self-management among children and adolescents, improvements in health outcomes, particularly HbA1c and glycemic control, have not been found consistently in existing studies, and there remains a lack of data about individual apps and features that make them most effective.
Racial/Ethnic Minorities
Racial and ethnic minority populations experience significantly higher rates of diabetes and are disproportionately affected by diabetes-related cardiovascular complications [83, 84]. Mobile devices provide the opportunity to reach diverse, at-risk populations in need of health interventions who appear to be adopting these devices as their primary method of connectivity [18]. Furthermore, in a 2014 review, Kumanyika et al. [85] highlighted the potential of mHealth interventions in addressing obesity and obesity-related chronic disease in racial/ethnic minority adults, and called for evidence to inform the development of mHealth-based interventions. Yet, mHealth-delivered interventions targeting racial/ethnic minorities at-risk for or managing diabetes are still lacking, despite several studies identifying a high level of interest among these groups in using mHealth for managing diabetes [86, 87]. Furthermore, results from these few studies appear mixed. While one study demonstrated an association between high levels of social support and the use of mHealth tools for diabetes self-care among African American adults [88], another found that an mHealth-enabled weight loss intervention improved outcomes in Hispanics and non-Hispanic Whites, but showed no effect in African Americans [89].
A robust body of literature points to community-based participatory research (CBPR) approaches for promoting healthy lifestyles and reducing cardiometabolic risk in racial/ethnic minority communities [90]. Interventions designed with CBPR principles often focus on a research topic of importance to the community, ensuring that intervention strategies are compatible with the needs, behaviors, and beliefs about health in the target community. The evaluation of mHealth technology for targeting cardiometabolic risk factors and managing diabetes in high-risk, minority populations is a critically important first step in developing diabetes prevention and management strategies to reduce health disparities. Though few studies use CBPR principles to engage a high-risk target population during intervention design and development, Yingling and colleagues demonstrated that engaging the targeted community in the process may aid in early identification of issues, suggestions, and preferences when integrating mHealth tools (i.e., a wearable device for physical activity promotion) in an intervention [15]. As mHealth tools advance, so too will the need for understanding how to design effective and sustainable mHealth-enabled interventions that are tailored to the specific needs of at-risk racial/ethnic minority communities.
Conclusions
Mobile health-enabled tools are clearly pervasive in diabetes prevention and management, with wearable devices and mobile applications most prominent. Both wearable devices and mobile applications have potential as complementary tools in behavioral interventions targeting those at risk for or managing diabetes. Wearable devices and mobile applications currently appear to be most successful when used as part of an intervention grounded in behavioral theory. However, mHealth technology needs to be studied more rigorously to acquire a sound empirical basis before integrating widely in interventions. While much of the recent work investigates mHealth devices as a complementary tool in interventions, little is still known about the effectiveness of mHealth modalities as stand-alone intervention tools for reducing diabetes risk. Future studies investigating mHealth technology in diabetes prevention and management require randomized controlled trial designs, larger sample sizes, study cohorts that include a wider range of age groups and are more ethnically diverse, and longer study durations to better understand their feasibility, acceptability and effectiveness in sustaining behavior change long-term across disparate populations. Specifically, more work is needed to identify the role of mHealth technology in treating vulnerable populations and ameliorating cardiovascular health disparities. As mobile health technology development and utilization advances, this technology will likely play an increasingly prominent role in reducing cardiometabolic risk in the US population.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mendis S. Global status report on noncommunicable diseases 2014. Switzerland: World Health Organization; 2014.
Zhuo X, Zhang P, Barker L, et al. The lifetime cost of diabetes and its implications for diabetes prevention. Diabetes Care. 2014;37(9):2557–64.
Wagner EH. The role of patient care teams in chronic disease management. Br Med J. 2000;320(7234):569.
Bodenheimer T, Lorig K, Holman H, et al. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–75.
Zgibor JC, Songer TJ. External barriers to diabetes care: addressing personal and health systems issues. Diabetes Spectr. 2001;14(1):23–8.
Fjeldsoe BS, Alison L, et al. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med. 2009;36(2):165–73.
Ramadas A, Quek KF, Chan C, et al. Web-based interventions for the management of type 2 diabetes mellitus: a systematic review of recent evidence. Int J Med Inform. 2011;80(6):389–405.
Burke LE, Ma J, Azar KM, et al. Current science on consumer use of mobile health for cardiovascular disease prevention a scientific statement from the American Heart Association. Circulation. 2015;132(12):1157–213.
Lyons EJ, Lewis ZH, Mayrsohn BG, et al. Behavior change techniques implemented in electronic lifestyle activity monitors: a systematic content analysis. J Med Int Res. 2014;16(8):e192.
Pellegrini CA, Verba SD, Otto AD, et al. The comparison of a technology‐based system and an in‐person behavioral weight loss intervention. Obesity. 2012;20(2):356–63.
Lewis ZH, Lyons EJ, Jarvis JM, et al. Using an electronic activity monitor system as an intervention modality: a systematic review. BMC Public Health. 2015;15:585. doi:10.1186/s12889-015-1947-3.
Rastogi R, Rajaraman SA, Dehennis A. A wearable continuous glucose monitoring system with built-in activity tracking. Diabetes Technol Ther. 2014;16:A65.
Finkelstein J, Bedra M, Li X, et al. Mobile app to reduce inactivity in sedentary overweight women. Stud Health Technol Inform. 2015;216:89–92.
•Barwais FA, Cuddihy TF, Tomson LM. Physical activity, sedentary behavior and total wellness changes among sedentary adults: a 4-week randomized controlled trial. Health Qual Life Outcomes. 2013;11:183. doi:10.1186/1477-7525-11-183. This study demonstrated the use of an activity monitor to decrease sedentary time in obese populations at risk for diabetes.
Yingling LR, Brooks AT, Wallen GR, et al. Community engagement to optimize the use of web-based and wearable technology in a cardiovascular health and needs assessment study: a mixed methods approach. JMIR Mhealth Uhealth. 2016;4(2):e38. doi:10.2196/mhealth.4489.
Mercer K, Li M, Giangregorio L, et al. Behavior change techniques present in wearable activity trackers: a critical analysis. JMIR Mhealth Uhealth. 2016;4(2):e40.
Arsand E, Muzny M, Bradway M, et al. Performance of the first combined smartwatch and smartphone diabetes diary application study. J Diabetes Sci Technol. 2015;9(3):556–63. doi:10.1177/1932296814567708.
Pew Research Center. The smartphone difference. 2015. Available at: http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/.
Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 1998;13:623–49.
Fox S, Duggan M. Tracking for health. Pew Research Center’s Internet & American Life Project. 2013.
Siopis G, Chey T, Allman-Farinelli M. A systematic review and meta-analysis of interventions for weight management using text messaging. J Hum Nutr Diet. 2015;28:1–15. doi:10.1111/jhn.12207.
Knowler WC, Barrett-Connor E, Fowler SE, et al. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403.
Wadden TA, Webb VL, Moran CH, et al. Lifestyle modification for obesity new developments in diet, physical activity, and behavior therapy. Circulation. 2012;125(9):1157–70.
Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS Guideline for the management of overweight and obesity in adults. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25_PA):2985–3023. doi:10.1016/j.jacc.2013.11.004.
Khaylis A, Yiaslas T, Bergstrom J, et al. A review of efficacious technology-based weight-loss interventions: five key components. Telemedicine J e-Health. 2010;16(9):931–8. doi:10.1089/tmj.2010.0065.
Pagoto S, Schneider K, Jojic M, et al. Evidence-based strategies in weight-loss mobile apps. Am J Prev Med. 2013;45(5):576–82.
•Fukuoka Y, Gay CL, Joiner KL, et al. A novel diabetes prevention intervention using a mobile app: A randomized controlled trial with overweight adults at risk. Am J Prev Med. 2015;49(2):223–37. doi:10.1016/j.amepre.2015.01.003. Overweight and obese older adults at risk for diabetes had significant decreases in weight, demonstrating the successful use of mHealth technologies in this population.
•Block G, Azar KM, Romanelli RJ, et al. Diabetes prevention and weight loss with a fully automated behavioral intervention by email, web, and mobile phone: a randomized controlled trial among persons with prediabetes. J Med Int Res. 2015;17(10):e240. doi:10.2196/jmir.4897. This study demonstrated the importance of including several mHealth technologies to induce weight loss, but was unable to demonstrate long-term effects compared to control groups.
•Svetkey LP, Batch BC, Lin PH, et al. Cell phone intervention for you (CITY): a randomized, controlled trial of behavioral weight loss intervention for young adults using mobile technology. Obesity. 2015;23(11):2133–41. doi:10.1002/oby.21226. This study showed that despite high study retention, a mobile health technology-delivered intervention did not lead to weight loss.
Lowe J, Linjawi S, Mensch M, et al. Flexible eating and flexible insulin dosing in patients with diabetes: results of an intensive self-management course. Diabetes Res Clin Pract. 2008;80(3):439–43. doi:10.1016/j.diabres.2008.02.003.
Samann A, Muhlhauser I, Bender R, et al. Glycaemic control and severe hypoglycaemia following training in flexible, intensive insulin therapy to enable dietary freedom in people with type 1 diabetes: a prospective implementation study. Diabetologia. 2005;48(10):1965–70. doi:10.1007/s00125-005-1905-1.
Kósa I, Vassányi I, Pintér B, et al. Clinical experiences with a mobile diet logging application. Eur J Prev Cardiol. 2014;21(2):41.
Waki K, Fujita H, Uchimura Y, et al. Dialbetics: smartphone-based self-management for patients with type 2 diabetes. J Diabetes Sci Technol. 2012;6(2):A187.
Waki K, Fujita H, Uchimura Y, et al. DialBetics: a novel smartphone-based self-management support system for type 2 diabetes patients. J Diabetes Sci Technol. 2014;8(2):209–15. doi:10.1177/1932296814526495.
••Waki K, Fujita H, Uchimura Y, et al. Diabetics: smart phone-based self-management for type 2 diabetes patients. J Diabetes Sci Technol. 2013;7(1):A151. This study demonstrated that a smartphone app with glucose tracking and provider feedback could be used to significantly decrease HbA1c.
Waki K, Aizawa K, Kato S, et al. DialBetics with a multimedia food recording tool, Foodlog: smartphone-based self-management for type 2 diabetes. J Diabetes Sci Technol. 2015;9(3):534–40. doi:10.1177/1932296815579690.
Rhyner D, Loher H, Dehais J, et al. Carbohydrate estimation by a mobile phone-based system versus self-estimations of individuals with type 1 diabetes mellitus: a comparative study. J Med Internet Res. 2016;18(5):e101. doi:10.2196/jmir.5567.
Aizawa K, Maeda K, Ogawa M, et al. Comparative study of the routine daily usability of Foodlog: a smartphone-based food recording tool assisted by image retrieval. J Diabetes Sci Technol. 2014;8(2):203–8. doi:10.1177/1932296814522745.
Froisland DH, Arsand E. Integrating visual dietary documentation in mobile-phone-based self-management application for adolescents with type 1 diabetes. J Diabetes Sci Technol. 2015;9(3):541–8. doi:10.1177/1932296815576956.
Hales S, Dunn C, Wilcox S, et al. Is a picture worth a thousand words? Few evidence-based features of dietary interventions included in photo diet tracking mobile apps for weight loss. J Diabetes Sci Technol. 2016. doi:10.1177/1932296816651451.
Bort-Roig J, Gilson ND, Puig-Ribera A, et al. Measuring and influencing physical activity with smartphone technology: a systematic review. Sports Med. 2014;44(5):671–86. doi:10.1007/s40279-014-0142-5.
McMillan KA, Kirk A, Hewitt A, et al. A systematic and integrated review of mobile-based technology to promote active lifestyles in people with type 2 diabetes. J Diabetes SciTechnol. 2016. doi:10.1177/1932296816656018.
Conroy DE, Yang CH, Maher JP. Behavior change techniques in top-ranked mobile apps for physical activity. Am J Prev Med. 2014;46(6):649–52. doi:10.1016/j.amepre.2014.01.010.
Puig-Ribera A, Bort-Roig J, Gonzalez-Suarez AM, et al. Patterns of impact resulting from a ‘sit less, move more’ web-based program in sedentary office employees. PLoS ONE. 2015;10(4):e0122474. doi:10.1371/journal.pone.0122474.
Polonsky WH, Fisher L, Schikman CH, et al. Structured self-monitoring of blood glucose significantly reduces A1C levels in poorly controlled, noninsulin-treated type 2 diabetes: results from the Structured Testing Program study. Diabetes Care. 2011;34(2):262–7. doi:10.2337/dc10-1732.
Vashist SK. Non-invasive glucose monitoring technology in diabetes management: a review. Anal Chim Acta. 2012;750:16–27. doi:10.1016/j.aca.2012.03.043.
Bandodkar AJ, Wang J. Non-invasive wearable electrochemical sensors: a review. Trends Biotechnol. 2014;32(7):363–71. doi:10.1016/j.tibtech.2014.04.005.
Deiss D, Bolinder J, Riveline JP, et al. Improved glycemic control in poorly controlled patients with type 1 diabetes using real-time continuous glucose monitoring. Diabetes Care. 2006;29(12):2730–2.
Bailey TS, Zisser HC, Garg SK. Reduction in hemoglobin A1C with real-time continuous glucose monitoring: results from a 12-week observational study. Diabetes Technol Ther. 2007;9(3):203–10.
Garg S, Zisser H, Schwartz S, et al. Improvement in glycemic excursions with a transcutaneous, real-time continuous glucose sensor: a randomized controlled trial. Diabetes Care. 2006;29(1):44–50.
Tamborlane WV, Beck RW, Bode BW, et al. Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med. 2008;359(14):1464–76.
Schütz-Fuhrmann I, Cvach S, Stadler M, et al. Role of continuous glucose monitoring (CGM) with IPRO2 in the routine management of diabetes. Diabetes Technol Ther. 2013;15:A72–3.
Mdingi C, Rastogi R, Dehennis. Clinical benefit in glycemic control using a long-term, implantable, continuous glucose monitoring system in a 90-day feasibility study. Diabetes. 2014;63:A213–4.
Yoo HJ, Ang HG, Park SY, et al. Use of a real time continuous glucose monitoring system as a motivational device for poorly controlled type 2 diabetes. Diabetes Res Clin Pract. 2008;82(1):73–9.
Kim HS, Shin JA, Chang JS, et al. Continuous glucose monitoring: current clinical use. Diabetes Metab Res Rev. 2012;28 Suppl 2:73–8. doi:10.1002/dmrr.2346.
Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metabol Disord. 2013;12(1):1.
Issom DZ, Woldaregay AZ, Chomutare T, et al. Mobile applications for people with diabetes published between 2010 and 2015. Diabetes Manage. 2015;5(6):539–50.
Tanenbaum ML, Bhatt HB, Thomas VA, Wing RR. Use of self-monitoring tools in a clinic sample of adults with type 2 diabetes. Translational Behavioral Medicine. 2016. doi:10.1007/s13142-016-0418-4.
Arnhold M, Quade M, Kirch W. Mobile applications for diabetics: a systematic review and expert-based usability evaluation considering the special requirements of diabetes patients age 50 years or older. Ed. Gunther Eysenbach. J Med Int Res. 2014;16:e104.
Kirwan M, Vandelanotte C, Fenning A, et al. Diabetes self-management smartphone application for adults with type 1 diabetes: randomized controlled trial. J Med Internet Res. 2013;15(11):e235. doi:10.2196/jmir.2588.
Kim HS, Choi W, Baek EK, et al. Efficacy of the smartphone-based glucose management application stratified by user satisfaction. Diabetes Metab J. 2014;38(3):204–10. doi:10.4093/dmj.2014.38.3.204.
Rao A, Hou P, Golnik T, et al. Evolution of data management tools for managing self-monitoring of blood glucose results: a survey of iPhone applications. J Diabetes Sci Technol. 2010;4(4):949–57.
Harris LT, Tufano J, Le T, et al. Designing mobile support for glycemic control in patients with diabetes. J Biomed Inform. 2010;43(5 Suppl):S37–40. doi:10.1016/j.jbi.2010.05.004.
Becker S, Brandl C, Meister S, et al. Demographic and health related data of users of a mobile application to support drug adherence is associated with usage duration and intensity. PLoS ONE. 2015;10(1):e0116980. doi:10.1371/journal.pone.0116980.
Borrero AF, Vasques J, Vargas R. Implementation of a mobile application to promote self-care in elder diabetic patients. VI Latin American Congress on Biomedical Engineering CLAIB 2014, Paraná, Argentina 29, 30 & 31 October 2014; 2015: Springer International Publishing. Available at: http://springerlink.bibliotecabuap.elogim.com/chapter/10.1007%2F978-3-319-13117-7_203.
Hawkes CP, Hindmarsh PC, McCarthy M. Structured feedback in the development of the first educational smartphone application (Pumps4Kids) for Insulin Pump Starts. Diabetes. 2013: American Diabetes Association Available at: http://diabetes.diabetesjournals.org/content/diabetes/62/Supplement_1/A621.full.pdf.
Chomutare T, Fernandez-Luque L, Arsand E, et al. Features of mobile diabetes applications: review of the literature and analysis of current applications compared against evidence-based guidelines. J Med Internet Res. 2011;13(3):e65. doi:10.2196/jmir.1874.
American Diabetes Association. Standards of Medical Care in Diabetes 2016. Diabetes Care. 2016;39 Suppl 1:S1–112. doi:10.2337/dc16-S003.
Shah VN, Garg SK. Managing diabetes in the digital age. Clin Diabetes Endocrinol. 2015;1(1):1–7. doi:10.1186/s40842-015-0016-2.
••Quinn CC, Shardell MD, Terrin ML, et al. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011;34(9):1934–42. doi:10.2337/dc11-0366. A mobile phone application that communicated with the provider demonstrated the potential for patient-provider communication in mobile applications.
Park HS, Cho H, Kim HS. Development of cell phone application for blood glucose self-monitoring based on ISO/IEEE 11073 and HL7 CCD. Healthc Inform Res. 2015;21:83–94.
Frazetta D, Willet K, Fairchild R. A systematic review of smartphone application use for type 2 diabetic patients. Online Journal of Nursing Informatics (OJNI). 2012;16(3). Available at: http://ojni.org/issues/?p=2041.
Fox S, Duggan M. Mobile health 2012. Washington: Pew Internet & American Life Project; 2012.
Blondon KS, Hebert PL, Ralston JD. An exploration of the potential reach of smartphones in diabetes. In AMIA Annual Symposium Proceedings (Vol. 2014, p. 289). American Medical Informatics Association. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4419894.
Vaala SE, Hood KK, Laffel L, et al. Use of commonly available technologies for diabetes information and self-management among adolescents with type 1 diabetes and their parents: a web-based survey study. Interac J Med Res. 2015;4(4):e24.
Frøisland DH, Årsand E, Skårderud F. Improving diabetes care for young people with type 1 diabetes through visual learning on mobile phones: mixed-methods study. J Med Int Res. 2012;14(4):e111.
Swartwout E, El-Zein A, Deyo P, et al. Use of gaming in self-management of diabetes in teens. Curr Diabetes Rep. 2016;16(7):1–13.
Rothenberg R, Zetelski M, Sivitz J, et al. Use of smartphone, a cellular glucometer and social media app in the management of type 1 DM in the adolescent population: the future of diabetes care. Horm Res Paediatr. 2015;84:374–5.
Cafazzo JA, Casselman M, Hamming N, et al. Design of an mHealth app for the self-management of adolescent type 1 diabetes: a pilot study. J Med Internet Res. 2012;14(3):e70.
Cafazzo JA, Casselman M, Katzman DK, et al. Bant: an mHealth App for adolescent type I diabetes—a pilot study. J Adolesc Health. 2012;50(2):S77–8.
Muzny M, Chomutare T, Johansen SG, et al. Ambient light as an information mediator for parents to children with diabetes. Diab Technol Ther. 2015;17:A128.
Carroll AE, DiMeglio LA, Stein S, et al. Contracting and monitoring relationships for adolescents with type 1 diabetes: a pilot study. Diabetes Technol Ther. 2011;13(5):543–9.
Ayanian JZ, Landon BE, Newhouse JP, et al. Racial and ethnic disparities among enrollees in Medicare Advantage plans. N Engl J Med. 2014;371(24):2288–97.
Parrinello CM, Rastegar I, Godino JG, et al. Prevalence of and racial disparities in risk factor control in older adults with diabetes: the Atherosclerosis Risk in Communities Study. Diabetes Care. 2015;38(7):1290–8.
Kumanyika SK, Whitt-Glover MC, Haire-Joshu D. What works for obesity prevention and treatment in Black Americans? Research directions. Obes Rev. 2014;15 Suppl 4:204–12. doi:10.1111/obr.12213.
St. George SM et al. Access to and interest in using smartphone technology for the management of type 1 diabetes in ethnic minority adolescents and their parents. Diabetes Technol Ther. 2016;18:104–9.
Mayer L, Fei K, Buquez B, et al. Mobile technology access, usage, and attitudes among low-income, minority individuals in East Harlem, NY Victoria. J Gen Intern Med. 2015;30:S210.
Payne BD, Oster R, Shelley JP, et al. Association between diabetes self-care and perceived support in a sample of low-income African Americans. J Gen Intern Med. 2015;30:S103.
Dang S, Oropesa L, Byrne MM, et al. Race/ethnic disparities in weight and glycemia in older adults receiving lifestyle interventions via peer-leaders with or without mobile enhancement for diabetes prevention and management. J Am Geriatr Soc. 2014;62:S216.
Coughlin SS, Smith SA. A review of community-based participatory research studies to promote physical activity among African Americans. J Ga Public Health Assoc. 2016;5(3):220–7.
Yang CC, Hsu YL. A review of accelerometry-based wearable motion detectors for physical activity monitoring. Sensors. 2010;10:7772–88.
Acknowledgments
The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the U.S. Department of Health and Human Services. Funding for TP-W and LY is provided through the Division of Intramural Research of the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health (NIH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jacob Hartz, Leah Yingling, and Tiffany M. Powell-Wiley declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
This article is part of the Topical Collection on Diabetes and Cardiovascular Disease
Rights and permissions
About this article
Cite this article
Hartz, J., Yingling, L. & Powell-Wiley, T.M. Use of Mobile Health Technology in the Prevention and Management of Diabetes Mellitus. Curr Cardiol Rep 18, 130 (2016). https://doi.org/10.1007/s11886-016-0796-8
Published:
DOI: https://doi.org/10.1007/s11886-016-0796-8