Abstract
Cardiac hybrid imaging combines different imaging modalities in a way where both modalities equally contribute to image information. Hybrid positron emission tomography-computed tomography (PET-CT) imaging is a promising tool for evaluation of coronary artery disease (CAD) because it enables detection of coronary atherosclerotic lesions by CT angiography and their consequences on myocardial blood flow by PET perfusion in a single study. This appears to offer superior diagnostic accuracy in patients with intermediate risk for CAD compared with stand-alone imaging. Novel, commercially available hybrid scanners containing PET and magnetic resonance as well as development of targeted probes to evaluate molecular and cellular disease mechanisms are expected to provide many new applications for cardiac hybrid imaging. This article focuses on the advantages of cardiac hybrid imaging in the detection of CAD in light of currently available clinical data and discusses the potential future applications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiac hybrid imaging combines different imaging modalities in a way that both modalities equally contribute to image information [1]. The added value of hybrid imaging originates from the spatial correlation of structural and functional information into one fused image. This should provide incremental information beyond that offered by attenuation correction or side-by-side interpretation of the data sets [1, 2]. Hybrid scanners combining positron emission tomography (PET) with high-resolution multi-detector computed tomography (CT) are becoming the standard for almost all commercially available systems. The newest generation of hybrid scanners offers combination of PET with magnetic resonance (MR) imaging. Co-registration of images is immediate and reliable with integrated scanners due to capability to perform PET and either CT or MR image acquisition almost simultaneously with the patient’s position fixed. However, software-based co-registration of image data sets from stand-alone scanners is also reliable and feasible. Dedicated cardiac fusion software packages are now commercially available, allowing hybrid imaging with an excellent interobserver reproducibility and short processing durations. Furthermore, image transfer processes to workstations performing co-registration are currently simple and fast.
The main clinical application of cardiac hybrid imaging is anatomical and functional evaluation of coronary lesions in patients with suspected or documented coronary artery disease (CAD). Multidetector CT can now provide an angiographic visualization of the coronary arteries with high temporal and spatial resolution, offering an acceptable and attractive noninvasive alternative to invasive coronary angiography [3]. However, anatomical imaging, noninvasive or invasive, does not accurately indicate whether the detected coronary narrowing causes ischemia, which is the cause of symptoms of the patients and the target of the revascularization therapy. Prior to elective invasive coronary angiography, a test for ischemia is strongly recommended by professional practice guidelines [4]. Both earlier observational studies and recent randomized trials indicate that revascularization procedures performed in patients with documented ischemia reduce total mortality through reduction of ischemia [4–7]. The prospective nuclear substudy of the COURAGE trial showed that percutaneous coronary interventions were more effective in reducing myocardial ischemia than optimal medical treatment alone, and that the extent of reduction was associated with the prognosis of the patient [6]. In the randomized prospective FAME trial, measurement of fractional flow reserve (FFR) that detects hemodynamic significance of stenosis based on intracoronary pressure gradient, prior to percutaneous coronary intervention, resulted in a significant 35% reduction in overall mortality and rate of myocardial infarction compared with anatomic evaluation of stenosis alone [7]. Because discrepancies between the apparent anatomical severity of a lesion and its hemodynamic significance are common, especially in stable CAD [8], functional evaluation of intermediate stenosis is essential for therapeutic decisions.
Hybrid imaging combining PET and multidetector CT angiography (CTA) allow combining morphologic information about coronary artery stenosis location and degree with functional information on pathophysiologic lesion severity. The new PET/MR scanners offer attractive possibilities for combining measures of ventricular function, perfusion, viability, and infarct scar for evaluation of ischemic heart disease. There are also other promising future applications that involve molecular imaging of cardiac targets, and these may further enhance the clinical utility of hybrid imaging using PET/CT or PET/MR. This article presents the benefits of hybrid imaging in light of currently available clinical data and discusses future possibilities.
Features of Stand-Alone Imaging Modalities in Detection of CAD
Coronary CTA
Coronary CTA has become an established noninvasive method for anatomic detection of coronary atherosclerotic plaques and luminal stenosis. Current multislice devices coupled with up-to-date acquisition protocols allow robust and reproducible assessment of coronary atherosclerosis with high temporal and spatial resolution as well as acceptable radiation dose [3]. Multiple single-center studies [3] as well as multicenter studies [9–11] have demonstrated high diagnostic accuracy of CTA for the identification of coronary artery stenosis that is greater than 50% by invasive angiography. In the ACCURACY trial, 230 patients underwent CTA and invasive coronary angiography. On a patient-based analysis, the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were 95%, 83%, 64%, and 99%, respectively, to detect ≥50% stenosis [11]. With the exception of the CORE-64 trial, the studies have consistently shown that CTA has a particularly high NPV close to 100%. This makes CTA an excellent tool for exclusion of CAD in patients with low-to-intermediate pretest likelihood of disease [3, 4, 9, 11].
The assessment of the severity of coronary artery stenosis can be challenging by coronary CTA. Typically, it tends to overestimate the degree of intermediate stenosis, especially in the presence of dense calcified plaques (blooming artifact) resulting in lower PPV [3]. Furthermore, evaluation of stenosis in vessels with small diameter and in the presence of image artifacts caused by irregular or fast heart rate is challenging [3]. Studies comparing coronary CTA and single photon emission computed tomography (SPECT) perfusion imaging have indicated that only 40% to 65% of the stenoses classified as significant by coronary CTA are associated with myocardial ischemia [12–15]. Similarly, the correlation comparing the stenosis severity by coronary CTA and invasive quantitative coronary angiography has been only modest [16, 17].
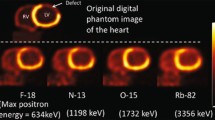
PET Perfusion Imaging
Myocardial perfusion imaging is an extensively validated noninvasive method for the detection of myocardial ischemia [18]. Myocardial ischemia is depicted by reduced uptake of the perfusion tracer during exercise or pharmacological stress. Myocardial perfusion imaging has high diagnostic accuracy for the detection of angiographically significant CAD. Data from a large number of studies using either SPECT or PET perfusion imaging indicate that normal myocardial perfusion in patients with intermediate to high likelihood of CAD predicts a very low rate of cardiac death or nonfatal myocardial infarction (1%/year) [19, 20]. Moreover, patients with less reversible ischemia on perfusion imaging have a survival advantage with medical therapy rather than revascularization, whereas those with more extensive ischemia are more likely to benefit from invasive procedures [5, 6]. These features make myocardial perfusion imaging a strong technique to guide selection of candidates for cardiac catheterization and possible revascularization.
Myocardial perfusion PET offers certain advantages compared with SPECT. PET can measure myocardial radioactivity concentrations with better spatial and contrast resolutions and it has accurate, well-validated attenuation correction. As a result, image artifacts caused by soft tissue attenuation are rare and perfusion images of the myocardium are of high quality. The diagnostic accuracy of perfusion PET for the detection of angiographically significant anatomical CAD is very high (both sensitivity and specificity ≥90%) [20]. A unique feature of PET is that myocardial blood flow can be quantified in mL/min/g at rest and during pharmacologically induced hyperemia using PET [20–23]. The clinical benefits of measuring myocardial perfusion in absolute terms have been highlighted in a recent clinical study comparing diagnostic accuracy of quantitative and relative analysis of 15O-water PET perfusion imaging in patients with suspected CAD [24] as well as in earlier studies [25, 26]. The studies have shown that quantitative analysis of myocardial blood flow by PET is particularly helpful for revealing the true extent of CAD in patients with multivessel disease and for detection of balanced multivessel disease [23–26]. Compared with SPECT, the use of myocardial perfusion PET imaging is low. However, due to increase in the number of PET scanners and development of techniques and perfusion tracers that do not require on-site cyclotron its use is expected to increase [20, 27].
A challenge for interpretation of PET perfusion imaging is caused by the lack of anatomical information of the coronary tree in the images. Thus, perfusion imaging alone is unable to differentiate microvascular dysfunction from epicardial stenosis as a cause of abnormally low perfusion. The knowledge on individual coronary anatomy would also help assignment of perfusion defects to certain coronary lesions, because the standard distribution of myocardial perfusion territories does not correspond to the true coronary anatomy in a large number of patients, particularly in the vascular territories of the left circumflex and right coronary artery [27, 28]. In a recent study, disagreement between the standard myocardial vascular territories and the individual obtained using hybrid perfusion and CTA was found in 9% of all segments. Finally, a limitation of myocardial perfusion PET is that it reveals coronary lesions that induce perfusion defects, but do not exclude the presence of subclinical nonobstructive coronary atherosclerosis that may also have prognostic significance [29].
Cardiac MRI
Cardiac MR has become an important tool for investigating the morphology and function of the cardiovascular system [30]. The strengths of MRI are that it provides high resolution images of the myocardium with high blood-tissue contrast that enables accurate measurement of ventricular volumes without the need for using geometrical models. Detection of CAD by MR is based on evaluation of reversible wall motion abnormalities during dobutamine stress, but more recently also on visualization of myocardial perfusion by T1-weighted imaging after gadolinium contrast injection. A unique feature offered by MR is the detection of myocardial tissue abnormalities, particularly necrosis or scar, using the late gadolinium enhancement imaging technique [30, 31].
Hybrid imaging combining MR with PET or CT is potentially desirable for many reasons, including lack of additional ionizing radiation, good tissue characterization properties of MR, possibility to detect myocardial infarct scar with MR in parallel to viable tissue with fluorodeoxyglucose PET, and possibility to do simultaneous (isochronic) acquisition with MRI and PET. Hybrid scanners containing MR and PET scanners have been available for short period of time and there are still technical issues to be resolved before their potential in cardiac applications can be fully explored [32•, 33]. However, there are clinical examples that novel fast-perfusion sequences (kt-SENSE) allow the ability to obtain full-coverage volumetric perfusion data of the left ventricle, which permits simple fusion with three-dimensional volume-rendered CTA into hybrid images [34].
Advantages of Hybrid Imaging in the Detection of CAD
Clinical Data on Hybrid Imaging
The clinical feasibility of integrated hybrid imaging of CTA and myocardial perfusion was first documented in 2005 with the use of 13N-NH3 PET and 4-slice CT scanner [35]. This and subsequent studies have confirmed the complementary role of both techniques in the evaluation of patients with suspected CAD, resulting in improved specificity and PPV in the detection of angiographically significant stenosis [35–37, 38••, 39]. The largest of these studies using integrated PET and 64-detector CT prospectively enrolled 107 patients with chest pain with intermediate likelihood of CAD and compared hybrid 15O-H2O PET and CTA versus CTA alone in the detection of hemodynamically significant coronary stenosis [38••]. Hybrid imaging was technically feasible and scan time remained short, because single 6-min PET scan during adenosine stress was used. The hemodynamic significance of stenoses was defined by quantitative coronary angiography including FFR measurement of intracoronary pressure gradient when feasible. Although both PET and CTA alone demonstrated high (97%) NPV, CTA alone was suboptimal in assessing the severity of stenosis (PPV 76%) and perfusion imaging alone could not separate microvascular disease from epicardial stenoses (PPV 77%) in all patients. The use of PET-CTA significantly improved diagnostic accuracy to 98%. Sensitivity, specificity, PPV, and NPV were 93%, 99%, 96%, and 99%, respectively. This indicates that noninvasive hybrid PET-CTA imaging is a highly accurate diagnostic method for the detection of hemodynamically significant CAD compared with PET or CTA alone. The promising results of hybrid PET-CT imaging in the detection of CAD need to be confirmed in prospective, multicenter studies involving different tracers and scanner types.
The incremental value of co-registration and fusion of stand-alone acquired CTA and myocardial perfusion images compared with the side-by-side analysis for the diagnosis of obstructive CAD has been addressed in several studies [40–42]. The results indicate that fusion of perfusion and CTA added diagnostic information in approximately one third of patients resulting in improved diagnostic performance compared with the side-by-side analysis [40–42]. In one study, the number of lesions with equivocal hemodynamic relevance was reduced especially in patients with multivessel disease, intermediate severity stenoses, and diseased side branches [40]. Another study pointed to improved sensitivity in patients with multivessel disease [41]. A recent study implemented automated CTA-guided SPECT contour and territory adjustments found that hybrid imaging particularly improved diagnostic accuracy in the left circumflex and right coronary artery territories [42].
The prognostic value of CTA combined with perfusion imaging over myocardial perfusion imaging alone was demonstrated in a trial including 541 patients at intermediate risk of CAD [43••]. After adjusting for clinical risk factors, obstructive plaque visualized by CTA and abnormal myocardial perfusion scan were independent predictors of late events, with significant incremental improved prediction of risk by the combination of the two modalities compared with either modality alone. An annual event rate of 1% was found in those with concordantly normal CTA and perfusion, and conversely those with concordantly abnormal CTA and perfusion had an event rate of 9%. The findings were confirmed in another, more recent study using SPECT-CT hybrid imaging [44]. The prognostic value of combining quantitative analysis of myocardial perfusion by PET with CTA will be interesting topic for future studies.
In addition to luminal stenosis, CT allows visualization of the coronary vessel wall, thereby providing information on the presence and composition of eccentric nonobstructive plaques. Although the clinical significance of atherosclerotic plaque characterization by CT is still investigational, evidence is accumulating that some features, such as plaque size, low attenuation, spotty calcifications, and eccentric vascular remodeling, can provide prognostic information on the risk of future cardiac events in stable CAD patients [43••, 45, 46].
Clinical Impact of Hybrid Imaging
Challenges in the detection of CAD and the advantages provided by hybrid imaging with PET/CT are summarized in Table 1. Currently it remains largely unknown what kind of patients should undergo such integrated examinations for clinical effectiveness and minimization of costs and radiation dose [2]. One of the strengths of hybrid imaging is that it can guide selection of the most appropriate treatment strategy (medical conservative vs percutaneous vs surgical revascularization). Therefore, it can be anticipated that the patients with multivessel disease are most likely to benefit from hybrid imaging that can be helpful for the evaluation of the extent of disease and localize the culprit flow-limiting lesions as shown in Fig. 1. Thus, the proportion of patients needing dual scanning depends on the characteristics of the patient population, especially the pretest likelihood of CAD. An observational study indicated that the finding of flow-limiting coronary stenosis by noninvasive hybrid imaging had impact on the frequency of subsequent revascularization [47]. However, further studies are needed to evaluate whether imaging-guided use of interventions will also influence clinical outcome of patients.
Detection of culprit lesion by hybrid positron emission tomography/computed tomography (PET/CT) angiography imaging in a patient with multivessel coronary artery disease (CAD). A 58-year-old lady with multiple risk factors of CAD (hypercholesterolemia, hypertension, and previous smoking), atypical chest pain, and asymptomatic ST-depression in exercise test. Multiplanar reconstructions of CT angiography images of the right coronary artery (RCA) and the left anterior descending coronary artery (LAD) show multiple atherosclerotic lesions associated with luminal narrowing. Hybrid volume-rendered images of CT angiography and myocardial perfusion during adenosine stress as assessed by 15O-labeled water PET show normal (> 2.5 mL/g/min) or mildly reduced (2.0–2.5 mL/g/min) perfusion as seen in yellow and green colors, respectively, in the LAD territory (left image). Stress myocardial perfusion was severely reduced as seen in blue color (< 1.5 mL/g/min) in the areas supplied by the RCA (right image). Invasive coronary angiography showed three-vessel disease, but the most severe stenosis was in the distal RCA corresponding with the noninvasive findings. After percutaneous coronary intervention of the single stenosis patient became asymptomatic
In clinical practice, a sequential diagnostic approach is often applied, with additional scans performed only if the results of the initial modality are equivocal. For example, the hemodynamic severity of intermediate stenosis in CTA can be confirmed by immediate perfusion imaging or the culprit lesion responsible for perfusion defect can be localized by CTA. In sequential approach, the order of the scans can vary depending on the pretest likelihood. Because of the very high NPV of CTA, patients with low to moderate pretest likelihood of CAD could undergo CTA as the first-line examination followed by confirmation of ischemia by perfusion imaging only in those patients with suspicion of obstructive CAD. Conversely, in the presence of higher likelihood of CAD, the fraction of patients with obstructive disease is high and, therefore, perfusion as the first-line examination would make sense. CTA would be needed only if anatomical information is needed over positive perfusion result. Naturally, both of these approaches have limitations. In the first option, knowledge of coronary function or microvascular disease is missed. In the second option, preclinical atherosclerotic disease is not detected.
Radiation Exposure
In addition to costs, an obvious concern related to hybrid imaging is patient radiation dose that requires careful consideration of the needs and benefits of imaging [48]. It is currently assumed that there is a linear relationship between radiation dose and the risk of cancer. The effective patient radiation dose from cardiac CT varies widely depending on the protocol, instrumentation, and patient size [48, 49]. Due to improvements in image acquisition protocols (eg, the introduction of electrocardiogram (ECG)-dependent tube current modulation, body mass index–adapted tube voltage modulation, and prospective ECG-triggered sequential scanning), the radiation exposure from CTA has diminished considerably in the clinical practice [49–51]. It has been reported that the use of new iterative reconstruction enables further reduction of the radiation dose by 30% to 50% [52]. An advantage of the short half-life of PET perfusion tracers is that the radiation exposure is much lower than that related to SPECT perfusion imaging [38••]. The radiation doses from PET perfusion imaging are ranging from 1 to 2 mSv [38••, 48]. Recent developments in detector technology as well as the omission of rest study in the presence of normal stress study may allow further reduced radiation exposure. An advantage of MR over CT and PET imaging is that it does not cause exposure to ionizing radiation.
Novel Applications of Hybrid Imaging
Molecular Imaging
Although traditional imaging is based on detection of changes in the anatomy and physiologic features, such as blood flow or contractile function, cardiovascular molecular imaging aims at visualization and measurement of biological processes at the molecular and cellular levels. Molecular imaging has provided techniques and new targeted probes to better understand the pathophysiologic mechanism underlying cardiovascular diseases [53, 54]. Examples of clinical problems that might benefit from molecular imaging include the identification of vulnerable atherosclerotic plaques before rupture and subsequent myocardial infarction [55, 56], detection of biomechanisms that precede left ventricular remodeling and development of heart failure [57, 58], and the assessment of risk of ventricular arrhythmias by neuronal imaging [59]. Additionally, molecular imaging has great potential to facilitate the discovery and development of novel therapies through improved target identification and implementation of more efficient end points. Owing to high sensitivity and availability of tracers with low risk of toxicity, PET is the leading imaging technique to proceed with translation of molecular imaging into clinical trials [53, 60]. Molecular imaging depends on hybrid imaging approaches, where the nuclear imaging component is used for molecular targeting seen as a “hot spot” and the CT or other anatomical imaging modality is used for localization of the molecular signal. For example, hybrid PET and CT or MR scanners offer the possibility to integrate targeted PET images with high-resolution morphologic images provided by CT or MR to obtain an anatomic distribution of the probe and account for partial volume errors that would cause underestimation of the true regional radiotracer activity.
Conclusions
Cardiac hybrid imaging has rapidly developed into a useful technique for the clinician. The combination of morphologic imaging of coronary arteries using multidetector CTA and functional imaging of myocardial perfusion using PET, SPECT, and also recently cardiac MR is very powerful noninvasive imaging method that provides comprehensive information both for diagnosis and decision making for treatment of CAD. Hybrid imaging appears to offer superior diagnostic information in patients with intermediate risk for disease compared with stand-alone imaging. However, further studies are needed to confirm the clinical impact and cost effectiveness of this technique. Ongoing multicenter trials, such as SPARC and EVINCI, are expected to provide important information on these issues in the near future. The new PET/MR scanners and targeted molecular probes have provided interesting possibilities for hybrid imaging that are developing toward clinical application.
Abbreviations
- ACCURACY:
-
Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography
- CORE-64:
-
Coronary Evaluation Using Multi-Detector Spiral Computed Tomography Angiography Using 64 Detectors
- COURAGE:
-
Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation
- EVINCI:
-
Evaluation of Integrated Cardiac Imaging in Ischemic Heart Disease
- FAME:
-
Fractional Flow Reserve Versus Angiography for Guiding PCI in Patients with Multivessel Evaluation
- SPARC:
-
The study of myocardial perfusion and coronary anatomy imaging roles in CAD
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Knuuti J,. Kaufmann PA. Hybrid imaging: PET–CT and SPECT–CT. In: Zamorano JL, Bax JJ, Rademakers FE, Knuuti J, editors. The ESC textbook of cardiovascular imaging. Springer; 2009. p. 89–101.
Flotats A, Knuuti J, Gutberlet M, Marcassa C, Bengel FM, Kaufmann PA, et al. Hybrid cardiac imaging: SPECT/CT and PET/CT. A joint position statement by the European Association of Nuclear Medicine (EANM), the European Society of Cardiac Radiology (ESCR) and the European Council of Nuclear Cardiology (ECNC). Eur J Nucl Med Mol Imaging. 2011;38:201–12.
Schroeder S, Achenbach S, Bengel F, Burgstahler C, Cademartiri F, de Feyter P, et al. Cardiac computed tomography: indications, applications, limitations, and training requirements: report of a Writing Group deployed by the Working Group Nuclear Cardiology and Cardiac CT of the European Society of Cardiology and the European Council of Nuclear Cardiology. Eur Heart J. 2008;29:531–56.
Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, et al. Guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2010;31:2501–55.
Shaw LJ, Berman DS, Maron DJ, Mancini GB, Hayes SW, Hartigan PM, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation. 2008;117:1283–91.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107:2900–7.
Tonino PA, Fearon WF, De Bruyne B, Oldroyd KG, Leesar MA, Ver Lee PN, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010;55:2816–21.
Gould KL. Identifying and measuring severity of coronary artery stenosis. Quantitative coronary arteriography and positron emission tomography. Circulation. 1988;78:237–45.
Meijboom WB, Meijs MF, Schuijf JD, Cramer MJ, Mollet NR, van Mieghem CA, et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol. 2008;52:2135–44.
Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med. 2008;359:2324–36.
Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008;52:1724–32.
Schuijf JD, Wijns W, Jukema JW, et al. Relationship between noninvasive coronary angiography with multi-slice computed tomography and myocardial perfusion imaging. J Am Coll Cardiol. 2006;48:2508–14.
Hacker M, Jakobs T, Hack N, et al. Sixty-four slice spiral CT angiography does not predict the functional relevance of coronary artery stenoses in patients with stable angina. Eur J Nucl Med Mol Imaging. 2007;34:4–10.
Sato A, Tamura M, Ohigashi H, et al. Quantitative measures of coronary stenosis severity by 64-slice CT angiography and relation to physiologic significance of perfusion in nonobese patients: comparison with stress myocardial perfusion imaging. J Nucl Med. 2008;49:564–72.
Gaemperli O, Schepis T, Velenta I, et al. Functionally relevant coronary artery disease: comparison of 64-section CT angiography with myocardial perfusion SPECT. Radiology. 2008;248:414–23.
Leber AW, Knez A, von Ziegler F, et al. Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol. 2005;46:147–54.
Mejiboom WB, van Mieghem CA, Mollet NR, et al. 64-slice computed tomography coronary angiography in patients with high-intermediate, or low pretest probability of significant coronary artery disease. J Am Coll Cardiol. 2007;50:1469–75.
Underwood SR, Anagnostopoulos C, Cerqueira M, Ell PJ, Flint EJ, Harbinson M, et al. Myocardial perfusion scintigraphy: the evidence. Eur J Nucl Med Mol Imaging. 2004;31:261–91.
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation. 1998;97:535–43.
Di Carli MF, Hachamovitch R. New technology for noninvasive evaluation of coronary artery disease. Circulation. 2007;115:1464–80.
Bergmann SR, Fox KA, Rand AL, McElvany KD, Welch MJ, Markham J, et al. Quantification of regional myocardial blood flow in vivo with H215O. Circulation. 1984;70:724–33.
Hutchins GD, Schwaiger M, Rosenspire KC, Krivokapich J, Schelbert H, Kuhl DE. Noninvasive quantification of regional blood flow in the human heart using N-13 ammonia and dynamic positron emission tomographic imaging. J Am Coll Cardiol. 1990;15:1032–42.
Knuuti J, Kajander S, Maki M, Ukkonen H. Quantification of myocardial blood flow will reform the detection of cad. J Nucl Cardiol. 2009;16:497–506.
Kajander SA, Joutsiniemi E, Saraste M, Pietilä M, Ukkonen H, Saraste A, Sipilä HT, Teräs M, Mäki M, Airaksinen J, Hartiala J, Knuuti J. Clinical value of absolute quantification of myocardial perfusion with 15O-water in coronary artery disease. Circ Cardiovasc Imaging 2011; [Epub ahead of print].
Parkash R, deKemp RA, Ruddy TD, Kitsikis A, Hart R, Beauchesne L, et al. Potential utility of rubidium 82 pet quantification in patients with 3-vessel coronary artery disease. J Nucl Cardiol. 2004;11:440–9.
Yoshinaga K, Katoh C, Noriyasu K, Iwado Y, Furuyama H, Ito Y, et al. Reduction of coronary flow reserve in areas with and without ischemia on stress perfusion imaging in patients with coronary artery disease: a study using oxygen 15-labeled water pet. J Nucl Cardiol. 2003;10:275–83.
Nekolla SG, Saraste A. Novel F-18-labeled PET myocardial perfusion tracers: bench to bedside. Curr Cardiol Rep. 2011;13:145–50.
Javadi MS, Lautamaki R, Merrill J, Voicu C, Epley W, McBride G, et al. Definition of vascular territories on myocardial perfusion images by integration with true coronary anatomy: a hybrid PET/CT analysis. J Nucl Med. 2010;51:198–203.
Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364:226–35.
Karamitsos TD, Dall’Armellina E, Choudhury RP, Neubauer S. Ischemic heart disease: comprehensive evaluation by cardiovascular magnetic resonance. Am Heart J. 2011;162:16–30.
Saraste A, Nekolla S, Schwaiger M. Contrast-enhanced magnetic resonance imaging in the assessment of myocardial infarction and viability. J Nucl Cardiol. 2008;15:105–17.
• Büscher K, Judenhofer MS, Kuhlmann MT, Hermann S, Wehrl HF, Schäfers KP, Schäfers M, Pichler BJ, Stegger L. Isochronous assessment of cardiac metabolism and function in mice using hybrid PET/MRI. J Nucl Med 2010;51:1277–84. This is a preclinical demonstration of feasibility of obtaining simultaneous MR and PET cardiac images of myocardial infarction with a prototype MR/PET hybrid scanner with a PET insert.
Nekolla SG, Martinez-Moeller A, Saraste A. PET and MRI in cardiac imaging: from validation studies to integrated applications. Eur J Nucl Med Mol Imaging. 2009;36:S121–30.
Manka R, Kuhn FP, Kuest SM, Gaemperli O, Kozerke S, Kaufmann PA. Hybrid cardiac magnetic resonance/computed tomographic imaging: first fusion of three-dimensional magnetic resonance perfusion and low-dose coronary computed tomographic angiography. Eur Heart J 2011; [epub ahead of print].
Namdar M, Hany TF, Koepfli P, Siegrist PT, Burger C, Wyss CA, et al. Integrated PET/CT for the assessment of coronary artery disease: a feasibility study. J Nucl Med. 2005;46:930–5.
Rispler S, Keidar Z, Ghersin E, Roguin A, Soil A, Dragu R, et al. Integrated single-photon emission computed tomography and computed tomography coronary angiography for the assessment of hemodynamically significant coronary artery lesions. J Am Coll Cardiol. 2007;49:1059–67.
Groves AM, Speechly-Dick ME, Kayani I, Pugliese F, Endozo R, McEwan J, et al. First experience of combined cardiac PET/64-detector CT angiography with invasive angiographic validation. Eur J Nucl Med Mol Imaging. 2009;36:2027–33.
•• Kajander S, Joutsiniemi E, Saraste M, Pietila M, Ukkonen H, Saraste A, Sipila HT, Teras M, Maki M, Airaksinen J, Hartiala J, Knuuti J. Cardiac positron emission tomography/computed tomography imaging accurately detects anatomically and functionally significant coronary artery disease. Circulation 2010;122:603–13. This demonstrated the clinical feasibility and improved diagnostic accuracy of integrated CTA and PET perfusion imaging over either imaging modality alone for the detection of hemodynamically significant coronary stenosis defined by invasive angiography and FFR measurements in patients with intermediate risk of CAD.
Sato A, Nozato T, Hikita H, Miyazaki S, Takahashi Y, Kuwahara T, et al. Incremental value of combining 64-slice computed tomography angiography with stress nuclear myocardial perfusion imaging to improve noninvasive detection of coronary artery disease. J Nucl Cardiol. 2010;17:19–26.
Gaemperli O, Schepis T, Valenta I, Husmann L, Scheffel H, Duerst V, et al. Cardiac image fusion from standalone SPECT and CT: clinical experience. J Nucl Med. 2007;48:696–703.
Santana CA, Garcia EV, Faber TL, Sirineni GK, Esteves FP, Sanyal R, et al. Diagnostic performance of fusion of myocardial perfusion imaging (MPI) and computed tomography coronary angiography. J Nucl Cardiol. 2009;16:201–11.
Slomka PJ, Cheng VY, Dey D, Woo J, Ramesh A, Van Kriekinge S, et al. Quantitative analysis of myocardial perfusion SPECT anatomically guided by coregistered 64-slice coronary CT angiography. J Nucl Med. 2009;50:1621–30.
•• van Werkhoven JM, Schuijf JD, Gaemperli O, Jukema JW, Boersma E, Wijns W, Stolzmann P, Alkadhi H, Valenta I, Stokkel MP, Kroft LJ, de Roos A, Pundziute G, Scholte A, van der Wall EE, Kaufmann PA, Bax JJ. Prognostic value of multislice computed tomography and gated single-photon emission computed tomography in patients with suspected coronary artery disease. J Am Coll Cardiol 2009;53:623–32. This demonstrated the prognostic value of combined CTA and perfusion imaging over myocardial perfusion imaging alone in patients at intermediate risk of CAD.
Pazhenkottil AP, Nkoulou RN, Ghadri JR, Herzog BA, Buechel RR, Küest SM, et al. Prognostic value of cardiac hybrid imaging integrating single-photon emission computed tomography with coronary computed tomography angiography. Eur Heart J. 2011;32:1465–71.
Pundziute G, Schuijf JD, Jukema JW, Boersma E, de Roos A, van der Wall EE, et al. Prognostic value of multislice computed tomography coronary angiography in patients with known or suspected coronary artery disease. J Am Coll Cardiol. 2007;49:62–70.
Motoyama S, Kondo T, Sarai M, Sugiura A, Harigaya H, Sato T, et al. Multislice computed tomographic characteristics of coronary lesions in acute coronary syndromes. J Am Coll Cardiol. 2007;50:319–26.
Pazhenkottil AP, Nkoulou RN, Ghadri J-R, Herzog BA, Kuest SM, Husmann L, Wolfrum M, Goetti R, Buechel RR, Gaemperli O, Luscher TF, Kaufmann PA. Impact of cardiac hybrid single-photon emission computed tomography/computed tomography imaging on choice of treatment strategy in coronary artery disease. Eur Heart J 2011; (in press).
Einstein AJ, Moser KW, Thompson RC, Cerqueira MD, Henzlova MJ. Radiation dose to patients from cardiac diagnostic imaging. Circulation. 2007;116:1290–305.
Hausleiter J, Meyer T, Hermann F, Hadamitzky M, Krebs M, Gerber TC, et al. Estimated radiation dose associated with cardiac CT angiography. JAMA. 2009;301:500–7.
Leipsic J, Labounty TM, Heilbron B, Min JK, Mancini GB, Lin FY, et al. Estimated radiation dose reduction using adaptive statistical iterative reconstruction in coronary CT angiography: the ERASIR study. AJR Am J Roentgenol. 2010;195:655–60.
Husmann L, Valenta I, Gaemperli O, et al. Feasibility of low-dose coronary CT angiography: first experience with prospective ECG-gating. Eur Heart J. 2008;29(2):191–7.
Achenbach S, Marwan M, Ropers D, et al. Coronary computed tomography angiography with a consistent dose below 1 mSv using prospectively electrocardiogram-triggered high-pitch spiral acquisition. Eur Heart J;31(3):340–6.
Saraste A, Nekolla SG, Schwaiger M. Cardiovascular molecular imaging: an overview. Cardiovasc Res. 2009;50:1088–94.
Nahrendorf M, Sosnovik DE, French BA, Swirski FK, Bengel F, Sadeghi MM, et al. Multimodality cardiovascular molecular imaging, part II. Circ Cardiovasc Imaging. 2009;2:56–70.
Rudd JH, Narula J, Strauss HW, Virmani R, Machac J, Klimas M, et al. Imaging atherosclerotic plaque inflammation by fluorodeoxyglucose with positron emission tomography: ready for prime time? J Am Coll Cardiol. 2010;55:2527–35.
Abdelbaky A, Tawakol A. Noninvasive positron emission tomography imaging of coronary arterial inflammation. Curr Cardiovasc Imaging Rep. 2011;4:41–9.
Kramer CM, Sinusas AJ, Sosnovik DE, French BA, Bengel FM. Multimodality imaging of myocardial injury and remodeling. J Nucl Med. 2010;51:107S–21S.
Naresh NK, Ben-Mordechai T, Leor J, Epstein FH. Molecular imaging of healing after myocardial infarction. Curr Cardiovasc Imaging Rep. 2011;4:63–76.
Jacobson AF, Senior R, Cerqueira MD, Wong ND, Thomas GS, Lopez VA, et al. Myocardial iodine-123 meta-iodobenzylguanidine imaging and cardiac events in heart failure. Results of the prospective ADMIRE-HF (AdreView Myocardial Imaging for Risk Evaluation in Heart Failure) study. J Am Coll Cardiol. 2010;55:2212–21.
Knuuti J, Bengel FM. Positron emission tomography and molecular imaging. Heart. 2008;94:360–7.
Acknowledgments
The authors acknowledge financial support from The Academy of Finland Centre of Excellence in Molecular Imaging in Cardiovascular and Metabolic Research, Helsinki, Finland and The Turku Collegium for Science and Medicine of University of Turku, Turku, Finland.
Disclosure
Conflicts of interest: A. Saraste: none; J. Knuuti: has been a consultant for Lantheus Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saraste, A., Knuuti, J. Cardiac PET, CT, and MR: What Are the Advantages of Hybrid Imaging?. Curr Cardiol Rep 14, 24–31 (2012). https://doi.org/10.1007/s11886-011-0231-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-011-0231-0