Abstract
In acute ischemic stroke, time is brain. Current guidelines recommend that the time from arrival at hospital to initiation of administration of tissue plasminogen activator, also known as the door-to-needle (DTN) time, should be 60 min or less. However, DTN times in practice usually exceed this recommended time. The median DTN times from the American Heart Association/American Stroke Association Get With The Guidelines-Stroke program and the multinational Safe Implementation of Treatment in Stroke International Stroke Thrombolysis Register are 75 min and 65 min, respectively. Prehospital factors associated with delays include patient-related factors such as poor recognition of stroke symptoms, poor use of emergency medical services, and complex psychosocial factors. Accurate recognition of stroke symptoms at a dispatcher and paramedic level is associated with shorter onset-to-arrival times. Prenotification of regional stroke centers by paramedics is strongly associated with shorter DTN times. In-hospital delays resulting in prolonged DTN times can be attenuated by having well-defined rapid triage pathways, defined stroke teams, single-call stroke team activation, established code stroke protocols, rapid access to diagnostic imaging, and laboratory services. In this review we summarize factors associated with prolonged DTN times and processes that allow faster onset-to-treatment times. Recent developments in the field are highlighted.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
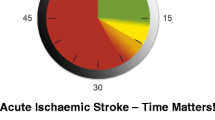
In acute ischemic stroke (AIS), “time is brain” [1, 2]. The seminal National Institute of Neurological Disorders and Stroke Tissue Plasminogen Activator Stroke study established that intravenously administered tissue plasminogen activator (tPA) improves outcomes in AIS in a time-dependent manner [3]. The relationship between shorter treatment time and increased efficacy of intravenously administered tPA has been further clarified in a recent meta-analysis of pooled data from all the trials [4]. The number needed to treat (NNT) with intravenously administered tPA to achieve no stroke-related disability (modified Rankin score 0 or 1) is 4.5 when treatment is within 1.5 h of the symptoms, 9 when treatment is within 1.5-3 h, and 14 when treatment is within 3–4.5 h [5]. Therefore, in AIS a delay of 20 min to treatment initiation would result in the number needed to treat increasing by one patient [6••]. The importance of rapid treatment is reflected in national guidelines for treatment of AIS and the Brain Attack Coalition recommendations that recommend that the time from arrival at the emergency department to initiation of intravenous administration of tPA should be 60 min or less [7–9]. The Brain Attack Coalition recommends that the goal in AIS is to notify the stroke team within 15 min of the arrival of the patient at the emergency department, begin brain imaging within 25 min of arrival, interpret the CT scan within 45 min of arrival, and begin administration of tPA within 60 min of arrival [10••].
Currently, neither North American nor European hospitals are meeting the recommended 60-min door-to-needle (DTN) benchmark consistently [11]. The median DTN times from the American Heart Association (AHA)/American Stroke Association (ASA) Get With The Guidelines-Stroke (GWTG-Stroke) program and the multinational Safe Implementation of Treatment in Stroke International Stroke Thrombolysis Register are 75 min and 65 min, respectively [12, 13••]. Despite a significant increase in the use of tPA following the extension of the treatment window to 4.5 h, less than a third of patients receive tPA within 60 min of arrival at stroke centers [13••, 14, 15]. There remains an urgent need to adopt better strategies to optimize prehospital and in-hospital systems to achieve shorter DTN and onset-to-treatment times.
The goals of this review are to highlight the factors that result in prehospital and in-hospital delays in the treatment of AIS with intravenously administered tPA (Table 1). Furthermore, we aim to highlight pertinent recent improvements in processes involved in the systematic delivery of intravenously administered tPA and enumerate potential future directions that will allow rapid screening and treatment of AIS patients.
Prehospital Delays
The care of AIS patient begins in the prehospital phase. In a comprehensive systematic review, Evenson et al. [16] suggest that this phase accounts for the largest proportion of the delay in receiving thrombolysis. The study of factors related to onset-to-arrival (OTA) times has been impeded by the lack of accurately recorded onset times in up to 50-60 % of cases. Missing onset times in large stroke registries may reflect lack of witnesses of the beginning of the event (e.g., the patient is “found down”), inaccurate history, or incomplete recording of data in the medical record. Additionally, OTA is defined and measured differently across studies, making it difficult to compare findings and to determine the relative importance of predictors of longer OTA times.
Lack of recognition of stroke symptoms by patients or eyewitnesses or failure to immediately call appropriate emergency medical services (EMS) for help are frequently causes of OTA delays. The factors governing help-seeking decisions are complex. Patient factors such as fear, denial, reticence to inconvenience EMS, and the desire to contact family members or friends contribute to OTA delay [17]. Even though most patients and eyewitness are aware of at least one symptom of stroke, with unilateral weakness and speech disturbance most commonly recognized [18•], less than half of stroke patients recognize their own symptoms as being caused by stroke, often attributing their symptoms erroneously to alternative conditions with consequent delays in activating EMS [19–21]. When stroke is suspected, there is a tendency for both patients and eyewitnesses to contact their general practitioner rather than EMS, resulting in increases in OTA times [18•]. Education campaigns can be effective in increasing knowledge of stroke warning signs and reducing OTA times [22, 23]. However, knowledge of stroke symptoms in patients and eyewitnesses is not by itself sufficient to influence appropriate responses in AIS [24], with there being no direct correlation between people with the best stroke knowledge and those with the shortest OTA times [23]. Thus, there exists a discrepancy between theoretical stroke knowledge and translating that knowledge into appropriate behavior in an acute real-world situation. It appears that perceived severity of symptoms is more associated with help-seeking behavior than symptom knowledge [23].
Once the patient or family has called 911, accurate stroke diagnosis by dispatcher services and paramedics at the scene ensures rapid transport to a stroke center, which is vital to the delivery of acute stroke therapy and minimization of OTA delay. Existing dispatcher-level computer algorithms for stroke diagnosis have varying degrees of sensitivity and positive predictive values [25, 26]. Newly developed dispatcher algorithms for stroke emergencies result in improved diagnostic accuracy of dispatchers in identifying strokes [27, 28]. Currently, there is an ongoing prospective study evaluating the diagnostic accuracy of a new dispatcher-level stroke screening tool adapted from the Cincinnati Prehospital Stroke Scale [29]. However, the accuracy of dispatcher screening tools is moderate at best, so paramedics need to be educated to appropriately diagnose suspected stroke, otherwise missed diagnoses will lead to OTA delays. Accurate paramedic stroke recognition is associated with shorter OTA times [30]. The HoPSTO study demonstrated that a multilevel education program improved paramedic diagnostic accuracy, resulting in an increase in the proportion of patients presenting for stroke evaluation within a 3-h window [31]. Validated scales for EMS diagnosis of stroke include the Los Angeles Prehospital Stroke Screen [32] and the Cincinnati Prehospital Stroke Scale [33]. In large urban centers, prehospital protocols for paramedics that allow transport of suspected AIS patients directly to designated stroke centers result in reduced OTA times and significantly improve treatment rates with intravenously administered tPA [34]. The AHA and ASA recommend the establishment of regionalized stroke systems of care that include rapid dispatch and EMS transport of suspected AIS patients to capable hospitals for immediate treatment [35].
In the large nationwide GWTG-Stroke program, shorter OTA times were seen in patients who were transported to hospital by EMS [36••]. EMS-transported patients were more likely to be Caucasian, older, and have a history of coronary artery disease and atrial fibrillation. The South London Stroke Register data identified black ethnicity, living alone, and nighttime stroke onset as associated with increased OTA times [37•]. Furthermore, several studies report that use of EMS [36••, 37•, 38–40], higher stroke severity, and daytime onset are related to shorter OTA times [36••, 37•, 38]. Other factors associated with OTA less than 3 h include presentation to an academic hospital, weekday onset during regular working hours, awakening with deficits, and an altered level of consciousness [36••, 38, 39]. Despite our increasing understanding of factors that result in protracted OTA times, the proportion of early-arriving patients with AIS has stagnated, with no overall change from 2003 to 2009 in the GWTG-Stroke registry [36••]. Renewed efforts may be needed to better educate the public to immediately call 911 when stroke symptoms occur.
Prenotification of hospitals by EMS has been shown to reduce in-hospital delays, the time to assemble the stroke team, lengths of stay, and mortality. Prenotification also increased the proportion of patients treated with intravenously administered tPA, CT completion rates, and CT scan interpretation rates [41, 42•, 43••]. The AHA/ASA, the Brain Attack Coalition, the National Association of EMS Physicians and the National Association of State EMS Directors, and European Stroke Organization guidelines all endorse the practice of EMS prenotification in stroke centers [7, 44–46]. However prenotification rates are suboptimal, with prenotification in only 66 % of AIS patients in GWTG-Stroke; there were wide disparities between hospitals and geographic regions [47••]. The same study identified black race as being associated with lower prenotification rates. Higher rates of prenotification were seen in patients transported to hospitals that did not have an academic affiliation, hospitals with higher intravenously administered tPA volume, and in geographic regions outside northeastern USA. Hospital prenotification by EMS allows a smooth transition between prehospital and in-hospital care of the AIS patient and is essential for achieving reductions in onset to tPA administration times.
In-Hospital Delays
A problem with early arrival, with longer time left within the treatment window, is that there is a well-documented association between longer time remaining to treat and longer DTN time. This inverse relationship between earlier arrival of the patient with AIS at the emergency department and longer DTN times was first reported in the STARS study [48]. Since that report multiple studies have confirmed the tendency of treating physicians to delay initiation of thrombolysis owing to the perception that there is sufficient time prior to the expiration of the thrombolysis window [13••, 49, 50]. In the GWTG-Stroke database, patients arriving in the golden hour, within 1 h of onset of stroke symptoms, received thrombolysis more frequently than those arriving more than 60 min from the time when they were last seen as normal; however, the recommended DTN time of less than 60 min was only achieved in 18 % of eligible patients [50]. Application of standardized and diligently monitored thrombolysis protocols performed by specialized stroke teams can mitigate this effect [51]. Other groups with prolonged DTN times include older patients with particularly high or low scores on the National Institutes of Health Stoke Scale, possibly due to physician uncertainty regarding the beneficial effects of tPA in this patient population [49], Conversely, greater stroke severity in younger patients increases the odds of receiving thrombolysis within the recommended 60-min time window [49, 50].
In-hospital logistics of imaging acquisition, obtaining and processing blood, and the clinical history and examination components contribute to the DTN times. In addition to the appropriate use of EMS as outlined already, the development of stroke code systems and acute stroke teams that can be activated by EMS, community hospitals, or emergency departments of stroke centers has been shown to reduce DTN times [52–56]. Implementation of stroke code systems is associated with a 20 % relative reduction in DTN times, 18 % relative reduction in door-to-imaging (DTI) time, and increased tPA use without compromising safety [57]. Activation of the stroke code is most effective at reducing DTN times when the code activates not only neurologists or stroke specialists, but also other multidisciplinary team members, including EMS, the emergency department, the radiology department, and the nursing staff [55]. Single-call systems or an all-points alarm to activate all stroke team members and a formalized acute stroke triage pathway have been shown to shorten DTN times [58, 59•]. Additionally, patients arriving directly at designated stroke centers as opposed to community hospitals and those centers with a greater annual volume of tPA-treated stroke patients have shorter DTN times [13••, 54].
Inappropriate investigations, such as chest radiographs and nonessential blood tests, performed during the hyperacute management of AIS patients can adversely impact DTN times. Waiting for results of platelet counts, prothrombin time, or partial thromboplastin times prior to initiation of administration of tPA is not necessary unless the patient is taking anticoagulants or there is a suspicion of a coagulopathy [60••]. Interpretation of images by the stroke physician prior to initiation of administration tPA without confirmation from a radiologist appears safe and reduces DTN times [61]. When international normalized ratio (INR) testing is necessary, point-of-care laboratory testing has been proposed to reduce DTN times [62, 63]. For patients taking warfarin, reductions of up to 50 % in the time it takes to make a decision to initiate thrombolysis are possible when using point-of-care testing compared with routine laboratory testing [64•].
The processes surrounding image acquisition and interpretation constitute a large proportion of the DTN time. In GWTG-Stroke, age greater than 70 years, female gender, nonwhite race, history of diabetes, peripheral vascular disease, prosthetic heart valve, arrival more than 60 min after symptom onset, and arrival by private transport (rather than by EMS) was associated with an increase in DTI times [65••]. For most patients hyperacute imaging is not performed within the recommended 25-min DTI time window. Patients with severe neurologic deficits are more likely to have shorter DTI times [65••]. Interestingly, patients who have longer OTA times also have longer DTI times, compounding the delay to thrombolysis [66]. The addition of advanced imaging, i.e., angiography and perfusion imaging prior to thrombolysis, may double the in-hospital delay for patients when compared with patients who only receive a noncontrast head CT scan [6••]. Once a decision to administer tPA has been made by excluding contraindications such as intracranial hemorrhage, unavailability of a drug in the treatment location or unavailability of personnel qualified to administer it can result in further delays and should be avoided [35].
Implementing Processes To Improve Door-to-Needle Times
When Toyota’s lean manufacturing principles and value stream analysis is applied to acute stroke care, significant reductions in onset-to-treatment times have been noted [67••]. In one analysis, routing patients directly for a head CT scan before they go to the patient room, using parallel workflow processes, and implementing point-of-care testing resulted in a 21-min reduction in DTN times and an absolute increase of 26 % in the number of patients being treated within the recommend 60-min window from arrival at hospital [67••]. The improved DTN times and concomitant increases in the rates of patients treated early with thrombolysis did not come at the expense of an increase in hemorrhage rates. A strikingly low median DTN time of 20 min was achieved in Helsinki by implementing multiple concurrent strategies, including education of dispatch personnel and EMS; effective hospital prenotification; taking a history as the patient is en route; computerized order entry; transport directly to the CT suite; relocating the stroke team and intravenous administration of tPA while the patient is in the CT scanner; and point-of care-testing [6••, 68]. Improvement in DTN times in the aforementioned study did not have an associated significant financial cost.
Most of the studies examining preintervention and postintervention effects with OTA or DTN times as an outcome are nonrandomized single-center prospective cohort studies with small sample sizes or large-registry-driven retrospective analyses without a control arm [1, 6••, 13••, 14, 17, 27, 31, 34, 36••, 37•, 41, 55, 57, 58, 59•, 61, 67••]. Table 1 summarizes the interventions most commonly used to reduce DTN times. Although these studies provide valuable insights into the factors that result in prolonged or shortened onset-to-treatment times and strategies that improve the timeliness of thrombolysis, they have several limitations. Small sample sizes and lack of randomization or control groups make it challenging to know if the intervention-related improved process times translate to improved patient outcomes or result in unintended deleterious effects. Nonetheless, currently there are no data to suggest that shorter DTN times are associated with increased risk of tPA-related complications such as symptomatic intracranial hemorrhage [13••]. Many studies used historical controls; however, in the absence of concurrent controls, secular trends cannot be entirely separated from the intervention applied and the protocol implemented. The Hawthorne effect [69], in which study participants change their behavior because they are aware that they are being observed, must be considered when interpreting such studies. In large registries and retrospective analyses, missing data often result in exclusion of some proportion of patients, and it is unclear how this impacts the interpretation of results.
The AHA/ASA Target: Stroke initiative is a national quality improvement program designed to facilitate implementation of best practices for rapid, safe delivery of thrombolysis [10••]. The goal is to speed treatment so that at least 50 % of tPA-treated patients receive tPA within 60 min or less of arrival at hospital. A detailed Target: Stroke tool kit—including protocols, order sets, algorithms, time trackers, and other materials to assist physicians and hospitals—is freely available online at http://www.targetstroke.org.
New Paradigms for Improving Stroke Onset to tPA Administration Times: The Dawn of Point-of-Emergency Thrombolysis
Prehospital and in-hospital delays in AIS care lead to delayed treatment with intravenously administered tPA or an inability to administer the therapy because time has run out. It is estimated that in the USA only 1.8-3.0 % of all ischemic stroke patients are treated with intravenously administered tPA [70, 71]. To allow rapid screening and diagnosis of AIS and reduce prehospital and in-hospital delays, mobile telestroke units, with a CT scanner installed in the ambulance, are feasible and have been deployed [72, 73]. The strategy of diagnosis and treatment of AIS at the emergency site, rather than after arrival at the hospital, is showing promise. Walter et al. [74••] demonstrated that prehospital stroke treatment is safe and results in a median difference of 41 min from alarm to therapy decision. More recently, the PHANTOM-S pilot study reported similar results suggesting that prehospital care in a mobile stroke unit was feasible and safe with onset to tPA administration times of less than 90 min achievable in 48 % of patients [75••]. This radical approach of taking the hospital to the patient is in its infancy but shows promise to substantially increase the rates of intravenous administration of tPA and dramatically reduce prehospital and in-hospital delays. However, it remains to be seen if this approach is sustainable, cost-effective, and feasible outside urban centers. Another challenge is the difficulty in accurately identifying thrombolysis-eligible stroke at dispatch, leading to frequent false-positive activations of the mobile stroke unit for acute stroke mimics.
Conclusions
The exquisite sensitivity of the brain to ischemia necessitates prompt diagnosis and rapid initiation of treatment in AIS patients. Despite several education campaigns and increasing general awareness of stroke, there has been no overall national change in the proportion of patients arriving in early tPA treatment windows. A combination of patient and prehospital care factors is responsible for longer OTA times. This highlights the need for reevaluating current patient and EMS education models with a view to creating interventions that not only improve knowledge but also translate into meaningful changes in patient and provider behaviors. Currently in the USA, Canada, and Europe less that 30 % of eligible AIS patients are treated within the recommended 60 min from arrival at hospital [13••, 14, 15]. From 2003 to 2009 there was little change—less than 10 % improvement—in the proportion of patients treated within 60 min of arrival at hospital [13••]. The AHA/ASA Target: Stroke initiative (http://www.targetstroke.org) provides guidance on enacting strategies to reduce DTN times. Additionally, several single-center studies have highlighted processes that improve DTN times, most notably bypassing the emergency department to transport patients directly to the CT suite, application of Toyota's lean manufacturing principles and value stream analysis to identify inefficiencies in patient flow at an institutional level, and point-of-care INR testing. However, these data are largely from single-center studies, necessitating a multicenter approach to understand factors responsible for in-hospital delays and to study the effects of newly implemented strategies on a system level.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Saver JL. Time is brain–quantified. Stroke. 2006;37(1):263–6.
Vergouwen MD, Algra A, Pfefferkorn T, et al. Time is brain(stem) in basilar artery occlusion. Stroke. 2012;43(11):3003–6.
Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. New Engl J Med. 1995;333(24):1581–7.
Wardlaw JM, Murray V, Berge E, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet. 2012;379(9834):2364–72.
Lees KR, Bluhmki E, von Kummer R, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375(9727):1695–703.
•• Meretoja A, Strbian D, Mustanoja S, Tatlisumak T, Lindsberg PJ, Kaste M. Reducing in-hospital delay to 20 minutes in stroke thrombolysis. Neurology. 2012;79(4):306–13. This article demonstrates the value of using multiple concurrent strategies to reduce DTN times to 20 min.
Alberts MJ, Hademenos G, Latchaw RE, et al. Recommendations for the establishment of primary stroke centers. Brain Attack Coalition. JAMA. 2000;283(23):3102–9.
Adams Jr HP, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007;115(20):e478–534.
Summers D, Leonard A, Wentworth D, et al. Comprehensive overview of nursing and interdisciplinary care of the acute ischemic stroke patient: a scientific statement from the American Heart Association. Stroke. 2009;40(8):2911–44.
•• Fonarow GC, Smith EE, Saver JL, et al. Improving door-to-needle times in acute ischemic stroke: the design and rationale for the American Heart Association/American Stroke Association's Target: Stroke initiative. Stroke. 2011;42(10):2983–9. The AHA/ASA Target: Stroke initiative is a national quality improvement program designed to facilitate implementation of best practices for rapid, safe delivery of thrombolysis. This article outlines time-based tPA treatment related goals and suggests mechanisms to achieve them.
Smith EE, von Kummer R. Door-to-needle times in acute ischemic stroke: how low can we go? Neurology. 2012;79(4):296–7.
Ahmed N, Wahlgren N, Grond M, et al. Implementation and outcome of thrombolysis with alteplase 3–4.5 h after an acute stroke: an updated analysis from SITS-ISTR. Lancet Neurol. 2010;9(9):866–74.
•• Fonarow GC, Smith EE, Saver JL, et al. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke: patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. 2011;123(7):750–8. This article examines the timeliness of tPA administration and factors that result in delay in the largest analysis of its kind of the GWTG-Stroke database. It demonstrates that only a minority of patients are treated within the prescribed 60-min window from arrival at hospital.
Messe SR, Fonarow GC, Smith EE, et al. Use of tissue-type plasminogen activator before and after publication of the European Cooperative Acute Stroke Study III in Get With The Guidelines-Stroke. Circ Cardiovasc Qual Outcomes. 2012;5(3):321–6.
Nadeau JO, Shi S, Fang J, et al. TPA use for stroke in the Registry of the Canadian Stroke Network. Can J Neurol Sci. 2005;32(4):433–9.
Evenson KR, Foraker RE, Morris DL, Rosamond WD. A comprehensive review of prehospital and in-hospital delay times in acute stroke care. Int J Stroke. 2009;4(3):187–99.
Mackintosh JE, Murtagh MJ, Rodgers H, Thomson RG, Ford GA, White M. Why people do, or do not, immediately contact emergency medical services following the onset of acute stroke: qualitative interview study. PloS One. 2012;7(10):e46124.
• Lecouturier J, Murtagh MJ, Thomson RG, et al. Response to symptoms of stroke in the UK: a systematic review. BMC Health Serv Res. 2010;10:157. This article highlights patient factors resulting in OTA delays.
Salisbury HR, Banks BJ, Footitt DR, Winner SJ, Reynolds DJ. Delay in presentation of patients with acute stroke to hospital in Oxford. QJM. 1998;91(9):635–40.
Giles MF, Flossman E, Rothwell PM. Patient behavior immediately after transient ischemic attack according to clinical characteristics, perception of the event, and predicted risk of stroke. Stroke. 2006;37(5):1254–60.
Shah M, Makinde KA, Thomas P. Cognitive and behavioral aspects affecting early referral of acute stroke patients to hospital. J Stroke Cerebrovasc Dis. 2007;16(2):71–6.
Alberts MJ, Perry A, Dawson DV, Bertels C. Effects of public and professional education on reducing the delay in presentation and referral of stroke patients. Stroke. 1992;23(3):352–6.
Teuschl Y, Brainin M. Stroke education: discrepancies among factors influencing prehospital delay and stroke knowledge. Int J Stroke. 2010;5(3):187–208.
Dombrowski SU, Sniehotta FF, Mackintosh J, et al. Witness response at acute onset of stroke: a qualitative theory-guided study. PloS One. 2012;7(7):e39852.
Deakin CD, Alasaad M, King P, Thompson F. Is ambulance telephone triage using advanced medical priority dispatch protocols able to identify patients with acute stroke correctly? Emerg Med J. 2009;26(6):442–5.
Ramanujam P, Guluma KZ, Castillo EM, et al. Accuracy of stroke recognition by emergency medical dispatchers and paramedics—San Diego experience. Prehosp Emerg Care. 2008;12(3):307–13.
Krebes S, Ebinger M, Baumann AM, et al. Development and validation of a dispatcher identification algorithm for stroke emergencies. Stroke. 2012;43(3):776–81.
Bray JE, Martin J, Cooper G, Barger B, Bernard S, Bladin C. An interventional study to improve paramedic diagnosis of stroke. Prehosp Emerg Care. 2005;9(3):297–302.
Govindarajan P, Ghilarducci D, McCulloch C, Pierog J, Bloom E, Johnston C. Comparative evaluation of stroke triage algorithms for emergency medical dispatchers (MeDS): prospective cohort study protocol. BMC Neurol. 2011;11:14.
Mosley I, Nicol M, Donnan G, Patrick I, Kerr F, Dewey H. The impact of ambulance practice on acute stroke care. Stroke. 2007;38(10):2765–70.
Wojner-Alexandrov AW, Alexandrov AV, Rodriguez D, Persse D, Grotta JC. Houston paramedic and emergency stroke treatment and outcomes study (HoPSTO). Stroke. 2005;36(7):1512–8.
Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke. 2000;31(1):71–6.
Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Ann Emerg Med. 1999;33(4):373–8.
Gladstone DJ, Rodan LH, Sahlas DJ, et al. A citywide prehospital protocol increases access to stroke thrombolysis in Toronto. Stroke. 2009;40(12):3841–4.
Schwamm LH, Pancioli A, Acker 3rd JE, et al. Recommendations for the establishment of stroke systems of care: recommendations from the American Stroke Association's Task Force on the Development of Stroke Systems. Circulation. 2005;111(8):1078–91.
•• Tong D, Reeves MJ, Hernandez AF, et al. Times from symptom onset to hospital arrival in the Get With The Guidelines–Stroke program 2002 to 2009: temporal trends and implications. Stroke. 2012;43(7):1912–7. This review of the GWTG-Stroke database outlines factors responsible for delays in onset-to-treatment times and highlights the lack of improvement in OTA times over the study period. Use of EMS, daytime stroke, and higher stroke severity result in shorter OTA times.
• Addo J, Ayis S, Leon J, Rudd AG, McKevitt C, Wolfe CD. Delay in presentation after an acute stroke in a multiethnic population in south London: the South London Stroke Register. J Am Heart Assoc. 2012;1(3):e001685. This article considers the factors related to OTA delays in a multiethnic European population.
Maestroni A, Mandelli C, Manganaro D, et al. Factors influencing delay in presentation for acute stroke in an emergency department in Milan. Italy Emerg Med J. 2008;25(6):340–5.
Morris DL, Rosamond W, Madden K, Schultz C, Hamilton S. Prehospital and emergency department delays after acute stroke: the Genentech Stroke Presentation Survey. Stroke. 2000;31(11):2585–90.
Wojner AW, Morgenstern L, Alexandrov AV, Rodriguez D, Persse D, Grotta JC. Paramedic and emergency department care of stroke: baseline data from a citywide performance improvement study. Am J Crit Care. 2003;12(5):411–7.
Kim SK, Lee SY, Bae HJ, et al. Pre-hospital notification reduced the door-to-needle time for iv t-PA in acute ischaemic stroke. Eur J Neurol. 2009;16(12):1331–5.
• Lin CB, Peterson ED, Smith EE, et al. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes. 2012;5(4):514–22. This is one of several articles demonstrating the strong association between hospital prenotification by EMS and shorter DTN times.
•• McKinney JS, Mylavarapu K, Lane J, Roberts V, Ohman-Strickland P, Merlin MA. Hospital prenotification of stroke patients by emergency medical services improves stroke time targets. J Stroke Cerebrovasc Dis. 2013;22(2):113–8. This is one of several articles demonstrating the strong association between hospital prenotification by EMS and shorter DTN times.
Acker 3rd JE, Pancioli AM, Crocco TJ, et al. Implementation strategies for emergency medical services within stroke systems of care: a policy statement from the American Heart Association/American Stroke Association Expert Panel on Emergency Medical Services Systems and the Stroke Council. Stroke. 2007;38(11):3097–115.
Crocco TJ, Grotta JC, Jauch EC, et al. EMS management of acute stroke–prehospital triage (resource document to NAEMSP position statement). Prehosp Emerg Care. 2007;11(3):313–7.
European Stroke Organisation Executive C, Committee ESOW. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis. 2008;25(5):457–507.
•• Lin CB, Peterson ED, Smith EE, et al. Patterns, predictors, variations, and temporal trends in emergency medical service hospital prenotification for acute ischemic stroke. J Am Heart Assoc. 2012;1(4):e002345. This is one of several articles demonstrating the strong association between hospital prenotification by EMS and shorter DTN times. In addition, the authors examine the factors related to prenotification by EMS in the large GWTG-Stroke database.
Albers GW, Bates VE, Clark WM, Bell R, Verro P, Hamilton SA. Intravenous tissue-type plasminogen activator for treatment of acute stroke: the Standard Treatment with Alteplase to Reverse Stroke (STARS) study. JAMA. 2000;283(9):1145–50.
Mikulik R, Kadlecova P, Czlonkowska A, et al. Factors influencing in-hospital delay in treatment with intravenous thrombolysis. Stroke. 2012;43(6):1578–83.
Saver JL, Smith EE, Fonarow GC, et al. The "golden hour" and acute brain ischemia: presenting features and lytic therapy in >30,000 patients arriving within 60 minutes of stroke onset. Stroke. 2010;41(7):1431–9.
Kohrmann M, Schellinger PD, Breuer L, et al. Avoiding in hospital delays and eliminating the three-hour effect in thrombolysis for stroke. Int J Stroke. 2011;6(6):493–7.
Belvis R, Cocho D, Marti-Fabregas J, et al. Benefits of a prehospital stroke code system. Feasibility and efficacy in the first year of clinical practice in Barcelona, Spain. Cerebrovasc Dis. 2005;19(2):96–101.
Hill MD, Buchan AM. Canadian Alteplase for Stroke Effectiveness Study I, Thrombolysis for acute ischemic stroke: results of the Canadian Alteplase for Stroke Effectiveness Study. CMAJ. 2005;172(10):1307–12.
de la Ossa NP, Sanchez-Ojanguren J, Palomeras E, et al. Influence of the stroke code activation source on the outcome of acute ischemic stroke patients. Neurology. 2008;70(15):1238–43.
Nazir FS, Petre I, Dewey HM. Introduction of an acute stroke team: an effective approach to hasten assessment and management of stroke in the emergency department. J Clin Neurosci. 2009;16(1):21–5.
Hamidon BB, Dewey HM. Impact of acute stroke team emergency calls on in-hospital delays in acute stroke care. J Clin Neurosci. 2007;14(9):831–4.
Tai YJ, Weir L, Hand P, Davis S, Yan B. Does a 'code stroke' rapid access protocol decrease door-to-needle time for thrombolysis? Intern Med J. 2012;42(12):1316–24.
Mehdiratta M, Woolfenden AR, Chapman KM, et al. Reduction in IV t-PA door to needle times using an Acute Stroke Triage Pathway. Can J Neurol Sci. 2006;33(2):214–6.
• Nolte CH, Malzahn U, Kuhnle Y, Ploner CJ, Muller-Nordhorn J, Mockel M. Improvement of door-to-imaging time in acute stroke patients by implementation of an all-points alarm. J Stroke Cerebrovasc Dis. 2013;22(2):149–53. This article demonstrates the utility of a single-call activation system in acute stroke.
•• Jauch EC, Saver JL, Adams Jr HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947. This article provides comprehensive guidelines for management of AIS.
Sattin JA, Olson SE, Liu L, Raman R, Lyden PD. An expedited code stroke protocol is feasible and safe. Stroke. 2006;37(12):2935–9.
Green TL, Mansoor A, Newcommon N, Stephenson C, Stewart E, Hill MD. Reliability of point-of-care testing of INR in acute stroke. Can J Neurol Sci. 2008;35(3):348–51.
Rizos T, Jenetzky E, Herweh C, et al. Point-of-care reversal treatment in phenprocoumon-related intracerebral hemorrhage. Ann Neurol. 2010;67(6):788–93.
• Walter S, Kostopoulos P, Haass A, et al. Point-of-care laboratory halves door-to-therapy-decision time in acute stroke. Ann Neurol. 2011;69(3):581–6. Use of point-of-care INR testing when indicated can result in substantial reduction in DTN times as demonstrated in this article..
•• Kelly AG, Hellkamp AS, Olson D, Smith EE, Schwamm LH. Predictors of rapid brain imaging in acute stroke: analysis of the Get With the Guidelines-Stroke program. Stroke. 2012;43(5):1279–84. This is the largest study examining factors resulting in short DTI times in the national GWTG-Stroke database.
Rose KM, Rosamond WD, Huston SL, Murphy CV, Tegeler CH. Predictors of time from hospital arrival to initial brain-imaging among suspected stroke patients: the North Carolina Collaborative Stroke Registry. Stroke. 2008;39(12):3262–7.
•• Ford AL, Williams JA, Spencer M, et al. Reducing door-to-needle times using Toyota's lean manufacturing principles and value stream analysis. Stroke. 2012;43(12):3395–8. This single-center study demonstrates the usefulness of Toyota's lean manufacturing principles and value stream analysis in identifying institutional inefficiencies in the acute stroke treatment pathway.
Strbian D, Soinne L, Sairanen T, et al. Ultraearly thrombolysis in acute ischemic stroke is associated with better outcome and lower mortality. Stroke. 2010;41(4):712–6.
Wolfe F, Michaud K. The Hawthorne effect, sponsored trials, and the overestimation of treatment effectiveness. J Rheumatol. 2010;37(11):2216–20.
Qureshi AI, Suri MF, Nasar A, et al. Thrombolysis for ischemic stroke in the United States: data from National Hospital Discharge Survey 1999–2001. Neurosurgery. 2005;57(4):647–54. discussion 647–54.
Kleindorfer D, Lindsell CJ, Brass L, Koroshetz W, Broderick JP. National US estimates of recombinant tissue plasminogen activator use: ICD-9 codes substantially underestimate. Stroke. 2008;39(3):924–8.
Kostopoulos P, Walter S, Haass A, et al. Mobile stroke unit for diagnosis-based triage of persons with suspected stroke. Neurology. 2012;78(23):1849–52.
Liman TG, Winter B, Waldschmidt C, et al. Telestroke ambulances in prehospital stroke management: concept and pilot feasibility study. Stroke. 2012;43(8):2086–90.
•• Walter S, Kostopoulos P, Haass A, et al. Diagnosis and treatment of patients with stroke in a mobile stroke unit versus in hospital: a randomised controlled trial. Lancet Neurol. 2012;11(5):397–404. This article, as well as [75••], represents a radical rethinking of how to achieve a significant reduction in DTN times by bringing tPA treatment by ambulance to the patient in the field, eliminating the time required for transportation to the emergency department.
•• Weber JE, Ebinger M, Rozanski M, et al. Prehospital thrombolysis in acute stroke: results of the PHANTOM-S pilot study. Neurol. 2013;80(2):163–8. The authors demonstrate the efficacy and safety of point-of-emergency thrombolysis in the field, prior to transport to the emergency department.
Conflicts of Interest
Jamsheed A. Desai declares no conflicts of interest.
Eric E. Smith declares no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Cardiovascular Disease and Stroke
Rights and permissions
About this article
Cite this article
Desai, J.A., Smith, E.E. Prenotification and Other Factors Involved in Rapid tPA Administration. Curr Atheroscler Rep 15, 337 (2013). https://doi.org/10.1007/s11883-013-0337-5
Published:
DOI: https://doi.org/10.1007/s11883-013-0337-5