Opinion statement
Adjuvant therapy for non-metastatic renal cell carcinoma (RCC) remains controversial. Of the four reported randomized controlled trials evaluating adjuvant vascular endothelial growth factor (VEGF) inhibition, only one met its primary endpoint. The S-TRAC study demonstrated a statistically significant improvement in disease-free survival (DFS) of greater than 1 year with adjuvant sunitinib compared to placebo in patients with high-risk localized RCC and earned it FDA approval. However, the larger ASSURE study which reported first did not find a difference in DFS or overall survival between 1 year of adjuvant sunitinib or sorafenib compared to placebo. Given the discordant results of the two sunitinib studies, two other negative studies of adjuvant targeted therapy with pazopanib and axitinib, the lack of definite overall survival benefit in any study, and the high incidence of treatment-related adverse events with sunitinib, we do not recommend the routine use of adjuvant sunitinib. The decision to offer adjuvant sunitinib should be considered on an individual basis after an informed discussion of the potential toxicities and the risk/benefit ratio. Despite numerous efforts and recently published works, there is a paucity of prognostic and predictive molecular biomarkers in RCC. Further investigation is needed to discover new tools that can enhance the identification of patients who are most likely to benefit from adjuvant treatment beyond pathologic stage. Immune checkpoint inhibitors have great potential to significantly improve outcomes in high-risk localized RCC. Building on their established efficacy in the metastatic setting, several ongoing clinical trials are evaluating their value as single agents or in combination in the neoadjuvant and adjuvant settings. At this time, we recommend participation in clinical trials as the preferred therapeutic option for patients with high-risk, non-metastatic RCC planned for nephrectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal cell carcinoma (RCC) is a frequently diagnosed urologic malignancy, constituting approximately 65,430 cases in 2018 in the USA and over 400,000 new cases globally [1, 2]. For patients with non-metastatic disease, surgical resection via partial or radical nephrectomy is the current standard-of-care [3]. Cancer-specific survival rates for non-metastatic clear cell RCC are estimated at 84 and 76% at 5 and 10 years respectively after initial surgical resection [4]. However, around 30–40% of patients with high-risk features such as high nuclear grade, locally advanced stage, and/or regional lymph node involvement experience disease recurrence which is generally incurable. The optimal treatment strategy for such high-risk patients would be to offer an effective anticancer perioperative systemic treatment with the goal of eradicating micrometastatic disease and potentially improving cure rates, without subjecting patients to significant toxicity. Such a multimodal strategy has been successful in several other solid tumors such as bladder, breast, colon, and lung cancer [5,6,7,8].
Multiple agents such as interferon, interleukin-2, tumor vaccines, chemotherapies and medroxyprogesterone acetate have been evaluated in RCC in the adjuvant setting without improvement in disease-free survival (DFS) or overall survival (OS) [9,10,11,12,13,14,15,16,17,18]. More recently, enhancement in our understanding of the pathogenesis of advanced RCC has significantly enriched the treatment landscape with the introduction of agents targeting the vascular endothelial growth factor (VEGF) pathway and mammalian target of rapamycin (mTOR) inhibitors. These therapies have significantly improved outcomes in the metastatic setting [19], and thus, were rational to investigate in the adjuvant setting. However, to date only one of four reported randomized controlled clinical trials has demonstrated improved DFS with adjuvant tyrosine kinase inhibition, albeit with an earlier trial with the same agent, sunitinib, reporting no difference [20••, 21••, 22••, 23••]. Consequently, there is no well-established adjuvant systemic therapy strategy in RCC.
Immune checkpoint inhibitors (CPI) have demonstrated durable efficacy with a favorable safety and tolerability profile in both treatment naïve and VEGF targeted therapy refractory metastatic RCC [24, 25]. Therefore, great enthusiasm exists to evaluate them in the non-metastatic setting to prevent disease recurrence and improve cure rates. In this review, we discuss the current evidence regarding VEGF targeted therapy as adjuvant treatment in RCC as well as discuss the ongoing trials evaluating CPI in this setting.
Risk stratification in localized renal cell carcinoma
For localized disease, multiple prognostic nomograms incorporating the American Joint Committee on Cancer (AJCC) TNM staging, Eastern Cooperative Oncology Group (ECOG) performance status, and histologic features such as presence or absence of necrosis and Fuhrman nuclear grade have been developed to identify patients at high risk for disease recurrence [26,27,28,29,30,31,32,33,34]. Among the most frequently used nomograms are the Leibovich and the UCLA Integrated Staging System (UISS) scores. The Leibovich score was specifically designed to predict DFS after surgery for patients with localized clear cell RCC and stratifies patients into three risk groups based on tumor stage, regional lymph node status, nuclear grade, and the presence or absence of necrosis [28]. Recently, Leibovich and colleagues presented a prognostic model including non-clear cell subtypes (papillary and chromophobe) of RCC as well [4]. The UISS score stratifies patients into five risk categories based on TNM stage, Fuhrman nuclear grade, and performance status and is designed to classify patients into risk groups and predict survival for patients with both clear cell and non-clear cell RCC [27]. These prognostic models have been used for patient selection in several contemporary adjuvant clinical trials. However, significant heterogeneity has been described across these nomograms with regard to estimation of recurrence risk [35].
Advances in our understanding of RCC pathogenesis have highlighted the significance of VHL, BAP1, PBRM1, and SETD2 mutations as key drivers of RCC progression [36,37,38]. Transcriptomic approaches based on gene expression have the potential to improve the risk stratification of RCC. Prognostic assays based on gene expression data have been successfully incorporated in clinical practice in other tumor types such as breast and prostate carcinoma [39, 40]. Brooks et al. developed a genomic classifier (ClearCode 34) based on expression of 34 genes to identify good-risk (ccA) and poor-risk (ccB) subtypes of RCC that is able to discriminate significant differences in outcomes [41]. The prognostic significance of this signature was subsequently validated using gene expression data from patients with non-metastatic RCC included in The Cancer Genome Atlas (TCGA) database and an institutional cohort of RCC patients. Rini and colleagues investigated a 16-gene expression signature in a retrospective cohort of 942 patients with stage I–III clear cell RCC who underwent nephrectomy [42]. A total of 11 genes representing vascular, immune response, inflammation, cell cycle, and cell growth pathways, as well as, 5 reference genes were selected for inclusion in the recurrence score. This 16-gene recurrence score was subsequently validated in an independent cohort of patients with stage I–III RCC and was associated with worse recurrence-free survival (RFS) after adjusting for tumor size, nuclear grade, and Leibovich score. Its prognostic value was validated using a cohort of patients with high-risk RCC treated with adjuvant sunitinib versus placebo in the S-TRAC trial [43•]. Increase in recurrence score was associated with worse RFS, DFS, and cancer-specific survival (CSS) in patients treated with both sunitinib and placebo treatment arms and may help identify patients who would most need an effective adjuvant therapy.
Long non-coding RNAs (lncRNAs) have a critical role in cancer recurrence and prognosis [44]. RNA-sequencing of 444 stage I–III clear cell RCC tumors captured in the TCGA dataset permitted development of a four-lncRNA-based classifier that significantly stratified patients into high- versus low-risk groups in terms of clinical outcome [45]. The signature achieved a higher accuracy than clinical staging such as TNM and SSIGN score. Genes important in cell cycle proliferation may also aid in prediction of recurrence. Morgan et al. identified a multigene signature derived from a RNA expression array measuring genes involved in cell cycle proliferation as an independent predictor of recurrence and disease-specific mortality after nephrectomy in 565 patients with localized clear cell, papillary, or chromophobe RCC [46]. A composite score incorporating clinical data (Karakiewicz nomogram) was developed, which was correlated with outcomes suggesting that the combination of clinical and genomic features could improve risk stratification. While these studies represent significant attempts at improving the risk stratification of localized RCC, most require further prospective validation before adoption into clinical practice.
Contemporary trials of targeted therapies in the adjuvant setting
The blockade of tumor angiogenesis via VEGF pathway inhibition is the main mechanism of action of targeted therapies in RCC [19]. Their efficacy in advanced disease led to the development of several phase III clinical trials investigating their role in the adjuvant setting. The results of some studies have been reported thus far (Table 1): ASSURE (sunitinib vs. sorafenib vs. placebo), S-TRAC (sunitinib vs. placebo), PROTECT (pazopanib vs. placebo), and ATLAS (axitinib vs. placebo). The primary endpoint for all these studies was DFS, defined as the interval between randomization and first tumor recurrence, occurrence of metastasis or a secondary cancer, or death. OS, defined as the time from randomization to death from any cause, was a secondary endpoint across the trials.
The ASSURE trial (NCT00326898) was the largest study to investigate VEGF targeted agents adjuvantly in RCC [20••]. A total of 1943 patients with high-risk RCC as defined by AJCC (pT1bN0M0 with nuclear grade ≥ 3, or pT2-4N0M0 or pTanyN+M0) were randomized in a 1:1:1 fashion to receive sunitinib 50 mg oral per day (4 weeks on and 2 weeks off schedule) with sorafenib placebo, sorafenib 400 mg oral twice daily (continuous schedule) with sunitinib placebo, or placebo/placebo for 1 year after nephrectomy. Enrollment of patients with non-clear cell histology was allowed. High rates of treatment discontinuation due to toxicity among the initial 1323 patients enrolled led to an amendment to lower the starting dose to sunitinib 37.5 mg daily and sorafenib 400 mg (200 mg twice daily). Patients with tolerable grade 2 adverse events (AEs) could be dose escalated to the full doses. Dose reductions due to toxicity were permitted for both sunitinib (lowest level: 25 mg daily) and sorafenib (lowest: 400 mg every other day). Median DFS was 5.8 years for sunitinib (HR 1.02, 97.5% CI 0.85–1.23; p = 0.8038), 6.1 years for sorafenib (HR 0.97, 97.5% CI 080–1.17; p = 0.7184), compared to 6.6 years for patients in the placebo arm. No difference in OS was noted between the three cohorts. Subgroup analyses of patients at the highest risk by stage (pT3-4 or pN+) with clear cell histology (n = 1069) and those that had higher dose intensity of sunitinib or sorafenib failed to demonstrate benefit from adjuvant sunitinib or sorafenib compared to placebo [47•]. ASSURE highlighted the tolerability issues associated with VEGF tyrosine kinase inhibition when administered in the adjuvant setting. Grade 3 or higher AEs occurred in 63% of patients in the sunitinib arm, 72% in the sorafenib arm, and 25% in the placebo arm. Among all patients, the starting dose had to be reduced to 37.5 mg daily for sunitinib (69.6%) and 200 mg twice daily for sorafenib (69.8%). Treatment discontinuation due to treatment-related AEs occurred in 44% of patients treated with sunitinib and 45% of patients who received sorafenib. Despite dose reductions, 34% at reduced dose sunitinib and 30% at reduced dose sorafenib still required treatment discontinuation.
The S-TRAC trial (NCT00375674) randomized 615 patients with resected locoregional clear cell RCC at high risk for recurrence per UISS criteria (pT2N0M0 grade ≥ 3 or pT3-4N0M0 or pTxN+M0) to receive sunitinib 50 mg daily (4 weeks on and 2 weeks off schedule) or placebo (1:1) for 1 year [21••]. S-TRAC required treatment to be started at the full dose and limited dose reductions during treatment to only one dose level (no lower than 37.5 mg daily). Based on blinded independent central review with a median follow-up of 5.4 years, patients treated with sunitinib had a statistically significant increase in DFS compared to those treated with placebo (6.8 vs. 5.6 years, HR 0.76; 95% CI 0.59–0.98; p = 0.03). There was no statistically significant difference in investigator-assessed DFS between both treatment arms (6.5 vs. 4.5 years, HR 0.81; 95% CI 0.64–1.02; p = 0.08). There was no difference in OS (HR 1.01). Follow-up analyses identified 67 deaths with sunitinib and 74 deaths with placebo [48].
The toxicity profile of sunitinib was similar to that seen in the ASSURE trial. Grade 3–4 events occurred in 60.5% of patients in the sunitinib arm. The treatment discontinuation rate due to AEs was 28% and dose reductions were needed in 34% of patients. Recently, patient-reported outcomes from S-TRAC highlighted reduced quality of life and increased toxicity compared to the placebo arm. Diarrhea, palmar-plantar erythrodysesthesia, and hypertension were the most common events described in the sunitinib arm with appetite loss and diarrhea being clinically meaningful to the patients. [49].
A prospective exploratory biomarker analysis in a subset of patients from the S-TRAC trial has been conducted to examine potential associations between treatment effects and tissue biomarkers including CD4, CD68, CD8, and programmed cell death ligand 1 (PD-L1). Greater CD8+ T cell density in tumor tissue was associated with longer DFS with sunitinib but not placebo, suggesting potential predictive utility, although further independent cohort validation studies are warranted [50].
Based on the improvement in DFS seen in the S-TRAC trial, the Food and Drug Administration (FDA) extended the sunitinib indication to patients at high risk for recurrence after nephrectomy, and it is now a standard treatment option for patients whose disease meets the S-TRAC criteria. Nevertheless, the decision remains controversial among many patients and physicians given the discrepant results, lack of OS benefit, and toxicity profile. Indeed, prior to the FDA and International Kidney Cancer Coalition (IKCC) decision, the European Association of Urology (EAU) convened a panel of kidney cancer experts and patient advocates from the IKCC [51•]. Their meta-analysis of the ASSURE and S-TRAC data, did not demonstrate a significant DFS benefit. The consensus of the patient and physician panels was that the evidence to support adjuvant sunitinib was weak, and they did not recommend sunitinib as adjuvant therapy.
The PROTECT trial (NCT01235962) randomized 1538 patients to pazopanib 800 mg oral per day or placebo (1:1) for 1 year [22••]. Eligible patients had intermediate- or high-risk clear cell RCC (pT2N0M0 grade ≥ 3, pT3-4N0M0, pTxN1M0). As in the ASSURE trial, the starting dose of pazopanib was reduced from 800 to 600 mg daily, after enrollment of 403 patients, due to high rates of treatment discontinuations due to toxicity. The primary endpoint was subsequently changed to DFS among the patients treated with pazopanib 600 mg vs. placebo (n = 1135). The modified primary endpoint was not achieved; there was no significant difference in DFS between patients treated with pazopanib 600 mg daily or placebo (HR 0.86; 95% CI 0.70–1.06; p = 0.16). However, the subpopulations with no reduction in the starting dose—pazopanib 800 mg (HR 0.69; 95% CI 0.51–0.94; p = 0.02)—and the combined population—pazopanib 800 and 600 mg (HR 0.80; 95% CI 0.68–0.95; p = 0.01)—achieved a significant intention-to-treat DFS benefit leading to 31 and 20% risk reductions, respectively. While it may be premature, no OS benefit for either subpopulation was seen. The treatment discontinuation rate was 35% with pazopanib 600 mg and 39% at the full 800 mg dose.
A recent systematic review and meta-analysis of patients treated on the ASSURE, S-TRAC, and PROTECT trials did not reveal a statistically significant benefit of DFS or OS in patients with intermediate/high risk disease and was associated with significantly higher rates of high-grade AEs [52].
Recently, the results from ATLAS (NCT01599754), a randomized phase 3 trial evaluating axitinib 5 mg oral twice daily or placebo (1:1), have been reported. Eligibility required clear cell RCC intermediate or high risk for recurrence after nephrectomy (≥ pT2 and/or pN+) [23••]. Patients were required to take the drugs for 1 year but could remain on it for up to 3 years based on physician and patient discretion. An independent data monitoring committee recommended stopping the study at a planned interim analysis due to futility at 203 DFS events. Overall, a total of 724 patients were randomized in a 1:1 fashion and included in the intention-to-treat population. Among these, a higher percentage of patients were Asian (73%) and at highest risk of recurrence (56%), defined as pT3 grade ≥ 3 or pT4 and/or N+. Axitinib dose reductions were permitted to a minimum of 1 mg twice a day and dose escalations up to 10 mg twice a day were allowed. There was no significant difference in DFS per independent review committee assessment in the intention-to-treat population (HR 0.870, 95% CI 0.660–1.147; p 0.3211) or per investigator assessment (HR 0.776, 95% CI 0.599–1.005; p 0.0536). In the subgroup of patients at highest risk (pT3, Grade ≥ 3 or pT4 and/or N+), a trend towards improved DFS was observed by an independent review committee (HR 0.735, 95% CI 0.525–1.028; p 0.0704) and by investigators (HR 0.641, 95% CI 0.468–0.879; p 0.0051). OS data were not mature. Treatment-related AEs occurred in 91% of patients treated with axitinib with 49% experiencing a grade 3–4 event. In axitinib-treated patients, 56% had dose reductions, 51% dose interruptions, and 23% had to permanently discontinue treatment. Duration of treatment for patients in the axitinib arm was as follows: > 1 year (31%), 1–2 years (27%), 2–3 years (22%), and 3 full years (20%).
Given the poor prognosis associated with its expression in localized RCC, agents targeting the carbonic anhydrase IX protein (CAIX) have also been investigated in the adjuvant setting [53]. The ARISER trial (NCT00087022) evaluated the efficacy of a monoclonal antibody (girentuximab) targeting CAIX in patients with pT1b-pT2 grade ≥ 3, pT3-4, or N+ RCC compared to placebo [54]. Girentuximab was administered as a first single dose 50 mg intravenous infusion, followed by weekly 20 mg infusions. Co-primary endpoints were DFS and OS assessed by independent radiologic review. No statistically significant DFS (HR = 0.97; 95% CI 0.79–1.18) or OS (HR = 0.99; 95% CI 0.74–1.32) benefit was observed. Drug-related AEs occurred in 21.6% of patients, which was similar in both arms. Subsequent analyses showed that a high CAIX score expression in primary tumor tissue (a calculation based on staining intensity and expression) portended the greatest DFS benefit especially in patients younger than 65 years, good ECOG performance status, or low grade tumors. Ultimately, this agent did not move forward in the clinic.
In addition to the previously mentioned studies, the ongoing SORCE (sorafenib vs. placebo) and EVEREST (everolimus vs. placebo) phase III clinical trials are assessing the utility of sorafenib and everolimus in the adjuvant setting, respectively. These studies have completed accrual and the final results are awaited (Table 2).
SORCE (NCT00492258) is a phase III study comparing sorafenib 400 mg twice daily for 3 years, sorafenib 400 mg twice daily for 1 year followed by placebo for 2 years, and placebo for 3 years. Patients are randomized in a 3:3:2 fashion. This study is targeting intermediate- or high-risk disease by Leibovich score and allows both clear cell and non-clear cell histologies. Similar to the ASSURE trial, the initial starting dose was reduced due to toxicity issues, in this case to sorafenib 400 mg once daily. The primary objective is DFS. The study has completed recruitment and final results are not yet published.
The phase III EVEREST trial (NCT01120249) is evaluating the role of the mTOR inhibitor everolimus 10 mg oral daily versus placebo for 1 year in clear and non-clear cell RCC at intermediate- or high-risk of recurrence. Using a 1:1 randomization, 1545 patients were accrued, and the final results are expected in 2021.
Lastly, akin to adjuvant therapy, the concept of targeting microscopic disease post-metastectomy is being investigated. A randomized phase 2 study (NCT01444807) compared 1 year of postsurgical sorafenib or observation after metastectomy and did not find a benefit in RFS [55]. Tolerability was a significant issue with only two patients among the 32 enrolled in the sorafenib arm being able to tolerate the full dose. E2810 (NCT01575548) is a fully accrued and maturing phase III trial which is evaluating postsurgical pazopanib for 1 year compared to placebo in patients with metastatic RCC who have no evidence of residual disease after metastatectomy.
Dissecting the evidence
Whether to use adjuvant VEGF inhibition for localized RCC remains controversial given the discordant results of the randomized trials to date. S-TRAC is the only study to show a statistically significant DFS benefit. Based on the S-TRAC results, the FDA approved sunitinib for high-risk patients in 2017 as adjuvant therapy for RCC. However, the voting was split with only 6 of the 12 ODAC members voting in favor. Conversely, the European Medicines Agency (EMA) opted to recommend against sunitinib in the adjuvant setting given the low benefit to risk ratio [51•].
The reasons behind the discrepant results have been debated. All studies proposed the same underlying hypothesis, were phase III randomized trials with an experimental arm with an oral VEGF targeted agent and a placebo control arm, and employed a primary DFS endpoint. However, some subtle but important differences have been noted. Heterogeneity in study design has been proposed as a possible reason to explain the different outcomes. These studies differed in terms of the stage of disease permitted (intermediate and/or high-risk patients using different risk recurrence classifications), inclusion or not of non-clear cell histologies, drug dosing from initiation to lowest dose reduction permitted, as well as primary endpoint assessment (investigator or independent central review).
S-TRAC was the most restrictive in terms of eligibility requiring the highest risk population by stage and excluding the non-clear cell histologies that have poorer prognosis when metastatic and where sunitinib has lower efficacy in the metastatic setting [56]. To assess whether differences in the primary DFS result between S-TRAC and ASSURE could be based on targeting only the highest risk clear cell disease, a post-hoc subgroup analysis of patients from the ASSURE trial with stage pT3-4 or pN+ clear cell disease, similar to those in the S-TRAC trial, demonstrated no statistically significant DFS benefit compared to placebo [47•]. S-TRAC employed central review of imaging at baseline and at recurrence, opposed to ASSURE which relied on investigator-based assessment, which could have influenced the reliability of the results. However, to counter that point, there was no difference in investigator-assessed DFS between the treatment arms in the S-TRAC trial which is in line with results from the ASSURE trial.
Differences in drug exposure have also been cited as a potential explanation for the differences in the trials. The sunitinib starting dose was not reduced in S-TRAC trial, and dose reductions were limited to 37.5 mg/day. In the ASSURE trial, the starting dose was reduced 37.5 mg/day for 70% of the patients and dose reductions were permitted as low as 25 mg/day. Reports in advanced disease have demonstrated a relationship between drug-dose and drug-efficacy among the VEGFR multityrosine kinase inhibitors [57,58,59,60]. The results of the adjuvant PROTECT study support the relationship between pazopanib exposure and clinical efficacy and safety [61•]. Among the patients treated with pazopanib 600 mg daily on the PROTECT trial, there was trend towards improved DFS in patients with a high pazopanib trough concentration compared to those who had low trough concentration or those who received placebo and a significant benefit in DFS was achieved among patients treated with pazopanib 800 mg daily.
None of the studies evaluating adjuvant targeted therapies in RCC have shown a survival benefit, which prompts the question of whether DFS is a good surrogate endpoint in this setting. Given the significant time requirements to test an OS endpoint, an earlier intermediate endpoint like DFS is preferred. DFS has been shown to correlate with OS in other diseases such as breast and colon cancer [62, 63]. The validity of DFS as a surrogate endpoint and its correlation with OS in RCC adjuvant studies was investigated in a meta-analysis of 13 randomized clinical trials which evaluated a heterogeneous array of adjuvant agents from cytokines to vaccines to chemotherapy to VEGF blockade. Only a modest correlation (R2 0.48) between 5-year DFS and OS rates was found [18]. The correlation of DFS with OS using patient data from the S-TRAC trial has been investigated [64]. The investigators found similar moderate correlations (R2 from 0.51 to 0.88) between OS and both investigator-assessed and blinded independent review DFS. Most of the ongoing trials in non-metastatic RCC consider OS as secondary endpoint with few studies considering both DFS and OS as co-primary endpoints likely due to duration and sample size requirements. Further studies are warranted to evaluate the relationship between DFS and OS.
Adjuvant checkpoint blockade
Cancer immunotherapies that target the T cell have enhanced disease control with some durable long-term responses in a broad array of advanced cancers. The efficacy of CPI targeting the Programmed Death-1 (PD-1) and Cytotoxic T Lymphocyte Associated protein-4 (CTLA-4) pathways in metastatic RCC [24, 25] has generated enthusiasm for the potential utility of these therapies in the adjuvant setting. Experience from other solid tumors such as melanoma indicates that CPIs in the adjuvant setting could be a promising strategy [65, 66].
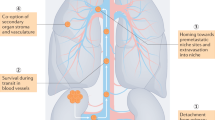
Currently, several clinical trials are examining the efficacy of immunotherapy in the adjuvant setting through either single or dual CPI (Table 2 and Fig. 1). The IMMotion010 (NCT03024996) and KEYNOTE-564 (NCT03142334) trials are phase III studies evaluating the role of atezolizumab (anti-PD-L1) and pembrolizumab (anti-PD-1), respectively, for 1 year compared to placebo in clear cell RCC. Tumors with sarcomatoid features are allowed in both trials. IMMotion010 includes high-risk disease and KEYNOTE-564 targets those patients with intermediate- and high-risk of recurrence. Both allow patients who present with isolated, soft tissue metastases that have been completely resected at the time of nephrectomy (synchronous) or ≤ 1 year from nephrectomy (metachronous). The primary objective of both studies is DFS.
Other ongoing clinical trials are evaluating dual CPI. RAMPART (NCT03288532) is a phase III multi-arm study assessing durvalumab (anti-PD-L1) alone or in combination with tremelimumab (anti-CTLA-4) for 1 year compared to surveillance. Patients with intermediate- or high-risk disease based on Leibovich score are eligible. It is expected that intermediate-risk patients will contribute 25% of the total accrual target. Enrollment of patients with non-clear cell histology is permitted except for pure oncocytoma, collecting duct, or medullary carcinomas. DFS and OS are co-primary endpoints. Only two doses of tremelimumab are given at the beginning of the treatment with continuation of adjuvant PD-L1 blockade for 1 year. Hoping to capitalize on the success of dual CPI in the first-line metastatic setting [25], the CheckMate 914 study (NCT03138512) is evaluating the ability of adjuvant nivolumab (anti-PD-1) plus ipilimumab (anti-CTLA-4) to increase DFS over placebo when given for 6 months. Intermediate or high-risk patients (pT2N0M0 grade ≥ 3 or pT3-4N0M0 or pTxN+M0) with predominantly clear cell disease are included. The combination will be given together for the first four doses followed by monthly nivolumab monotherapy for the remainder of the 6 months.
Although most studies are evaluating CPI solely in the adjuvant setting, their use in the neoadjuvant setting might elicit a more potent anti-tumor immune response due to presence of larger repertoire of tumor-associated antigens [67•]. Efficacy results from phase 2 trials testing neoadjuvant PD-1 pathway blockade in different solid tumors including bladder, lung, and breast cancer have shown promising results with impressive pathological responses [68,69,70,71]. In RCC, at least four clinical trials are evaluating the effects of CPI in the neoadjuvant context (NCT02595918, NCT02575222, NCT02212730, NCT02762006) and preliminary results of two have demonstrated feasibility and safety of nivolumab without delays in surgical treatment (NCT02575222, NCT02595918).
Of the phase 3 perioperative CPI studies in RCC, only one, the PROSPER RCC study (ECOG-ACRIN 8143), is evaluating the role of combined neoadjuvant plus adjuvant blockade (NCT03055013). PROSPER takes a three-dimensional approach of pre-surgical priming with PD-1 blockade in the form of nivolumab, followed by surgical resection, and consolidation with adjuvant PD-1 blockade for 9 months. It is not placebo controlled, and the control arm is standard-of-care partial or radical nephrectomy followed by observation. Patients with clinical T2-4 or any node positive tumors are eligible. Oligometastatic disease that can be surgically resected within a 12-week window is permitted. Both clear cell and non-clear cell tumors are eligible. The neoadjuvant component will allow the unique opportunity for correlative biomarker analyses of the impact of the neoadjuvant PD-1 priming on the immune response and discovery of any biomarkers that may predict optimal use of this strategy or portend better outcomes regardless of adjuvant therapy.
Conclusions
Given the discordant results from the currently reported adjuvant VEGFR tyrosine kinase inhibitor trials, the utility of adjuvant VEGF blockade in RCC today is debatable and participation in ongoing prospective CPI trials should be the priority. How best to incorporate these agents into the perioperative paradigm is evolving at a rapid pace. The future is bright, with several important ongoing CPI trials addressing different key questions from the efficacy of adjuvant monotherapy to dual checkpoint inhibition to a combined neoadjuvant/adjuvant approach. The recent successes of CPI-VEGF inhibitor combinations in the metastatic setting may make this an attractive approach in the adjuvant setting, although their tolerability profile will need to be carefully considered. Ideally, patient selection for future perioperative therapy trials should be based on genomic or molecular biomarkers in addition to the current prognostic tools based on disease stage, histology, and performance status.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Motzer RJ, Jonasch E, Agarwal N, et al. Kidney cancer, version 2.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2017;15:804–34.
Leibovich BC, Lohse CM, Cheville JC, et al. Predicting oncologic outcomes in renal cell carcinoma after surgery. Eur Urol. 2018;73:772–80.
Grossman HB, Natale RB, Tangen CM, et al. Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer. N Engl J Med. 2003;349:859–66.
Pisters KM, Evans WK, Azzoli CG, et al. Cancer Care Ontario and American Society of Clinical Oncology adjuvant chemotherapy and adjuvant radiation therapy for stages I-IIIA resectable non small-cell lung cancer guideline. J Clin Oncol. 2007;25:5506–18.
Early Breast Cancer Trialists’ Collaborative G, Davies C, Godwin J, et al. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 2011;378:771–84.
Andre T, de Gramont A, Vernerey D, et al. Adjuvant fluorouracil, leucovorin, and oxaliplatin in stage II to III colon cancer: updated 10-year survival and outcomes according to BRAF mutation and mismatch repair status of the MOSAIC study. J Clin Oncol. 2015;33:4176–87.
Wood C, Srivastava P, Bukowski R, et al. An adjuvant autologous therapeutic vaccine (HSPPC-96; vitespen) versus observation alone for patients at high risk of recurrence after nephrectomy for renal cell carcinoma: a multicentre, open-label, randomised phase III trial. Lancet. 2008;372:145–54.
Pizzocaro G, Piva L, Colavita M, et al. Interferon adjuvant to radical nephrectomy in Robson stages II and III renal cell carcinoma: a multicentric randomized study. J Clin Oncol. 2001;19:425–31.
Messing EM, Manola J, Wilding G, et al. Phase III study of interferon alfa-NL as adjuvant treatment for resectable renal cell carcinoma: an Eastern Cooperative Oncology Group/Intergroup trial. J Clin Oncol. 2003;21:1214–22.
Hinotsu S, Kawai K, Ozono S, et al. Randomized controlled study of natural interferon alpha as adjuvant treatment for stage II or III renal cell carcinoma. Int J Clin Oncol. 2013;18:68–74.
Clark JI, Atkins MB, Urba WJ, et al. Adjuvant high-dose bolus interleukin-2 for patients with high-risk renal cell carcinoma: a cytokine working group randomized trial. J Clin Oncol. 2003;21:3133–40.
Aitchison M, Bray CA, Van Poppel H, et al. Adjuvant 5-flurouracil, alpha-interferon and interleukin-2 versus observation in patients at high risk of recurrence after nephrectomy for renal cell carcinoma: results of a phase III randomised European Organisation for Research and Treatment of Cancer (Genito-Urinary Cancers Group)/National Cancer Research Institute trial. Eur J Cancer. 2014;50:70–7.
Passalacqua R, Caminiti C, Buti S, et al. Adjuvant low-dose interleukin-2 (IL-2) plus interferon-alpha (IFN-alpha) in operable renal cell carcinoma (RCC): a phase III, randomized, multicentre trial of the Italian Oncology Group for Clinical Research (GOIRC). J Immunother. 2014;37:440–7.
Atzpodien J, Schmitt E, Gertenbach U, et al. Adjuvant treatment with interleukin-2- and interferon-alpha2a-based chemoimmunotherapy in renal cell carcinoma post tumour nephrectomy: results of a prospectively randomised trial of the German Cooperative Renal Carcinoma Chemoimmunotherapy Group (DGCIN). Br J Cancer. 2005;92:843–6.
Pizzocaro G, Piva L, Di Fronzo G, et al. Adjuvant medroxyprogesterone acetate to radical nephrectomy in renal cancer: 5-year results of a prospective randomized study. J Urol. 1987;138:1379–81.
Harshman LC, Xie W, Moreira RB, et al. Evaluation of disease-free survival as an intermediate metric of overall survival in patients with localized renal cell carcinoma: a trial-level meta-analysis. Cancer. 2018;124(5):925–33.
Choueiri TK, Motzer RJ. Systemic therapy for metastatic renal-cell carcinoma. N Engl J Med. 2017;376:354–66.
•• Haas NB, Manola J, Uzzo RG, et al. Adjuvant sunitinib or sorafenib for high-risk, non-metastatic renal-cell carcinoma (ECOG-ACRIN E2805): a double-blind, placebo-controlled, randomised, phase 3 trial. Lancet. 2016;387:2008–16 Largest phase III trial evaluating adjuvant sunitinib or sorafenib versus placebo in patients with RCC at risk of recurrence after nephrectomy but failed to demostrate a disease free or overall survival benefit.
•• Ravaud A, Motzer RJ, Pandha HS, et al. Adjuvant sunitinib in high-risk renal-cell carcinoma after nephrectomy. N Engl J Med. 2016;375:2246–54. Phase III trial evaluating sunitinib versus placebo in high risk clear cell adjuvant renal cell carcinoma which contrary to ASSURE did show a significant increase in disease free survival but has not shown an improvement in overall survival.
•• Motzer RJ, Haas NB, Donskov F, et al. Randomized phase III trial of adjuvant pazopanib versus placebo after nephrectomy in patients with localized or locally advanced renal cell carcinoma. J Clin Oncol. 2017;35:3916–23 PROTECT was a phase III trial comparing adjuvant pazopanib versus placebo in renal cell carcinoma patients who had undergone nephrectomy and did not find a difference in disease free or overall survival at the 600mg dose.
•• Gross-Goupil M, Kwon TG, Eto M, et al. Axitinib versus placebo as an adjuvant treatment for renal cell carcinoma: results from the phase III, randomized ATLAS trial. Ann Oncol. 2018;29:2371–8. Recently reported phase III trial evaluating adjuvant axitinib versus placebo in patients with locoregional renal cell carcinoma at risk of recurrence after nephrectomy which did not demonstrate a significant difference in disease free survival.
Motzer RJ, Escudier B, McDermott DF, et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med. 2015;373:1803–13.
Motzer RJ, Tannir NM, McDermott DF, et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N Engl J Med. 2018;378:1277–90.
Kim SP, Alt AL, Weight CJ, et al. Independent validation of the 2010 American Joint Committee on Cancer TNM classification for renal cell carcinoma: results from a large, single institution cohort. J Urol. 2011;185:2035–9.
Patard JJ, Kim HL, Lam JS, et al. Use of the University of California Los Angeles integrated staging system to predict survival in renal cell carcinoma: an international multicenter study. J Clin Oncol. 2004;22:3316–22.
Leibovich BC, Blute ML, Cheville JC, et al. Prediction of progression after radical nephrectomy for patients with clear cell renal cell carcinoma: a stratification tool for prospective clinical trials. Cancer. 2003;97:1663–71.
Frank I, Blute ML, Cheville JC, et al. An outcome prediction model for patients with clear cell renal cell carcinoma treated with radical nephrectomy based on tumor stage, size, grade and necrosis: the SSIGN score. J Urol. 2002;168:2395–400.
Kattan MW, Reuter V, Motzer RJ, et al. A postoperative prognostic nomogram for renal cell carcinoma. J Urol. 2001;166:63–7.
Cindolo L, de la Taille A, Messina G, et al. A preoperative clinical prognostic model for non-metastatic renal cell carcinoma. BJU Int. 2003;92:901–5.
Raj GV, Thompson RH, Leibovich BC, Blute ML, Russo P, Kattan MW. Preoperative nomogram predicting 12-year probability of metastatic renal cancer. J Urol. 2008;179:2146–51.
Karakiewicz PI, Briganti A, Chun FK, et al. Multi-institutional validation of a new renal cancer-specific survival nomogram. J Clin Oncol. 2007;25:1316–30.
Zisman A, Pantuck AJ, Dorey F, et al. Improved prognostication of renal cell carcinoma using an integrated staging system. J Clin Oncol. 2001;19:1649–57.
Pal SK, Haas NB. Adjuvant therapy for renal cell carcinoma: past, present, and future. Oncologist. 2014;19(8):851–9.
Kapur P, Pena-Llopis S, Christie A, et al. Effects on survival of BAP1 and PBRM1 mutations in sporadic clear-cell renal-cell carcinoma: a retrospective analysis with independent validation. Lancet Oncol. 2013;14:159–67.
Varela I, Tarpey P, Raine K, et al. Exome sequencing identifies frequent mutation of the SWI/SNF complex gene PBRM1 in renal carcinoma. Nature. 2011;469:539–42.
Hakimi AA, Ostrovnaya I, Reva B, et al. Adverse outcomes in clear cell renal cell carcinoma with mutations of 3p21 epigenetic regulators BAP1 and SETD2: a report by MSKCC and the KIRC TCGA research network. Clin Cancer Res. 2013;19:3259–67.
Klein EA, Yousefi K, Haddad Z, et al. A genomic classifier improves prediction of metastatic disease within 5 years after surgery in node-negative high-risk prostate cancer patients managed by radical prostatectomy without adjuvant therapy. Eur Urol. 2015;67:778–86.
Sparano JA, Gray RJ, Makower DF, et al. Prospective validation of a 21-gene expression assay in breast cancer. N Engl J Med. 2015;373:2005–14.
Brooks SA, Brannon AR, Parker JS, et al. ClearCode34: a prognostic risk predictor for localized clear cell renal cell carcinoma. Eur Urol. 2014;66:77–84.
Rini B, Goddard A, Knezevic D, et al. A 16-gene assay to predict recurrence after surgery in localised renal cell carcinoma: development and validation studies. Lancet Oncol. 2015;16:676–85.
• Rini BI, Escudier B, Martini JF, et al. Validation of the 16-gene recurrence score in patients with locoregional, high-risk renal cell carcinoma from a phase III trial of adjuvant sunitinib. Clin Cancer Res. 2018;24:4407–15. Analysis validating the 16-gene recurrence score prognostic value in patients enrolled on the S-TRAC trial.
Lin C, Yang L. Long noncoding RNA in cancer: wiring signaling circuitry. Trends Cell Biol. 2018;28:287–301.
Qu L, Wang ZL, Chen Q, et al. Prognostic value of a long non-coding RNA signature in localized clear cell renal cell carcinoma. Eur Urol. 2018;74:756–63.
Morgan TM, Mehra R, Tiemeny P, et al. A multigene signature based on cell cycle proliferation improves prediction of mortality within 5 yr of radical nephrectomy for renal cell carcinoma. Eur Urol. 2018;73:763–9.
• Haas NB, Manola J, Dutcher JP, et al. Adjuvant treatment for high-risk clear cell renal cancer: updated results of a high-risk subset of the ASSURE randomized trial. JAMA Oncol. 2017;3:1249–52 Subanalyses of the ASSURE trial continued to show no disease free or overall survival benefit in subsets of patients with high risk diesase by stage, clear cell disease or by dose intensity of the TKI.
Motzer RJ, Ravaud A, Patard JJ, et al. Adjuvant sunitinib for high-risk renal cell carcinoma after nephrectomy: subgroup analyses and updated overall survival results. Eur Urol. 2018;73:62–8.
Staehler M, Motzer RJ, George DJ, et al. Adjuvant sunitinib in patients with high-risk renal cell carcinoma: safety, therapy management, and patient-reported outcomes in the S-TRAC trial. Ann Oncol. 2018;29:2098–104.
George DJ, Martini JF, Staehler M, et al. Immune biomarkers predictive for disease-free survival with adjuvant sunitinib in high-risk locoregional renal cell carcinoma: from randomized phase III S-TRAC study. Clin Cancer Res. 2018;24:1554–61.
• Bex A, Albiges L, Ljungberg B, et al. Updated European Association of Urology guidelines regarding adjuvant therapy for renal cell carcinoma. Eur Urol. 2017;71(5):719–22 Metaanalysis and guidelines from a panel of European Association of Urology comprised of kidney cancer experts and patient representatives which did not recommend the adjuvant administration of sunitinib.
Sun M, Marconi L, Eisen T, et al. Adjuvant vascular endothelial growth factor-targeted therapy in renal cell carcinoma: a systematic review and pooled analysis. Eur Urol. 2018;74:611–20.
Bui MH, Seligson D, Han KR, et al. Carbonic anhydrase IX is an independent predictor of survival in advanced renal clear cell carcinoma: implications for prognosis and therapy. Clin Cancer Res. 2003;9:802–11.
Chamie K, Donin NM, Klopfer P, et al. Adjuvant weekly girentuximab following nephrectomy for high-risk renal cell carcinoma: the ARISER randomized clinical trial. JAMA Oncol. 2017;3:913–20.
Procopio G, Cognetti F, Miceli R, et al. A randomized, open label, multicenter phase 2 study, to evaluate the efficacy of sorafenib (So) in patients (pts) with metastatic renal cell carcinoma (mRCC) after a radical resection of metastases: RESORT trial. J Clin Oncol. 2018;36, no. 15_suppl 4502–4502.
Fernández-Pello S, Hofmann F, Tahbaz R, et al. A systematic review and meta-analysis comparing the effectiveness and adverse effects of different systemic treatments for non-clear cell renal cell carcinoma. Eur Urol. 2017;71(3):426–36.
Houk BE, Bello CL, Poland B, Rosen LS, Demetri GD, Motzer RJ. Relationship between exposure to sunitinib and efficacy and tolerability endpoints in patients with cancer: results of a pharmacokinetic/pharmacodynamic meta-analysis. Cancer Chemother Pharmacol. 2010;66:357–71.
Rini BI, Garrett M, Poland B, Dutcher JP, Rixe O, Wilding G, et al. Axitinib in metastatic renal cell carcinoma: results of a pharmacokinetic and pharmacodynamic analysis. J Clin Pharmacol. 2013;53:491–504.
Rini BI, Melichar B, Fishman MN, Oya M, Pithavala YK, Chen Y, et al. Axitinib dose titration: analyses of exposure, blood pressure and clinical response from a randomized phase II study in metastatic renal cell carcinoma. Ann Oncol. 2015;26:1372–7.
Suttle AB, Ball HA, Molimard M, Hutson TE, Carpenter C, Rajagopalan D, et al. Relationships between pazopanib exposure and clinical safety and efficacy in patients with advanced renal cell carcinoma. Br J Cancer. 2014;111:1909–16.
• Sternberg CN, Donskov F, Haas NB, et al. Pazopanib exposure relationship with clinical efficacy and safety in the adjuvant treatment of advanced renal cell carcinoma. Clin Cancer Res. 2018;24:3005–13 Study demonstrating that higher pazopanib exposure was associated with improved efficacy in patients who received adjuvant pazopanib on the PROTECT trial.
Early Breast Cancer Trialists’ Collaborative G. Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet. 2015;386:1341–52.
Sargent DJ, Patiyil S, Yothers G, Haller DG, Gray R, Benedetti J, et al. End points for colon cancer adjuvant trials: observations and recommendations based on individual patient data from 20,898 patients enrolled onto 18 randomized trials from the ACCENT group. J Clin Oncol. 2007;25(29):4569–74.
George DJ, Pantuck AJ, Figlin RA, et al. Correlations between disease-free survival (DFS) and overall survival (OS) in patients (pts) with renal cell carcinoma (RCC) at high risk for recurrence: results from S-TRAC trial. Ann Oncol. 2018;29(Issue suppl_8):2018.
Eggermont AM, Chiarion-Sileni V, Grob JJ, et al. Adjuvant ipilimumab versus placebo after complete resection of high-risk stage III melanoma (EORTC 18071): a randomised, double-blind, phase 3 trial. Lancet Oncol. 2015;16:522–30.
Weber J, Mandala M, Del Vecchio M, et al. Adjuvant nivolumab versus ipilimumab in resected stage III or IV melanoma. N Engl J Med. 2017;377:1824–35.
• Liu J, Blake SJ, Yong MC, et al. Improved efficacy of neoadjuvant compared to adjuvant immunotherapy to eradicate metastatic disease. Cancer Discov. 2016;6:1382–99. Preclinical data showing greater therapeutic efficacy of neoadjuvant PD-1 based immunotherapies compared to adjuvant administration.
Necchi A, Anichini A, Raggi D, et al. Pembrolizumab as neoadjuvant therapy before radical cystectomy in patients with muscle-invasive urothelial bladder carcinoma (PURE-01): an open-label, single-arm, phase II study. J Clin Oncol. 2018:JCO1801148. https://doi.org/10.1200/JCO.18.01148 [Epub ahead of print].
Powles T, Rodriguez-Vida A, Duran I, et al. A phase II study investigating the safety and efficacy of neoadjuvant atezolizumab in muscle invasive bladder cancer (ABACUS). J Clin Oncol. 2018;36(15_suppl):4506–4506.
Nanda R, Liu MC, Yau C, et al. Pembrolizumab plus standard neoadjuvant therapy for high-risk breast cancer (BC): results from I-SPY 2. J Clin Oncol. 2017;35(suppl 15) abstr 506:506.
Forde PM, Chaft JE, Smith KN, et al. Neoadjuvant PD-1 blockade in resectable lung cancer. N Engl J Med. 2018;378(21):1976–86.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Nieves Martinez Chanza has received compensation from Bayer for participation on advisory boards and has received reimbursement for travel expenses from Pfizer.
Abhishek Tripathi declares that he has no conflict of interest.
Lauren C. Harshman has received research funding (paid to her institution) from Bayer, Sotio, Bristol-Myers Squibb, Merck, Takeda, Dendreon/Valeant, Janssen, Medivation/Astellas, Genentech, and Pfizer; has received compensation for participation on advisory boards from Bayer, Genentech, Dendreon, Pfizer, Medivation/Astellas, Merck, Exelixis, Corvus, Novartis, EMD Serono and Jounce Therapeutics; and has received reimbursement for travel expenses from Bayer.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Genitourinary Cancers
Rights and permissions
About this article
Cite this article
Martinez Chanza, N., Tripathi, A. & Harshman, L.C. Adjuvant Therapy Options in Renal Cell Carcinoma: Where Do We Stand?. Curr. Treat. Options in Oncol. 20, 44 (2019). https://doi.org/10.1007/s11864-019-0639-0
Published:
DOI: https://doi.org/10.1007/s11864-019-0639-0