Opinion statement
Oropharyngeal squamous cell carcinoma (OPSCC) incidence rates have been steadily increasing over the past several decades, and this has been largely attributed to human papillomavirus (HPV)-related OPSCC. The rise of HPV-related OPSCC and the observed distinct survival advantage it offers compared to HPV-unrelated OPSCC have resulted in the development of a new staging system specifically for OPSCC in the eighth edition of the AJCC Staging Manual for head and neck cancer. The observations on HPV-related OPSCC and its prognostic implications have coincided with increasing utilization of transoral surgical approaches to oropharyngeal tumors, such as transoral laser microsurgery (TLM) and transoral robotic surgery (TORS). These approaches were once thought to only be applicable to patients with low T-stage OPSCC tumors; however, they are being increasingly utilized in locally advanced OPSCC cases as several studies have shown that both of these transoral approaches are oncologically sound alternatives to concurrent chemoradiation therapy (CCRT), which was previously the standard-of-choice treatment in patients with locally advanced disease. Moreover, these transoral approaches have displayed better long-term swallowing outcomes compared to CCRT, as severe dysphagia is often the most bothersome functional impairment to OPSCC survivors who have undergone CCRT. While open surgical approaches were previously not utilized in the locally advanced OPSCC setting due to the risk of severe surgical complications compared to the potential benefits of organ preservation with CCRT and comparable survival rates after either treatment regimen, these approaches are still reasonable options for select patients in the salvage surgery setting, as they allow for maximum exposure to the deep oropharyngeal anatomy. Data from multiple clinical trials evaluating the potential for TORS to de-escalate radiation dose or CCRT regimen in certain settings will inform clinical decision-making for OPSCC patients for the next decade and allow for more personalized treatments tailored to an individual patient’s disease burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oropharyngeal squamous cell carcinoma (OPSCC) includes cancers arising from the palatine tonsils, base of tongue, soft palate, and pharyngeal walls and has been noted to have a steadily increasing incidence over the past several decades. In 2018 alone, there have been 92,887 new cases and 51,005 deaths worldwide due to OPSCC [1]. Chaturvedi et al. have noted that the rise in incidence in OPSCC has been largely attributed to human papillomavirus (HPV)-related OPSCC, and even with conservative estimates, the incidence of OPSCC is expected to surpass the incidence of cervical cancer in the USA by 2020 [2]. The demographic groups that are most commonly affected by HPV-related OPSCC include nonsmokers, males, Caucasians, and individuals under the age of 60 [3, 4]. HPV-related OPSCC has been noted to have a distinct survival advantage compared to HPV-unrelated OPSCC, which has resulted in the development of a separate staging system for HPV-positive oropharyngeal cancer in the eighth edition of the American Joint Committee on Cancer (AJCC) Staging Manual for head and neck cancer [5••].
Since the 1980–1990s, definitive concurrent chemoradiation therapy (CCRT) was the standard-of-choice treatment option for locally advanced OPSCC. Given that tumors arising from oropharynx can be difficult to directly visualize and obtain adequate margins, direct surgical approaches involve radical resections with mandibulotomy, which can result in functional impairments in swallowing and cosmetic deformities and high rates of positive margins, while not providing a distinct benefit in terms of overall survival or loco-regional control [6]. CCRT was the favored treatment option as it had improved overall survival rates and loco-regional control rates compared to radiation therapy alone and did not appear to have the initial morbidities associated with radical surgery [7,8,9], but the survivors often develop acute and late toxicities from treatment, including significant dysphagia requiring the use of percutaneous endoscopic gastrostomy (PEG) feeding tubes for nutrition [10].
Given the rise of OPSCC in a younger, healthier patient population, there has been a push for treatment approaches that will provide not only the best oncologic outcome but also preserve function and reduce morbidity. Endoscopic approaches to the oropharynx, via transoral laser microsurgery (TLM) and transoral robotic surgery (TORS), have proven to be appropriate treatment options for patients with OPSCC due to enhanced transoral access to these tumors, and there are ongoing clinical trials revisiting whether surgical resection of OPSCC with TORS can allow for de-escalation of the radiation dose given to patients or to limit the use of concurrent chemotherapy with radiation for OPSCC patients [11,12,13]. Using these surgical approaches will hopefully diminish morbidity and expedite patients’ swallowing rehabilitation. This review will discuss the recent advances in surgical options for locally advanced OPSCC and examine future directions in the treatment of this disease in light of these novel surgical approaches to the oropharynx.
Transoral laser microsurgery
Transoral laser microsurgery (TLM) is a minimally invasive endoscopic surgical technique that is performed under direct laryngoscopy with an operative microscope, microsurgical instruments, and typically a carbon dioxide (CO2) laser. This technique has been used to resect benign and malignant lesions from the oropharynx since the early 1970s [14]. It offers an ability to directly visualize and approach tumors in the oropharynx while minimizing the surgical morbidity of radical, open surgical resections. With this approach, the tumor resection is tailored to the extent of its invasion into the surrounding anatomical regions, as the tumor is resected segmentally until normal tissue is identified rather than via an en bloc approach [15]. While this technique was initially utilized in tumors with limited extent of invasion, its use has broadened to include advanced T-stage tumors at a variety of sites in the upper aerodigestive tract, including the oropharynx [16].
Steiner et al. first published long-term results of 48 patients who underwent TLM at a single institution for base of tongue cancers, and 94% had stage III or IVa cancer based on the fifth edition of the AJCC staging system. The local control rate was 85% and the 5-year recurrence-free and overall survival rates were 73% and 52%. Most notably, approximately 90% of the patients maintained normalcy of diet and understandability of speech [15]. Rich et al. also studied the outcomes of 84 patients with stage III or IV OPSCC treated with TLM and adjuvant therapy with radiation or chemoradiation and found that the 5-year overall survival and disease-specific survival was 88% and 92%, respectively, and that 81% had acceptable swallowing function at the last follow-up [17]. Rich et al. further explored swallowing outcomes in a separate study of 118 patients and found that while 93% of patients with T1 to T3 OPSCC had good swallowing function at 2 years, only 40% of patients with T4 base of tongue tumors had good swallowing at this time point, suggesting that T4 stage tumors are most significantly associated with poor swallowing outcomes following TLM [18]. Haughey et al. published the only multicenter study of TLM with 204 patients with stage III or IV OPSCC and also noted 3-year overall survival rate of 86% and local control rate of 97%, with 87% of patients having normal swallowing or only episodic dysphagia [16]. These swallowing outcomes are encouraging in light of both prospective and single institution reports of high rates of late toxicities after chemoradiation in patients with advanced-stage OPSCC, where approximately 30% of patients still required gastrostomy tube support for nutrition > 1 year after treatment with standard portal radiation [10, 19]. With these important, landmark studies in mind, TLM has gained popularity as an oncologically sound surgical option for patients with advanced tumors. Furthermore, these studies demonstrate the more than acceptable swallowing outcomes that patients are left with following TLM.
The main limitation of TLM is that it has a steep learning curve and is highly operator dependent. As the instruments are being used through a laryngoscope, motion of the instruments is restricted to a narrower field-of-view and requires repositioning the laryngoscope to approach the tumor from different angles. The CO2 laser is also not ideal for obtaining hemostasis, and the procedure requires frequently alternating the laser with surgical clips or cautery instruments to gain hemostasis. Furthermore, although there have been several single-center studies and one multicenter study published on outcomes following TLM, there is currently a lack of prospective clinical trial data comparing it with other standard treatments. Nevertheless, based on the current evidence from the aforementioned studies, TLM appears to be a highly effective surgical treatment option for locally advanced OPSCC in the hands of an experienced surgeon with favorable oncologic outcomes and preserved swallowing function in the vast majority of cases.
Transoral robotic surgery
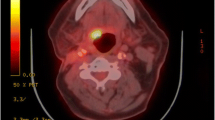
The introduction of transoral robotic surgery (TORS) as a safe and feasible surgical approach to the oropharynx has led to a huge shift in our treatment paradigm for oropharyngeal tumors [20, 21]. Surgical approaches to the base of tongue traditionally required mandibulotomy and lip-splitting incisions, but with TORS, the base of tongue can be accessed even without a neck incision. The tumor can be resected en bloc, keeping the specimen anatomically sound and allowing the surgeon to obtain accurate margins for the oncologic resection. Though radical tonsillectomy is possible without the use robotic equipment, the use of the robotic system led to increased maneuverability and visualization during this procedure. Currently, the da Vinci robot is the most commonly used, with a camera that enables magnification as well as excellent three-dimensional visualization of the surgical field, as seen in Fig. 1. The flexible robotic arms allow for a bimanual surgical approach to regions in the oropharynx that were previously unreachable transorally [22].
Transoral endoscopic view of a T1 tonsillar squamous cell carcinoma tumor provided with the use of the da Vinci robot system. This image illustrates how the robot can provide excellent three-dimensional visualization of the deep oropharyngeal anatomy and allow the surgeon to effectively resect relatively small tumors with negative margins.
Deciding whether TORS is appropriate for oropharyngeal cancer patients depends on whether the tumor is safely resectable transorally, whether the outcomes are comparable in terms of survival and function, and whether we can then spare the patient from other toxic therapies. Contraindications for TORS have been clearly defined, and specifically are related to whether the tumor abuts the carotid artery, if the tumor resection would require greater than 50% of the tongue base or posterior pharyngeal wall, or if the tumor is fixed to the prevertebral fascia or causing significant trismus [23]. Midline tongue base tumors that would put both lingual arteries at risk for resection or injury are also not amenable to TORS, as this would put the tongue unnecessarily at risk for devascularization and necrosis. With these guidelines in mind, some advanced T-category tumors can still be amenable to TORS resection. Prior history of radiation does not preclude one from being a TORS candidate, but these patients should be counseled on potential increase in wound complications, as the wound is left open to heal by secondary intention. In general, open approaches with free tissue reconstruction are preferred in the salvage setting as discussed later in this review.
Oncologic outcomes after TORS are comparable to nonsurgical treatment of advanced oropharyngeal tumors, specifically when examining overall and disease-specific survival. Both TORS and intensity-modulated radiation therapy (IMRT) result in 2-year overall survival rates ranging from 82 to 96% [24•]. Even for advanced-staged tumors, TORS has proven to provide patients with excellent oncologic outcomes, with a reported disease-specific survival of 98% and 90% at 1 and 2 years post-TORS, respectively [25]. Adjuvant radiation may still be necessary postoperatively, but patients are often spared at least 10 Gray (Gy) of their radiation dose, which significantly decreases radiation-induced toxicity to the pharynx [26, 27].
Since both TORS and radiation result in equivalent disease-specific and overall survival rates, assessing functional outcomes, particularly swallowing ability after treatment, may be the most important consideration in choosing a treatment modality. Dysphagia is one of the most bothersome functional impairments to an oropharyngeal cancer survivor, and many believe that with TORS, we can minimize this posttreatment sequelae while still preserving oncologic outcomes [28]. A prospective study of 81 OPSCC patients following primary treatment with TORS reported that only 9% still had use for their gastrostomy tube 1 year after TORS [29], which is significantly lower than the reported 31% of patients who continue to depend on their gastrostomy tube for nutritional support during the same time interval after combined chemoradiation therapy [19]. Aside from just swallowing function, TORS has been shown to result in high self-reported quality of life (QOL) scores, specifically with respect to the patient’s overall QOL, esthetic result, and social concerns at 1 year after surgery, with radiation therapy negatively impacting QOL scores [29].
Given this importance placed on QOL, ideal candidacy for TORS is largely based on postoperative swallowing outcomes. No longer do we ask whether a given tumor can be resected, but we now ask whether the tumor should be resected. Hence, importance is placed on using robotic surgery as a tool to de-escalate adjuvant therapy and to improve swallowing outcomes while maintaining excellent oncologic outcomes. Therefore, the ideal TORS candidate is a patient with a T1 to T2 tumor with low burden neck disease (< 5 nodes, no clinical extra-nodal extension). Adjuvant therapy in this patient population will reliably avoid chemotherapy and reduce the total radiation therapy dose to the primary tumor region from 70 to 60 Gy. Conversely, patients with large tumors and aggressive neck disease who will require both chemotherapy and radiation regardless of whether an operation is performed are not thought to be good TORS candidates, as de-escalation is frequently not achievable. Results from ECOG 33-11, which recently completed accrual, will likely provide insights into de-escalation in appropriately selected patients with advanced-stage OPSCC. Additionally, data from the National Cancer Database has suggested that approximately 60–65% of patients receiving TORS end up also receiving adjuvant chemoradiation [30, 31], which further underscores the need for appropriate patient selection undergoing TORS. More prospective studies evaluating TORS and patient outcomes following it are essential to guide future patient selection, as most of the current data is retrospective.
Open surgical approaches
Open surgical approaches to the oropharynx include lip-split mandibulotomy and lateral pharyngotomy. These techniques were developed in the mid-nineteenth and early twentieth centuries, respectively [32, 33], and they are still used currently in the setting of salvage surgery for locally advanced oropharyngeal cancer that recurs following primary radiotherapy (RT) or CCRT. The choice between these two options can be dependent on the location of the tumor and the amount of exposure needed. Lateral oropharyngeal lesions can be approached with a lateral pharyngotomy or lip-split mandibulotomy and midline lesions in the oropharynx are mainly approached with lip-split mandibulotomy, as it offers the widest and most reliable access to the deep anatomy of the oral cavity and oropharynx [34]. Larger resections also typically require free-flap reconstruction.
Prior to the advent of TORS and the increasing utilization of transoral surgical approaches to cancers in the oropharynx, outcomes data on the use of open surgical resection for oropharyngeal tumors were limited, as the standard-of-choice treatment in cases of locally advanced disease was primary RT with neck dissection or CCRT in order to maximize organ preservation and minimize the risk of severe surgical complications [35, 36]. Dziegielewski et al. published their complication rate in 214 patients who underwent lip-splitting mandibulotomy for access for primary cancer resection was 10.5%. Fixation failure (malunion, nonunion, mandibular fracture) occurred in 2.7% of cases and poor wound healing (hardware exposure, orocutaneous fistulae, osteomyelitis, and osteoradionecrosis) occurred in 7.7% of patients [34]. Their review of the literature on the average complication rate reported following mandibulotomy was 31.7% (range 12.5–61.3%), with a majority of these being attributed to poor wound healing and fixation failure, and the authors concluded that lower complication rates than originally perceived can obtained with this technique using modifications, such as direct interosseous wires in combination with a compression miniplate or employing a mentalis-wire tacking stitch [34]. Laccourreye et al. reported their outcomes on using lateral pharyngotomy in 91 patients with lateral oropharyngeal carcinoma and found that 27.4% had surgical complications resulting from this procedure, and the three most common complications were severe swallowing impairment (6.5%), aspiration pneumonia (4.3%), and oropharyngeal salivary fistula (4.3%) [37]. Median duration of hospitalization was 16 days in their patients and was significantly correlated with development of significant postoperative complications, duration of tracheostomy tube, and nasogastric tube dependency. They also noted that postoperative recovery of swallowing function was uneventful in 93.3% of the patients with a median duration of nasogastric tube of 11 days (range 3–30 days) [37]. Other mandible-preserving approaches, such as the lingual release approach, transcervical approach, and transhyoid approach, have also been compared to the mandibulotomy. Pang et al. compared outcomes from these mandible-preserving approaches to mandibulotomy outcomes in a meta-analysis, which included six studies with a total 309 patients, and found no significant differences in surgical margins, overall survival rate, recurrence rate, and speech and tongue movement between both approaches, but patients who underwent surgery with a mandible-preserving approach had significantly lower fistula formation rates than the mandibulotomy approach patients [38].
Regardless of the treatment modality used, HPV-negative patients with stage III and stage IV OPSCC have recurrence rates as high as 50%, and salvage surgery remains the only curative option for patients with local treatment failure after primary radiation or surgery with adjuvant radiation [39]. Roosli et al. described their outcomes following salvage surgery for recurrent OPSCC in 51 patients and noted that the 5-year overall survival and disease-specific survival rates were 29% and 40%, respectively, and the postoperative complication rate was 17.5% [40]. Patel et al. further examined differences in salvage surgery outcomes for 19 patients with p16-positive OPSCC and 13 patients with p16-negative OPSCC [41]. 76.4% of patients in their study underwent a mandibulotomy approach and 14.7% had mandibulectomy performed. The 5-year overall survival rate following salvage surgery was 25% compared to 2% without salvage surgery and the postoperative complication rate was 44.1%; however, they found no significant differences in overall survival or recurrence-free survival rates between the two cohorts [41]. These studies highlight that some patients may benefit from salvage surgery using an open surgical approach in the setting of locally recurrent OPSCC and that proper patient selection is critical to limiting the postoperative morbidity associated with this approach.
Clinical trials
Several surgical trials are in progress currently, with multiple new additions in the past 5 years. The PATHOS trial (NCT02215265) is currently being conducted in the UK and will assess patient-reported swallowing outcomes at 12 months on the MD Anderson Dysphagia Inventory (MDADI) in patients randomized to four different groups after transoral resection of the primary tumor. Patients randomized to group A will undergo primary surgical resection with no adjuvant therapy [42•]. Patients randomized to groups B1 and B2 include those with T3 (or T1–T2 tumors with additional risk factors), N2a or N2b disease, peri-neural invasion (PNI) or lymphovascular invasion (LVI), or close margins. Groups B1 and B2 will undergo postoperative RT at 50 Gy and 60 Gy, respectively. Patients in groups C1 or C2 include those with any T or N stage, extra-nodal extension (ENE), or positive margins (< 1 mm) around the tumor but negative marginal biopsies. Patients in C1 and C2 will undergo postoperative RT with 60 Gy and cisplatin in 30 fractions over 6 weeks or no chemotherapy, respectively. Secondary outcome measures include quantitative and qualitative swallowing assessments at baseline and at multiple intervals after treatment up to 24 months. QOL outcomes and acute and late toxicities, as well as overall and disease-specific survival are also measured. The study is currently active in 26 different centers in the UK, and the estimated completion date is February 2020. This trial is of particular interest as it is the only current trial to randomize patients with ENE into chemoradiation versus radiation adjuvant groups, as their retrospective data suggests that ENE is not as important of a prognostic indicator in the HPV-positive cohort.
The SIRS trial (NCT02072148) will vary postoperative adjuvant therapy in patients undergoing TORS and neck dissection. Patients with a complete resection (tonsil > 1 mm, pT1–2, N1–2b), no LVI or PNI, no extra-capsular spread (ECS), no matted or level III lymph nodes, and less than three positive lymph nodes will be considered “low-risk” and will merely undergo PET/CT surveillance every 4 months for 5 years. Patients with a complete resection (as above) and positive LVI, PNI, ≤ 1 mm ECS, and < 3 positive nodes will be considered “intermediate-risk” and will undergo PET/CT surveillance every 4 months for 5 years and postoperative RT with 50 Gy to the primary tumor site. Patients with an incomplete surgical resection with positive surgical margins, more than three positive lymph nodes, ≥ 1 mm ECS, or matted or supraclavicular lymph nodes will be considered “high-risk” and will undergo routine PET/CT surveillance and concurrent cisplatin (40 mg/m2) weekly with 56 Gy RT to the primary tumor site. The primary outcome assessed will be disease-free survival (DFS) and loco-regional control (LRC) at 3 and 5 years posttreatment. Recruitment is planned for 200 patients, and the estimated completion date is March 2019.
The ECOG 33-11 trial (NCT01898494) will examine various adjuvant therapy regimens in patients undergoing transoral surgery in advanced-stage OPSCC patients. Low-risk patients randomized to arm A are those with T1–T2, N0–N1 disease, and clear (> 3 mm margins) with no ENE, PNI, or LVI. Arm A patients will undergo only observation at 7 weeks. Patients in the intermediate-risk group are stratified dichotomously into ≤ 10 pack-years (arm B) or > 10 pack-year (arm C) history of tobacco use and one or more of the following: < 3 mm margins, ≤ 1 mm ENE, N2a disease, PNI, or LVI. Arm B patients with ≤ 10 pack-years will be treated postoperatively with 50 Gy, and arm C patients with > 10 pack-years will be treated with 60 Gy. High-risk patients (arm D), those with positive margins with any T-stage, > 1 mm ENE, or ≥ 5 metastatic lymph nodes will complete 66 Gy and cisplatin 40 mg/m2 weekly. Unknown-risk patients, including those with N2c or N3 disease, will also be treated with 60 Gy. The primary outcome measure is 2-year PFS, with secondary outcomes of swallowing function (MDADI, PSS-HN, MDADI), QOL (FACT-HN), incidence of grade 3–4 bleeding events, and positive margins during surgery. Three hundred seventy-seven patients will be assessed at multiple institutions throughout the USA, and the trial has completed accrual with results being anticipated in the near future.
The ORATOR trial (NCT01590355) will randomize early-stage OPSCC patients to 70 Gy over 7 weeks with 63 Gy and 56 Gy to high- and low-risk nodal areas, respectively, as well as concurrent chemotherapy (unspecified), or TORS and neck dissection. The primary outcome will be QOL 1-year posttreatment, with secondary outcomes of overall survival (OS), PFS, toxicity, and swallowing function. Sixty-eight patients will be recruited, and the estimated completion date is June 2021.
NCT02159703, an ongoing study at the University of Pennsylvania, will enroll 60 HPV-positive T1–2 and/or N2a–c OPSCC patients undergoing TORS and selective neck dissection to receive standard adjuvant RT to the regional nodes (± chemotherapy if indicated), but omitting RT to the primary tumor when completely resected with negative margins according to final pathologic analysis. Primary outcomes will include LRC and adverse events within 2 years. The study remains active and results are expected in 2019.
As the results of multiple surgical trials are on the horizon, clinicians may expect the treatment of both early- and advanced-stage oropharyngeal cancer to change dramatically in the coming decade. Multidimensional analysis of OS and disease-specific survival, as well as functional outcomes with swallowing assessments, and QOL measures will allow for individualized treatment tailored to each patient and their burden of disease.
Conclusions
While combined chemoradiation was the standard-of-choice for much of the twentieth century, advances in transoral surgical techniques such as TORS and TLM have made surgical resection a viable treatment option for patients with stage III–IV OPSCC. Numerous studies have shown that TORS and TLM cannot only achieve favorable oncologic outcomes in these cases but also result in superior long-term swallowing outcomes compared to CCRT. Open surgical approaches, such as lip-split mandibulotomy and lateral pharyngotomy, continue to be practical surgical approaches in the setting of salvage surgery, where wider exposure is often necessary to obtain adequate margins. Currently, there are several ongoing clinical trials investigating the use of TORS to de-escalate postoperative adjuvant therapy. The results of these trials will have major implications for its use as a first-line treatment option for locally advanced OPSCC.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011;29(32):4294–301.
Chaturvedi AK, Engels EA, Anderson WF, Gillison ML. Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States. J Clin Oncol. 2008;26(4):612–9.
Ryerson AB, Peters ES, Coughlin SS, Chen VW, Gillison ML, Reichman ME, et al. Burden of potentially human papillomavirus-associated cancers of the oropharynx and oral cavity in the US, 1998–2003. Cancer. 2008;113(10 Suppl):2901–9.
•• Lydiatt WM, Patel SG, O’Sullivan B, Brandwein MS, Ridge JA, Migliacci JC, et al. Head and neck cancers—major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67(2):122–37 Introduced major changes to the clinical and pathologic staging of oropharyngeal cancers.
Allal AS, Nicoucar K, Mach N, Dulguerov P. Quality of life in patients with oropharynx carcinomas: assessment after accelerated radiotherapy with or without chemotherapy versus radical surgery and postoperative radiotherapy. Head Neck. 2003;25(10):833–9 discussion 9–40.
Calais G, Alfonsi M, Bardet E, Sire C, Germain T, Bergerot P, et al. Randomized trial of radiation therapy versus concomitant chemotherapy and radiation therapy for advanced-stage oropharynx carcinoma. J Natl Cancer Inst. 1999;91(24):2081–6.
Wendt TG, Grabenbauer GG, Rödel CM, Thiel HJ, Aydin H, Rohloff R, et al. Simultaneous radiochemotherapy versus radiotherapy alone in advanced head and neck cancer: a randomized multicenter study. J Clin Oncol. 1998;16(4):1318–24.
Brizel DM, Albers ME, Fisher SR, Scher RL, Richtsmeier WJ, Hars V, et al. Hyperfractionated irradiation with or without concurrent chemotherapy for locally advanced head and neck cancer. N Engl J Med. 1998;338(25):1798–804.
Machtay M, Moughan J, Trotti A, Garden AS, Weber RS, Cooper JS, et al. Factors associated with severe late toxicity after concurrent chemoradiation for locally advanced head and neck cancer: an RTOG analysis. J Clin Oncol. 2008;26(21):3582–9.
Mirghani H, Blanchard P. Treatment de-escalation for HPV-driven oropharyngeal cancer: where do we stand? Clin Transl Radiat Oncol. 2018;8:4–11.
Masterson L, Moualed D, Liu ZW, Howard JE, Dwivedi RC, Tysome JR, et al. De-escalation treatment protocols for human papillomavirus-associated oropharyngeal squamous cell carcinoma: a systematic review and meta-analysis of current clinical trials. Eur J Cancer. 2014;50(15):2636–48.
Chen AM, Felix C, Wang PC, Hsu S, Basehart V, Garst J, et al. Reduced-dose radiotherapy for human papillomavirus-associated squamous-cell carcinoma of the oropharynx: a single-arm, phase 2 study. Lancet Oncol. 2017;18(6):803–11.
Strong MS, Jako GJ, Vaughan CW, Healy GB, Polanyi T. The use of CO2 laser in otolaryngology: a progress report. Trans Sect Otolaryngol Am Acad Ophthalmol Otolaryngol. 1976;82(5):595–602.
Steiner W, Fierek O, Ambrosch P, Hommerich CP, Kron M. Transoral laser microsurgery for squamous cell carcinoma of the base of the tongue. Arch Otolaryngol Head Neck Surg. 2003;129(1):36–43.
Haughey BH, Hinni ML, Salassa JR, Hayden RE, Grant DG, Rich JT, et al. Transoral laser microsurgery as primary treatment for advanced-stage oropharyngeal cancer: a United States multicenter study. Head Neck. 2011;33(12):1683–94.
Rich JT, Milov S, Lewis JS, Thorstad WL, Adkins DR, Haughey BH. Transoral laser microsurgery (TLM) +/- adjuvant therapy for advanced stage oropharyngeal cancer: outcomes and prognostic factors. Laryngoscope. 2009;119(9):1709–19.
Rich JT, Liu J, Haughey BH. Swallowing function after transoral laser microsurgery (TLM) ± adjuvant therapy for advanced-stage oropharyngeal cancer. Laryngoscope. 2011;121(11):2381–90.
Shiley SG, Hargunani CA, Skoner JM, Holland JM, Wax MK. Swallowing function after chemoradiation for advanced stage oropharyngeal cancer. Otolaryngol Head Neck Surg. 2006;134(3):455–9.
Weinstein GS, O’Malley BW, Hockstein NG. Transoral robotic surgery: supraglottic laryngectomy in a canine model. Laryngoscope. 2005;115(7):1315–9.
Weinstein GS, O’Malley BW, Magnuson JS, Carroll WR, Olsen KD, Daio L, et al. Transoral robotic surgery: a multicenter study to assess feasibility, safety, and surgical margins. Laryngoscope. 2012;122(8):1701–7.
Bhayani MK, Holsinger FC, Lai SY. A shifting paradigm for patients with head and neck cancer: transoral robotic surgery (TORS). Oncology (Williston Park). 2010;24(11):1010–5.
Weinstein GS, O’Malley BW, Rinaldo A, Silver CE, Werner JA, Ferlito A. Understanding contraindications for transoral robotic surgery (TORS) for oropharyngeal cancer. Eur Arch Otorhinolaryngol. 2015;272(7):1551–2.
• de Almeida JR, Byrd JK, Wu R, Stucken CL, Duvvuri U, Goldstein DP, et al. A systematic review of transoral robotic surgery and radiotherapy for early oropharynx cancer: a systematic review. Laryngoscope. 2014;124(9):2096–102 A large systematic review comparing effectiveness of TORS versus IMRT for early T-stage oropharyngeal cancer.
Weinstein GS, O’Malley BW, Cohen MA, Quon H. Transoral robotic surgery for advanced oropharyngeal carcinoma. Arch Otolaryngol Head Neck Surg. 2010;136(11):1079–85.
Weinstein GS, Quon H, O’Malley BW, Kim GG, Cohen MA. Selective neck dissection and deintensified postoperative radiation and chemotherapy for oropharyngeal cancer: a subset analysis of the University of Pennsylvania transoral robotic surgery trial. Laryngoscope. 2010;120(9):1749–55.
Starmer HM, Quon H, Kumar R, Alcorn S, Murano E, Jones B, et al. The effect of radiation dose on swallowing: evaluation of aspiration and kinematics. Dysphagia. 2015;30(4):430–7.
Wilson JA, Carding PN, Patterson JM. Dysphagia after nonsurgical head and neck cancer treatment: patients’ perspectives. Otolaryngol Head Neck Surg. 2011;145(5):767–71.
Dziegielewski PT, Teknos TN, Durmus K, Old M, Agrawal A, Kakarala K, et al. Transoral robotic surgery for oropharyngeal cancer: long-term quality of life and functional outcomes. JAMA Otolaryngol Head Neck Surg. 2013;139(11):1099–108.
Kelly JR, Park HS, An Y, Contessa JN, Yarbrough WG, Burtness BA, et al. Comparison of survival outcomes among human papillomavirus-negative cT1-2 N1-2b patients with oropharyngeal squamous cell cancer treated with upfront surgery vs definitive chemoradiation therapy: an observational study. JAMA Oncol. 2017;3(8):1107–11.
Kelly JR, Park HS, An Y, Yarbrough WG, Contessa JN, Decker R, et al. Upfront surgery versus definitive chemoradiotherapy in patients with human papillomavirus-associated oropharyngeal squamous cell cancer. Oral Oncol. 2018;79:64–70.
Butlin HT. Diseases of the tongue. London: Cassel & Company; 1885. p. 324–32.
Trotter W. A method of lateral pharyngotomy for the exposure of large growths of the epilaryngeal region. Proc R Soc Med. 1920;13(Laryngol Sect):196–8.
Dziegielewski PT, Mlynarek AM, Dimitry J, Harris JR, Seikaly H. The mandibulotomy: friend or foe? Safety outcomes and literature review. Laryngoscope. 2009;119(12):2369–75.
Parsons JT, Mendenhall WM, Stringer SP, Amdur RJ, Hinerman RW, Villaret DB, et al. Squamous cell carcinoma of the oropharynx: surgery, radiation therapy, or both. Cancer. 2002;94(11):2967–80.
Mendenhall WM, Amdur RJ, Stringer SP, Villaret DB, Cassisi NJ. Radiation therapy for squamous cell carcinoma of the tonsillar region: a preferred alternative to surgery? J Clin Oncol. 2000;18(11):2219–25.
Laccourreye O, Benito J, Menard M, Garcia D, Malinvaud D, Holsinger C. Lateral pharyngotomy for selected invasive squamous cell carcinoma of the lateral oropharynx—part I: how. Laryngoscope. 2013;123(11):2712–7.
Pang P, Li RW, Shi JP, Xu ZF, Duan WY, Liu FY, et al. A comparison of mandible preservation method and mandibulotomy approach in oral and oropharyngeal cancer: a meta-analysis. Oral Oncol. 2016;63:52–60.
Goodwin WJ. Salvage surgery for patients with recurrent squamous cell carcinoma of the upper aerodigestive tract: when do the ends justify the means? Laryngoscope. 2000;110(3 Pt 2 Suppl 93):1–18.
Röösli C, Studer G, Stoeckli SJ. Salvage treatment for recurrent oropharyngeal squamous cell carcinoma. Head Neck. 2010;32(8):989–96.
Patel SN, Cohen MA, Givi B, Dixon BJ, Gilbert RW, Gullane PJ, et al. Salvage surgery for locally recurrent oropharyngeal cancer. Head Neck. 2016;38(Suppl 1):E658–64.
• Owadally W, Hurt C, Timmins H, Parsons E, Townsend S, Patterson J, et al. PATHOS: a phase II/III trial of risk-stratified, reduced intensity adjuvant treatment in patients undergoing transoral surgery for human papillomavirus (HPV) positive oropharyngeal cancer. BMC Cancer. 2015;15:602 A multicenter phase II/III randomized controlled trial stratifying patients with HPV-positive OPSCC undergoing TORS resection into groups based on pathological risk factors for recurrence for adjuvant treatment.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Head and Neck Cancer
Rights and permissions
About this article
Cite this article
Qureshi, H.A., Abouyared, M., Barber, B. et al. Surgical Options for Locally Advanced Oropharyngeal Cancer. Curr. Treat. Options in Oncol. 20, 36 (2019). https://doi.org/10.1007/s11864-019-0621-x
Published:
DOI: https://doi.org/10.1007/s11864-019-0621-x