Opinion statement
Anthracycline-based regimens have been an important treatment component for patients with breast cancer. As demonstrated in the last Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) meta-analysis, anthracycline-based regimens decrease breast cancer mortality by 20–30%. Anthracycline toxicities include the rare—but potential morbid—cardiotoxicity or leukemogenic effect, and the almost universal—but very distressing—alopecia. Due to potential toxicities, and large number of patients being exposed, several worldwide trials have re-examined the role of anthracycline-based regimens in the management of breast cancer. Current literature supports that anthracyclines are not required for all patients with breast cancer and should be avoided in those with high cardiac risk. Recent results from the ABC trials suggest that anthracyclines should not be spared for patients with triple negative breast cancer (regardless of axillary node involvement) or HER2−/ER+ with significant node involvement. Based on current literature, for HER2-negative patients with low-risk breast cancer, anthracyclines could be spared with regimens such as cyclophosphamide, methotrexate, and fluorouracil (CMF) or docetaxel and cyclophosphamide (TC). Patients with intermediate or high-risk breast cancer should be considered for anthracycline-based regimens based on other factors such as age, comorbidities, tumor grade, lymphovascular invasion, and genomic profiling. Patients with HER2-positive breast cancer with low risk could be treated with paclitaxel and trastuzumab. For the remaining patients with HER2 overexpression, while docetaxel, carboplatin, and trastuzumab (TCH) has demonstrated to improve disease-free survival (DFS), anthracycline-containing regimens should be discussed, especially for those with very high-risk breast cancer. Although several biomarkers, such as topoisomerase II (TOP2A) and chromosome 17 centromeric duplication (Ch17CEP) have been proposed to predict benefit from anthracycline regimens, further research is required to delineate their proper utility in the clinical setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) is the most common malignancy and a leading cause of cancer-related death among women worldwide [1, 2]. Approximately 80% of patients present with local or locally advanced disease and undergo resection, followed by adjuvant therapies which may include chemotherapy, endocrine, biologic, or radiation therapy. Mortality from BC has been steadily decreasing since 1989. The 5-year overall survival (OS) rates for patients with stage I and stage II BC are around 99 and 93%, respectively [3]. This improvement in OS can be attributed to improved screening, as well as more effective adjuvant systemic therapeutic options [4]. Early in the 1970s, chemotherapy was explored in the management of BC, and with further studies, anthracyclines have been incorporated into the backbone of adjuvant regimens. Anthracycline-based regimens have led to significant improvement in clinical outcomes [5], but these regimens are also associated with adverse events [6, 7]. In the present article, we review the role of anthracyclines in the management of early stage BC.
Pharmacologic and toxicity profile of anthracyclines
Derived in the 1950s from rhodomycin B, anthracyclines were isolated from a species of actinomyces, Streptomyces peucetius, and demonstrated antibacterial activity in vitro. Anthracyclines exert their antitumor effects via three mechanisms [8]: (A) Through interaction with the DNA gyrase, topoisomerase II (TOP2A), anthracyclines can intercalate DNA to form a “drug-stabilized cleavable complex,” causing double-stranded chromosomal DNA breaks which inhibits transcription and replication, leading to cell cycle arrest and apoptosis [9]. (B) Anthracyclines can modulate signal transduction pathways such as the Fas ligand pathway which has been implicated in growth inhibition [10][8]. (C) Anthracyclines can generate reactive oxygen species (ROS) which can induce DNA damage and lipid peroxidation, known to be the mechanism behind anthracycline-induced cardiotoxicity [11]. In fact, dexrazoxane, an agent used to prevent cardiotoxicity from anthracyclines, acts by chelating iron and reducing the formation of ROS [12]. The most worrisome toxicities associated with anthracyclines include cardiotoxicity and leukemogenic effects, whereas alopecia is almost universal with these regimens [6, 7, 13,14,15].
Anthracycline cardiotoxicity
Anthracyclines can accumulate in the mitochondria of myocardial cells, inhibiting oxidative phosphorylation and generating ROS, leading to endomyocardial interstitial fibrosis and vacuolation [16, 17]. Cardiac acute/subacute toxicity can start either at the time of infusion or within the first 2–3 days and includes arrhythmias, supraventricular tachycardia, and hemodynamic instability [18]. Chronic dilated cardiomyopathy occurs in a dose-dependent manner and is observed at peak incidence 1 to 3 months post exposure, but cases have been reported several years after initial therapy [19].
Risk factors for anthracycline-induced cardiotoxicity include previous cardiac disease, gender, age, prior mediastinal irradiation, and concomitant exposure to other cardiotoxic agents such as trastuzumab [20, 21]. Moreover, cardiotoxicity risk correlates to cumulative doses of anthracyclines [22, 23]. In a retrospective review of three phase III trials (two breast cancer trials and one lung cancer trial), doxorubicin-related congestive heart failure (CHF) was defined as cardiomegaly on chest X-ray, basilar rales, S3 gallop, or either paroxysmal nocturnal dyspnea, orthopnea, or significant dyspnea on exertion. Doxorubicin-related CHF was identified in 5 or 26% of patients treated at a cumulative doxorubicin dose of 400 or 550 mg/m2, respectively, and 66% of these patients had decline in left ventricular ejection fraction (LVEF) 0–30% from baseline while on study. Cardiac events were defined as a decline in absolute value ≥ 20% in LVEF from baseline, a decline in absolute value ≥ 10% in LVEF from baseline and to below 50%the institution’s lower limit of normal (LLN), a postbaseline decline in absolute value ≥ 5% in LVEF below the institution’s LLN, or the occurrence of CHF on study. Cardiac events were identified in 9 or 65% of patients at a cumulative doxorubicin dose of 250 or 550 mg/m2, respectively [15]. In addition, a review of the Surveillance, Epidemiology, and End Results (SEER) Medicare database showed that among women aged 66–70 years with stage I–III breast cancer and no history of CHF, those who received anthracycline-based regimen had a higher incidence of CHF (identified through claims in Medicare inpatient, outpatient, and physician files containing ICD-09 of CHF) compared to those receiving other regimens (hazard ratio [HR] = 1.26, 95% confidence interval [CI] 1.12–1.42) [24]. Each anthracycline drug differs with respect to their pharmacokinetic profile and the cumulative dose at which chronic cardiotoxicity can develop (Table 1).
With the introduction of anti-HER2 agents, concomitant infusion of trastuzumab and anthracyclines became a challenge given significant increase in cardiac toxicity in trials evaluating concurrent use of these drugs. The herceptin adjuvant (HERA) trial showed a 1.73% 1-year incidence of symptomatic CHF in the group receiving trastuzumab (with 94% of these patients previously undergoing anthracycline-based chemotherapy) vs. 0.06% in the observation group, while the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-31 trial showed a 4.1% 3-year incidence of New York Heart Association (NYHA) Class III or IV heart failure in trastuzumab and anthracycline-treated patients vs. 0.8% in the control group [25, 26].
Current American Society of Clinical Oncology (ASCO) guidelines define a subset of patients that are at a higher risk of developing cardiac dysfunction following treatment with anthracyclines [27•]. These include patients who (1) receive high-dose anthracyclines (doxorubicin > 250 mg/m2 or epirubicin > 600 mg/m2), (2) receive low-dose anthracyclines (doxorubicin < 250 mg/m2 or epirubicin < 600 mg/m2) with concomitant lower dose radiation therapy (< 30 Gy) involving the heart in the treatment field, (3) receive low-dose anthracyclines and have multiple cardiovascular risk factors (smoking, hypertension, hyperlipidemia, diabetes or obesity), are older than 60 years of age or have baseline cardiac dysfunction (LVEF < 50%), or (4) receive low-dose anthracyclines followed by trastuzumab. For these patients, ASCO recommends obtaining echocardiogram, or if not available, either cardiac magnetic resonance imaging (MRI) or multigated acquisition (MUGA) scan, with serum cardiac biomarkers if there is evidence of cardiac dysfunction on physical exam [27•]. Although dexrazoxane is approved for use to prevent anthracycline-related toxicity, there is concern that it might lead to decreased antitumor efficacy [28]. Not only does it inhibit formation of ROS, but it is also a TOP2A inhibitor, directly interfering with anthracycline activity [29]. ASCO recommends against routine use of prophylactic dexrazoxane in the adjuvant setting, limiting their use to patients who have received cumulative doses of anthracyclines up to 300 mg/m2, but may still benefit from continued use [30].
Anthracycline-associated leukemogenic effect
There is also evidence that anthracyclines are potentially leukemogenic, particularly when combined with platinums or alkylators [31, 32]. Both acute myelogenous leukemia (AML) and myelodysplastic syndrome (MDS) have been observed, with a relatively short time to onset of 2–3 years [33]. Translocations in chromosome 11q23, 21q22, and 3q23 have been implicated in the pathogenesis of anthracycline-induced leukemia [33]. Similar to cardiotoxicity, a cumulative dose effect has also been observed in anthracycline-induced leukemia. In an analysis of 19 randomized trials, there were 7110 patients treated with epirubicin (92% of whom received cyclophosphamide) and the 8-year risk of developing treatment-related AML/MDS was 0.55% (95% CI, 0.33–0.78) with the risk being higher as the epirubicin dose per cycle and cumulative doses of epirubicin with cyclophosphamide increased. In particular, for patients who received a total dose of epirubicin and cyclophosphamide less than the standard dose (< 720 and < 6300 mg/m2, respectively), the 8-year cumulative probability of AML/MDS was 0.37% (95% CI, 0.13–0.61) compared to 4.97% (95% CI, 2.06–7.87) for those who received higher than standard cumulative doses of the same drugs [13].
Among 20,063 patients in the National Comprehensive Cancer Network (NCCN) with stage I to III breast cancer treated between 1998 and 2007, 50 patients developed treatment-associated marrow neoplasm(MN) (not limited to AML/MDS); of these, 14 had received no chemotherapy, while 30 and 6 patients had received 4 and 6 cycles of chemotherapy (anthracycline and/or cyclophosphamide), respectively. The probability of OS after MN diagnosis was 50% at 1 year and 30% at 2 years. The MN risk was similar for those treated with surgery plus radiation compared with surgery alone (HR = 2.6, 95% CI 0.57–11.9, P = 0.21). However, there was a significant increase in MN risk among patients treated with both surgery plus chemotherapy (HR = 6.8, 95% CI 1.3–36.1, P = 0.03) and those treated with all three modalities (HR = 7.6, 95% CI 1.6–35.8, P = 0.01). The cumulative incidence of MN doubled between years 5 (0.27%) and 10 (0.49%) for those receiving chemotherapy. In addition, the incidence of MN was greater than that observed in general SEER population after controlling for age and race (50 vs. 14.1 cases, observed/expected ratio = 3.6, 95% CI 2.6–4.6, P < 0.01) [34••].
Anthracycline-induced alopecia
Alopecia is almost universal for patients receiving adjuvant anthracyclines for breast cancer and is rated by patients as one of the most distressing adverse toxicities [35, 36]. Scalp cooling can cause cutaneous vasoconstriction in the scalp which reduces blood—and chemotherapy—uptake in the hair follicles, and reduces biochemical activity, which make hair follicle less susceptible to chemotherapy-induced damage [37]. In the multicenter, randomized, non-blinded scalp cooling to prevent chemo-related hair loss (SCALP) trial, women with early breast cancer undergoing adjuvant chemotherapy were randomized to scalp cooling or not, and the outcome hair preservation was defined as grade 0 (no hair loss) or grade 1 (< 50% hair loss not requiring a wig) alopecia. For those who received anthracycline-based regimen, none of the patient in the non-cooling arm achieved hair preservation, whereas the cooling arm achieved a hair preservation rate of 16% (95% CI, 4–46) [38].
The role of adjuvant chemotherapy in breast cancer
Adjuvant chemotherapy, targeted to treat micrometastatic disease, has improved breast cancer mortality and recurrence [39••, 40••]. After initial trials with adjuvant melphalan monotherapy showing improvement in disease-free survival (DFS) in early BC [41], Bonadonna et al. proposed a move towards combination chemotherapy [42] comparing cyclophosphamide, methotrexate, and fluorouracil (CMF) (N = 207) for 12 cycles vs. placebo (N = 179) in premenopausal and postmenopausal patients who had undergone radical mastectomy and had one or more histologically proven positive axillary lymph nodes. Treatment failure, defined as local, regional, or distant recurrence, occurred in 24% of placebo patients and 5.3% of patients in the combination chemotherapy arm (P < 0.01) at 27-month follow-up [42]. These results demonstrated that there was a benefit to treating operable disease with adjuvant chemotherapy. A meta-analysis performed by Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) showed that adjuvant chemotherapy with regimens such as CMF improves 10-year breast cancer recurrence (relative risk (RR )= 0.70, 2P < 0.001) and mortality (RR = 0.76, 2P < 0.001) compared to placebo[40••].
Pivotal trials of anthracyclines in the management of early breast cancer
The concept that anthracyclines could be effectively incorporated into adjuvant chemotherapeutic regimens was first proposed by the NSABP B-11 study which found a significant improvement in DFS with the addition of doxorubicin to melphalan (L-PAM) and fluorouracil (PAF); doxorubicin treatment was not associated with increase in hematologic and cardiac toxicity [43]. Patients were defined as “tamoxifen-nonresponders,” i.e., less than 49 years of age, or 50–59 years with progesterone receptor (PR) levels less than 10 fmol/mg of cytosolic protein. Estrogen receptor (ER) status was not taken into consideration [44]. Although these early studies were suggestive of a benefit to the addition of anthracyclines, it was not until the NSABP B-15 study that anthracyclines were adopted as standard of care. In the NSABP B-15 trial, 6 cycles of CMF were compared to 4 cycles of doxorubicin plus cyclophosphamide (AC) and 4 cycles of AC followed by 3 cycles of CMF among 2194 women with at least one histologically axillary lymph node-positive, tamoxifen non-responsive, operable BC [5]. There was no significant statistical difference in 3-year DFS (P = 0.5) or OS (P = 0.8) among the three groups. However, the AC regimen could be given over a shorter course of time (63 vs. 154 days). In addition, AC was associated with milder short-term toxicities such as nausea, vomiting, or infusion site reactions.
Epirubicin was investigated in BC management given decreased cardiotoxicity and potentially equivalent antitumor effect compared to doxorubicin. In a combined analysis of the French Adjuvant Study Group (FASG) 02 and 07 trials to determine the role of epirubicin in chemo-hormonal therapy, 457 patients with ER+, axillary node-positive BC received tamoxifen with or without fluorouracil, epirubicin (50 mg/m2), and cyclophosphamide for six 21-day cycles (FEC50). Addition of FEC50 to tamoxifen improved 9-year DFS (84 vs. 72%, P = 0.008), with similar OS (86 vs. 78%, P = 0.11) [45]. The EBCTCG meta-analysis demonstrated that anthracycline-based regimes improve 10-year breast cancer mortality (RR = 0.79, 2P < 0.001) and recurrence (RR = 0.73, 2P < 0.001) compared to no chemotherapy. Moreover, AC for 4 cycles vs. CMF were equivalent for recurrence (RR = 0.99, 95% CI 0.90–1.08, 2P = 0.76) and breast cancer-related mortality (RR = 0.98, 95% CI 0.89–1.08, 2P = 0.67) [40••].
Role of anthracyclines in modern era
Anthracycline-free regimens
Taxanes were found to have clinical activity in breast cancer [46••], and trials have investigated taxane-based regimens that exclude anthracyclines due to their potential long-term toxicities [47]. The US Oncology Research trial group 9735 enrolled 1016 women with both node positive and negative operable BC, and randomized them to 4 cycles of docetaxel plus cyclophosphamide (TC) or AC [48]. At 7-year follow-up, DFS was improved with TC (81 vs. 75%, HR = 0.74, 95% CI 0.56–0.98, P = 0.033), and OS also favored the TC arm (87 vs. 82%, HR = 0.69, 95% CI 0.50–0.97, P = 0.032). Grade 3–4 anemia occurred more frequently in older women receiving AC compared to TC (5 vs. < 1%), whereas the incidence of febrile neutropenia was higher among older women in the TC arm compared to AC arm (8 vs. 4%). There were three treatment-related deaths without relapse, all in the AC group, one due to cardiomyopathy and CHF, and two older patients dying secondary to complications related to MDS and myelofibrosis.
A significant limitation of earlier adjuvant trials in BC was the unintentional inclusion of patients with HER2-positive disease. Given that HER2 expressing tumors have increased sensitivity to anthracyclines, it has been argued that the inclusion of such patients may have led to an overestimation of the benefit derived from anthracyclines. The ABC trials are a joint analysis of three sequential trials, USOR 06-090 (N = 1286), NSABP B-46 (N = 1051), and NSABP B-49 (N = 1819), which randomized women with node-positive or high-risk node-negative early stage, HER2-negative BC to either TC for 6 cycles (TC6) or one of the several available taxane and anthracycline-based regimens (TaxAC) which most often included docetaxel as the taxane of choice [49••]. These anthracycline-based regimens included (1) docetaxel, doxorubicin, and cyclophosphamide (TAC) every 21 days for 6 cycles; (2) AC every 3 weeks for 4 cycles followed by weekly paclitaxel for 12 cycles; (3) dose-dense AC every 2 weeks for 4 cycles followed by paclitaxel for 12 weeks; and (4) dose-dense AC followed by paclitaxel every 2 weeks for 4 cycles. These trials were designed to determine whether TC6 was non-inferior to the standard TaxAC regimen with the primary endpoint being invasive DFS (IDFS). Follow-up in the studies ranged from 2.2 to 6.3 years, and included 2094 women in the TC6 group and 2062 women in the TaxAC group, with 40% being node negative. The 4-year IDFS rate was 88.2% in the TC6 group vs. 90.7% in the TaxAC group (HR = 1.23, 95% CI 1.01–1.50, P = 0.04). Planned exploratory interaction tests by protocol, hormone receptor status, and nodal status were negative, with a suggested benefit favoring TaxAC in the hormone-negative group (HR 1.42, 95% CI 1.04–1.94) but not for hormone-positive patients (HR 1.12, 95% CI 0.86–1.45). However, unplanned interaction tests by combined hormone receptor and nodal status revealed a statistically significant interaction for hormone-positive and nodal status (P = 0.026) with suggested benefit of TaxAC for node-positive patients (0 nodes: HR 0.69, 95% CI 0.39–1.19; 1–3 nodes: HR 1.14, 95% CI 0.77–1.69; ≥ 4 nodes: HR 1.46, 95% CI 0.95–2.26), but interaction test was not statistically significant for hormone-negative patients (P = 0.71). Five out of 2062 patients (0.24%) in the TaxAC cohort developed leukemia, whereas no cases were seen in the TC6 cohort. These results revealed that TC6 is statistically inferior to TaxAC in terms of IDFS, suggesting that anthracyclines should not be spared in patients with high risk of breast cancer recurrence such as those with triple negative disease or HER2−/hormone positive with significant axillary node involvement [49••].
Dose-dense anthracycline regimens
The C9741 trial evaluated the effect of dose density (2 vs. 3 weeks) and treatment sequence (concurrent vs. sequential) in patients with operable breast cancer by randomizing 2005 patients (with 1973 included in final analysis) to four different treatment arms using a 2 × 2 factorial design: (1) concurrent AC-paclitaxel vs. sequential AC-paclitaxel and (2) every 3 weeks vs. a dose-dense regimen every 2 weeks [50]. Multivariate Cox analysis showed prolonged DFS for dose-dense regimens (RR = 0.74, 95% CI 0.59–0.93, P = 0.01) but no difference in concurrent vs. sequential therapy (RR = 0.93, 95% CI 0.75–1.18, P = 0.58). Similar findings were also observed for OS favoring dose-dense regimens (RR = 0.69, 95% CI 0.50–0.93, P = 0.013) with no significant difference for concurrent vs. sequential therapy (RR = 0.89, 95% CI 0.66–1.20, P = 0.48) [50]. In a meta-analysis, three trials, enrolling 3337 patients, evaluated the effect of dose-dense chemotherapy. Dose-dense chemotherapy improved OS (HR = 0.84; P = 0.03) and DFS (HR = 0.83; P = 0.005) compared to conventional schedule, although no benefit was observed in patients with hormone receptor-positive tumors [51].
Role of anthracyclines in HER2-positive breast cancer
The initial trials for adjuvant BC predate the utilization of anti-HER2 therapy [52]. Earlier studies of HER2 expressing cancers showed relative resistance to chemotherapy, throwing into uncertainty the efficacy of combination therapy [53, 54]. However, a significant limitation of those studies was the use of CMF instead of the standard AC regimen. In the CALGB-8541 trial, patients with HER2 overexpression who received higher doses of anthracycline-based chemotherapy [doxorubicin, cyclophosphamide, and fluorouracil (FAC)] had longer DFS and OS, compared to those who received the low-dose regimen [55, 56].
Trastuzumab, a humanized monoclonal antibody directed against the extracellular subdomain IV of the HER2 receptor, was approved by the Food and Drug Administration for the management of metastatic BC in 1998 [57]. In a joint analysis of the NSABP B-31 and NCCTG N9831 trials involving 3351 women with early BC, addition of 52-week trastuzumab to doxorubicin, cyclophosphamide, and paclitaxel improved the primary endpoint DFS (HR = 0.48, 95% CI 0.39–0.59, P < 0.001) and OS (HR = 0.67, 95% CI 0.48–0.93, P = 0.015) [26, 58•].
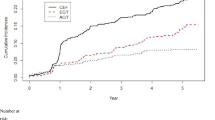
Although the exact mechanism of trastuzumab-induced cardiomyopathy remains unclear, in vivo studies have shown that in mice pretreated with anthracyclines, trastuzumab can cause myofibrillar disarray, potentiating the cardiotoxicity already caused by anthracyclines [59]. The BCIRG-006 trial (N = 3222) was conducted to compare a chemotherapy regimen of AC followed by docetaxel (AC-T) vs. chemotherapy plus 52-week trastuzumab (AC plus docetaxel/trastuzumab [ACTH] or docetaxel, carboplatin, and trastuzumab [TCH]) [60••]. After 10-year follow-up, when compared to the control arm AC-T, DFS was improved by ACTH (74.6 vs. 67.9%, P < 0.0001) and TCH (73 vs. 67.9%, P = 0.0011). However, in the ACTH arm, there were 21 cases of grade 3/4 CHF, 7 cases of leukemia, and 200 cases of ≥ 10% decrease in LVEF. On the other hand, in the TCH group, there were 4 cases of grade 3/4 CHF, no cases of leukemia, and 97 cases of decreased LVEF [61]. This study was not adequately powered to prove non-inferiority between the two trastuzumab-containing regimens. There was a numerical benefit to receiving ACTH over TCH with respect to preventing BC recurrences (124 vs. 144 events), leading to the question of whether a better powered trial would demonstrate a bigger difference between the two regimens [62]. Although there was certainly a significant increase in the risk of cardiomyopathy, there were no deaths reported in the trial from CHF, leading to the question of whether the benefit of ACTH was offset by cardiac toxicity. In addition, critics argue that the study employed every 3-week dosing of anthracyclines which has previously been shown to be inferior to dose-dense regimens of every 2-week schedule, thus limiting the optimal use of anthracyclines.
An overview of important anthracycline-based trials for all breast cancer subtypes is provided in Table 2. In addition, Fig. 1 provides an illustration of the timeline of introduction of anthracyclines into adjuvant regimens and its evolution over the last few decades.
Biomarkers to predict anthracycline efficacy
Retrospective analysis of randomized trials suggested that anthracycline-based regimens had increased efficacy in patients with HER2 overexpression [64], and other studies suggested that the reason for this increased efficacy was amplification—and possible deletion—of the TOP2A gene [65, 66] which has been found to be amplified in 35% of HER2-positive BC [67]. Interestingly, the TOP2A and HER2 genes are both located on chromosome 17q21–22.
One of the first studies to show increased efficacy of anthracyclines in TOP2A-amplified BC was a retrospective analysis of the Danish Breast Cancer Cooperative Group (DBCCG) 89D trial, which examined the efficacy of substituting methotrexate for epirubicin (CMF vs. CEF) in 980 premenopausal and postmenopausal women with early stage operable BC [68]. In this retrospective analysis, TOP2A amplification and deletion was seen in 12 and 11.3% of patients, respectively. Patients with TOP2A amplifications had an improved recurrence-free survival [RFS] (HR = 0.43, 95% CI 0.24–0.78) and OS (HR = 0.57, 95% CI 0.29–1.13) when treated with CEF compared to CMF; of note, similar results were found for TOP2A deletion. On the other hand, in patients with a normal TOP2A genotype, similar outcomes were observed between the two treatment arms [66]. In a meta-analysis of five randomized adjuvant trials, the benefit of treatment with anthracyclines over treatment with CMF was greater for individuals with HER2 gene amplification than it was for individuals without HER2 gene amplification when analyzing event-free survival (EFS) (P for interaction = 0.0485), but not when analyzing OS (P for interaction = 0.071); moreover, there was no significant difference in the benefit of treatment with anthracyclines over treatment with CMF when assessing the three separate TOP2A cohorts (normal, deleted, or amplified) in terms of either EFS (P for interaction = 0.0513) or OS (P for interaction = 0.1608) [69]. These results suggest that the benefit of anthracyclines is not limited to patients with HER2 amplification or TOP2A amplification/deletion.
Chromosome 17 centromeric duplication (Ch17CEP) has also been evaluated as a potential predictive biomarker for anthracycline sensitivity [70]. In a pooled analysis of five trials that compared anthracycline-based chemotherapy with CMF, both CEP17and TOP2A treatment-by-marker interactions remained significant in adjusted analyses for RFS and OS, whereas HER2 did not. A combined CEP17 and TOP2A-adjusted model predicted anthracycline benefit across all five trials for both RFS (HR = 0.64; P = 0.001) and OS (HR = 0.66; P = 0.005) [71]. These data suggest that HER2 might not be a predictor of benefit from anthracyclines, and CEP17 and TOP2A alterations seem like potential biomarkers of anthracycline benefit regardless of HER2 status. However, it is unknown whether these results are maintained for regimens that include either concurrent or sequential taxanes.
Genomic profiling is being used to tailor management of ER+ breast cancer (Oncotype DX Recurrence score, MammaPrint, PAM50) [72, 73]. However, these agents have not been designed to decide specific chemotherapy regimens to be used. Gene signatures based in DNA damage repair pathways have been reported as potential biomarkers of anthracyclines in ER+ and ER− BC. However, these signatures require prospective validation before being considered as routine tools in the management of breast cancer. Currently, there is no indication for routine testing of these biomarkers to select specific chemotherapy regimens during clinical care of patients with breast cancer.
Conclusions
Anthracycline-based regimens are an important component in the management of patients with breast cancer, especially for patients with high risk of recurrence such as those with triple negative disease (regardless of axillary node involvement) or HER2−/ER+ with axillary node involvement. While cardiotoxicity and secondary hematological malignancies associated with anthracyclines have low incidence, the morbidity associated with these treatment-related complications could be significant; therefore, clinicians must carefully assess the risk/benefit of anthracycline use in patients who are at risk of these complications. Further research is required to identify biomarkers predictive of anthracycline response in breast cancer.
Abbreviations
- BC:
-
Breast cancer
- OS:
-
Overall survival
- TOP2A:
-
Topoisomerase 2A
- ROS:
-
Reactive oxygen species
- SEER:
-
Surveillance, Epidemiology, and End Results
- LVEF:
-
Left ventricular ejection fraction
- CHF:
-
Congestive heart failure
- HR:
-
Hazard ratio
- RR:
-
Relative risk
- NSABP:
-
National Surgical Adjuvant Breast and Bowel Project
- ASCO:
-
American Society of Clinical Oncology
- AML:
-
Acute myelogenous leukemia
- MDS:
-
Myelodysplastic syndrome
- DFS:
-
Disease-free survival
- CMF:
-
Cyclophosphamide, methotrexate, and fluorouracil
- L-PAM:
-
L-Phenylalanine mustard
- PAF:
-
L-PAM and fluorouracil
- PR:
-
Progesterone receptor
- ER:
-
Estrogen receptor
- AC:
-
Doxorubicin and cyclophosphamide
- CEF:
-
Cyclophosphamide, epirubicin, and fluorouracil
- TC:
-
Docetaxel and cyclophosphamide
- FAC:
-
Doxorubicin, cyclophosphamide, and fluorouracil
- FASG:
-
French Adjuvant Study Group
- TaxAC:
-
Taxane and anthracycline-based regimen
- TNBC:
-
Triple negative breast cancer
- EFS:
-
Event-free survival
- ACTH:
-
AC plus docetaxel and trastuzumab
- TCH:
-
Docetaxel, carboplatin, and trastuzumab
- FEC100:
-
Fluorouracil, epirubicin, and cyclophosphamide
- EC-D:
-
Epirubicin and cyclophosphamide followed by docetaxel
- Ch17CEP:
-
Chromosome 17 centromeric duplication
- CDK4/6:
-
Cyclin-dependent kinases 4/6
- Rb:
-
Retinoblastoma
- E2F:
-
Elongation factor 2
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance•• Of major importance.
Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA: Cancer J Clinicians. 2010;60(5):277–300. https://doi.org/10.3322/caac.20073.
Howlader N, Chen VW, Ries LA, et al. Overview of breast cancer collaborative stage data items—their definitions, quality, usage, and clinical implications: a review of SEER data for 2004–2010. Cancer. 2014 Dec 1;120(Suppl 23):3771–80. https://doi.org/10.1002/cncr.29059.
DeSantis C, Ma J, Bryan L, et al. Breast cancer statistics, 2013. CA: Cancer J Clinicians. 2014 Jan-Feb;64(1):52–62. https://doi.org/10.3322/caac.21203.
Berry DA, Cronin KA, Plevritis SK, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005 Oct 27;353(17):1784–92. https://doi.org/10.1056/NEJMoa050518.
Fisher B, Brown AM, Dimitrov NV, et al. Two months of doxorubicin-cyclophosphamide with and without interval reinduction therapy compared with 6 months of cyclophosphamide, methotrexate, and fluorouracil in positive-node breast cancer patients with tamoxifen-nonresponsive tumors: results from the National Surgical Adjuvant Breast and Bowel Project B-15. J Clin Oncol: Off J Am Soc Clin Oncol. 1990;8(9):1483–96. https://doi.org/10.1200/JCO.1990.8.9.1483.
Gianni L, Herman EH, Lipshultz SE, et al. Anthracycline cardiotoxicity: from bench to bedside. J Clin Oncol: Off J Am Soc Clin Oncol. 2008;26(22):3777–84. https://doi.org/10.1200/JCO.2007.14.9401.
Balduzzi A, Castiglione-Gertsch M. Leukemia risk after adjuvant treatment of early breast cancer. Womens Health (Lond). 2005;1(1):73–85. https://doi.org/10.2217/17455057.1.1.73.
Beretta GL, Zunino F. Molecular mechanisms of anthracycline activity. Top Curr Chem. 2008;283:1–19. https://doi.org/10.1007/128_2007_3.
Zunino F, Capranico G. DNA topoisomerase II as the primary target of anti-tumor anthracyclines. Anticancer Drug Des. 1990;5(4):307–17.
Friesen C, Herr I, Krammer PH, et al. Involvement of the CD95 (APO-1/FAS) receptor/ligand system in drug-induced apoptosis in leukemia cells. Nat Med. 1996;2(5):574–7.
Myers C. The role of iron in doxorubicin-induced cardiomyopathy. Semin Oncol. 1998;25(4 Suppl 10):10–4.
Kwok JC, Richardson DR. The cardioprotective effect of the iron chelator dexrazoxane (ICRF-187) on anthracycline-mediated cardiotoxicity. Redox Rep. 2000;5(6):317–24. https://doi.org/10.1179/135100000101535898.
Praga C, Bergh J, Bliss J, et al. Risk of acute myeloid leukemia and myelodysplastic syndrome in trials of adjuvant epirubicin for early breast cancer: correlation with doses of epirubicin and cyclophosphamide. J Clin Oncol: Off J Am Soc Clin Oncol. 2005 Jun 20;23(18):4179–91. https://doi.org/10.1200/JCO.2005.05.029.
Shepherd L, Ottaway J, Myles J, et al. Therapy-related leukemia associated with high-dose 4-epi-doxorubicin and cyclophosphamide used as adjuvant chemotherapy for breast cancer. J Clin Oncol: Off J Am Soc Clin Oncol. 1994 Nov;12(11):2514–5. https://doi.org/10.1200/JCO.1994.12.11.2514.
Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97(11):2869–79. https://doi.org/10.1002/cncr.11407.
Siwik DA, Pagano PJ, Colucci WS. Oxidative stress regulates collagen synthesis and matrix metalloproteinase activity in cardiac fibroblasts. Am J Physiol Cell Physiol. 2001;280(1):C53–60.
Melendez GC, Hundley WG. Is myocardial fibrosis a new frontier for discovery in cardiotoxicity related to the administration of anthracyclines? Circ Cardiovasc Imaging. 2016;9(12) https://doi.org/10.1161/CIRCIMAGING.116.005797.
Bristow MR, Thompson PD, Martin RP, et al. Early anthracycline cardiotoxicity. Am J Med. 1978 Nov;65(5):823–32.
Steinherz LJ, Steinherz PG, Tan CT, et al. Cardiac toxicity 4 to 20 years after completing anthracycline therapy. Jama. 1991 Sep 25;266(12):1672–7.
Singal PK, Iliskovic N. Doxorubicin-induced cardiomyopathy. N Engl J Med. 1998 Sep 24;339(13):900–5. https://doi.org/10.1056/NEJM199809243391307.
Lipshultz SE, Lipsitz SR, Mone SM, et al. Female sex and higher drug dose as risk factors for late cardiotoxic effects of doxorubicin therapy for childhood cancer. N Engl J Med. 1995;332(26):1738–43. https://doi.org/10.1056/NEJM199506293322602.
Shulman LN, Berry DA, Cirrincione CT, et al. Comparison of doxorubicin and cyclophosphamide versus single-agent paclitaxel as adjuvant therapy for breast cancer in women with 0 to 3 positive axillary nodes: CALGB 40101 (Alliance). J Clin Oncol: Off J Am Soc Clin Oncol. 2014;32(22):2311–7. https://doi.org/10.1200/jco.2013.53.7142.
Zambetti M, Moliterni A, Materazzo C, et al. Long-term cardiac sequelae in operable breast cancer patients given adjuvant chemotherapy with or without doxorubicin and breast irradiation. J Clin Oncol: Off J Am Soc Clin Oncol. 2001;19(1):37–43. https://doi.org/10.1200/jco.2001.19.1.37.
Pinder MC, Duan Z, Goodwin JS, et al. Congestive heart failure in older women treated with adjuvant anthracycline chemotherapy for breast cancer. J Clin Oncol: Off J Am Soc Clin Oncol. 2007;25(25):3808–15. https://doi.org/10.1200/JCO.2006.10.4976.
Piccart-Gebhart MJ, Procter M, Leyland-Jones B, et al. Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med. 2005 Oct 20;353(16):1659–72. https://doi.org/10.1056/NEJMoa052306.
Romond EH, Perez EA, Bryant J, et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005 Oct 20;353(16):1673–84. https://doi.org/10.1056/NEJMoa052122.
• Armenian SH, Lacchetti C, Barac A, et al. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol: Off J Am Soc Clin Oncol. 2017;35(8):893–911. https://doi.org/10.1200/JCO.2016.70.5400. ASCO guidelines to monitor cardiac dysfunction.
Swain SM, Whaley FS, Gerber MC, et al. Cardioprotection with dexrazoxane for doxorubicin-containing therapy in advanced breast cancer. J Clin Oncol: Off J Am Soc Clin Oncol. 1997;15(4):1318–32. https://doi.org/10.1200/JCO.1997.15.4.1318.
Perry MC, Doll DC, Freter CE. Chemotherapy source book. 5th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2012.
Hensley ML, Hagerty KL, Kewalramani T, et al. American Society of Clinical Oncology 2008 clinical practice guideline update: use of chemotherapy and radiation therapy protectants. J Clin Oncol: Off J Am Soc Clin Oncol. 2009;27(1):127–45. https://doi.org/10.1200/JCO.2008.17.2627.
Pedersen-Bjergaard J, Sigsgaard TC, Nielsen D, et al. Acute monocytic or myelomonocytic leukemia with balanced chromosome translocations to band 11q23 after therapy with 4-epi-doxorubicin and cisplatin or cyclophosphamide for breast cancer. J Clin Oncol: Off J Am Soc Clin Oncol. 1992 Sep;10(9):1444–51. https://doi.org/10.1200/JCO.1992.10.9.1444.
Diamandidou E, Buzdar AU, Smith TL, et al. Treatment-related leukemia in breast cancer patients treated with fluorouracil-doxorubicin-cyclophosphamide combination adjuvant chemotherapy: the University of Texas M.D. Anderson Cancer Center experience. J Clin Oncol: Off J Am Soc Clin Oncol. 1996;14(10):2722–30. https://doi.org/10.1200/JCO.1996.14.10.2722.
Arriagada R, Gutierrez J. Anthracyclines: is more, better and/or more dangerous? Ann Oncol: Off J Eur Soc Med Oncol / ESMO. 2003;14(5):663–5.
•• Wolff AC, Blackford AL, Visvanathan K, et al. Risk of marrow neoplasms after adjuvant breast cancer therapy: the national comprehensive cancer network experience. J Clin Oncol: Off J Am Soc Clin Oncol. 2015;33(4):340–8. https://doi.org/10.1200/jco.2013.54.6119. NCCN risk of bone marrow neoplasm with breast cancer treatment.
Hesketh PJ, Batchelor D, Golant M, et al. Chemotherapy-induced alopecia: psychosocial impact and therapeutic approaches. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer. 2004;12(8):543–9. https://doi.org/10.1007/s00520-003-0562-5.
van den Hurk CJ, Mols F, Vingerhoets AJ, et al. Impact of alopecia and scalp cooling on the well-being of breast cancer patients. Psycho-Oncol. 2010;19(7):701–9. https://doi.org/10.1002/pon.1615.
Massey CS. A multicentre study to determine the efficacy and patient acceptability of the Paxman Scalp Cooler to prevent hair loss in patients receiving chemotherapy. European journal of oncology nursing: the official journal of European Oncology Nursing Society. 2004;8(2):121–30. https://doi.org/10.1016/j.ejon.2003.10.006.
Nangia J, Wang T, Osborne C, et al. Effect of a scalp cooling device on alopecia in women undergoing chemotherapy for breast cancer: the SCALP randomized clinical trial. JAMA. 2017;317(6):596–605. https://doi.org/10.1001/jama.2016.20939.
•• Early Breast Cancer Trialists’ Collaborative G. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomized trials [Meta-Analysis Research Support, Non-U.S. Gov’t]. Lancet (London, England). 2005;365(9472):1687–717. https://doi.org/10.1016/S0140-6736(05)66544-0. EBCTCG metaanayslis of chemotherapy in breast cancer 2005.
•• Early Breast Cancer Trialists’ Collaborative G, Peto R, Davies C, et al. Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomized trials. Lancet (London, England). 2012;379(9814):432–44. https://doi.org/10.1016/S0140-6736(11)61625-5. EBCTCG metaanayslis of chemotherapy in breast cancer 2012.
Fisher B, Glass A, Redmond C, et al. L-phenylalanine mustard (L-PAM) in the management of primary breast cancer. An update of earlier findings and a comparison with those utilizing L-PAM plus 5-fluorouracil (5-FU). Cancer. 1977;39(6 Suppl):2883–903.
Bonadonna G, Brusamolino E, Valagussa P, et al. Combination chemotherapy as an adjuvant treatment in operable breast cancer. N Engl J Med. 1976;294(8):405–10. https://doi.org/10.1056/NEJM197602192940801.
Fisher B, Redmond C, Wickerham DL, et al. Doxorubicin-containing regimens for the treatment of stage II breast cancer: the National Surgical Adjuvant Breast and Bowel Project experience. J Clin Oncol: Off J Am Soc Clin Oncol. 1989;7(5):572–82. https://doi.org/10.1200/JCO.1989.7.5.572.
Fisher B, Redmond C, Brown A, et al. Influence of tumor estrogen and progesterone receptor levels on the response to tamoxifen and chemotherapy in primary breast cancer. J Clin Oncol: Off J Am Soc Clin Oncol. 1983;1(4):227–41. https://doi.org/10.1200/JCO.1983.1.4.227.
Namer M, Fargeot P, Roche H, et al. Improved disease-free survival with epirubicin-based chemoendocrine adjuvant therapy compared with tamoxifen alone in one to three node-positive, estrogen-receptor-positive, postmenopausal breast cancer patients: results of French Adjuvant Study Group 02 and 07 trials. Ann Oncol. 2006;17(1):65–73. https://doi.org/10.1093/annonc/mdj022.
•• Bachegowda LS, Makower DF, Sparano JA. Taxanes: impact on breast cancer therapy. Anti-Cancer Drugs. 2014;25(5):512–21. https://doi.org/10.1097/cad.0000000000000090. Excellent review on role of taxanes in breast cancer treatment.
King KM, Lupichuk S, Baig L, et al. Optimal use of taxanes in metastatic breast cancer. Curr Oncol. 2009;16(3):8–20.
Jones S, Holmes FA, O’Shaughnessy J, et al. Docetaxel with cyclophosphamide is associated with an overall survival benefit compared with doxorubicin and cyclophosphamide: 7-year follow-up of US Oncology Research Trial 9735. J Clin Oncol: Off J Am Soc Clin Oncol. 2009;27(8):1177–83. https://doi.org/10.1200/JCO.2008.18.4028.
•• Blum JL, Flynn PJ, Yothers G, et al. Anthracyclines in early breast cancer: the ABC Trials-USOR 06-090, NSABP B-46-I/USOR 07132, and NSABP B-49 (NRG Oncology). Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2017;35(23):2647–55. https://doi.org/10.1200/JCO.2016.71.4147. ABC trials of antracycline-free vs taxane-antracycline regimens in early breast cancer.
Citron ML, Berry DA, Cirrincione C, et al. Randomized trial of dose-dense versus conventionally scheduled and sequential versus concurrent combination chemotherapy as postoperative adjuvant treatment of node-positive primary breast cancer: first report of Intergroup Trial C9741/Cancer and Leukemia Group B Trial 9741. J Clin Oncol: Off J Am Soc Clin Oncol. 2003;21(8):1431–9. https://doi.org/10.1200/JCO.2003.09.081.
Bonilla L, Ben-Aharon I, Vidal L, et al. Dose-dense chemotherapy in nonmetastatic breast cancer: a systematic review and meta-analysis of randomized controlled trials. J Natl Cancer Inst. 2010;102(24):1845–54. https://doi.org/10.1093/jnci/djq409.
Munro AF, Cameron DA, Bartlett JM. Targeting anthracyclines in early breast cancer: new candidate predictive biomarkers emerge. Oncogene. 2010;29(38):5231–40. https://doi.org/10.1038/onc.2010.286.
Allred DC, Clark GM, Tandon AK, et al. HER-2/neu in node-negative breast cancer: prognostic significance of overexpression influenced by the presence of in situ carcinoma. J Clin Oncol: Off J Am Soc Clin Oncol. 1992;10(4):599–605. https://doi.org/10.1200/JCO.1992.10.4.599.
Gusterson BA, Gelber RD, Goldhirsch A, et al. Prognostic importance of c-erbB-2 expression in breast cancer. International (Ludwig) Breast Cancer Study Group. J Clin Oncol: Off J Am Soc Clin Oncol. 1992;10(7):1049–56. https://doi.org/10.1200/JCO.1992.10.7.1049.
Wood WC, Budman DR, Korzun AH, et al. Dose and dose intensity of adjuvant chemotherapy for stage II, node-positive breast carcinoma. N Engl J Med. 1994;330(18):1253–9. https://doi.org/10.1056/NEJM199405053301801.
Muss HB, Thor AD, Berry DA, et al. c-erbB-2 expression and response to adjuvant therapy in women with node-positive early breast cancer. N Engl J Med. 1994;330(18):1260–6. https://doi.org/10.1056/NEJM199405053301802.
Slamon DJ, Leyland-Jones B, Shak S, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–92. https://doi.org/10.1056/NEJM200103153441101.
• Perez EA, Romond EH, Suman VJ, et al. Four-year follow-up of trastuzumab plus adjuvant chemotherapy for operable human epidermal growth factor receptor 2-positive breast cancer: joint analysis of data from NCCTG N9831 and NSABP B-31. J Clin Oncol: Off J Am Soc Clin Oncol. 2011;29(25):3366–73. https://doi.org/10.1200/JCO.2011.35.0868. Four-year follow up NSABP 31 N9831 trials of trastuzumab plus chemotherapy.
Sawyer DB, Zuppinger C, Miller TA, et al. Modulation of anthracycline-induced myofibrillar disarray in rat ventricular myocytes by neuregulin-1beta and anti-erbB2: potential mechanism for trastuzumab-induced cardiotoxicity. Circulation. 2002;105(13):1551–4.
•• Slamon D, Eiermann W, Robert N, et al. Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med. 2011;365(14):1273–83. https://doi.org/10.1056/NEJMoa0910383. BCIRG-006 trastuzumab vs non-trastuzumab regimen in early breast cancer.
Slamon D, Eiermann W, Robert NJ. Ten-year follow-up of BCIRG-006 comparing doxorubicin plus cyclophosphamide followed by docetaxel with doxorubicin plus cyclophosphamide followed by docetaxel and trastuzumab with docetaxel, carboplatin and trastuzumab in HER2-positive early breast cancer patients. 2015 San Antonio Bresat Cancer Symposium. 2015 Presented December 11, 2015;Abstract S5–04.
Burstein HJ, Piccart-Gebhart MJ, Perez EA, et al. Choosing the best trastuzumab-based adjuvant chemotherapy regimen: should we abandon anthracyclines? J Clin Oncol: Off J Am Soc Clin Oncol. 2012;30(18):2179–82. https://doi.org/10.1200/JCO.2012.42.0695.
Slamon D, Eiermann W, Robert N, et al. Abstract S5-04: Ten year follow-up of BCIRG-006 comparing doxorubicin plus cyclophosphamide followed by docetaxel (AC→T) with doxorubicin plus cyclophosphamide followed by docetaxel and trastuzumab (AC→TH) with docetaxel, carboplatin and trastuzumab (TCH) in HER2+ early breast cancer. Cancer Res. 2016;76(4 Supplement):S5-04-S5-04. https://doi.org/10.1158/1538-7445.Sabcs15-s5-04.
Pritchard KI, Shepherd LE, O’Malley FP, et al. HER2 and responsiveness of breast cancer to adjuvant chemotherapy. N Engl J Med. 2006;354(20):2103–11. https://doi.org/10.1056/NEJMoa054504.
Park K, Kim J, Lim S, et al. Topoisomerase II-alpha (topoII) and HER2 amplification in breast cancers and response to preoperative doxorubicin chemotherapy. Eur J Cancer. 2003;39(5):631–4.
Knoop AS, Knudsen H, Balslev E, et al. Retrospective analysis of topoisomerase IIa amplifications and deletions as predictive markers in primary breast cancer patients randomly assigned to cyclophosphamide, methotrexate, and fluorouracil or cyclophosphamide, epirubicin, and fluorouracil: Danish Breast Cancer Cooperative Group. J Clin Oncol: Off J Am Soc Clin Oncol. 2005;23(30):7483–90. https://doi.org/10.1200/JCO.2005.11.007.
Press MF, Sauter G, Buyse M, et al. Alteration of topoisomerase II-alpha gene in human breast cancer: association with responsiveness to anthracycline-based chemotherapy. J Clin Oncol: Off J Am Soc Clin Oncol. 2011;29(7):859–67. https://doi.org/10.1200/JCO.2009.27.5644.
Ejlertsen B, Mouridsen HT, Jensen MB, et al. Improved outcome from substituting methotrexate with epirubicin: results from a randomized comparison of CMF versus CEF in patients with primary breast cancer. European journal of cancer (Oxford, England: 1990). 2007;43(5):877–84. https://doi.org/10.1016/j.ejca.2007.01.009.
Di Leo A, Desmedt C, Bartlett JM, et al. HER2 and TOP2A as predictive markers for anthracycline-containing chemotherapy regimens as adjuvant treatment of breast cancer: a meta-analysis of individual patient data. Lancet Oncol. 2011;12(12):1134–42. https://doi.org/10.1016/S1470-2045(11)70231-5.
Bartlett JM, Munro AF, Dunn JA, et al. Predictive markers of anthracycline benefit: a prospectively planned analysis of the UK National Epirubicin Adjuvant Trial (NEAT/BR9601). Lancet Oncol. 2010;11(3):266–74. https://doi.org/10.1016/S1470-2045(10)70006-1.
Bartlett JM, McConkey CC, Munro AF, et al. Predicting anthracycline benefit: TOP2A and CEP17-not only but also. J Clin Oncol. 2015;33(15):1680–7. https://doi.org/10.1200/JCO.2013.54.7869.
Sparano JA, Gray RJ, Makower DF, et al. Prospective validation of a 21-gene expression assay in breast cancer. N Engl J Med. 2015;373(21):2005–14. https://doi.org/10.1056/NEJMoa1510764.
Cardoso F, van’t Veer LJ, Bogaerts J, et al. 70-gene signature as an aid to treatment decisions in early-stage breast cancer. N Engl J Med. 2016;375(8):717–29. https://doi.org/10.1056/NEJMoa1602253.
Acknowledgements
The manuscript development is supported by The Einstein Paul Calabresi Career Development Program (NIH 5K12CA132783-08) and NIH/National Center for Advancing Translational Science (NCATS) Einstein-Montefiore CTSA (Grant Number UL1TR001073).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Breast Cancer
Rights and permissions
About this article
Cite this article
Jasra, S., Anampa, J. Anthracycline Use for Early Stage Breast Cancer in the Modern Era: a Review. Curr. Treat. Options in Oncol. 19, 30 (2018). https://doi.org/10.1007/s11864-018-0547-8
Published:
DOI: https://doi.org/10.1007/s11864-018-0547-8