Abstract
Economic evaluations are increasingly being used by decision-makers to estimate the cost-effectiveness of interventions. The objective of this study was to conduct a structured review of economic evaluations of interventions to prevent and treat osteoporosis. Articles were identified independently by two reviewers through searches on MEDLINE, the bibliographies of reviews and identified economic models, and expert opinion, using predefined inclusion and exclusion criteria. Data on country, type and level of interventions, type of fractures, interventions, study population and the authors’ stated conclusions were extracted. Forty-two relevant studies were identified. The majority of studies (71%) were conducted in Sweden, the UK and the US. The main interventions investigated were hormone replacement therapy (27%), bisphosphonates (17%) and combinations of vitamin D and calcium (16%). In 38% of studies, hip fracture was the sole fracture outcome. Eighty-eight percent (88%) of studies investigated female populations only. A relatively large number of economic evaluations were identified in the field of osteoporosis. Major changes have recently occurred in the treatment of this disease, following the publication of the results of the Women’s Health Initiative trial. Methodological developments in economic evaluations, such as the use of probabilistic sensitivity analysis and cost-effectiveness acceptability curves, have also taken place. Such changes are reflected in the studies that were reviewed. The development of economic models should be an iterative process that incorporates new information, whether clinical or methodological, as it becomes available.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Economic evaluations are increasingly being used by decision-makers to evaluate the cost-effectiveness of treatments. In Australia and in the Canadian province of Ontario, economic evaluations are mandatory components of the pharmaceutical licensing process [1]. In the UK, the National Institute for Clinical Excellence (NICE) requires an economic evaluation as part of its submission procedures for the appraisal of new technologies (www.nice.org.uk). In the USA, the Academy for Managed Care Pharmacy (AMCP) has developed submission guidelines that require evidence of cost-effectiveness of new treatments for the inclusion on pharmacy formularies (www.amcp.org).
Economic evaluations can be conducted alongside clinical trials where economic data are collected at the same time as clinical data. Often, however, economic evaluations are conducted using models that explicitly combine available information in a formal framework. These models enable the combination of evidence from a variety of sources in order to explore scenarios that for different reasons have not been empirically tested. For example, results from studies with relatively short follow-up periods can be extrapolated to longer time periods that are more relevant to policy-makers. Economic models can also explore the long-term effectiveness and cost-effectiveness of treatments in populations at different risk.
A number of interventions are available to prevent and treat osteoporosis [2, 3]. However, recommendations for the treatment and prevention of osteoporosis have changed radically in the last few years. In 2002, the Women’s Health Initiative trial was stopped early because of the excess risk in cardiovascular events that were observed in women taking estrogen and progestin [4, 5]. The segment of the study investigating the effects of estrogen alone in women without a uterus was also stopped early due to the increase in observed strokes [6]. Following these results, treatment with hormone replacement therapy (HRT) for long-term prevention is no longer recommended. However, newer therapies such as bisphosphonates and raloxifene have been shown to be effective in clinical trials. Less expensive therapies with no known adverse side effects such as vitamin D with or without calcium supplements and hip protectors are also being investigated [7, 8, 9, 10].
A number of economic evaluations have been conducted in the field of osteoporosis and have investigated the cost-effectiveness of interventions in a variety of settings and study populations. A review of models by Zethreaus et al. published in this journal in 2002 described some of these models [11]. Because of the increase in cost-effectiveness studies, and the rapid changes in the use of treatments for osteoporosis, we conducted an updated structured review of economic evaluations of interventions relating to the prevention and treatment of osteoporosis.
Materials and methods
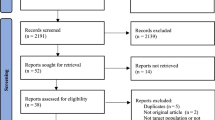
Two reviewers (RF and CI) conducted the search independently according to predefined inclusion and exclusion criteria. The inclusion criteria for the structured review were: economic evaluations of interventions to prevent or treat osteoporosis; economic evaluations could be modeling studies as well as economic evaluations of clinical study data; study populations could include elderly men as well as postmenopausal or elderly women; interventions included any treatment or device used to prevent or treat osteoporosis or osteoporotic fractures, with or without prior screening of bone mineral density (BMD); economic evaluation outcomes were cost per quality-adjusted life year (QALY) and cost per fracture avoided; the languages were English, French and Spanish (languages spoken by the reviewers).
The exclusion criteria for the structured review were: cost of illness and burden of disease studies; cost studies, such as retrospective claims analyses; editorials and reviews; any study describing a model, but not presenting results; economic evaluations of interventions to treat glucocorticoid-induced osteoporosis.
The search for papers was up to December 2004. Four broad search strategies were used to identify economic models of interventions to prevent and treat osteoporosis: a search on MEDLINE, a search of the bibliographies of relevant review articles, a search of the bibliographies of identified economic models of osteoporosis and a request for further references from expert opinion.
Both reviewers (CI and RF) conducted the search independently. The literature search on MEDLINE used combinations of the following Mesh terms: “Osteoporosis,” “Fractures,” “Economics,” “Cost-Benefit Analysis,” “Costs,” “Model” and “Models.” We also used the “Related Articles” function available in MEDLINE to identify any additional studies. Abstracts of papers from these searches were analyzed, and any potential study meeting the inclusion and exclusion criteria was obtained for further investigation. Bibliographies of review articles were analyzed to search for additional references [11, 12, 13, 14, 15, 16]. Bibliographies of identified economic models in osteoporosis were checked for any additional references that could have been missed from the other search strategies. At this stage, both reviewers compared their potential lists of studies to be included, and a single list was created. Any discrepancy was resolved through discussion between the reviewers. Finally, the third author (DT) reviewed our list to identify any potentially missing study.
Relevant information from each included study was extracted according to a predefined grid. Information included: study reference, country to which economic evaluation refers, type of fractures included, type of prevention or treatment (primary, secondary or treatment), interventions and control, study population and authors’ stated conclusions. Primary prevention is used for asymptomatic populations with no apparent osteoporosis or elevated risk of the condition to reduce their risk of onset in later life. Secondary prevention is used for asymptomatic patients who have been shown to have BMD sufficiently low to place them at elevated risk of fracture, to slow down the decline (or restore) BMD and hence reduce the risk of fracture. Treatment is used for patients known to have osteoporosis and who have already experienced one or more fractures to reduce their risk of further fractures [14].
Results
Forty-two (42) economic evaluations of interventions for the prevention or treatment of osteoporosis met the specified inclusion and exclusion criteria. A summary of the models by author, country, type of fracture, level of intervention (primary, secondary or treatment), intervention and control, study population and authors’ stated conclusions is presented in Table 1.
Twenty-nine percent (12) of the economic evaluations were set in the UK, 21% (9) were set in the USA and Sweden, respectively, 7% (3) were set in Canada, 5% (2) were set in Australia, Germany, and Spain, respectively, and 2% (1) were set in Italy, Japan, and Denmark, respectively. Three countries were associated with 71% of the economic evaluations, Sweden, the UK and the USA, reflecting the concern over the large burden of osteoporosis in these countries.
The main intervention investigated was HRT (in which we include Estrogen Replacement Therapy or ERT) with 27% (17) of studies investigating its cost-effectiveness. Bisphosphonates represented 17% (11) of the interventions, calcium and/or vitamin D 16% (10), calcitonin 9% (6), hypothetical interventions and hip protectors 8% (5) each, raloxifene 6% (4), and exercise, steroids and other, 3% (2) each. The numbers add to more than 42 as some studies investigate multiple therapies. It should be noted that seven of the HRT/ERT studies were conducted before 1994. In recent years, newer interventions such as bisphosphonates and raloxifene as well as cheaper interventions with no known side-effects such as vitamin D and calcium and hip protectors have been more readily investigated.
In 38% (16) of studies, hip fractures were the sole fracture outcome. Twenty-nine percent, 29% (12) investigated hip, wrist and vertebral fractures, 17% (7) hip, wrist, vertebral and other fractures (often proxied by shoulder fracture), 7% (3) analyzed hip and wrist fractures and 7% (3) vertebral fractures alone. Two percent 2% (1) investigated hip and vertebral fractures. Thirty-one percent (13) of the reviewed studies looked at primary intervention, 17% (7) at secondary intervention and 19% (8) investigated treatment. The remainder, 33% (14), analyzed various combinations of intervention levels. Finally 88% (37) of the studies investigated female populations. Only five studies included men in their analyses (although two of these studies questionably used general rates of fracture for both men and women).
Discussion
This structured review of economic evaluations for the prevention and treatment of osteoporosis identified 42 studies. The studies identified were published between 1980 and 2004 and span 24 years of research in the field of economic evaluation of interventions for the prevention and treatment of osteoporosis. Initially, the area was dominated by variations of a model developed in the USA, investigating the use of ERT and HRT in women with and without hysterectomy. Screening policies were also investigated to evaluate the cost-effectiveness of BMD measurements followed by HRT compared with universal HRT treatment [17, 18, 19, 20, 21, 22]. More recently, a model developed in Sweden has been employed a number of times to investigate various hypothetical interventions, at different costs, effectiveness and offset times [23, 24, 25]. Other models have been developed to investigate the cost-effectiveness of bisphosphonates and raloxifene following the results of clinical trials published in that area (FIT and MORE). Recently, a number of new models have also been published, investigating interventions such as vitamin D and calcium and hip protectors.
Despite the variety of interventions and populations considered, all but one of the reviewed studies employed cost-effectiveness models (one study provided an analysis based on economic data collected alongside clinical data [26]). The use of models is indicated in conditions such as osteoporosis because of the need to model long-term costs and effects that are not always available from trial or even observational data. In the absence of available data, decision-makers need formal frameworks on which to base their decisions, and such models can provide such as a basis when they are well conducted, transparent and explicit [27].
The quality of models in the field is variable [11, 14]. For example, some of the earlier studies made questionable use of cost-effectiveness decision rules [14]. However, the quality of the methodology and the reporting in publications is on average increasing, reflecting the availability of structured guidelines for developing and reporting cost-effectiveness models [28]. Most studies are explicit about the inputs and structure of the model. A number of models now include vertebral and wrist fractures as well as hip fractures. Some studies also include other fractures, sometimes proxied by shoulder fractures. Recently, much effort has been devoted to validating the models by providing explicit internal and external validity checks [29]. In addition, Zethreaus et al. have proposed making their model available to researchers in the field [11].
With the large number of assumptions that such models rely on, quantifying the uncertainty associated with the estimates is essential for the validity of the models. Although single and multi-way sensitivity analysis may be used to investigate the effect of different model parameters, only full probabilistic models allow the exploration of the interaction of different sources of uncertainty present within a model [28]. In these models, each input parameter is assigned an appropriate statistical distribution and a 95% confidence interval, representing a range of plausible values obtained from the literature. A Monte-Carlo simulation is then run to obtain a large number of iterations of the model. These results are used to obtain cost-effectiveness acceptability curves that show the probability that an intervention is cost-effective as a function of the decision-maker’s ceiling cost-effectiveness ratio (this ceiling will vary according to the resources available for health care and is in general unknown to the analyst). An increasing number of economic evaluations are using probabilistic sensitivity analyses and cost-effectiveness acceptability curves to investigate uncertainty in the model parameters and to present this to decision-makers (for example, [26, 30, 31, 32, 33, 34]).
Several specific trends were identified from the analysis of the studies included in the structured review: first, there is a major shift away from investigating the cost-effectiveness of HRT. While the reduction in fractures following HRT use has been established through trials [35], in earlier economic evaluations, a number of assumptions were made on the potential cardioprotective effect of HRT. Because of the high absolute risk of coronary heart disease (CHD), such assumptions had large impacts on the results. However, the results of the Women’s Health Initiative trial have radically challenged this approach [5, 6, 36]. With the current recommendations that HRT be used only for the short-term relief of menopausal symptoms, and the sharp drop in prescription and use of HRT [37], the long-term use of HRT for the prevention of fractures is no longer recommended [38]. Reflecting this major shift, no economic evaluations analyzing HRT have been published since 2002.
Second, the shift away from HRT has brought other therapies to the forefront. Bisphosphonates, such as alendronate, etidronate and risedronate, and raloxifene have been investigated following the results of large clinical trials [39, 40, 41, 42, 43]. Cheaper therapies with no side effects have also been investigated: vitamin D with or without calcium and hip protectors. These interventions have also been investigated in clinical trials, or are currently being investigated [7, 8, 9, 10].
Third, there has been a shift from investigating postmenopausal women only to also investigating the cost-effectiveness of treatments in elderly men. The interest in male osteoporosis has only recently been reflected in economic evaluations, as these all date from 2003 and 2004. It has been reported that actually one-third of hip fractures will occur in men [44]. Two studies investigated male and female populations [31, 45]. One study investigated alendronate in men only [30]. Two studies did not investigate men and women separately, although this may be problematic as hip fracture rates are different in both populations.
Finally, there has been a shift away from using BMD-based measures to predict the risk of fractures to using measures of fracture risk that are age dependent. It has been argued that they more accurately predict the risk of fracture than BMD-based measures [11, 29, 46].
There have been major developments in the treatment of osteoporosis in the last few years with the publication of the results of the Women’s Health Initiative on ERT and HRT, but also a number of clinical trials of other treatments for osteoporosis such as bisphosphonates, raloxifene, vitamin D and calcium and hip protectors. This shift of focus in treatments is reflected in the cost-effectiveness models that have been developed and subsequently published that have been described in this article. While a number of particular assumptions, such as the putative cardioprotective effect of HRT in these models may be obsolete, this does not make the models themselves obsolete. Methodological developments, such as the use of probabilistic sensitivity analysis and cost-effectiveness acceptability curves have also taken place. Such changes are reflected in the studies that were reviewed. If economic evaluations are to be useful decision-making tools, their development should follow an iterative process that incorporates new information, whether clinical or methodological, as it becomes available.
This structured review has provided an update and an extension to the review published by Zethreaus in 2002 [11]. It uses different inclusion and exclusion criteria from that study. For example, it does not include articles that described models without providing results [29, 47]. On the other hand, it includes studies that present cost per fracture as an outcome, while Zethreaus et al. did not. In this study, accepted methodologies for conducting systematic reviews were used. The search strategy was predefined, and data were extracted using pre-defined evidence tables. However, we did not provide a critical appraisal of the quality of theses economic evaluations, which would be necessary for it to qualify as a full systematic review. Future work should build on these initial results to provide a structured appraisal of the quality of the economic evaluations identified. Such work will provide researchers with additional information to build and develop future cost-effectiveness models that will provide economic and clinical evidence to decision-makers on treatment and prevention options for patients with osteoporosis.
References
Taylor RS, Drummond MF, Salkeld G, Sullivan SD (2004) Inclusion of cost effectiveness in licensing requirements of new drugs: the fourth hurdle. BMJ 329: 972–975
Fleurence RL, Iglesias CP, Torgerson DJ (2003) Cost-effectiveness of nutritional supplements for the treatment of osteoporosis. In: Bonjour JP, New S (eds) Nutritional aspects of bone health. Royal Society of Chemistry, London, pp 693–708
Fleurence RL, Iglesias CP, Torgerson DJ (2005) Economic aspects of osteoporosis treatment. In Cooper C, Lindsay R (eds) The prevention and treatment of osteoporosis in the high-risk patient. Martin Dunitz, London, pp 81–102
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, et al (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA 288:321–333
Wassertheil-Smoller S, Hendrix SL, Limacher M, Heiss G, et al (2003) Effect of estrogen plus progestin on stroke in postmenopausal women: the Women’s Health Initiative: a randomized trial. JAMA 289:2673–2684
Anderson GL, Limacher M, Assaf AR, Bassford T, et al (2004) Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA 291:1701–1712
Birks YF, Porthouse J, Addie C, Loughney K, et al (2004) Randomized controlled trial of hip protectors among women living in the community. Osteoporos Int 15:701–706
Trivedi DP, Doll R, Khaw KT (2003) Effect of four monthly oral vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community: randomised double blind controlled trial. BMJ 326:469
Porthouse J, Cockayne S, King C, Saxon L, et al (2005) Randomised controlled trial of calcium and supplementation with cholecalciferol (vitamin D3) for prevention of fractures in primary care. BMJ (in press)
The RECORD Trial Group (2005). Oral vitamin D3 and calcium for secondary prevention of low-trauma fractures in elderly people (Randomised Evaluation of Calcium Or vitamin D, RECORD): a randomised placebo-controlled trial. Lancet (in press)
Zethraeus N, Ben Sedrine W, Caulin F, Corcaud S, et al (2002) Models for assessing the cost-effectiveness of the treatment and prevention of osteoporosis. Osteoporos Int 13:841–857
Coyle D, Cranney A, Lee KM, Welch V, et al (2000) Cost-effectiveness research in osteoporosis. Drug Dev Res 49:135–140
Johannesson M, Jonsson B (1993) Economic evaluation of osteoporosis prevention. Health Policy 24:103–124
Sculpher M, Torgerson D, Goeree R, O’Brien BJ (1999) A critical structured review of economic evaluations of interventions for the prevention and treatment of osteoporosis. CHE Discussion Paper 169, University of York, York
Torgerson DJ, Reid DM (1997) The economics of osteoporosis and its prevention. A review. Pharmacoeconomics 11:126–138
Whittington R, Faulds D (1994) Hormone replacement therapy: II. A pharmacoeconomic appraisal of its role in the prevention of postmenopausal osteoporosis and ischaemic heart disease. Pharmacoeconomics 5:513–554
Cheung AP, Wren BG (1992) A cost-effectiveness analysis of hormone replacement therapy in the menopause. Med J Aust 156:312–316
Tosteson AN, Rosenthal DI, Melton III LJ, Weinstein MC (1990) Cost effectiveness of screening perimenopausal white women for osteoporosis: bone densitometry and hormone replacement therapy. Ann Intern Med 113:594–603
Tosteson AN, Weinstein MC (1991) Cost-effectiveness of hormone replacement therapy after the menopause. Bailliere’s Clin Obstetr Gynaecol 5:943–959
Weinstein MC (1980) Estrogen use in postmenopausal women—costs, risks, and benefits. N Engl J Med 303:308–316
Weinstein MC, Schiff I (1983) Cost-effectiveness of hormone replacement therapy in the menopause. Obstet Gynecol Surv 38:445–455
Weinstein MC, Tosteson AN (1990) Cost-effectiveness of hormone replacement. Ann N Y Acad Sci 592:162–172
Jonsson B, Kanis J, Dawson A, Oden A, et al (1999) Effect and offset of effect of treatments for hip fracture on health outcomes. Osteoporos Int 10:193–199
Kanis JA, Dawson A, Oden A, Johnell O, et al (2001) Cost-effectiveness of preventing hip fracture in the general female population. Osteoporos Int 12:356–361
Zethraeus N, Johannesson M, Jonsson B (1999) A computer model to analyze the cost-effectiveness of hormone replacement therapy. Int J Technol Assess Health Care 15:352–365
Fleurence RL, Torgerson DJ, Reid DM (2002) Cost-effectiveness of hormone replacement therapy for fracture prevention in young postmenopausal women: an economic analysis based on a prospective cohort study. Osteoporos Int 13:637–643
Buxton MJ, Drummond MF, Van Hout BA, Prince RL, et al (1997) Modelling in economic evaluation: an unavoidable fact of life. Health Econ 6:217–227
Sculpher M, Fenwick E, Claxton K (2000) Assessing quality in decision analytic cost-effectiveness models. A suggested framework and example of application. Pharmacoeconomics 17:461–477
Tosteson AN, Jonsson B, Grima DT, O’Brien BJ, et al (2001) Challenges for model-based economic evaluations of postmenopausal osteoporosis interventions. Osteoporos Int 12:849–857
Borgstrom F, Johnell O, Jonsson B, Zethraeus N, et al (2004) Cost effectiveness of alendronate for the treatment of male osteoporosis in Sweden. Bone 34:1064–1071
Fleurence RL (2004) The cost-effectiveness of fracture prevention treatments in the elderly. Int J Technol Assess Health Care 20:184–191
Iglesias CP, Torgerson DJ, Bearne A, Bose U (2002) The cost utility of bisphosphonate treatment in established osteoporosis. QJM 95:305–311
Kanis JA, Borgstrom F, Johnell O, Jonsson B (2004) Cost-effectiveness of risedronate for the treatment of osteoporosis and prevention of fractures in postmenopausal women. Osteoporos Int 15:862–871
Kanis JA, Borgstrom F, Johnell O, Oden A, Sykes D, Jonsson B (2005) Cost-effectiveness of raloxifene in the UK: an economic evaluation based on the MORE study. Osteoporos Int 16:15–25
Torgerson DJ, Bell-Syer SE (2001) Hormone replacement therapy and prevention of nonvertebral fractures: a meta-analysis of randomized trials. JAMA 285:2891–2897
Manson JE, Hsia J, Johnson KC, Rossouw JE, et al (2003) Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med 349:523–534
Majumdar SR, Almasi EA, Stafford RS (2004) Promotion and prescribing of hormone therapy after report of harm by the Women’s Health Initiative. JAMA 292:1983–1988
Grady D (2003) Postmenopausal hormones—therapy for symptoms only. N Engl J Med 348:1835–1837
Black DM, Cummings SR, Karpf DB, Cauley JA, et al (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348:1535–1541
Cummings SR, Eckert S, Krueger KA, Grady D, et al (1999) The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Multiple Outcomes of Raloxifene Evaluation. JAMA 281:2189–2197
Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, et al (1999) Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA 282:637–645
Levis S, Quandt SA, Thompson D, Scott J, et al (2002) Alendronate reduces the risk of multiple symptomatic fractures: results from the fracture intervention trial. J Am Geriatr Soc 50:409–415
Reginster J, Minne HW, Sorensen OH, Hooper M, et al (2000) Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int 11:83–91
Johnell O, Kanis J, Gullberg G (2001) Mortality, morbidity, and assessment of fracture risk in male osteoporosis. Calcif Tissue Int 69:182–184
Segui-Gomez M, Keuffel E, Frick KD (2002) Cost and effectiveness of hip protectors among the elderly. Int J Technol Assess Health Care 18:55–66
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1936
Stevenson MD, Oakley J, Chilcott JB (2004) Gaussian process modeling in conjunction with individual patient simulation modeling: a case study describing the calculation of cost-effectiveness ratios for the treatment of established osteoporosis. Med Decis Making 24:89–100
Ankjaer-Jensen A, Johnell O (1996) Prevention of osteoporosis: cost-effectiveness of different pharmaceutical treatments. Osteoporos Int 6:265–275
Armstrong K, Chen TM, Albert D, Randall TC, et al (2001) Cost-effectiveness of raloxifene and hormone replacement therapy in postmenopausal women: impact of breast cancer risk. Obstet Gynecol 98:996–1003
Brecht JG, Kruse HP, Felsenberg D, Mohrke W, et al (2003) Pharmacoeconomic analysis of osteoporosis treatment with risedronate. Int J Clin Pharmacol Res 23:93–105
Brecht JG, Kruse HP, Mohrke W, Oestreich A, et al (2004) Health-economic comparison of three recommended drugs for the treatment of osteoporosis. Int J Clin Pharmacol Res 24:1–10
Colon-Emeric CS, Datta SK, Matchar DB (2003) An economic analysis of external hip protector use in ambulatory nursing facility residents. Age Ageing 32:47–52
Coyle D, Cranney A, Lee KM (2001) Cost effectiveness of nasal calcitonin in postmenopausal women: use of Cochrane Collaboration methods for meta-analysis within economic evaluation. Pharmacoeconomics 19:565–575
Daly E, Roche M, Barlow D, Gray A, et al (1992) HRT: an analysis of benefits, risks and costs. Br Med Bull 48:368–400
Daly E, Vessey MP, Barlow D, Gray A, et al (1996) Hormone replacement therapy in a risk-benefit perspective. Maturitas 23:247–259
Francis RM, Anderson FH, Torgerson DJ (1995) A comparison of the effectiveness and cost of treatment for vertebral fractures in women. Br J Rheumatol 34:1167–1171
Garton MJ, Cooper C, Reid D (1997) Perimenopausal bone density screening—will it help prevent osteoporosis? Maturitas 26:35–43
Geelhoed E, Harris A, Prince R (1994) Cost-effectiveness analysis of hormone replacement therapy and lifestyle intervention for hip fracture. Aust J Public Health 18:153–160
Hart WM, Rubio-Terres C, Burrell A, Aristegui I, et al (2002) Pharmacoeconomic analysis of the treatment of postmenopausal osteoporosis with risedronate or alendronate. Revista Espanola de Enfermedades Metabolicas Oseas 11:97–104
Johnell O, Jonsson B, Jonsson L, Black D (2003) Cost effectiveness of alendronate (fosamax) for the treatment of osteoporosis and prevention of fractures. Pharmacoeconomics 21:305–314
Jonsson B (1998) Targeting high-risk populations. Osteoporos Int 8 [Suppl 1]:S13–S16
Jonsson B, Christiansen C, Johnell O, Hedbrandt J (1995) Cost-effectiveness of fracture prevention in established osteoporosis. Osteoporos Int 5:136–142
Kanis JA, Brazier JE, Stevenson M, Calvert NW, et al (2002) Treatment of established osteoporosis: a systematic review and cost-utility analysis. Health Technol Assess 6:1–146
Nagata-Kobayashi S, Shimbo T, Fukui T (2002) Cost-effectiveness analysis of screening for osteoporosis in postmenopausal Japanese women. J Bone Miner Metab 20:350–357
Rodriguez EC, Fidalgo Garcia ML, Rubio CS (1999) A cost-effectiveness analysis of alendronate compared to placebo in the prevention of hip fracture. Aten Primaria 24:390–396
Rosner AJ, Grima DT, Torrance GW, Bradley C, et al (1998) Cost effectiveness of multi-therapy treatment strategies in the prevention of vertebral fractures in postmenopausal women with osteoporosis. Pharmacoeconomics 14:559–573
Singh S, Sun H, Anis AH (2004) Cost-effectiveness of hip protectors in the prevention of osteoporosis related hip fractures in elderly nursing home residents. J Rheumatol 31:1607–1613
Torgerson D, Kanis JA (1995) Cost-effectiveness of preventing hip fractures in the elderly population using vitamin D and calcium. QJM 88:135–139
Torgerson D, Donaldson C, Reid D (1996) Using economics to prioritize research: a case study of randomized trials for the prevention of hip fractures due to osteoporosis. J Health Serv Res Policy 1:141–146
Visentin P, Ciravegna R, Fabris F (1997) Estimating the cost per avoided hip fracture by osteoporosis treatment in Italy. Maturitas 26:185–192
Waldegger L, Cranney A, Man-Son-Hing M, Coyle D (2003) Cost-effectiveness of hip protectors in institutional dwelling elderly. Osteoporos Int 14:243–250
Willis M, Odegaard K, Persson U, Mellstrom D, et al (2001) A cost-effectiveness model of tibolone as treatment for the prevention of osteoporosis fractures in postmenopausal women in Sweden. Clin Drug Invest 21:115–127
Willis M (2002) The health economics of calcium and vitamin D3 for the prevention of osteoporotic hip fractures in Sweden. Int J Technol Assess Health Care 18:791–807
Acknowledgements
We are grateful to Eli Lilly for their financial support for part of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fleurence, R.L., Iglesias, C.P. & Torgerson, D.J. Economic evaluations of interventions for the prevention and treatment of osteoporosis: a structured review of the literature. Osteoporos Int 17, 29–40 (2006). https://doi.org/10.1007/s00198-005-1943-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-005-1943-z



