Abstract
Purpose
The purpose of the study is to identify chronic condition clusters at pre- and post-cancer diagnosis, evaluate predictors of developing clusters post-cancer, and examine the impact on functional impairment among older cancer survivors.
Methods
We identified 5991 survivors age 65 and older of prostate, breast, colorectal, lung, bladder, kidney, head and neck, and gynecologic cancer and non-Hodgkin lymphoma from the Surveillance, Epidemiology and End Results-Medicare Health Outcomes Survey resource. Survivors completed surveys pre- and post-cancer diagnosis on 13 chronic conditions and functional status. Among those with ≥2 conditions, exploratory factor analysis identified clusters of conditions. Differences in cluster frequency from pre- to post-cancer diagnosis were evaluated across the top five cancer types using chi-square tests. Modified Poisson regression models estimated the relative risk of developing clusters post-diagnosis. Chi-square tests evaluated associations between function and clusters.
Results
Clusters included the following: cardiovascular disease cluster (pre 6.1 % and post 7.7 %), musculoskeletal cluster (28.2 % and 29.3 %), metabolic cluster (14.9 % and 17.6 %), and the major depressive disorder risk (MDDr) + gastrointestinal (GI) + pulmonary condition cluster (5.8 % and 8.7 %). Increases in MDDr + GI + Pulmonary cluster from pre- to post-cancer diagnosis were observed for prostate, lung, and colorectal cancer survivors. Functional impairment was more prevalent in survivors with defined clusters, especially in MDDr + GI + pulmonary, compared to survivors with ≥2 un-clustered conditions.
Conclusions
Distinct condition clusters of two or more chronic conditions are prevalent among older cancer survivors. Cluster prevalence increases from pre- to post-cancer diagnosis and these clusters have a significant impact on functional limitations.
Implications for Cancer Survivors
Tailored management on specific multimorbidity patterns will have implications for functional outcomes among older survivors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over half of cancer survivors 65+ years old have at least one chronic condition and almost one quarter have ≥4 conditions [1]. Multimorbidity, defined as the presence of more than one clinical condition of equal importance to a patient’s quality of life [2], increases the likelihood of mortality in older cancer patients [3]. Multimorbidity increases the complexity of clinical decision-making in cancer survivors [4–7].
Specific chronic conditions may cluster based on shared pathogenesis, such as cardiovascular disease and metabolic disorders [8]. Multimorbidity clusters may be different before and after a cancer diagnosis due to the impact of cancer and treatment, or may differ by cancer diagnosis [9]. Clusters may be associated with particular outcomes: for example, cardiorespiratory conditions may be associated with higher levels of pain and shortness of breath [10], while musculoskeletal conditions may have greater functional limitations; however, the previously used comorbidity index scores may mask this difference. The majority of evidence on chronic conditions in cancer survivorship has been demonstrated in the long-term survivors of childhood cancer [11–13]. There is limited evidence in the aging population on the occurrence of specific clusters, whether the clusters are different pre- and post-cancer diagnosis, and if specific clusters are associated with functional impairment.
Many older survivors suffer from multimorbidity in a health care system currently designed for treating single diseases, resulting in complicated long-term treatment recommendations, or situations where no recommendations exist [14, 15]. Our objective was to examine clusters pre- and post-cancer diagnosis and the association of these clusters with functional limitations in a population-based sample of older cancer patients. We hypothesized that multiple clusters would be observed before and after cancer diagnosis and that different clusters would have varying impacts on functional outcomes. The Surveillance, Epidemiology and End Results (SEER) national database of cancer registries linked with the Medicare Health Outcomes Survey (MHOS) provided a rich database to achieve our objective.
Methods
Data source
The SEER-MHOS data set includes cancer registry information linked with patient-reported surveys from a nationwide sample of individuals 65 years old or older who are enrolled in Medicare Advantage organizations [16]. MHOS collects survey data on comorbidities, symptoms, functional outcomes, and quality of life [17]. Currently, 14 annual survey cohorts from 1998 to 2013 are available for analysis. Individuals enrolled in participating Medicare Advantage organizations are randomly sampled by health plans, administered the survey by mail (>80 %) or telephone (∼20 %), and are then resurveyed 2 years later [16].
Of the 14 cohorts of data, we obtained data for nine of the most frequent cancer diagnoses (or diagnosis groups) in the USA, including breast, colorectal, prostate, lung, bladder, kidney, gynecologic, head and neck cancers, and non-Hodgkin lymphoma. We selected individuals who had completed a survey prior to a cancer diagnosis (median 12 months) and completed a survey post-cancer diagnosis (median 13 months). Of the 6233 with pre- and post-cancer surveys, we excluded 242 individuals diagnosed <65, leaving a final sample size of 5991.
Measures
Cancer, stage, and treatment
The SEER registry provides cancer type, stage at diagnosis, diagnosis date, and preliminary treatment information. We used the summary stage (2000) variable, derived from Collaborative Stage for 2004+ and Extent of Disease from 1998 to 2003 with the categories: in situ, localized, regional, distant, and unknown. Preliminary treatment information is reported in SEER on whether radiation or surgery were received.
Comorbidities
Comorbidities were measured via self-report from the question stem “has a doctor ever told that you had…” with response options of yes/no [7]. Comorbidities asked across all 14 cohorts of survey data were selected for this study. These included high blood pressure (HBP), angina/coronary artery disease (CAD), congestive heart failure (CHF), myocardial infarction (MI), other heart condition, stroke, diabetes, arthritis of the hip/knee, arthritis of the hand/wrist, sciatica, pulmonary conditions (emphysema, asthma, chronic obstructive pulmonary disease [COPD]), and gastrointestinal (GI) conditions (Crohn’s disease, ulcerative colitis, or inflammatory bowel disease). The algorithm for major depressive disorder risk (MDDr) includes two methods that can result in a positive screen for MDDr [18, 19]. The first method required a response of “yes” to “In the past year, have you had 2 weeks or more during which you felt, sad, blue, or depressed; or when you lost interest or pleasure in that you usually cared about or enjoyed?” The second method requires a response of “yes” to (1) feeling depressed or sad much of the time in the past 2 years and (2) having ≥2 years in life when feeling depressed or sad on most days, in addition to feeling downhearted/blue in the past 4 weeks at least “some of the time.” Either method classified a survivor as having MDDr.
Functional status (ADLs)
Functional limitations were assessed using an activity of daily living (ADL) index. The six items adapted from the Katz ADL [20] scale asked respondents how much difficulty they had doing six activities (no difficulty; a little difficulty; a lot of difficulty). A score of 6 indicates functional independence, 3–4 indicates moderate impairment, and ≤2 indicates significant impairment [20].
Demographic characteristics
The SEER registry links cases to the poverty level of the census tract where patients lived at the time of cancer diagnosis, thus providing a measure of poverty. Poverty levels were defined at 0–<5 % (includes those not in poverty), 5–<10 %, 10–<20 %, and 20–100 % below poverty. Race/ethnicity was derived using a variable that combined SEER-filled race information, CMS enrollment database, and self-reported race. Categories included non-Hispanic White, non-Hispanic Black, Asian or Pacific Islander, and other. Education was self-reported as <high school, high school graduate, some college, and college or higher.
Analysis
To identify clusters, we restricted the analysis to participants with ≥2 conditions and conducted an exploratory factor analysis (EFA) at pre- and post-cancer diagnosis. A tetrachoric correlation matrix was used to account for the dichotomous items [21] along with oblique (geomin) rotation with weighted least squares mean estimator. Factors were derived using the following criteria: eigenvalues (screen plot, eigenvalues >1), root mean square residual (<0.05), root mean square error of approximation (RMSEA; <0.06), and qualitatively assessing factors for conceptual relevance [22]. Items with a factor loading ≤0.20 were excluded from a factor. Priority was given to eigenvalues, RMSEA, and conceptual relevance. EFA procedures were conducted using MPlus version 7 [23].
The frequency of survivors in each cluster was determined by requiring that survivors report the majority of conditions within a cluster. For example, survivors needed to have ≥3 out of 5 conditions for a 5-condition cluster, ≥2 out of 3 conditions for a 3-condition cluster, or both conditions for a 2-condition cluster. An additional category of multiple conditions was created to account for survivors who had ≥2 conditions but did not meet any defined cluster criteria. Survivors could potentially have multiple clusters.
Cluster frequencies and chi-square tests were used to evaluate pre- and post-cancer diagnoses in the overall sample and for the five most prevalent cancer types: prostate (29.1 %), breast (22.5 %), colorectal cancer (15.1 %), genitourinary (10.7 %), and lung (9.9 %). Among those survivors without pre-cancer diagnosis clusters, we estimated the relative risk (RR) and 95 % confidence intervals (CIs) of developing specific clusters after cancer diagnosis using modified Poisson regression models adjusted for demographic and clinical characteristics. Finally, we used chi-square tests to examine the presence of functional limitations across clusters at pre- and post-cancer diagnosis.
Results
Study population
The average age at cancer diagnosis was 75 years (range 65–103). The mean age at pre-cancer and post-cancer survey completion was 74 and 77.7 years, respectively (Table 1). The majority of survivors were non-Hispanic White (79 %). Approximately 67 and 70 % of survivors reported ≥2 comorbidities before and after cancer diagnosis, respectively. Supplementary Table 1 provides frequencies of individual comorbidity.
EFA results
The EFA yielded four clusters at both pre-diagnosis and post-diagnosis. The full factor loadings and factor structure are shown in Supplementary Tables 2 and 3. The factor structure indicates that CVD cluster was comprised of MI, angina, CHF, other heart conditions, and stroke. The musculoskeletal cluster was comprised of arthritis of hip/knee, arthritis of hand/wrist, and sciatica. The metabolic cluster was comprised of diabetes and HBP. Finally, MDDr, pulmonary, and GI conditions (MDDr + GI + pulmonary) clustered together. In the pre-cancer diagnosis survey, the four-cluster model demonstrated satisfactory fit with CFI/TLI = 0.98/0.95 and RMSEA = 0.026. The same structure emerged for post-cancer diagnosis EFA (CFI/TLI = 0.98/0.95, RMSEA = 0.027).
Cluster frequency
Overall, 41.7 % of the patients reported one or more clusters prior to cancer diagnosis; the proportion of patients with one or more clusters increased to 46.2 % after cancer diagnosis. Table 2 shows that, overall, the musculoskeletal cluster was most frequently reported (28 and 29 % of cancer survivors at pre- and post-diagnosis, respectively), followed by metabolic (15 and 17 %, respectively), CVD (6.1 and 7.6 %, respectively), and MDDr + GI + pulmonary (5.8 and 8.7 %, respectively). Un-clustered conditions were observed in 25 % cancer survivors prior to cancer diagnosis and 26 % cancer survivors after cancer diagnosis. The proportion of prostate cancer survivors reporting musculoskeletal conditions was significantly higher after cancer diagnosis when compared to before (25.7 vs. 21.6 %, p = 0.0139). The proportion of breast and lung cancer survivors reporting metabolic conditions was significantly higher after cancer diagnosis (19.2 vs. 15.5 %, p = 0.032, and 16.9 vs. 11.8 %, p = 0.042). Finally, the proportion of cancer survivors reporting MDDr + GI + pulmonary cluster was significantly higher after the respective cancer diagnoses, when compared to before for prostate (3.2 vs. 5.9 %, p = 0.0005), colorectal cancer (5.2 vs. 8.1 %, p = 0.037), and lung cancer survivors (13.2 vs. 21.6 %, p = 0.0006).
Factors associated with post-cancer diagnosis cluster development
Entire cohort
Overall, 2.7, 1.6, and 2.9 % of survivors reported the development of new metabolic, CVD, and MDDr + GI + pulmonary cluster after cancer diagnosis, respectively. Factors associated with all three new clusters included increasing age (RR = 1.02–1.07) and less than a high school education (RR = 1.31–1.50; results shown in Supplementary Table 4). Minority survivors were at increased risk for developing the metabolic cluster (RR = 1.31, 95 % CI 1.28, 2.02) but at decreased risk for developing the MDDr + GI + pulmonary cluster (RR = 0.57, 95 % CI 0.45, 0.71).
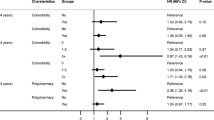
Prostate cancer
Approximately 4 % reported new development of the musculoskeletal cluster and 2.5 % reported the MDDr + GI + pulmonary cluster after prostate cancer diagnosis. Table 3 shows age was associated with new musculoskeletal cluster development (RR = 1.08, 95 % CI 1.06, 1.10). Factors associated with new MDDr + GI + pulmonary cluster included age, less than high school education, and >5 % below poverty level.
Colorectal cancer
There was a 2.9 % increase in the proportion of survivors reporting MDDr + GI + pulmonary cluster after colorectal cancer diagnosis. No sociodemographic or clinical characteristics included in the model were associated with increased risk.
Breast cancer
Approximately 5 % of survivors reported development of new metabolic cluster after diagnosis. Minorities were at significantly increased risk of developing new metabolic cluster (RR = 1.74, 95 % CI 1.09, 2.79).
Lung cancer
A total of 5.1 and 8.4 % of survivors reported development of new metabolic and MMDr + GI + pulmonary cluster. No sociodemographic or clinical characteristics included in the model were associated with increased risk.
Functional impairment frequency
The frequency of reporting at least moderate functional impairment was highest among the MDDr + GI + pulmonary condition cluster across cancer types with the exception of breast cancer, where the CVD cluster had the most functional impairment (Table 4). Other than survivors with ≤1 conditions, those with “un-clustered” conditions reported lowest functional impairment. Over half of the survivors with ≥2 clusters (52 %) and MDDr + GI + pulmonary condition cluster (56 %) met the criteria for functional impairment at pre-diagnosis.
Discussion
Over two thirds of older cancer survivors within this sample of Medicare Advantage beneficiaries reported ≥2 comorbidities pre- and post-cancer diagnosis. This study identified the co-occurrence of specific conditions both before and after cancer diagnosis. We identified several condition clusters, including a CVD cluster, musculoskeletal cluster, metabolic dyad, and a cluster of MDDr + GI + pulmonary conditions. Increases in cluster frequency from pre- to post-cancer diagnosis differed across cancer types. Survivors within clustered conditions had significantly higher frequency of functional impairment compared to those with “un-clustered” multimorbidity or with ≤1 condition.
The clusters identified through our data were generally consistent with our hypotheses and with clusters reported in other studies conducted among similarly aged non-cancer population [24]. Cardiovascular, metabolic, and musculoskeletal condition clusters are among the primary groups that have previously been identified in other studies. Our EFA found that diabetes and HBP exist as an independent dyad [25]; this differs from several studies reporting that these conditions clustered with other CVD diseases in the general population [26]. Our study also identified a fourth cluster that was comprised of three seemingly unrelated disease combinations: GI, pulmonary conditions, and MDDr. This may follow the trend of the “mental health problems cluster” summarized by Prado-Torres and colleagues in their systematic review [24]. For example, several studies in the review reported that conditions such as anxiety, asthma/COPD, depression, and intestinal diverticulitis, among others, were all within a single cluster [27, 28]. Survivors with one or both of these conditions may have an increased depression risk, thus creating this “heterogeneous” cluster in terms of pathophysiologic relationship.
As might be expected for colorectal and lung cancer survivors, MDDr + GI + pulmonary conditions increased from pre- to post-diagnosis. However, MDDr + GI + pulmonary conditions also increased for prostate cancer survivors. Consistent with reports of high risk of metabolic syndrome in breast cancer survivors [29], we found a significant 4 % increase in frequency of having both diabetes and HBP. Given that the surveys were delivered in relatively close timing (on average within 2 years), cluster increases may not necessarily be attributable to aging. Further study on clinical and biological factors that contribute to the increase of multimorbidity, especially clusters, is needed.
Multimorbidity among the older population has multiple health-status implications, especially in functional outcomes. Interestingly, those with ≥2 clusters did not have the highest functional impairment frequency. The high frequency of limitations within the MDDr + GI + pulmonary cluster is suggestive of the impact of these condition combinations in older survivors. Given that multimorbid adults report that maintaining independence, and thus their functional capabilities, ranks number one on their priority list, followed by pain/symptom relief, and then survival, identifying high-risk clusters for pre-emptive functional assessments and intervention may provide a targeted approach to preventing further decline [30].
However, despite the association between chronic health condition clusters and functional limitation, almost all of the limited number of interventions for multimorbid patients are designed for primary care or community settings for the general population of older adults and not cancer survivors [31]. Tailoring or developing interventions for an older cancer-specific population with multimorbidity must include integration of available evidence on the interaction between cancer, its treatments, and other conditions; how conditions may contribute to polypharmacy; the effect on survival estimates; and how this information affects patient preferences for care [2]. Our study suggests considerations of multimorbidity should include not only which conditions are present or how many but also in which combinations they occur.
Findings are subject to several limitations. First, the MHOS is not a cancer-specific instrument and thus does not include certain symptoms or conditions that are relevant for cancer patients (e.g., fatigue). Second, there are inherent limitations to “defining” whether a survivor does or does not qualify as having a cluster of conditions. Requiring that survivors have the majority, or both, of the conditions is the first step to examining a highly complex problem. Validation of the clusters in another cancer sample will also be required. Third, the data do not include Medicare Fee-for-Service beneficiaries who account for most of the Medicare population [16] and tend to report lower quality of life [32]. Fourth, the treatment data are limited to the first course of therapy data (surgery, radiation) from SEER and chemotherapy data is not reliable. Finally, we did not have data from a non-cancer population; therefore, we were unable to compare cancer vs. non-cancer. However, given that one in three individuals >65 years old will be diagnosed with cancer, a “within-cancer” population comparison holds significant value.
Multimorbidity clusters were prevalent within the vulnerable older cancer survivor population. Functional impairment was substantial across clusters and imposed an additional burden compared to having ≥2 conditions that were un-clustered. As survivors advance further from diagnosis, treating and/or managing multiple chronic conditions will be critical to maintain functional status and quality of life [33]. Multidisciplinary approaches, including oncologists, geriatricians, social workers, pharmacists, and physical therapists, among others, will be required to provide optimal comprehensive care for older cancer survivors living with multimorbidity [2].
References
Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162:2269–76.
Thompson K, Dale W How do I best manage the care of older cancer patients with multimorbidity? J Geriatr Oncol 2015.
Sogaard M, Thomsen RW, Bossen KS, Sorensen HT, Norgaard M. The impact of comorbidity on cancer survival: a review. J Clin Epidemiol. 2013;5:3–29.
Geraci JM, Escalante CP, Freeman JL, Goodwin JS. Comorbid disease and cancer: the need for more relevant conceptual models in health services research. J Clin Oncol. 2005;23:7399–404.
Ritchie CS, Kvale E, Fisch MJ. Multimorbidity: an issue of growing importance for oncologists. J Oncol Pract. 2011;7:371–4.
Hays RD, Reeve BB, Smith AW, Clauser SB. Associations of cancer and other chronic medical conditions with SF-6D preference-based scores in Medicare beneficiaries. Qual Life Res. 2014;23:385–91.
Smith AW, Reeve BB, Bellizzi KM, Harlan LC, Klabunde CN, Amsellem M, et al. Cancer, comorbidities, and health-related quality of life of older adults. Health Care Financ Rev. 2008;29:41–56.
Levitzky YS, Pencina MJ, D’Agostino RB, Meigs JB, Murabito JM, Vasan RS, et al. Impact of impaired fasting glucose on cardiovascular disease: the Framingham Heart Study. J Am Coll Cardiol. 2008;51:264–70.
Vigneri P, Frasca F, Sciacca L, Pandini G, Vigneri R. Diabetes and cancer. Endocr-Relat Cancer. 2009;16:1103–23.
Bekelman DB, Havranek EP, Becker DM, Kutner JS, Peterson PN, Wittstein IS, et al. Symptoms, depression, and quality of life in patients with heart failure. J Card Fail. 2007;13:643–8.
Phillips SM, Padgett LS, Leisenring WM, Stratton KK, Bishop K, Krull KR, et al. Survivors of childhood cancer in the United States: prevalence and burden of morbidity. Cancer Epidemiol Biomarkers Prev. 2015;24:653–63.
Bhatia S. Long-term complications of therapeutic exposures in childhood: lessons learned from childhood cancer survivors. Pediatrics. 2012;130:1141–3.
Bhatia S. Long-term health impacts of hematopoietic stem cell transplantation inform recommendations for follow-up. Expert Rev Hematol. 2011;4:437–52. quiz 453–4.
Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294:716–24.
Institute of Medicine Delivering high-quality cancer care. Charting a new course for a system in crisis. Washington, DC: National Academies Press; 2013.
Ambs A, Warren JL, Bellizzi KM, Topor M, Haffer SC, Clauser SB. Overview of the SEER—Medicare Health Outcomes Survey linked dataset. Health Care Financ Rev. 2008;29:5–21.
Haffer SC, Bowen SE. Measuring and improving health outcomes in Medicare: the Medicare HOS program. Health Care Financ Rev. 2004;25:1–3.
Rost K, Burnam MA, Smith GR. Development of screeners for depressive disorders and substance disorder history. Med Care. 1993;31:189–200.
White AJ, Reeve BB, Chen RC, Stover AM, Irwin DE. Coexistence of urinary incontinence and major depressive disorder with health-related quality of life in older Americans with and without cancer. J Cancer Surviv. 2014;8:497–507.
Katz S, Down TD, Cash HR, Grotz RC. Progress in the development of the index of ADL. The Gerontologist. 1970;10:20–30.
Kubinger K. On artificial results due to using factor analysis for dichotomous variables. Psychol Sci. 2003;45:106–10.
Fayers PM, Machin D Chapter 6: Factor analysis and structural equation modeling. In: Quality of Life: the assessment, analysis, and interpretation of patient-reported outcomes. Chichester; Hoboken, NJ: John Wiley & Sons, 2007, p. 131–160.
Muthen B, Muthen LK Mplus Version 7.1. 2012; 7.
Prados-Torres A, Calderon-Larranaga A, Hancco-Saavedra J, Poblador-Plou B, van den Akker M. Multimorbidity patterns: a systematic review. J Clin Epidemiol. 2014;67:254–66.
van den Bussche H, Koller D, Kolonko T, Hansen H, Wegscheider K, Glaeske G, et al. Which chronic diseases and disease combinations are specific to multimorbidity in the elderly? Results of a claims data based cross-sectional study in Germany. BMC Public Health 2011; 11:101-2458-11-101.
Kirchberger I, Meisinger C, Heier M, Zimmermann AK, Thorand B, Autenrieth CS, et al. Patterns of multimorbidity in the aged population results from the KORA-Age study. PLoS One. 2012;7, e30556.
Schafer I. Does multimorbidity influence the occurrence rates of chronic conditions? A claims data based comparison of expected and observed prevalence rates. PLoS One. 2012;7:e45390.
Prados-Torres A, Poblador-Plou B, Calderon-Larranaga A, Gimeno-Feliu LA, Gonzalez-Rubio F, Poncel-Falco A, et al. Multimorbidity patterns in primary care: interactions among chronic diseases using factor analysis. PLoS One. 2012;7, e32190.
Buttros Dde A, Nahas EA, Vespoli Hde L, Uemura G, de Almeida BR, Nahas-Neto J. Risk of metabolic syndrome in postmenopausal breast cancer survivors. Menopause. 2013;20:448–54.
Fried TR, Tinetti ME, Iannone L, O’Leary JR, Towle V, Van Ness PH HEalth outcome prioritization as a tool for decision making among older persons with multiple chronic conditions. Arch Intern Med 2011; 171:1856–1858.
Smith SM, Soubhi H, Fortin M, Hudon C, O’Dowd T. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2012;4, CD006560.
Riley G. Two-year changes in health and functional status among elderly Medicare beneficiaries in HMOs and Fee-for-Service. Health Serv Res. 2000;35:44–59.
Watson LC, Amick HR, Gaynes BN, Brownley KA, Thaker S, Viswanathan M, et al. Practice-based interventions addressing concomitant depression and chronic medical conditions in the primary care setting: a systematic review and meta-analysis. J Prim Care Commun Health. 2013;4:294–306.
Acknowledgments
KMK was supported by grants T32HS013852 and K12HS023009 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or AHRQ.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 31 kb)
Rights and permissions
About this article
Cite this article
Kenzik, K.M., Kent, E.E., Martin, M.Y. et al. Chronic condition clusters and functional impairment in older cancer survivors: a population-based study. J Cancer Surviv 10, 1096–1103 (2016). https://doi.org/10.1007/s11764-016-0553-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-016-0553-4