Abstract
Purpose
Anthracyclines are an integral component of breast cancer chemotherapy. They exert many cardiotoxic effects, including heart failure. The onset of anthracycline-induced heart failure (AIHF) can occur years after completion of chemotherapy and incurs significant morbidity and mortality. Few studies have attempted to characterize risk factors for its development. Our purpose was to determine the incidence of early and late AIHF in breast cancer survivors and to identify factors that increase the risk for late-onset AIHF.
Methods
Patients with invasive breast cancer who received doxorubicin-containing chemotherapy at University Hospitals Case Medical Center from 1998 to 2006 were included. Medical history and tumor and treatment characteristics were abstracted from medical records. Patients who developed heart failure were compared to those who did not and were also stratified based on timing of heart failure.
Results
One thousand one hundred fifty-three patients received doxorubicin-based chemotherapy for invasive breast cancer with an average follow-up of 7.6 years (standard deviation (SD) = 3.4). The overall incidence of heart failure was 10.4, with a 2.9 and 7.6 % incidence of early- and late-onset heart failure, respectively. Human epidermal growth factor receptor 2 (HER2) status, hypertension, and coronary artery disease were significant predictors for both heart failure groups (p < 0.001). Type II diabetes was a risk factor for the late-onset AIHF group (p < 0.001).
Conclusions
HER2 status and cardiovascular risk factors increased the risk of heart failure among doxorubicin users. Patients with type II diabetes were at increased risk of late-onset AIHF.
Implications for cancer survivors
We identified at risk survivors who may benefit from prolonged monitoring and/or early intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anthracyclines have been shown to improve survival and decrease mortality in breast cancer [1–3]. However, anthracycline-induced cardiomyopathy is a well-documented and often therapy-limiting toxicity [4, 5]. Anthracycline cardiotoxicity can occur at three different time periods: during administration of the drug (acute), within 1 year after therapy (early-onset), or more than 1 year after exposure (late-onset) [6, 7]. While acute and early-onset anthracycline cardiotoxicity manifesting as transient arrhythmias or asymptomatic decreases in ejection fraction usually resolve, late-onset anthracycline cardiotoxicity can progress to symptomatic and persistent heart failure [8]. Breast cancer patients who develop anthracycline-induced heart failure (AIHF) carry a poor prognosis as it is lethal 27 to 60 % of the time [9].
Late-onset AIHF is well-documented in the pediatric cancer survivor population [10]. Pediatric cancer survivors who received an anthracycline-containing treatment are 15 times more likely to develop heart failure compared to matched counterparts [11]. Population studies using SEER data also show that late-onset AIHF does occur in the adult breast cancer survivor population [12, 13], with the risk increasing significantly 5 years after completion of treatment [13]. The incidence of late-onset AIHF in the breast cancer varies greatly depending on how AIHF was assessed, with studies reporting between 1.6 and 5 % [4] and as high as 30 % [14].
Very few studies have been done looking specifically at risk factors for late-onset AIHF especially in the breast cancer survivor population [15], though late-onset anthracycline cardiotoxicity is well-documented in this group [16]. However, there are a number of patient and treatment characteristics that have been shown to increase the risk of developing anthracycline cardiotoxicity overall. Not surprisingly, comorbidities such as hypertension, diabetes mellitus, and dyslipidemia as well as patient age, which are known risk factors for heart disease, also increase the risk for anthracycline cardiotoxicity [12, 17]. Treatment characteristics such as concurrent left chest wall radiation therapy and total anthracycline dose have also been shown to be risk factors [18, 19]. The incidence of anthracycline cardiotoxicity rises with cumulative anthracycline dose [20] with incidences of 5 % at a cumulative dose of 400 mg/m2, 16 % at 500 mg/m2, 26 % at 550 mg/m2, and 48 % at 700 mg/m2. Cardiac enzymes such as troponin I and BNP have been found to be persistently elevated years after completion of anthracycline therapy, demonstrating its lasting cardiotoxic effects [21–23].
Diagnosis of AIHF is currently based on a decrease in left ventricular ejection fraction (LVEF) during and after anthracycline therapy, as measured by either echocardiogram or multi-gated acquisition scan (MUGA). However, studies show that acute decrease in LVEF does not necessarily predict late-onset AIHF [19, 23] and that patients who do not initially demonstrate any LVEF changes may develop AIHF years after completion of treatment [24]. Furthermore, as trastuzumab has become a part of standard adjuvant treatment for human epidermal growth factor receptor 2 (HER2)-positive breast cancers, studies have demonstrated an increased risk of heart failure with addition of trastuzumab to anthracyclines [25].
Currently, there are no standard guidelines for the monitoring and evaluation of AIHF in adult breast cancer survivors [16]. Patients typically undergo evaluation of heart function with an echocardiogram or MUGA before starting chemotherapy to determine eligibility for treatment with anthracyclines. Most patients are not again routinely evaluated unless they present with symptoms suggestive of heart failure. There is increasing thought that cardiac risks in breast cancer patients who have received anthracycline-based chemotherapy are not being adequately assessed [26, 27]. More importantly, while much research has been published regarding risk factors for, diagnosis of, possible prevention, and treatment of anthracycline cardiotoxicity, few studies have focused specifically on late-onset AIHF in breast cancer survivors. Even fewer of these studies have attempted to differentiate what, if any, characteristics separate acute/early anthracycline cardiotoxicity from late-onset AIHF. With an estimated 2.5 million breast cancer survivors [28] and an 89.2 % 5-year survival rate [29], it is likely that a significant number of breast cancer patients will experience heart failure in their lifetime due to exposure to anthracycline-containing chemotherapy. The objectives of this retrospective study are to calculate the incidence of anthracycline-induced heart failure and to assess the impact of various risk factors on the development of late-onset AIHF. We hope to identify an at risk patient population that would benefit from long-term follow-up or alternative cancer treatment strategies.
Materials and methods
Study design
This retrospective study was conducted at University Hospitals Case Medical Center (UHCMC) with IRB approval. We initially sought all patients in our institution’s tumor registry who received chemotherapy for invasive breast cancer between 1998 and 2006, including only those who received anthracyclines in this study. Patient comorbidities and dates of diagnoses were identified via linking with International Classification of Diseases (ICD)-9 billing codes for each patient encounter. Medical records were used to gather additional information and to confirm billing diagnoses. A random study number was then assigned to each patient to protect personal health information.
Data collection
The first author abstracted the data for all patients in this study. For each patient, the following information was collected from the tumor registry: histopathology, cancer laterality, chemotherapy start date, radiation start date, chemotherapy regimen (if anthracycline-containing regimen then type and cumulative dose), age at diagnosis, tobacco history (former, current, never), staging, hormone receptor status, HER2 status, and mortality status (deceased/alive) at the time of query. From the billing codes, the following information was obtained: diagnoses of type II diabetes mellitus, coronary artery disease, hypertension, dyslipidemia, and heart failure (if yes, date of diagnosis). From the medical record, the following data was obtained: cardiac imaging data (MUGA or echocardiogram) and date of last follow-up visit (inpatient, outpatient, or date of death). The medical record was also used to confirm heart failure diagnoses, comorbidities, and mortality. Cause of death usually could not be determined from the medical record. The anthracycline dose was calculated based on the standard for each regimen, e.g., 240 mg/m2 of doxorubicin in “ACx4,” unless otherwise stated by oncology notes in the medical record.
All patient records were queried for ICD-9 codes for heart failure (see Supplementary Table 1). These codes have been validated in a prior study identifying patients with heart failure [30]. The medical records of these patients were then used to validate the diagnosis of heart failure. In those patients, heart failure was defined as sonographic evaluation of LVEF ≤45 % combined with recorded clinical assessment of signs and symptoms, which has been used in a prior study assessing for AIHF [31]. Patients with heart failure were coded as having either early-onset heart failure or late-onset heart failure. Early-onset AIHF was defined as diagnosis of heart failure within 1 year of initiation of chemotherapy, and late-onset AIHF was defined as occurring more than a year after chemotherapy. Patients were then classified into the early heart failure, late heart failure, or control group (patients that received anthracycline-based chemotherapy that did not develop any heart failure). Length of follow-up was defined as time between initial date of cancer diagnosis and date of last follow-up visit (inpatient, outpatient, or date of death). Time to onset of heart failure was defined as the time between initial date of cancer diagnosis and the date of heart failure diagnosis.
Statistical analysis
Early or late heart failure patients were compared to the control (no heart failure) group and then to each other using either a chi-square test (for categorical variables) or a standard t test (for continuous variables). All statistics were done using SAS 9.3 and a p value < 0.05 was considered statistically significant.
Results
One thousand six hundred twenty-two breast cancer patients were considered for systemic chemotherapy between 1998 and 2006 at our institution. Of those not lost to follow-up, 1,169 received an anthracycline-containing regimen and were included for further study. One hundred twenty patients developed heart failure after receiving chemotherapy; 34 were classified as early-onset while 86 were classified as late-onset. Of the 1,049 patients who did not develop heart failure, the anthracycline doses was unknown in 16 patients and were excluded, leaving 1,033 patients in the control group (Fig. 1). Doxorubicin was the only anthracycline that any of these patients received. The most common regimen was four cycles of doxorubicin and cyclophosphamide for a cumulative doxorubicin dose of 240 mg/m2. Table 1 provides a summary of the population characteristics of these patients.
The overall incidence of heart failure after doxorubicin at our institution was 10.4 %, with the incidence of early-onset AIHF being 2.9 % and late-onset AIHF being 7.6 %. The average time to onset of heart failure in the early group was 0.57 years (standard deviation (SD) = 0.2) compared to 5.16 years (SD = 3.2) in the late-onset group. The average length of follow-up was 7.6 years (SD = 3.5) in the control group and 7.7 years (SD = 3.3) in the heart failure group. Table 2 summarizes the key patient, cancer, and treatment characteristics that were examined in this study. The early- and late-onset AIHF groups were compared to the control group and then to each other.
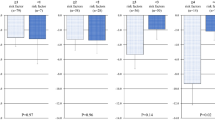
Risk factors for early- or late-onset AIHF
The early- and late-onset AIHF groups were first individually compared to the control group. Patients who developed early-onset AIHF were significantly older than those in the control group (p = 0.01). Such a difference did not exist between the late-onset group and control group. The only disease characteristic that was statistically significantly different from the control group in both early and late heart failure groups was HER2 status. Similar to the results of other studies looking at heart failure in patients who received anthracyclines, patient comorbidities such as coronary artery disease, hypertension, and dyslipidemia were all significant risk factors (p < 0.01) for heart failure in both the early- and late-onset AIHF groups. The use of trastuzumab was significantly higher in both heart failure groups compared to the control. Type II diabetes was only a significant risk factor in the late-onset AIHF group (p < 0.001) but not the early-onset AIHF group (p = 0.45). Current and former smoking status, a known cardiovascular risk factor, was not significant (p > 0.05) across all groups. Contrary to what other studies have shown, left-sided radiation was not a significant risk factor in either group. Early-onset AIHF was not significantly associated with increased mortality compared to the control group (29.4 versus 20.6 %, p > 0.05), whereas late-onset AIHF did confer a significant mortality risk (38.4 versus 20.6 %, p < 0.001, see Table 1).
Early-onset AIHF versus late-onset AIHF
The early-onset group was then compared to the late-onset group. The patients were not significantly different in age at diagnosis. There was also no difference in the tumor characteristics between the two groups. While HER2 status did not differ between the two groups, there were significantly more patients in the early-onset group who received trastuzumab compared to the late-onset group (38.2 versus 19.8 %, p = 0.035). There was also no difference in the incidence of cardiac comorbidities such as coronary artery disease and hypertension. Though the incidence of type II diabetes was much higher in the late-onset heart failure group compared to control, and which was not significant when comparing the early-onset and control group, there was no significant difference between the incidence of type II diabetes between the early- and late-onset heart failure group (p = 0.16).
Discussion
The purpose of this retrospective study was to examine the incidence of heart failure in breast cancer patients treated with anthracyclines, with focus on identifying unique risk factors for early and late AIHF. Due to the increase risk for mortality, as was seen in our study, the most serious manifestation of anthracycline cardiotoxicity is late-onset AIHF. In our population, the mortality in those who developed late-onset AIHF was 38.4 % compared to 20.6 % in the control group (p < 0.001). Although we cannot conclude that the increased mortality in the late-onset heart failure group was exclusively due to the cardiomyopathy as the mortality data did not specify cause of death, the significantly higher mortality is still a significant finding. Few studies have evaluated late-onset AIHF in breast cancer patients as a distinct entity, and therefore its incidence and predisposing factors are not well known. We used a common clinical definition of heart failure in our study, which is an absolute LVEF ≤45 % in the setting of confirmed clinical assessment.
We found the incidence of late-onset AIHF to be 7.6 %, which is comparable to other studies especially of adult survivors of pediatric cancers [6]. An important contribution to this area is the Romond et al. long-term follow-up study of the NSABP B-31 trial [32]. In this report, cardiac events in patients treated with and without trastuzumab after adjuvant doxorubicin and cyclophosphamide were described. Patients with an early drop in LVEF were excluded from receiving trastuzumab and therefore from analysis for late events. Romond et al. described a 3.4 % incidence of cardiac events, which is lower than what we found. However, because 7.8 % of patients experienced an early decrease in LVEF and were excluded from analysis, the patients included in the Romond et al. study were by definition a subset of those receiving anthracycline chemotherapy. This rate of early-onset AIHF is higher than found in our study (2.9 %) which may be because we only included symptomatic LV failure. The differences in incidence of heart failure between the two studies highlight the importance of standardizing the definition of anthracycline-associated heart failure when conducting cardiotoxicity research in cancer survivors [33].
As in other studies, we found that coronary artery disease, hypertension, and dyslipidemia were significant risk factors for the development of AIHF. Contrary to other studies, we did not find that higher cumulative doses of doxorubicin (>240 mg/m2) to be a significant heart failure risk factor. However, only three patients in the early-onset group and eight patients in the late-onset group received doxorubicin doses >240 mg/m2, and therefore, we may be underpowered to detect this effect. Furthermore, we also did not find that left-sided radiation was a significant risk for the development of heart failure, which was also seen in the Romond et al. study. This finding suggests that further studies are needed to assess the true cardiotoxic effect of left-sided radiation, which has been historically believed to be a significant risk factor for the development of heart failure.
HER2 status was a significant predictor for the development of heart failure. This finding is in concordance to numerous other studies that have showed trastuzumab to exert cardiotoxic effects [34]. Because not all patients who were HER2-positive received trastuzumab, HER2 status may be an independent risk factor for AIHF regardless of anti-HER2 therapy. However in our study, we did not examine the effect of HER2 independently of trastuzumab because given the few numbers of HER2-positive patients who did not receive trastuzumab, our study was not powered to evaluate this. Nevertheless, recent studies have shown that HER2 signaling plays a crucial role in cardiomyocyte physiology. Specifically, HER2 overexpression in transgenic mice has resulted in a phenotype with a condition resembling hypertrophic cardiomyopathy [35]. These studies reveal the intimate relationship between HER2 expression, anti-HER2 therapy, and cardiac myocyte structure/function.
Diabetic cardiomyopathy is defined as cardiac ventricular dysfunction in diabetes mellitus in the absence of underlying coronary artery disease or hypertension. Both diastolic and systolic dysfunction can result from the culmination of oxidative stress, inflammation, and multiple other molecular derangements [36, 37]. Diastolic dysfunction is often one of the earliest observable changes in cardiac function, whereas systolic dysfunction typically develops in later stages of the disease [38]. In our study, we found that type II diabetes mellitus was significantly associated with late-onset AIHF but not early-onset AIHF when compared to the control group (p < 0.001 versus p = 0.45, respectively). Again, to our knowledge, this association has not yet been reported in other studies. A plausible explanation for this association is that similar molecular mechanisms underlie the pathophysiology of both late-onset AIHF and diabetic cardiomyopathy, which is why systolic dysfunction is a cardinal manifestation of both disease processes that occur after many years of injury. This novel association highlights the importance of glycemic control in diabetic breast cancer survivors. Furthermore, it opens the door for further research regarding late-onset AIHF prevention.
The power of this study, due to the large number of patients, allowed significant associations to be revealed. It allowed us to examine the early-onset AIHF group and the late-onset AIHF group independently. Bias in the data abstraction process was minimized because there was only one abstractor and this eliminated abstractor conflicts. Limitations of our study stem primarily from its retrospective nature. Doxorubicin dosing was assumed to be standard per the regimen unless otherwise stated in the medical record. Timing of diagnosis of AIHF was based on outpatient billing and follow-up visit dates which can overestimate the true date of development of symptomatic heart failure. Furthermore, as heart failure in our study was defined as LVEF ≤ 45 % and with symptoms documented in clinical assessment, we undoubtedly underestimated the incidence of anthracycline-associated cardiotoxicity by not factoring in asymptomatic LV dysfunction. It is not yet known whether asymptomatic LV dysfunction secondary to anthracyclines increases morbidity and mortality, and therefore, we focused on symptomatic systolic heart failure in this study. Studies such as this can be inherently biased because patients with cardiac risk factors are likely to be evaluated with imaging and followed by a cardiologist, and therefore, more heart failure may be diagnosed. Finally, because we only had access to our institution’s health records, we also cannot know for certain that the diagnosis of heart failure was not made elsewhere.
We report the first study to look at risk factors for both early-onset and late-onset anthracycline-induced heart failure, with focus on late-onset. We provide data that there are key differences between early-onset AIHF and late-onset AIHF. We found that HER2 status was a risk factor for both early- and late-onset AIHF, which may be independent of trastuzumab administration. We also found that type II diabetes mellitus was significantly associated only with late-onset AIHF, which is a novel association. We also found that there was no significantly increased risk for heart failure secondary to cumulative anthracycline dose and concurrent left-sided radiation. These findings comprise a shift in the paradigm of thinking regarding anthracycline cardiotoxicity, as it may be an individual’s genetic makeup and pre-existent comorbidities rather than the treatment itself that elevate the risk for heart failure. In the age of molecular profiling, it may be possible to 1 day determine the risk of developing AIHF based on a patient’s genomic map [39]. Our findings also suggest that breast cancer survivors with these characteristics (diabetes and HER2-positive disease) may benefit from longer monitoring for the development of cardiac toxicity. Recent advancements in strain echocardiography technology demonstrate subclinical changes in cardiomyocyte function after anthracycline administration without any overt changes in LVEF [40, 41]. Therefore, these patients may also benefit from earlier intervention to attempt to prevent the development of late-onset toxicity. Further studies are needed to validate our findings and to assess the utility of implementing these interventions. There is also potential to develop a heart failure risk model based on these characteristics to determine whether a patient should be considered for an alternative non-anthracycline-based chemotherapy regimen. Furthermore, there currently are no standardized guidelines for monitoring the development of cardiotoxicity post-anthracycline administration [33], and our study attempts to take the first step in developing these guidelines by identifying at risk patients. However data from a larger number of patients from a variety of institutions will be needed for development of an accurate risk prediction model.
References
Dang CT. Drug treatments for adjuvant chemotherapy in breast cancer: recent trials and future directions. Expert Rev Anticancer Ther. 2006;6:427–36.
Sachelarie I, Grossbard ML, Chadha M, Feldman S, Ghesani M, Blum RH. Primary systemic therapy of breast cancer. Oncologist. 2006;11:574–89.
Maughan KL, Lutterbie MA, Ham PS. Treatment of breast cancer. Am Fam Physician. 2010;81:1339–46.
Barry E, Alvarez JA, Scully RE, Miller TL, Lipshultz SE. Anthracycline-induced cardiotoxicity: course, pathophysiology, prevention and management. Expert Opin Pharmacother. 2007;8:1039–58.
Von Hoff DD, Layard MW, Basa P, Davis Jr HL, Von Hoff AL, Rozencweig M, et al. Risk factors for doxorubicin-induced congestive heart failure. Ann Intern Med. 1979;91:710–7.
Chen MH, Colan SD, Diller L. Cardiovascular disease: cause of morbidity and mortality in adult survivors of childhood cancers. Circ Res. 2011;108:619–28.
Yeh ETH, Bickford CL. Cardiovascular complications of cancer therapy: incidence, pathogenesis, diagnosis, and management. J Am Coll Cardiol. 2009;53:2231–47.
Chatterjee K, Zhang J, Honbo N, Karliner JS. Doxorubicin cardiomyopathy. Cardiology. 2010;115:155–62.
Sabel MS, Levine EG, Hurd T, Schwartz GN, Zielinski R, Hohn D, et al. Is MUGA scan necessary in patients with low-risk breast cancer before doxorubicin-based adjuvant therapy? Multiple gated acquisition. Am J Clin Oncol. 2001;24:425–8.
Grenier MA, Lipshultz SE. Epidemiology of anthracycline cardiotoxicity in children and adults. Semin Oncol. 1998;25:72–85.
Trachtenberg BH, Landy DC, Franco VI, Henkel JM, Pearson EJ, Miller TL, et al. Anthracycline-associated cardiotoxicity in survivors of childhood cancer. Pediatr Cardiol. 2011;32:342–53.
Pinder MC, Duan Z, Goodwin JS, Hortobagyi GN, Giordano SH. Congestive heart failure in older women treated with adjuvant anthracycline chemotherapy for breast cancer. J Clin Oncol. 2007;25:3808–15.
Doyle JJ, Neugut AI, Jacobson JS, Grann VR, Hershman DL. Chemotherapy and cardiotoxicity in older breast cancer patients: a population-based study. J Clin Oncol. 2005;23:8597–605.
Yood MU, Wells KE, Alford SH, Dakki H, Beiderbeck AB, Hurria A, et al. Cardiovascular outcomes in women with advanced breast cancer exposed to chemotherapy. Pharmacoepidemiol Drug Saf [Internet]. 2012 [cited 2012 May 22]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/22419528.
Brower V. Cardiotoxicity debated for anthracyclines and trastuzumab in breast cancer. J Natl Cancer Inst. 2013;105:835–6.
Carver JR, Shapiro CL, Ng A, Jacobs L, Schwartz C, Virgo KS, et al. American society of clinical oncology clinical evidence review on the ongoing care of adult cancer survivors: cardiac and pulmonary late effects. J Clin Oncol. 2007;25:3991–4008.
Barrett-Lee PJ, Dixon JM, Farrell C, Jones A, Leonard R, Murray N, et al. Expert opinion on the use of anthracyclines in patients with advanced breast cancer at cardiac risk. Ann Oncol. 2009;20:816–27.
Ryberg M, Nielsen D, Cortese G, Nielsen G, Skovsgaard T, Andersen PK. New insight into epirubicin cardiac toxicity: competing risks analysis of 1097 breast cancer patients. J Natl Cancer Inst. 2008;100:1058–67.
Smith LA, Cornelius VR, Plummer CJ, Levitt G, Verrill M, Canney P, et al. Cardiotoxicity of anthracycline agents for the treatment of cancer: systematic review and meta-analysis of randomised controlled trials. BMC Cancer. 2010;10:337.
Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97:2869–79.
Feola M, Garrone O, Occelli M, Francini A, Biggi A, Visconti G, et al. Cardiotoxicity after anthracycline chemotherapy in breast carcinoma: effects on left ventricular ejection fraction, troponin I and brain natriuretic peptide. Int J Cardiol. 2011;148:194–8.
Garrone O, Crosetto N, Lo Nigro C, Catzeddu T, Vivenza D, Monteverde M, et al. Prediction of anthracycline cardiotoxicity after chemotherapy by biomarkers kinetic analysis. Cardiovasc Toxicol. 2012;12:135–42.
Romano S, Fratini S, Ricevuto E, Procaccini V, Stifano G, Mancini M, et al. Serial measurements of NT-proBNP are predictive of not-high-dose anthracycline cardiotoxicity in breast cancer patients. Br J Cancer. 2011;105:1663–8.
Meinardi MT, Van Der Graaf WTA, Gietema JA, Van Den Berg MP, Sleijfer DT, De Vries EGE, et al. Evaluation of long term cardiotoxicity after epirubicin containing adjuvant chemotherapy and locoregional radiotherapy for breast cancer using various detection techniques. Heart. 2002;88:81–2.
Russell SD, Blackwell KL, Lawrence J, Pippen Jr JE, Roe MT, Wood F, et al. Independent adjudication of symptomatic heart failure with the use of doxorubicin and cyclophosphamide followed by trastuzumab adjuvant therapy: a combined review of cardiac data from the National Surgical Adjuvant Breast and Bowel Project B-31 and the North Central Cancer Treatment Group N9831 clinical trials. J Clin Oncol. 2010;28:3416–21.
Verma S, Ewer MS. Is cardiotoxicity being adequately assessed in current trials of cytotoxic and targeted agents in breast cancer? Ann Oncol. 2011;22:1011–8.
Jannazzo A, Hoffman J, Lutz M. Monitoring of anthracycline-induced cardiotoxicity. Ann Pharmacother. 2008;42:99–104.
What are the key statistics about breast cancer? [Internet]. [cited 2011 Sep 13]. Available from: http://www.cancer.org/Cancer/BreastCancer/DetailedGuide/breast-cancer-key-statistics.
Cancer of the Breast—SEER stat fact sheets [Internet]. [cited 2011 Sep 13]. Available from: http://seer.cancer.gov/statfacts/html/breast.html#survival.
Allen LA, Yood MU, Wagner EH, Aiello Bowles EJ, Pardee R, Wellman R, et al. Performance of claims-based algorithms for identifying heart failure and cardiomyopathy among patients diagnosed with breast cancer. Med Care. 2012.
Ryberg M, Nielsen D, Skovsgaard T, Hansen J, Jensen BV, Dombernowsky P. Epirubicin cardiotoxicity: an analysis of 469 patients with metastatic breast cancer. J Clin Oncol. 1998;16:3502–8.
Romond EH, Jeong J-H, Rastogi P, Swain SM, Geyer CE, Ewer MS, et al. Seven-year follow-up assessment of cardiac function in NSABP B-31, a randomized trial comparing doxorubicin and cyclophosphamide followed by paclitaxel (ACP) with ACP plus trastuzumab as adjuvant therapy for patients with node-positive, human epidermal growth factor receptor 2-positive breast cancer. J Clin Oncol. 2012;30:3792–9.
Shelburne N, Adhikari B, Brell J, Davis M, Desvigne-Nickens P, Freedman A, et al. Cancer treatment-related cardiotoxicity: current state of knowledge and future research priorities. J. Natl. Cancer Inst. 2014;106.
Slamon D, Eiermann W, Robert N, Pienkowski T, Martin M, Press M, et al. Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med. 2011;365:1273–83.
Sysa-Shah P, Xu Y, Guo X, Belmonte F, Kang B, Bedja D, et al. Cardiac-specific over-expression of epidermal growth factor receptor 2 (ErbB2) induces pro-survival pathways and hypertrophic cardiomyopathy in mice. PLoS One. 2012;7:e42805.
Bugger H, Abel ED. Molecular mechanisms of diabetic cardiomyopathy. Diabetol. 2014.
Huynh K, Bernardo BC, McMullen JR, Ritchie RH. Diabetic cardiomyopathy: mechanisms and new treatment strategies targeting antioxidant signaling pathways. Pharmacol Ther 2014.
Vinereanu D, Nicolaides E, Tweddel AC, Mädler CF, Holst B, Boden LE, et al. Subclinical left ventricular dysfunction in asymptomatic patients with type II diabetes mellitus, related to serum lipids and glycated haemoglobin. Clin Sci. 2003;105:591–9.
Ky B, Vejpongsa P, Yeh ETH, Force T, Moslehi JJ. Emerging paradigms in cardiomyopathies associated with cancer therapies. Circ Res. 2013;113:754–64.
Poterucha JT, Kutty S, Lindquist RK, Li L, Eidem BW. Changes in left ventricular longitudinal strain with anthracycline chemotherapy in adolescents precede subsequent decreased left ventricular ejection fraction. J Am Soc Echocardiogr. 2012;25:733–40.
Stoodley PW, Richards DAB, Hui R, Boyd A, Harnett PR, Meikle SR, et al. Two-dimensional myocardial strain imaging detects changes in left ventricular systolic function immediately after anthracycline chemotherapy. Eur J Echocardiogr. 2011;12:945–52.
Conflict of interest
Authors Angel Qin, Cheryl Thompson, and Paula Silverman declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Qin, A., Thompson, C.L. & Silverman, P. Predictors of late-onset heart failure in breast cancer patients treated with doxorubicin. J Cancer Surviv 9, 252–259 (2015). https://doi.org/10.1007/s11764-014-0408-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-014-0408-9