Abstract
Objectives
Physical activity (PA) improves health-related quality of life (HRQL) in several cancer survivor groups but no studies have focused on young adult cancer survivors (YACS). This study determined the prevalence of PA in YACS and examined dose-response associations with HRQL.
Methods
A random sample of 2,000 YACS between the ages of 20–44 were identified through a Canadian provincial cancer registry and mailed a survey that included the Leisure-Time Exercise Questionnaire, the Medical Outcomes Study 36-Item Short Form (SF36) survey, and several validated psychosocial scales. The primary endpoint was the physical component summary (PCS) of the SF36.
Results
Completed questionnaires were received from 588 YACS. In terms of PA prevalence, 23% were completely sedentary, 25% were insufficiently active, 22% were active within public health guidelines, and 29% were active above public health guidelines. Analysis of covariance adjusted for important medical and demographic covariates showed a statistically significant and clinically meaningful dose-response association between PA and the PCS that spanned 6.3 points (95% confidence interval [CI] 3.7 to 8.8; p < 0.001) from completely sedentary to within guidelines. Similar associations were found for the mental component summary scale (p = 0.002), depression (p < 0.001), stress (p < 0.001) and self-esteem (p < 0.001). Associations between PA and HRQL were stronger for YACS that had previously received chemotherapy.
Conclusions
PA is strongly associated with HRQL in YACS but only half of YACS are meeting public health guidelines and almost a quarter are completely sedentary. Randomized controlled trials examining intervention strategies to increase PA and improve health outcomes in this understudied patient population are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 10,000 young adults between the ages of 20 and 44 years are diagnosed with cancer each year in Canada [1] and over 100,000 are diagnosed in the United States [2]. This age group encompasses the shift from adolescence, generally defined as 15–19 years of age, and the average age of onset for menopause-associated hormonal changes in women which directly affects their cancer profile. The most common types of cancers in the young adult age group are breast for females and testicular for males [3].
Young adult cancer survivors (YACS) possess many distinctive physiological and psychosocial characteristics. Even so, medicine has traditionally been divided into pediatric and internal medicine, resulting in young adults falling between the gaps of these two disciplines [4]. Twenty years ago, YACS had a higher survival rate than pediatric and older adult cancer survivors [4–6]. Since then, advances in treatment have increased the survival rates of pediatric and older adult cancer survivors but a similar improvement has not been observed for YACS [6–8]. Being diagnosed with cancer as a young adult can be particularly devastating because of the potential to spend decades living with the psychological, physical, reproductive, social and spiritual effects of the disease and its treatments [1]. Few interventions have been developed to address these long term concerns of YACS.
Physical activity (PA) may influence the long term health of YACS. Systematic reviews have summarized the evidence for the benefits of PA in several cancer survivor groups including mixed cancer survivors [9], breast cancer survivors [10], prostate cancer survivors [11], hematologic cancer survivors [12], advanced disease cancer survivors [13], and even older cancer survivors [14] but no studies have focused on YACS. Here, we report what we believe to be the first study examining PA in YACS. The specific objectives of the study were to: (a) estimate the PA prevalence rate in YACS, (b) determine the nature of the association between PA and HRQL in YACS, and (c) explore if any common medical or demographic variables moderated any of the associations between PA and HRQL. We hypothesized that PA would be positively associated with HRQL in YACS in a dose-response fashion, especially for the physical functioning aspects of HRQL.
Methods
Participants and procedures
Ethical approval for this study was granted by the Alberta Cancer Board and the University of Alberta. The study used a cross-sectional design with a mailed, self-administered survey. Eligibility for the study included: (a) diagnosed with invasive cancer in Alberta between the ages of 20–44 years in the past 10 years and (b) still currently between the ages of 20–44 years and living in Alberta. Prospective participants were drawn from the Alberta Cancer Registry. Previous research has outlined the legitimacy and advantages of using cancer registries as a recruitment tool [15] and we have used the Alberta Cancer Registry successfully in previous surveys [16–19]. The registry was searched by age, time since diagnosis, and address to identify YACS that were eligible for this study. A random sample of 2,000 YACS was drawn from a provincial, population-based sample of 5,352 diagnosed between the years of 1998–2007 that were still alive and living in Alberta.
The survey was conducted by the cancer registry on behalf of the investigators and followed the Total Design Method [20]. In the initial mailed materials, prospective participants received: (a) a letter of invitation from the registry explaining the general purpose of the registry and its role in this particular study, (b) a letter from the investigators explaining the study, and (c) a copy of the survey. A postcard reminder was mailed 3–4 weeks later, and a second survey was mailed 3–4 weeks after that to nonresponders.
Instruments
Physical activity
The Leisure Score Index (LSI) from the Leisure Time Exercise Questionnaire [21] was used to assess the average weekly frequency and duration of PA over the past month in three separate intensity categories: light (minimal effort, no perspiration), moderate (not exhausting, light perspiration), and vigorous (heart beats rapidly, sweating). An evaluation of the Godin Leisure-Time Exercise Questionnaire found a 1 month test-retest reliability of 0.62 [22, 23] and concurrent validity coefficient of 0.32 with on objective indicator of PA (i.e., an accelerometer) [23]. The percentage of participants meeting the public health PA guidelines was calculated based on the 2008 Physical Activity Guidelines for Americans [24] which suggest that individuals should obtain either 75 min of vigorous activity per week, 150 min of moderate activity per week, or an equivalent combination that double weights the vigorous minutes. Participants were divided into the following four categories: (1) completely sedentary (no moderate or vigorous PA), (2) insufficiently active (some PA but less than the equivalent of 150 min of moderate activity/week), (3) within guidelines (within the equivalent of 150 to 300 min of moderate activity/week), and (4) above guidelines (≥ the equivalent of 300 min of moderate activity/week).
The Medical Outcomes Study 36-Item Short Form (SF-36) survey [25, 26] was used to assess HRQL. The SF36 contains eight subscales that can be summed and weighted to provide a physical component summary (PCS) score and a mental component summary (MCS) score. Higher scores indicate better functioning. The validity and reliability of the SF-36 has been established in cancer survivors [27] revealing Cronbach’s α coefficient for all subscales ranging from 0.79 to 0.90, test-retest scores from 0.81 to 0.93 and validity coefficients of ≥0.61 for all subscales. Stress was assessed by the Perceived Stress Scale [28] which has a Cronbach’s α of 0.87 and a test re-test reliability score of 0.86 [29]. The correlations between perceived stress and other stress measures ranged from 0.22 to 0.32 [29].
Self-esteem was assessed by the Rosenberg Self-Esteem Scale [30] which has a Cronbach’s α and test-retest of 0.88 and a construct validity of 0.46 to 0.71 [31]. Depression was measured by the Center for Epidemiologic Studies-Depression (CES-D) scale [32]. In an evaluation with a cancer population the CES-D had a Cronbach’s α of 0.89 and a test-retest score of 0.57. The correlations between the CES-D and other depressive assessments were between 0.65 and 0.77 [33].
Demographic variables were assessed by self-report and included age, sex, employment, education, income, ethnicity, marital status, and height and weight to calculate body mass index (BMI). Medical variables were collected by self-report and included time since diagnosis, type of cancer, disease stage, previous and current treatments, previous recurrence, and current status of cancer. Registry data consisting of age, sex, time since diagnosis, and type of cancer were available for a comparison between responders and nonresponders.
Statistical analyses
We conducted one-way analyses of covariance (ANCOVAs) with the public health PA guideline categories as the independent variable and the HRQL scales, self esteem, depression and stress scales as the dependent variables. Our primary analyses were adjusted for important demographic and medical covariates including age, sex, marital status, education, ethnicity, BMI, months since diagnosis, surgery, chemotherapy, radiation, current treatment status, current cancer status, smoking, drinking, and number of comorbidities. Significant ANCOVAs were followed by Tukey post hoc tests. Standardized effect size d was calculated for scales without a minimally important difference (MID). Effect size d is commonly interpreted as 0.20 being small, 0.50 being medium, and 0.80 being large with ds between 0.33 and 0.50 being considered clinically meaningful. Interactions were explored with two-way factorial ANCOVAs using the public health PA guideline categories and selected moderators with a minimum cell size of 60 participants (i.e., age, sex, marital status, education, ethnicity, BMI, months since diagnosis, surgery, chemotherapy, radiation, current treatment status, and current cancer status).
Results
Sample characteristics
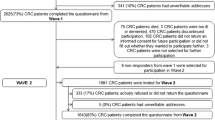
Figure 1 provides a summary of participant flow through the study. Of the 2,000 mailed surveys, 460 (23%) were returned because of a wrong address. Of the remaining 1,540 surveys, 894 did not respond, 54 responded and noted that were unwilling to participate, 4 returned the completed survey after the deadline, and 588 returned the completed survey, resulting in a 29% completion rate (588/2,000) and a 38% response rate (588/1,540) excluding the wrong addresses.
We were able to access data from the registry to examine the representativeness of our sample of YACS compared to the broader population of YACS in Alberta. We found that our sample was: (a) similar in age (55% versus 55% in the age range 30–39), (b) slightly over represented women (73% versus 64%), (c) similar on 8 out of 10 cancer diagnoses with the exceptions of a slight overrepresentation of breast cancer (24% versus 18%) and a slight underrepresentation of testicular cancer (6% versus 12%) consistent with the observed sex differences, (d) similar on receipt of surgery (78% versus 79%) with a slight overrepresentation on receipt of chemotherapy (47% versus 40%) and radiation therapy (39% versus 32%), and (e) similar on time since diagnosis (5.0 versus 5.4 years).
Sample characteristics are presented in Tables 1 and 2. The mean age of the participants was 38.2 ± 5.6, 70.4% were female, 72.8% were married, and 61.9% had completed university/college. The mean BMI of participants was 26.5 ± 5.7 with 52.7% of the participants being overweight or obese. The most common cancers were breast (n = 137), thyroid (n = 80) and lymphoma (n = 72). At the time of the survey, 87.4% of participants were disease-free.
Prevalence rate of physical activity
Based on the public health guidelines, 23.5% of YACS were completely sedentary (CS), 25.2% were insufficiently active (IA), 22.3% were within guidelines (WG), and 29.1% were above guidelines (AG). On average, participants reported 86 min of moderate and 72 min of vigorous PA. By public health category, CS participants reported no moderate or vigorous PA, IA participants reported an average of 58 (SD = 38) moderate and 10 (SD = 18) vigorous minutes, WG participants reported an average of 104 (SD = 75) moderate and 53 (SD = 44) vigorous minutes, and AG participants reported an average of 165 (SD = 219) moderate and 199 (SD = 179) vigorous minutes.
Associations between physical activity and health-related quality of life
HRQL data by public health guidelines are presented in Table 3 and Fig. 2a–e. ANOVAs indicated significant associations between the public health PA guidelines and the PCS (p < 0.001), MCS (p = 0.002), depression (p < 0.001), stress (p < 0.001), and self-esteem (p < 0.001). Tukey post hoc tests indicated that the general pattern for the PCS and psychosocial variables was a linear increase from CS to IA to WG with a plateauing at AG. For MCS, there was a threshold association between IA and WG. In terms of the magnitude of the associations, the maximal differences among the PA categories were 6.3 points (CI, 3.7 to 8.8) for the PCS, 4.6 points (CI, 1.2 to 8.1) for the MCS, and standardized effect sizes of d = 0.46 for depression, d = 0.63 for self-esteem, and d = 0.55 for stress (Table 3).
Data for the eight subscales of the SF36 are presented in Table 4. ANOVAs indicated significant associations between the public health PA guidelines and physical functioning (p < 0.001), bodily pain (p < 0.001), role physical (p < 0.001), general health (p < 0.001), vitality (p < 0.001), social functioning (p < 0.001), role emotional (p < 0.001) and mental health (p = 0.004). Tukey post hoc tests showed that the general pattern of association for the eight subscales was a linear increase from CS to IA to WG with a plateauing at AG. The overall maximal differences among the PA categories was 5.9 points (CI, 3.3 to 8.2) for physical functioning, 4.9 points (CI, 2.2 to 7.6) for bodily pain, 6.7 (CI, 3.6 to 9.4) points for role physical, 7.3 points (CI, 4.3 to 10.4) for general health, 8.4 points (CI, 5.2 to 11.0) for vitality, 5.7 (CI, 2.3 to 8.8) points for social functioning, 4.7 (CI,1.2 to 7.9) points for role emotional, and 3.9 (CI, 1.2 to 7.9) for mental health.
Moderators of the associations between physical activity and quality of life
There was a significant interaction between public health PA guidelines and past chemotherapy for the PCS (p for interaction = 0.031) and self-esteem (p for interaction =0.035). The association between PA and the PCS was stronger (7.1 points) and dose-response (from CS to WG) for participants who had received past chemotherapy whereas it was more modest (2.9 points) and threshold (from IA to WG) for individuals who had not received past chemotherapy (Fig. 3a). Similarly, the association between public health PA guidelines and self-esteem was also stronger (3.9 points) and dose-response (CS to WG) for individuals who had received past chemotherapy and more modest (1.5 points) and threshold (IA to WG) for individuals who had not received past chemotherapy (Fig. 3b).
There were borderline significant interactions between public health PA guidelines and past chemotherapy for stress (p for interaction = 0.054; Fig. 3c) and depression (p for interaction = 0.078; Fig. 3d) that exhibited the same patterns as the PCS and self-esteem. There was also a borderline significant interaction between public health PA guidelines and sex for depression (p for interaction = 0.088; Fig. 3e). The association between PA and depression was much stronger (3.6 points) and dose-response (CS to AG) for women whereas it was much weaker and U-shaped for men.
Discussion
In this Canadian provincial survey, only half of YACS were meeting public health PA guidelines and almost a quarter were completely sedentary. The 53.4% of YACS that were meeting PA guidelines is slightly lower than the 61.1% of young adults in the general Alberta population [34] although the studies are not directly comparable due to differences in measurement and definitions of meeting guidelines. In other studies of YACS, Coups and Ostroff [35] reported that 41% of YACS aged 18–39 were physically active whereas Bellizzi et al. [36] reported that 37.6% of YACS aged 18–40 were active. Again, direct comparisons with our study are not straight forward due to differences in PA measures and guideline definitions. Both of those studies noted that YACS were more likely to be active than middle-aged and older cancer survivors but not more active than age-matched population controls. Whether YACS are more or less active than their age-matched controls is an important question but it does not negate the potential benefits that may accrue to YACS from PA participation.
The main finding of our study is the steep dose-response associations between PA and HRQL in YACS, especially for the physical functioning aspects of HRQL. In particular, there were significant increases in the PCS from completely sedentary to insufficiently active and from insufficiently active to meeting guidelines, with no further increase for exceeding the guidelines. The gain was 2.2 points for being insufficiently active and 3.1 points for being within the guidelines. The total increase of over 5 points on the PCS is 2.5 times the MID of 2 points for this scale. There are no published studies that have examined the association between PA and HRQL in YACS with which to compare our findings. Studies are available on various adult cancer survivor populations and our findings are consistent with these studies showing stronger associations or effects of PA on physical functioning [37, 38]. Mechanisms through which PA may influence physical functioning in YACS include improved cardiorespiratory fitness, muscular strength and endurance, body composition, range of motion, balance, and reduction in comorbidities.
In contrast, the association between PA and the MCS appeared to follow a threshold association. After adjustment for important medical and demographic covariates, the gain from completely sedentary to insufficiently active was only 0.4 points whereas the gain from insufficiently active to within guidelines was 2.9 points, just under the MID of 3.0 points for this scale. Meeting the public health PA guidelines was also associated with improvements in self-esteem, stress, and depression, indicating overall better mental health with meeting the PA guidelines. Improvements in mental health from PA may similarly result from improved fitness but they may also arise from psychosocial aspects of PA including increased social interaction, friendly competition, as a distraction from daily worries, improved body image, and self-confidence that may be particularly important for YACS.
Associations between PA and HRQL were particularly pronounced for YACS that had received previous chemotherapy, although we acknowledge that our medical data is based on self-report. For the PCS, there was a 7.2 point gain from CS to WG which is over triple the MID for this scale. Conversely, for participants that had not received previous chemotherapy, there was a threshold effect of meeting the PA guidelines of 2.9 points. This is consistent with research in ovarian cancer survivors that demonstrated a stronger association between PA and HRQL in survivors with existing disease [17], suggesting that the benefits of PA are more pronounced in groups that need it the most (i.e., are at the lower end of functioning). There were also significant or borderline significant interactions between PA and past chemotherapy for self-esteem, stress, and depression, suggesting that this interaction is unlikely a chance finding. For YACS who have received chemotherapy, it appears that even smaller amounts of PA (i.e., being insufficiently active) may be beneficial whereas for YACS that have not been treated with chemotherapy, achieving the PA guidelines may be necessary for meaningful benefits.
There was a borderline significant association between public health PA guidelines and sex for depression. Women demonstrated a clear and strong dose-response association between PA and depression. Men, on the other hand, demonstrated a more modest dose-response association from CS to WG but then actually exhibited an increase in depression from WG to AG. The etiology of why women report greater depression than men is still unknown [39] but it is possible that women benefit more from PA because of their higher levels of depression. Moreover, the stronger association between PA and depression for women may be because women experience more frequent symptoms such as anxiety, sleep disturbances, and weight gain [40] and PA is known to reduce anxiety [41], help regulate sleep [42] and maintain weight [43]. It is also possible that women benefit more from the social aspects of PA. Given that this finding occurred only for depression and was only borderline significant, it should be interpreted with caution and additional research on any sex differences is needed. Other moderators were examined but did not influence the association between PA and HRQL including age, marital status, education, BMI, months since diagnosis, surgery, radiation, current treatment status, current cancer status, smoking, drinking, and the number of comorbidities.
Our study has important strengths and limitations. To the best of our knowledge, our study is the first to focus on PA in YACS. Moreover, we obtained a large, random, population-based sample of YACS from a comprehensive registry in Alberta, Canada and used validated measures of PA and HRQL. Perhaps the most significant limitation of our study is that it was cross-sectional and the causal effects of PA on HRQL cannot be determined. Other limitations include the self-report measures of PA and medical data, the modest response rate that resulted in a select sample of YACS that underrepresented younger YACS, men, and longer term survivors. Despite these limitations, our study provides the first data documenting the PA prevalence rates of YACS and identifying some of the complex associations between PA and HRQL in YACS.
In summary, PA is strongly associated with HRQL, self-esteem, stress and depression in YACS, especially those that have received past chemotherapy. Yet, only about half of YACS are achieving the public health PA guidelines and nearly a quarter are completely sedentary. Lack of PA may place YACS at increased risk for poor disease outcomes, other chronic diseases, and premature death in addition to poorer HRQL. Additional research is warranted into intervention strategies to increase PA in YACS and determine the causal effects on PA on HRQL and disease outcomes in this understudied cancer patient population.
References
Theis B, Nishri, D, Balh S, Ugnat A-M, Marrett L, Cancer in young adults in Canada. Toronto: Cancer Care Ontario; 2006. ISBN 0-921325-10-X.
Ries LAG, Melbert D, Krapcho M, Stinchcomb DG, Howlader N, Horner MJ, Mariotto A, Miller BA, Feuer EJ, Altekruse SF, Lewis DR, Clegg L, Eisner MP, Reichman M, Edwards BK (eds). SEER Cancer Statistics Review, 1975-2005, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2005/, based on November 2007 SEER data submission, posted to the SEER web site, 2008.
Marrett LD, Frood J, Nishri D, Ugnat A, The Cancer in Young Adults in Canada (CYAC) Working Group. Cancer incidence in young adults in Canada: preliminary results of a cancer surveillance project. Chron Dis Can. 2002;23(2):58–64.
Burke ME, Albritton, K, Marina, N. Challenges in the recruitment of adolescents and young adults to cancer clinical trials. Cancer, 2007;110(11): 2385–2393.
Bleyer A. Cancer in older adolescents and young adults: epidemiology, diagnosis, treatment, survival and importance of clinical trials. Med Pediatr Oncol. 2006;38:1–10.
Soliman H, Agresta SV. Current issues in adolescent and young adult cancer survivorship. Cancer Control. 2008;15(1):55–62.
Bleyer A. Young adult oncology: the patients and their survival challenges. CA Cancer J Clin. 2007;57(4):242–55.
Shaw PH, Ritchey AK. Different rates of clinical trial enrollment between adolescents and young adults ages 15–22 years old and children under 15 with cancer at a children’s hospital. J Pediatr Hematol/Oncol. 2007;29(12):811–4.
Schmitz KH, Holtzman J, Courneya KS, Masse LC, Duval S, Kane R. Controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. Cancer Epidemiol Biomark Prev. 2005;14(7):1588–95.
McNeely ML, Campbell KL, Rowe BH, Klassen TP, Mackey JR, Courneya KS. Effects of exercise on breast cancer patients and survivors: a systematic review and meta-analysis. Can Med Assoc J. 2006;175(1):34–41.
Thorsen L, Courneya KS, Stevinson C, Fossa SD. A systematic review of physical activity in prostate cancer survivors: outcomes, prevalence, and determinants. Support Care Cancer. 2008;16(9):987–97.
Liu RDKS, Chinapaw MJM, Huijgen PC, van Mechelen W. Physical exercise interventions in haematological cancer patients, feasible to conduct but effectiveness to be established: a systematic review. Cancer Treat Rev. 2008;35(2):185–92.
Lowe SS, Watanabe SM, Courneya KS. Physical activity as a supportive care intervention in palliative cancer patient: a systematic review. J Support Oncol. 2009;7(1):27–34.
Courneya KS, Vallance JKH, McNeely M, Karvinen KH, Peddle CJ, Mackey JR. Exercise issues in older cancer survivors. Crit Rev Oncol/Hematol. 2004;51:249–61.
Pakilit A, Kahn BA, Petersen MS, Abraham LS. Making effective use of tumor registries for cancer survivorship research. Cancer 2001;92(5):1305–14.
Vallance JKH, Courneya KS, Jones LW, Reiman T. Differences in quality of life between non-hodgkin’s lymphoma survivors meeting and not meeting public health exercise guidelines. Psycho Oncol. 2005;14:979–91.
Stevinson C, Faught W, Steed H, Tonkin K, Ladha AB, Vallance JK, et al. Associations between physical activity and quality of life in ovarian cancer suvivors. Gynecol Oncol. 2007;106(1):244–50.
Peddle CJ, Plotnikoff RC, Wild C, Au H-J, Courneya KS. Medical, demographic, and pscyhosocial correlates of exercise in colorectal cancer survivors: an application of self determination theory. Support Care Cancer. 2007;16(1):9–17.
Karinen KH, Courneya KS, North S, Venner P. Associations between exercise and quality of life in badder cancer survivors: a population-based study. Cancer Epidemiol Biomark Prev. 2007;16:984–90.
Dillman DA. Mail and telephone surveys- the total design method. New York; Wiley; 1978. 375 pp.
Godin G, Jobin J, Bouillon J. Assessment of leisure time exercise behaviour by self report: a concurrent validity study. Can J Public Health. 1986;77(5):359–62.
Okun M, Karoly P, Lutz R. Clarifying the contribution of subjective norm to predicting leisure-time exercise. Am J Health Behav. 2002;26(4):296–305.
Goldberg DP, Rickels K, Downing R, Hesbacher P. A comparison of two psychiatric screening tests. Br J Psychol. 1976;129:61–7.
US Department of Health and Human Services (USDHHS). 2008 Physical Activity Guidelines for Americans. Washington, DC: USDHHS; http://www.health.gov/paguidelines/default/aspx. Accessed December 4, 2008.
Ware J, Snow KK, Kosisnki M, Gandek B. SF-36 health survey: manual and interpretation guide. Boston: The Health Institite, New England Medical Center; 1993.
Ware J, Kosisnki M. Physical and mental health summary scales: a manual for users of version 1 (2nd Edition). Lincoln, RI: QualityMetric, 2001.
Pinar R. Reliability and construct validity pf the SF 36 in Turkish cancer patients. Qual Life Res. 2004;14(1):259–64.
Cohen S, Kamarck T, Mermelstein R. A global measure of stress. J Health Soc Behav. 1983;24(4):385–96.
Reis RS, Hino A, Anez CR. Perceived stress scale: reliability and validity study in Brazil. J Health Psychol. 2010;15(1):107–14.
Rosenburg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965, 326 pp
Robins R, Hendin HM, Trzesniewski KH. Measuring global self-esteem: construct vlidation of single-item measure and the Rosenburg self esteem scale. Pers Soc Psychol Bull. 2001;27:151.
Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10(2):77–84.
Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: evaluation of the centre for epidemilogical studies depression (CES-D). J Psychosom Res. 1999;46(5):437–43.
Loitz C, Berry TR, Spence JC. 2009 Alberta survey on physical activity: a concise report, Active Centre for Active Living; 2009 http://www.centre4activeliving.ca/publications/ab-survey-physical-activity/2009-report.pdf.
Coups EJ, Ostroff JS. A population-based estimate of the prevalence of behavioural risk factors among adult cancer survivors and noncancer controls. Prev Med. 2004;40:702–11.
Bellizzi KM, Rowland JH, Jeffery DD, McNeel T. Health behaviours of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol. 2005;23(34):8884–93.
Courneya KS, Mackey JR, Bell GJ, Jones LW, Field CJ, Fairey AS. Randomized controlled trial of exercise training in postmenopausal breast cancer survivors. J Clin Oncol. 2003;21(9):1660–8.
Courneya KS, Friedenreich CM, Sela RA, Quinney HA, Rhodes R, Handman M. The group pscyhotherapy and home-based physical exercise (group-hope) trial in cancer survivors: physical fitness and quality of life outcomes. Psycho Oncol. 2003;12(4):357–74.
Young E, Korszun A. Sex, trauma, stress hormones and depression. Mol. Psychiatry. 2010;15(1):23–28.
Bhatia SC, Bhatia SK. Depression in women: diagnostic and treatment considerations. Am Fam Physician. 1999;60(1):225–34.
Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin Psychol Rev. 2001;21(1):33–61.
Youngstedt SD. Effects of exercise on sleep. Clin Sports Med. 2005;24(2):355–65.
Blair SN. Evidence for success of exercise in weight loss and control. Ann Intern Med. 1993;119(7):702–6.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bélanger, L.J., Plotnikoff, R.C., Clark, A. et al. Physical activity and health-related quality of life in young adult cancer survivors: a Canadian provincial survey. J Cancer Surviv 5, 44–53 (2011). https://doi.org/10.1007/s11764-010-0146-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-010-0146-6