Abstract
Background
The discussions at the surgical levels (sympathectomy levels) about endoscopic thoracic sympathectomy (ETS) method, which is applied in hyperhidrosis treatment in the present day and acknowledged as the golden treatment method, continue. Mainly, most of the studies evaluates postoperative early period results. Our aim in this study is to compare the long-term quality of life depending on the different surgical levels (sympathectomy levels) and evaluate the postoperative complications.
Methods
165 patients operated due to palmar hyperhidrosis between January 2012 and July 2017 were evaluated. Sympathectomy was performed either by clipping or cauterization and sympathetic nerves included were T2–4, T3–4, or T3 levels. Data were retrospectively reviewed for complications, factors affecting the postoperative quality of life.
Results
Ninety of the patients were male (54.5%) and 75 (45.5%) were female. The level of ganglion block was T2–T4 in 62 patients (37.6%), T3–T4 in 46 patients (27.9%), and T3 in 57 patients (34.5%). Early complications were observed in 27 patients (16.4%). Compensatory hyperhidrosis (CH) was observed in 62 patients (37.6%). There was a significant difference in the postoperative quality of life according to ETS level (p < 0.001). Patients who underwent T2–T4 sympathectomy had a lower quality of life than patients who underwent isolated T3 or T3–T4 sympathectomy.
Conclusion
Based on our results, we recommend performing lower level resections to increase the long-term quality of life in palmar hyperhidrosis patients. The lower risk of CH and comparable quality of life suggest that T3 sympathectomy is more effective.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hyperhidrosis has become one of the major pathological conditions that impact and limit human sociocultural relationships. It is frequently seen in young adults, with more pronounced symptoms in individuals with an anxiety disorder. Patients usually experience more severe symptoms in social situations, resulting in avoidance. For this reason, hyperhidrosis causes social and psychological problems [1].
Although there are conservative medical approaches to the treatment of hyperhidrosis, surgery is still considered the most effective treatment. The success rate of sympathectomy in hyperhidrosis is over 95% [2]. There are numerous studies in the literature on endoscopic thoracic sympathectomy (ETS), though a consensus is yet to be reached on the appropriate level at which to perform sympathectomy. The main reasons for this are the development of compensatory hyperhidrosis (CH) and failure to evaluate patients’ quality of life in the postoperative period.
The aim of the current study was to compare the postoperative satisfaction and long-term quality of life according to surgical (sympathectomy) level among patients who underwent ETS for palmar hyperhidrosis in our center.
Materials and methods
The study was approved by the institutional review board and conducted in accordance with the principles of the Declaration of Helsinki.
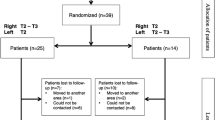
A total of 232 patients who underwent surgery for primary palmar hyperhidrosis in our hospital between January 2012 and July 2017 were retrospectively evaluated. Of these, 165 patients who presented with isolated palmar hyperhidrosis were included in the study. The study flowchart is shown in Fig. 1.
Patient selection
Preoperative evaluations included routine biochemistry, coagulation tests and hemogram; T3, T4, and thyroid stimulating hormone (TSH) to assess thyroid functions; and electrocardiogram (ECG) to assess cardiac functions. Body mass index (BMI) was also calculated for each patient before surgery.
A routine assessment of patient satisfaction was performed preoperatively. The patients’ preoperative satisfaction levels were scored between 1 and 5 (5: very low, 4: low, 3: fair, 2: high, and 1: very high).
Surgical technique
Sympathectomy was performed by three different procedures, depending on surgeon’s preference.
Following general anesthesia, patients were intubated with a double-lumen tube. Patients were seated in a 45° semi-Fowler position. An incision approximately 2 cm in length was made in the second to third intercostal space at the anterior axillary line and the thorax was assessed using a 30° 5-mm thoracoscope (Logic HD, Wolf, Knittlingen, Germany) via an 11-inch trocar. When necessary, a second port incision was made in the fourth intercostal space.
After the identification of the sympathetic chain, the sympathetic ganglion was cut using thermoablation with an endoscopic hook. In addition, thermoablation was performed in the segment between the two nerves using the endoscopic hook. In the clips technique, the sympathetic chain of the related segment was dissected using the hook and the sympathetic ganglion was clipped using 5-mm endoscopic clips (Covidien Inc.).
Sympathectomy was performed either by clipping or cauterization and the sympathetic nerves included were at T2–4, T3–4, or T3 levels. After the procedure, the air was removed from the thorax through catheter aspiration. The procedure was concluded without placing a drain tube. To reduce postoperative pain, all patients received an intercostal nerve block with bupivacaine. The patients’ vital signs were monitored for 24 h postoperatively.
Postoperative follow-up
Treatment success was evaluated using a quality of life scale developed by Amir et al. [3]. Unlike classic satisfaction assessment, this scale evaluates the patients’ social and emotional states. The evaluation yields a quality of life score ranging from 20 to 100, with lower scores reflecting a higher quality of life. Quality of life was considered very low at scores of ≥ 84, low at 69–84, fair at 52–68, high at 36–51, and very high at 20–35. The quality of life of the patients was evaluated in their postoperative first year.
Postoperative complications were categorized as early or late. Early complications included pneumothorax, hemorrhage, bradycardia/arrhythmia, paresthesia, and plegia. Complications occurring more than 1 month after surgery due to compensatory hyperhidrosis were considered late complications. CH was classified as mild, moderate, or severe.
Statistics
Statistical analyses were performed using IBM SPSS Windows 21.0 software. Numerical variables are expressed as mean, standard deviation, and median (minimum–maximum); categorical variables are expressed as numbers and percentages. Numerical data were evaluated for parametric test assumptions (normality and homogeneity of variance) before comparisons. The dependent-samples t test was used to analyze differences between pre- and postoperative quality of life scores. The Kruskal–Wallis test was used to compare the change in the quality of life between the surgical treatment groups. A p value < 0.05 was considered statistically significant.
Results
The patients’ mean age was 22.8 ± 5.7 (range 18–43) years. Ninety patients were male (54.5%) and 75 (45.5%) were female. The mean BMI was 22.4 kg/m2. A total of 143 patients (86.7%) underwent clipping, and 22 (13.3%) underwent sympathectomy. The level of ganglion block was T2–T4 in 62 patients (37.6%), T3–T4 in 46 patients (27.9%), and T3 in 57 patients (34.5%). A single-port approach was used for 156 patients (94.5%) and a double-port approach was used in 9 patients (5.5%). The mean length of hospital stay was 1.8 ± 1.0 days.
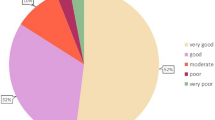
Preoperative satisfaction levels were very low in 63 patients (38.2%), low in 75 patients (45.5%), and fair in 23 patients (13.9%). Four patients (1.8%) whose preoperative satisfaction levels were high underwent surgery.
Early complications were observed in 27 patients (16.4%). The most common complication was pneumothorax, which occurred in 18 patients (10.9%). Four of these pneumothorax cases were mild and treated with oxygen. Six patients had a severe pneumothorax, and eight had a moderate pneumothorax. We used oxygen to resolve the pneumothorax of eight of these patients, but it did not resolve or increase, so we had to place a chest drain in these patients. We think that chest drains were needed because of the injury to the lung parenchyma in the operation. The mean time to lung expansion in patients who had tube thoracostomy was 3.2 ± 0.4 days. Hemorrhage not requiring revision was observed in one patient (0.6%), paresis in two patients (1.2%), forearm plegia in two patients (1.2%), and postoperative bradycardia requiring medical treatment in one patient (0.6%). There were no statistically significant differences in complications based on surgical level, port number, sex, or age (p > 0.05) (Table 1).
CH occurred in 12 patents in the first 3 weeks after surgery. Fifty patients had CH after the first postsurgical month. CH was observed in 62 patients (37.6%). CH of the back was most common, affecting 38 patients (23%). CH also occurred in the feet in 15 patients (9.1%), the abdomen in 15 patients (9.1%), facial area in 6 patients (3.6%), chest area in 8 patients (4.8%), inguinal area in 2 patients (1.2%), and the gluteal area in 8 patients (4.8%). CH was evaluated as mild in 18 patients (10.9%), moderate in 16 patients (9.7%), and severe in 28 patients (17%). The Incidence of CH was significantly associated with surgical level (p < 0.001) (Table 2).
The patients’ mean preoperative quality of life score according to the Amir quality of life scale was 86.5 ± 12.5, and mean postoperative long-term quality of life as assessed using the Amir scale was 38.8 ± 16.3. There was a significant difference in the postoperative quality of life according to the ETS level (p < 0.001). Patients who underwent T2–T4 sympathectomy had a lower quality of life than patients who underwent isolated T3 or T3–T4 sympathectomy. In subgroup analysis, a comparison of T3 and T3–T4 sympathectomy groups revealed no significant difference in quality of life (p = 0.291) (Table 3). There was also no significant difference in quality of life in terms of port numbers (p = 0.521). There was no statistically significant difference between quality of life scores in patients who underwent sympathectomy by clipping and by cauterization (p = 0.174). Quality of life score was not associated with BMI (p = 0.344). The surgical success rate was 96.9%. Recurrence was observed in five patients (3%). All patients with recurrence had undergone T2–T4 sympathectomy.
Discussion
Hyperhidrosis is a pathological condition characterized by sweating more than necessary for physiologic thermoregulation. Palmar hyperhidrosis causes psychological as well as social problems and impairs patients’ quality of life. The condition leads to fear, anxiety, and avoidance of social situations, and therefore requires treatment [1].
Although there are numerous treatment methods available, ETS remains the gold standard treatment for hyperhidrosis. The most common complication of ETS is CH. Its incidence varies greatly, with studies reporting rates of 3–98%. This wide range depends on patient heterogeneity, surgical level, and differences in technique. In most studies on patients who underwent ETS due to isolated palmar hyperhidrosis, higher rates of CH were observed when the T2 sympathetic ganglion was cut [5,6,7]. Lin et al. [4] found that CH with T3 sympathectomy was significantly lower than with T2 sympathectomy (p = 0.001). In 2011, Cerfolio et al. [5] found that CH was better in T3 and T4 sympathectomies compared with T2 in their meta-analysis.
Therefore, the current surgical approach to isolated palmar hyperhidrosis does not include the T2 sympathetic ganglion. The prevalence of CH in our study was 37.6%. In addition, CH was more frequent among patients who had T2–T4 sympathectomy (p < 0.001). Although CH was evaluated as severe in most patients, their postoperative satisfaction levels were found to be high nonetheless.
A lower incidence of CH has been reported in surgical procedures involving the T3 and T4 sympathetic nerves in isolated palmar hyperhidrosis. Especially in the meta-analyses performed by Zhang et al. [6], postoperative quality of life and surgical success rates were higher in patients who underwent T4 sympathectomy compared with T3 sympathectomy. They also reported that resection of lower level ganglia reduced complications. However, Ellatif et al. [7] reported that the satisfaction rates were similar in lower level resections, and rates of palmar dryness decreased. They determined that palmar dryness was less common among those who underwent sympathectomy at the T4 compared with the T3 level. In contrast, Deng et al. [8] found in their meta-analysis that the surgical success rate was high, and the rate of CH was low in sympathectomies performed at the T3 and T3–T4 levels. Another meta-analysis by Cerfolio et al. [5] showed that cutting the T3 sympathetic nerve was optimal in patients with palmar hyperhidrosis. However, cutting both the T3 and T4 sympathetic nerves increases the surgical success rate. Although the risk of CH increases with T3 sympathectomy, isolated T4 sympathectomy does not provide an adequate reduction in palmar sweating [5] (Table 4).
Consistent with the literature, we had greater surgical success with isolated T3 and T3–T4 sympathectomies than with T2–T4 sympathectomies. However, in contrast to the literature, our success rate was higher in isolated T3 sympathectomies than in T3–T4 sympathectomies, despite similar long-term quality of life scores in both groups.
In 2009, Yazbek et al. [2] reported better results with T3 than with T2. After this publication, some surgeons in our hospital avoided cutting the T2 sympathetic nerve. In our study, the most important reason for having more than one surgical level and technique stems from the presence and preferences of more than one surgeon. Some surgeons prefer to use the clip method because they believe this technique is reversible in the event of CH.
Yanagihara et al. [19] reported that CH could not be prevented in either clipping or cauterization procedures, postoperative patient satisfaction levels were very good, and there was no significant difference between the two methods. Similarly, in our study, we observed no significant differences between clipping and cauterization in terms of quality of life, CH, or early postoperative complications.
Although there are many studies in the literature on video-assisted thoracoscopic surgery (VATS) sympathectomy, very few studies have evaluated the preoperative and postoperative quality of life. We believe that quality of life is a more important outcome measure than CH or postoperative complications. In this study, patients who underwent ETS reported high postoperative quality of life, even in the presence of CH. In addition, when postoperative quality of life was evaluated in terms of surgical level, there was a significant difference in postoperative quality of life between patients who underwent T2–T4 sympathectomy and those who underwent T3–T4 and T3 sympathectomy; patients who had T2 sympathectomy reported much poorer quality of life. Postoperative quality of life tended to be higher among patients who underwent T3 sympathectomy when compared with those who underwent T3–T4 sympathectomy, but the difference was not statistically significant. Dharmaraj et al. [20] compared pre- and postoperative quality of life in 50 patients who underwent ETS and reported a significant change in the quality of life postoperatively. In a 2012 study, Wolosker et al. [21] evaluated the quality of life of 453 patients who underwent ETS at 30 days postoperatively and at 5 years and found that quality of life was as good at 5 years as after the first month. In 2016, Menna et al. [22] conducted a study of 216 patients with axillary and palmar hyperhidrosis and also concluded that long-term postoperative quality of life of patients was comparable to the short-term quality of life. In these studies, CH and recurrence were the main factors affecting the postoperative quality of life. In addition, most studies on quality of life did not include a comparative evaluation of sympathectomy surgical level and long-term quality of life.
Limitations
The main limitations of the study are its retrospective design. The presence of more than one surgeon and performing different procedures according to the preferences of these surgeons create bias in the study.
Conclusion
Our findings indicate that postoperative quality of life was lower and CH was higher in patients with palmar hyperhidrosis who underwent T2 sympathectomy compared with those who underwent T3 and T3–4 sympathectomies. Based on our results, we recommend performing lower level resections to increase the long-term quality of life in these patients. Unlike previous studies, we observed a lower rate of CH among patients who underwent T3 sympathectomy than those who underwent T3–T4 sympathectomy. However, long-term quality of life was similar at both levels. The lower risk of CH and comparable quality of life suggest that T3 sympathectomy is more effective. However, this should be corroborated with large, prospective randomized studies on this subject.
References
Sezen CB, Akboğa SA, Süleymanov A, Gökçe A, Çelik A, Kurul İC. Is oxybutynin treatment as effective as surgery in palmar and axillary hyperhidrosis? Haseki Tip Bul. 2017;55:199.
Yazbek G, Wolosker N, Kauffman P, de Campos JRM, Puech-Leão P, Jatene FB. Twenty months of evolution following sympathectomy on patients with palmar hyperhidrosis: sympathectomy at the T3 level is better than at the T2 level. Clinics. 2009;64:743–9.
Amir M, Arish A, Weinstein Y, Pfeffer M, Levy Y. Impairment in quality of life among patients seeking surgery for hyperhidrosis (excessive sweating): preliminary results. Isr J Psychiatry Relat Sci. 2000;37:25.
Lin M, Tu YR, Li X, Lai FC, Chen JF, Dai ZJ. Comparison of curative effects of sympathectomy at different segments on palmar hyperhidrosis. Zhonghua Yi Xue Za Zhi. 2006;86:2315–7.
Cerfolio RJ, De Campos JRM, Bryant AS, Connery CP, Miller DL, DeCamp MM, et al. The society of thoracic surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg. 2011;91:1642–8.
Zhang W, Yu D, Wei Y, Xu J, Zhang X. A systematic review and meta-analysis of T2, T3 or T4, to evaluate the best denervation level for palmar hyperhidrosis. Sci Rep. 2017;7:1–9.
Abd Ellatif ME, El Hadidi A, Musa AM, Askar W, Abbas A, Negm A, et al. Optimal level of sympathectomy for primary palmar hyperhidrosis: T3 versus T4 in a retrospective cohort study. Int J Surg. 2014;12:778–82.
Deng B, Tan Q-Y, Jiang Y-G, Zhao Y-P, Zhou J-H, Ma Z, et al. Optimization of sympathectomy to treat palmar hyperhidrosis: the systematic review and meta-analysis of studies published during the past decade. Surg Endosc. 2011;25:1893–901.
Yazbek G, Wolosker N, de Campos JRM, Kauffman P, Ishy A, Puech-Leão P. Palmar hyperhidrosis—which is the best level of denervation using video-assisted thoracoscopic sympathectomy: T2 or T3 ganglion? J Vasc Surg. 2005;42:281–5.
Lee DY, Kim DH, Paik HC. Selective division of T3 rami communicantes (T3 ramicotomy) in the treatment of palmar hyperhidrosis. Ann Thorac Surg. 2004;78:1052–5.
Jie Y, Tan J, Ye G, Gu W, Jun W, Liu Y. T3/T4 thoracic sympathectomy and compensatory sweating in treatment of palmar hyperhidrosis. Chin Med J. 2007;120:1574–7.
Chang Y-T, Li H-P, Lee J-Y, Lin P-J, Lin C-C, Kao E-L, et al. Treatment of palmar hyperhidrosis: T4 level compared with T3 and T2. Ann Surg. 2007;246:330.
Wolosker N, Yazbek G, Ishy A, De Campos JRM, Kauffman P, Puech-Leao P. Is sympathectomy at T4 level better than at T3 level for treating palmar hyperhidrosis? J Laparoendosc Adv Surg Tech. 2008;18:102–6.
Li X, Tu Y-R, Lin M, Lai F-C, Chen J-F, Dai Z-J. Endoscopic thoracic sympathectomy for palmar hyperhidrosis: a randomized control trial comparing T3 and T2–4 ablation. Ann Thorac Surg. 2008;85:1747–51.
Kim WO, Kil HK, Yoon KB, Yoon DM, Lee JS. Influence of T3 or T4 sympathectomy for palmar hyperhidrosis. Am J Surg. 2010;199:166–9.
Ishy A, Ribas Milanez De Campos J, Wolosker N, Kauffman P, Tedde ML, Chiavoni CR, et al. Objective evaluation of patients with palmar hyperhidrosis submitted to two levels of sympathectomy: T3 and T4. Interact CardioVasc Thorac Surg. 2011;12:545–9.
Fiorelli A, D’Aponte A, Canonico R, Palladino A, Vicidomini G, Limongelli F, et al. T2–T3 sympathectomy versus sympathectomy for essential palmar hyperhidrosis: comparison of effects on cardio-respiratory function. Eur J Cardio Thorac Surg. 2012;42:454–61.
Joo S, Lee GD, Haam S, Lee S. Comparisons of the clinical outcomes of thoracoscopic sympathetic surgery for palmar hyperhidrosis: R4 sympathectomy versus R4 sympathetic clipping versus R3 sympathetic clipping. J Thorac Dis. 2016;8:934–41.
Yanagihara TK, Ibrahimiye A, Harris C, Hirsch J, Gorenstein LA. Analysis of clamping versus cutting of T3 sympathetic nerve for severe palmar hyperhidrosis. J Thorac Cardiovasc Surg. 2010;140:984–9.
Dharmaraj B, Kosai NR, Gendeh H, Ramzisham AR, Das S. A prospective cohort study on quality of life after endoscopic thoracic sympathectomy for primary hyperhidrosis. Clin Ter. 2016;167:67–71.
Wolosker N, De Campos JRM, Kauffman P, De Oliveira LA, Munia MAS, Jatene FB. Evaluation of quality of life over time among 453 patients with hyperhidrosis submitted to endoscopic thoracic sympathectomy. J Vasc Surg. 2012;55:154–6.
Menna C, Ibrahim M, Andreetti C, Ciccone AM, D’Andrilli A, Maurizi G, et al. Long term compensatory sweating results after sympathectomy for palmar and axillary hyperhidrosis. Ann Cardiothorac Surg. 2016;5:26–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest related to this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dogru, M.V., Sezen, C.B., Girgin, O. et al. Is there any relationship between quality of life and the level of sympathectomy in primary palmar hyperhidrosis? Single-center experience. Gen Thorac Cardiovasc Surg 68, 273–279 (2020). https://doi.org/10.1007/s11748-019-01210-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-019-01210-7