Abstract
Objectives
Postoperative disorders of the central nervous system remain a major problem in thoracic aortic surgery. Both retrograde cerebral perfusion and selective antegrade cerebral perfusion have become established techniques for cerebral circulatory management. In this study, we compared neurologic outcomes and mortality between retrograde cerebral perfusion and antegrade selective cerebral perfusion in patients with acute type A aortic dissection who underwent emergency ascending aorta replacement.
Methods
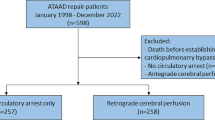
Between January 2003 and April 2011, a total of 203 patients with acute type A aortic dissection underwent emergency ascending aorta replacement in our hospital. We performed retrograde cerebral perfusion in 109 patients before 2006, and then mainly performed antegrade selective cerebral perfusion in 94 patients from 2006 onward.
Results
Cardiopulmonary bypass time and systemic circulatory arrest time were significantly longer in the antegrade selective cerebral perfusion group (p = 0.04, p < 0.001, respectively). The incidences of transient brain dysfunction and permanent brain dysfunction after surgery did not differ significantly between the groups. There were also no differences between the groups in other intraoperative variables, such as aortic cross-clamp time and the lowest rectal temperature, or in operative outcomes, including postoperative intensive-care-unit stay, mean peak amylase, and lipase levels until postoperative day 7, and 30-day mortality.
Conclusion
Both retrograde cerebral perfusion and antegrade selective cerebral perfusion were associated with acceptable levels of postoperative neurologic deficits, mortality, and morbidity. Either of these techniques for brain protection can be used selectively, based on a comprehensive assessment of general condition, in patients undergoing surgery for acute type A aortic dissection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Considerable progress has recently been made in brain protection during thoracic aortic surgery. However, postoperative disorders of the central nervous system remain a major problem. Before 2006, we performed retrograde cerebral perfusion (RCP) with moderate hypothermic circulatory arrest (MHCA) in patients with acute type A aortic dissection, who underwent ascending aorta replacement. Since 2006, we have mainly used selective antegrade cerebral perfusion (SCP) with MHCA. Recently, patients who undergo thoracic aortic surgery are becoming older, and severe atherosclerotic lesion is detected in such elderly patients. It is supposed that RCP is appropriate to the patients with severe atherosclerotic lesion in aortic arch because it does not need cannulation to the neck vessels. Therefore, we can select RCP or SCP according to the patient’s condition. In this study, we compared neurologic outcomes and mortality between RCP and SCP in patients who underwent emergency ascending aorta replacement for acute type A aortic dissection.
Patients and methods
From January 2003 through April 2011, a total of 203 patients with acute type A aortic dissection underwent emergency ascending aorta replacement in our hospital. We performed RCP with MHCA before 2006. Since 2006, we have mainly performed SCP with MHCA. RCP was performed in 109 patients and SCP in 94. All the patients underwent emergency surgery. The study was approved by our Institutional Human Research Ethics Committee. The need for individually obtaining informed consent from patients whose records were evaluated was waived because individuals were not identified in this study.
The cannulation sites for arterial return were femoral artery and right subclavian artery regardless the brain protection was RCP or SCP. RCP was performed under the following conditions. The patient was cooled to a rectal temperature of 25 °C before systemic circulatory arrest. RCP was maintained at a flow rate of about 200 ml/min, with a perfusion pressure of about 40 mmHg. After distal anastomosing to the ascending aorta, antegrade cerebral and body perfusion was resumed through the side branch of the graft and rewarming was started. For SCP, the patients were cooled to a rectal temperature of 27 °C. Cerebral perfusion was initiated with a balloon-tipped cannula inserted directly in the brachiocephalic artery, the left common carotid artery, and the left subclavian artery from inside the aortic arch at a flow rate of 10 ml/kg/min and then adjusted to maintain a perfusion pressure between 40 and 60 mmHg.
Peak levels of amylase and lipase were measured until postoperative day (POD) 7 to evaluate visceral perfusion during circulatory arrest. Transient brain dysfunction and permanent brain dysfunction were also assessed. Transient brain dysfunction was defined as symptoms that resolved before discharge from the hospital, such as restlessness, disorientation, and delirium. Permanent brain dysfunction included brain infarction and hypoxic encephalopathy detected by brain CT. All neurologic deficits occurred after surgery. We excluded one patient in RCP group and three patients in SCP group, who had brain dysfunction before surgery. One patient in RCP group had disturbance of consciousness. Three patients in SCP group included two patients who had disturbance of consciousness and one patient who had brain infarction.
Statistical analysis was conducted using Dr. SPSS II (SPSS, Chicago, IL, USA). Numerical values are expressed as mean ± SD. Fisher’s exact test was used to compare differences in categorical variables between the two techniques. Independent t tests were used to compare differences in numerical variables between techniques.
Results
Among the 109 patients in the RCP group, 101 underwent ascending aorta replacement, and eight underwent ascending aorta and aortic root replacement. Of the 94 patients in the SCP group, 85 underwent ascending aorta replacement, and nine underwent ascending aorta and aortic root replacement. Mean age was 65.6 ± 11.7 years in the RCP group and 67.2 ± 9.3 years in the SCP group (p = 0.37). Fifty-three patients (49 %) were male in the RCP group, and 45 (48 %) were male in the SCP group (p = 0.54) (Table 1).
Outcomes are summarized in Table 2. Cardiopulmonary bypass time (RCP 211 ± 51, SCP 229 ± 72 min; p = 0.04) and systemic circulatory arrest time (RCP 53 ± 16, SCP 65 ± 15 min; p < 0.001) were significantly longer in the SCP group. Aortic cross-clamp times (RCP 172 ± 42, SCP 176 ± 48 min; p = 0.55) were similar. The lowest rectal temperature was 23.7 ± 1.1 °C in the RCP group and 25.6 ± 1.2 °C in the SCP group (p < 0.001). The postoperative intensive-care-unit (ICU) stay was 5.4 ± 5.4 days in the RCP group and 6.0 ± 5.3 days in the SCP group (p = 0.43). The mean peak amylase level up to POD 7 was 374 ± 351 U/l in the RCP group and 375 ± 389 U/l in the SCP group (p = 0.98). The mean peak lipase level up to POD 7 was 160 ± 273 U/l in the RCP group and 146 ± 194 U/l in the SCP group (p = 0.70). Forty-one patients (38 %) had transient brain dysfunction in the RCP group as compared with 32 (34 %) in the SCP group (p = 0.66). Permanent brain dysfunction developed in 10 patients (9 %) in the RCP group and 11 (12 %) in the SCP group (p = 0.65). Head CT findings of the patients with permanent brain dysfunction in the RCP group included brain infarction in eight patients and hypoxic encephalopathy in two patients, and all of the 11 patients with permanent brain dysfunction in the SCP group had brain infarction. All of the patients who had transient neurologic deficit obtained full recovery. Some of the patients who had permanent neurologic deficit obtained full or partial recovery. Seven patients (6 %) in the RCP group and 2 (2 %) in the SCP group died within 30 days after operation (p = 0.18). The causes of deaths were as follows: In the RCP group, due to brain infarction were two; and due to intestinal necrosis, myonephropathic metabolic syndrome, toxic epidermal necrolysis, disseminated intravascular coagulation, and respiratory insufficiency was one each. In the SCP group, the causes of deaths were brain infarction and intestinal necrosis.
Discussion
Despite progress in techniques for brain protection and cardiopulmonary bypass, brain-related complications remain major causes of mortality and morbidity after thoracic aortic surgery [1]. Okita et al. reported that RCP was associated with a significantly higher prevalence of transient brain dysfunction than SCP in patients who underwent total arch replacement [2]. In our study, neurologic outcomes, transient brain dysfunction, permanent brain dysfunction, and other postoperative variables did not differ significantly between these two techniques. Only cardiopulmonary bypass time and systemic circulatory arrest time were significantly longer in SCP group.
Several studies have demonstrated that the most permanent neurologic deficits after aortic surgery are caused by embolic phenomena and are not directly related to the technique used for cerebral protection [3, 4]. In contrast, temporary neurologic dysfunction is more closely related to global ischemia and a longer cerebral ischemic time. The incidence of temporary neurologic dysfunction has been shown to correlate with the duration of cerebral perfusion management [5, 6]. In our study, temporary neurologic dysfunction was defined as symptoms that resolved before discharge from the hospital, such as restlessness, disorientation, and delirium. There was no difference in temporary neurologic dysfunction between the RCP group and SCP group in our study, suggesting that both techniques provide acceptable cerebral outcomes in patients with acute type A dissection, who undergo ascending aorta replacement. The technique best suited to the individual patient can therefore be selected. Patients who had severe atheromatous plaque in the aortic arch could occur brain infarction by SCP cannulation easily. Therefore, we use RCP in such patients recently.
Systemic circulatory arrest can have adverse visceral outcomes [7], including ischemic pancreatitis or postoperative renal insufficiency. MHCA can also increase visceral ischemic time, causing adverse visceral outcomes. Peak serum levels of amylase and lipase were measured as indicators of ischemic pancreatitis in our study. Mean peak amylase and lipase levels up to POD 7 did not differ significantly between the groups, although circulatory arrest time was significantly longer in the SCP group. Our findings suggest that there was no significant difference in pancreatic ischemia after surgery between the RCP and SCP groups. Milewski et al. reported no significant difference in the development of postoperative renal insufficiency between RCP with deep hypothermic circulatory arrest and SCP with MHCA [8]. One advantage of MHCA has been suggested to be the avoidance of hypothermic temperatures, allowing shorter cardiopulmonary bypass times and potentially reducing the risk of coagulopathy [7].
Several previous studies have evaluated postoperative neurologic deficits in patients who underwent surgery for acute type A dissections. Bavaria et al. found that cerebrovascular accidents developed in 3 % of patients after dissection repair [9]. Bakhtiary et al. reported that new postoperative permanent neurologic deficits occurred in 5 (4.2 %) of 120 consecutive patients who underwent SCP during repair of acute type A dissections [10]. As compared with the results of these previous studies, the incidence of permanent neurologic deficits was higher in our study (i.e., about 10 % in the both the RCP and SCP groups).
In conclusion, both RCP and SCP were associated with acceptable levels of postoperative neurologic deficits, mortality, and morbidity. Either of these techniques for brain protection can be used selectively, based on a comprehensive assessment of general condition, in patients undergoing surgery for acute type A aortic dissection.
References
Usui A, Miyata H, Ueda Y, Motomura N, Takamoto S. Risk-adjusted and case-matched comparative study between antegrade and retrograde cerebral perfusion during aortic arch surgery: based on the Japan adult cardiovascular surgery database : the Japan cardiovascular surgery database organization. Gen Thorac Cardiovasc Surg. 2012;60:132–9.
Okita Y, Minatoya K, Tagusari O, Ando M, Nagatsuka K, Kitamura S. Prospective comparative study of brain protection in total aortic arch replacement: deep hypothermic circulatory arrest with retrograde cerebral perfusion or selective antegrade cerebral perfusion. Ann Thorac Surg. 2001;72:72–9.
Hagl C, Ergin MA, Galla JD, Lansman SL, McCullough JN, Spielvogel D, et al. Neurologic outcome after ascending aorta-aortic arch operations: effect of brain protection technique in high-risk patients. J Thorac Cardiovasc Surg. 2001;121:1107–21.
Griepp RB. Cerebral protection during aortic arch surgery. J Thorac Cardiovasc Surg. 2001;121:425–7.
Khaladj N, Shrestha M, Meck S, Peterss S, Kamiya H, Kallenbach K, et al. Hypothermic circulatory arrest with selective antegrade cerebral perfusion in ascending aortic and aortic arch surgery: a risk factor analysis for adverse outcome in 501 patients. J Thorac Cardiovasc Surg. 2008;135:908–14.
Ergin MA, Uysal S, Reich DL, Apaydin A, Lansman S, McCullough JN, et al. Temporary neurological dysfunction after deep hypothermic circulatory arrest: a clinical marker of long-term functional deficit. Ann Thorac Surg. 1999;67:1887–90.
Kamiya H, Hagl C, Kropivnitskaya I, Bothig D, Kallenbach K, Khaladj N, et al. The safety of moderate hypothermic lower body circulatory arrest with selective cerebral perfusion: a propensity score analysis. J Thorac Cardiovasc Surg. 2007;133:501–9.
Milewski RK, Pacini D, Moser W, Moeller P, Cowie D, Szeto WY, et al. Retrograde and antegrade cerebral perfusion: results in short elective arch reconstructive times. Ann Thorac Surg. 2010;89:1448–57.
Bavaria JE, Brinster DR, Gorman RC, Woo YJ, Gleason T, Pochettino A. Advances in the treatment of acute type A dissection: an integrated approach. Ann Thorac Surg. 2002;74:1848–52.
Bakhtiary F, Dogan S, Zierer A, Dzemali O, Oezaslan F, Therapidis P, et al. Antegrade cerebral perfusion for acute type A aortic dissection in 120 consecutive patients. Ann Thorac Surg. 2008;85:465–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sugiura, T., Imoto, K., Uchida, K. et al. Comparative study of brain protection in ascending aorta replacement for acute type A aortic dissection: retrograde cerebral perfusion versus selective antegrade cerebral perfusion. Gen Thorac Cardiovasc Surg 60, 645–648 (2012). https://doi.org/10.1007/s11748-012-0142-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-012-0142-z