Abstract
From October 2000 to August 2012, 232 consecutive patients with acute type A aortic dissection had surgery (mean age: 66.3 ± 13.0, 21–96). All patients had surgery on an emergency or urgent basis. Thirty-four were in shock status and five required percutaneous assisted circulation. A cardiac tamponade was detected in 53 patients and a moderate or severe aortic regurgitation in 34 patients. Forty-six (19.8 %) had neurological symptom consisting with coma in 4, stroke in 12, TIA in 28, and paraplegia in 2. Fourteen patients had coronary malperfusion, 11 had visceral malperfusion, and 33 had leg malperfusion. The extent of the aortic replacement was ascending aorta in 4, hemiarch in 141, total arch in 84, total arch to descending aorta in 2, and TEVAR in 1. Aortic valve resuspension or valve repair was performed in 207, root replacement with valve sparing in 22, and Bentall procedure in 4. Brain protection was achieved by deep hypothermic circulatory arrest with or without retrograde cerebral perfusion in 78, and antegrade selective cerebral perfusion in 150. The overall hospital mortality was 13.4 % (31/232). Newly developed permanent neurological deficits occurred in 2.7 % (5/186) of patients and transient neurological dysfunction (TND) occurred in 1.6 % (3/186). There was no difference in incidence of hospital death, stroke and TND between the DHCA and ACP group also between the patients who had a hemiarch or a total arch replacement.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute aortic dissection
- Brain protection
- Antegrade selective cerebral perfusion
- Near infrared spectroscopy
- Malperfusion
Introduction
Recent advances in surgery for the aortic arch are becoming widely recognized. This achievement has been attributed to the development of water-sealed grafts, the evolution of cardiopulmonary bypass techniques and equipment, better understanding regarding brain protection, and refinement of the surgical procedures. Precise diagnosis of aortic disease has provided recruitment of patients with chest pain to the earlier surgery for aortic dissection. According to a survey by the Japanese Association for Thoracic Surgery, since 1984 the annual number of operations for the aortic dissection, has steadily increased from 519 in 1984 to 5,376 in 2010 [1]. However, The 30 day mortality for acute type A aortic dissection in 2000 was reported to be 18.4 % (350/1,901) and was 14.2 % (335/3,628) in 2010, on the other hand, the 30 day mortality after the aortic arch surgery in 2000 was 8.9 % (55/616) comparing with 3.5 % (72/2,073) in the 2010 data of the Japanese registry (Fig. 26.1) [2, 3]. Thus the improvement of surgical results for acute aortic dissection is inferior to the aortic arch surgery. Main reasons are considered as increase of the patients with complicated condition, such as end organ malperfusion, including preoperative brain complications and with other critical conditions. The purpose of this report is to describe our strategy and results of surgery for acute type A aortic dissection, mainly focusing the brain protection. This study was approved by our Institutional Review Board, and the need for individual consent was waived.
Patients and Methods
From October 2000 to August 2012, 275 consecutive patients with acute type A aortic dissection were admitted in our hospital and 43 had medical treatment because of medical (completely thrombosed false lumen) or personal reasons (Tables 26.1 and 26.2). Every patient had preoperative CT scan and carotid scan. Two hundreds and thirty-two patients underwent surgery (mean age: 66.3 ± 13.0, 21–96). Thirty-four patients (14.7 %) were octogenarian or nonagenarian. All patients had surgery on emergency or urgent basis. Thirty-four (14.7 %) were in shock status and five required percutaneous assisted circulation. A cardiac tamponade was detected in 53 patients (22.8 %). Salvage surgery, such as cardiopulmonary resuscitation or percutaneous circulatory support because of hemodynamic instability, was performed in 15 patients (6.4 %). On the other hand, two patients had “delayed surgery” because of preoperative large stroke or cerebral bleeding (Fig. 26.2). Organ malperfusion was detected in 89 (38.4 %) patients. Forty-six (19.8 %) had neurological symptom consisting with coma in 4, stroke in 12, TIA in 28, and paraplegia in 2 (Figs. 26.3 and 26.4). One patient with left hemiplegia had preoperative selective perfusion of the right common carotid artery from the right femoral artery was performed and she survived (Figs. 26.5 and 26.6). Fourteen patients had coronary malperfusion, 11 had visceral malperfusion and 33 had leg malperfusion. Fifteen patients had two or more organ malperfusion. A moderate or severe aortic regurgitation was detected in 34 patients (14.6 %). There were 8 patients with Marfan syndrome and 14 patients had chronic kidney disease (serum creatinine > 2.0 mg/dl). Two hundreds and thirteen patients (91.8 %) had patent false lumen and 19 (8.2 %) had thrombosed false lumen. The entry sites were aortic root in 6 (2.6 %), ascending aorta in 143 (61.6 %), aortic arch in 40 (17.2 %), proximal descending aorta in 23 (9.9 %), and undetected in 20 (8.6 %).
Postoperative CT scan of the patient in Fig. 26.5 showed a large infarction but minimum brain edema. She regained consciousness and went home. POD postoperative day
Surgical Procedures
Patients were placed in the supine position and the diodes of the NIRS were attached on the foreheads bilaterally. For NIRS, we used the INVOS 5100C (Somanetics, Troy, MI), which provides continuous readings of the regional cerebral oxygen saturation (rSO2). The rSO2 readings are expressed as an index, measuring differences from an unknown baseline. Before being placed on the cardiopulmonary bypass, the innominate vein was fully mobilized by dividing several branches to facilitate the exposure of the aneurysm. Dissection of the aortic arch was limited only within the anterior aspect of the aortic arch and the left vagal nerve should not be dissected. In addition, dissection or taping of the arch vessels is not necessary.
Epi-aortic echo scanning was performed in every case. Preoperative CT scanning was done for every patient to assess the atheromatous or thrombosis of the false lumen in the ascending aorta. Both transesophageal and epi-aortic echography were applied to interrogate the ascending aorta and determine the optimal cannulation site. Single arterial cannulation was used in 212 patients (91.3 %), where the femoral artery was used in 173 patients (81.6 %), ascending aorta in 25 (11.8 %), and axillary artery in 14 (6.6 %). Double arterial inflow was applied to prevent or to mitigate organ malperfusion in 20 patients (8.7 %), consisted with femoral artery + ascending aorta in 8, femoral and axillary artery in 10, femoral artery plus left ventricular apex in 1 and ascending aorta and axillary artery in 1 (Table 26.3). For the ascending aorta cannulation, a 20 Fr arterial cannula (Duraflo II, Edwards Lifesciences LLC, Irvine, CA) with the Seldinger method was exclusively used.
The extent of the aortic replacement was ascending aorta in 4 (1.6 %), hemiarch in 145 (62.5 %), total arch in 84 (36.2 %), total arch to descending aorta in 2 (0.9 %), and TEVAR in 1 (0.4 %) (Table 26.4). Our indication for total arch replacement for acute type A aortic dissection have been (1) arch tear, (2) tear in the descending aorta, (3) Marfan patients, (4) young patients with uncomplicated dissection, and (5) arch rupture. Aortic valve resuspension or valve repair was performed in 207 (89.2 %), root replacement with valve sparing in 22 (9.5 %), and Bentall procedure in 4 (1.7 %). Our indications for root replacement have been applied in patients with the initial entry in the aortic root and with pre-existing annulo-aortic ectasia. A sealed graft (J graft. Japan Lifeline, Tokyo or Triplex, Terumo Corporation, Tokyo, Japan) were exclusively used. The four-branched (10 mm, 8 mm, 8 mm, 8 mm) were used in every patient who had the total arch replacement and each arch vessel was reconstructed individually. The aorta was always transected and external reinforcement of the anastomosis by the Teflon felt has been always used. The Gelatin – Resorcin – Formalin (GRF) glue or Bio-glue was usually used to obliterate proximal false lumen in the aortic root, but never used to the distal anastomosis of the hemiarch grafting. Additional procedures consisted with CABG in seven, Maze procedure in four and mitral valve repair in two.
Brain Protection
Brain protection was achieved by deep hypothermic circulatory arrest with or without retrograde cerebral perfusion in 78 (64.7 %), antegrade selective cerebral perfusion in 150 (33.6 %), and distal aortic clamping in 4 (1.7 %) (Table 26.4). Monitoring of the blood pressure in the both extremities and rSO2 during cardiopulmonary bypass was used. When a significant laterality of the blood pressure or rSO2 occurred, additional arterial inflow cannula was introduced immediately and liberally as described. Patients’ head was packed with cold ice jacket. Myocardial protection was achieved by antegrade or retrograde cardioplegia.
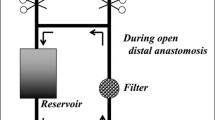
When the antegrade cerebral perfusion method was applied, the patient was cooled down to 23 °C in the tympanic temperature and below 30 °C in the rectal temperature. Circulatory arrest was done and the aortic arch was opened. A 14 or 16 Fr self-inflating serrated-balloon-tipped cannula (Fuji systems, Tokyo) was inserted from inside the aorta into the brachiocephalic artery, and 12 Fr cannulae were positioned in the left common carotid and left subclavian arteries. Snaring the neck vessels was not necessary. The antegrade ACP flow was maintained at 10–12 mL/kg/min using single independent roller pump, and the balloon tip pressure was maintained between 30 and 40 mmHg. After finishing the distal anastomosis, the lower body circulation was reinstituted through one branch of the graft, and the whole body rewarming was started. Coincident with re-warming, the antegrade ACP flow was gradually increased while maintaining the baseline values of rSO2. However, the antegrade ACP flow was limited to below 1,200 mL/min to prevent brain edema. The proximal anastomosis was then accomplished and coronary reperfusion was started, and defibrillation of the heart was done if necessary. The aortic arch was divided to make the arch vessel buttons and the arch vessels were reconstructed tandem to the graft branches [4].
When the deep hypothermic circulatory arrest with/without retrograde cerebral perfusion was applied, the tympanic temperature was kept below 20 °C during the distal anastomosis. The retrograde cerebral perfusion was achieved through the superior vena cava at 300 ml/min flow and was controlled not to exceed 20 mmHg at the SVC pressure [5].
Definition of Neurological Deficits
Permanent neurological dysfunction was defined as the presence of deficits that persisted at discharge, which were caused by an intraoperative procedure. Transient dysfunction was defined as the transient loss of orientation, slurred language, agitation, or a poor response to commands. Neurological dysfunction caused by preoperative brain malperfusion associated with the acute type A dissection, deep shock status or postoperative atrial fibrillation were excluded from this category [6]. Brain malperfusion was defined as cerebral blood flow disturbance secondary to acute aortic dissection involving aortic arch branches with newly developed stroke, TIA, or consciousness disorder.
Statistical Analysis
Data were processed using the Stat View J-5.0 software program (SAS Institute, Cary, NC). Continuous values are expressed as the means ± standard deviation. The data were analyzed by the Chi-squared test for categorical variables. A stepwise logistic regression analysis was performed to identify the risk factors for hospital mortality, PND and TND. Clinically relevant variables with p <0.05 in the univariate analysis were incorporated into the multivariate models. Survival and freedom from aortic aneurysm-related death were assessed by the Kaplan-Meier method. Differences were considered to be statistically significant at p < 0.05.
Results
CPB time was 208.6 ± 75.2 (99–546) min and myocardial ischemic time was 119.3 ± 48.2 (38–272) min. Mean cerebral perfusion time was 86.0 ± 51.8 min and circulatory arrest time of the lower body was 47.9 ± 31.4 min with ACP and brain circulatory arrest time was 27.7 ± 14.5 min with DHCA. The overall hospital mortality was 13.4 % (31/232) and it was 60.0 % (9/15) in salvage cases, 17.9 % (16/89) with organ malperfusion, and 21.7 % (10/46) with brain malperfusion. The causes of deaths were low cardiac output in 11, central nervous system in 8, necrosis of the intestine in 4, mediastinitis in 4, DIC 1, acute renal failure 1, aortic rupture 1, drug allergy 1, esophageal varices bleeding in 1, and asphyxia in 1. Among them, 14 patients were in preoperative shock state and 4 required percutaneous circulatory support. Preoperative malperfusion was recognized in coronary artery in four, brain in eight, superior mesenteric artery in two, and leg in one. Four patients were in coma state, three had stroke, and three had TIA (Table 26.5). Overall neurological dysfunction occurred in 32/232 (13.8 %) patients.
New permanent neurological deficits (PND), excluding 46 patients who had preoperative neurological disorder due to brain malperfusion, occurred in 2.7 % (5/186) of patients and transient neurological disorder (TND) occurred in 1.6 % (3/186). The hospital mortality of patients with preoperative neurological deficit was 21.7 % (10/46) and all four comatose patients died during hospitalization. The hospital mortalities of patients with preoperative stroke and TIA were 25.0 % (3/12) and 10.7 % (3/28) respectively. No patients with preoperative paraplegia died (Table 26.5). Both two patients who had delayed surgery because of cerebral problems survived. All four patients with preoperative coma never recovered. Among 12 patients with preoperative stroke, 2 had brain death, 1 died of mediastinitis, 1 had a worsening motor deficit, 6 recovered with some deficit, and 2 were unchanged neurologically. In 28 preoperative TIA patients, 1 had brain death, 2 died of mediastinitis and asphyxia, 3 was sent to nursing home due to neurological deterioration, 22 was neurologically normal. Three patients had a stroke secondary to postoperative atrial fibrillation and another 3 patients had newly developed paraplegia postoperatively.
In patients who had TAR the hospital mortality, PND, and TND were 8.3 % (7/84), 2.4 % (2/84), and 2.4 % (2/84), respectively and in the hemiarch patients, they were 14.6 % (21/144), 2.1 % (3/144), and 0.7 % (1/144), respectively. As for brain protection, the hospital mortality, PND, and TND in patients who had ACP were 10.7 % (16/150), 2.0 % (3/150), and 2.0 % (3/150), respectively and in the DHCA patients, they were 16.7 % (13/78), 2.6 % (2/78), and zero, respectively (Table 26.4). There was no significant difference incidence of 30-day death, stroke and TND between the DHCA and ACP group also between the patients who had a hemiarch replacement or a total arch replacement. A multivariate analysis demonstrated the risk factors for hospital mortality to be age, preoperative serum creatinine > 2.0 mg/dl, preoperative shock, coma or stroke, visceral malperfusion, and CPB time. Age, extent of aortic replacement were not risk factors for hospital mortality (Table 26.6). The multivariate analysis disclosed that preoperative coma or stroke was only risk factor for postoperative PND. Age, extent of aortic replacement, method of brain protection, CPB time were not proven to be risk for postoperative PND (Table 26.7). A transient neurological deficit (TND) occurred in 37 patients (8.7 %) following surgery, however, no variable was proved to be risk even by univariate analysis.
The follow-up was completed in 96.5 % of patients (mean 51.6 ± 38.4, 1–153 months). The survival, excluding the hospital mortality, at 5 and 10 years after surgery was 85.5 ± 3.0 % and 80.1 ± 5.0 %, respectively. Late death occurred in 25 patients, and the causes of death were pneumonia in 10, cardiac events in 3, cerebrovascular in 2, aorta-related in 2, malignancy in 2, and others (gastrointestinal, renal failure, accident, unknown) in 6. There were only two patients who died from aorta-related events during the follow-up period. The causes of death were rupture of the thoracoabdominal aortic aneurysm 8 years after hemiarch replacement and the other patient died of pneumonia after redo-surgery for aortic regurgitation. A multivariate analysis demonstrated the risk factors for late mortality to be age, preoperative shock, and postoperative neurological complications. Preoprative organ malperfusion, serum creatinine value, extent of aortic replacement, and brain protection method were not risk factors for late death (Table 26.8).
Twenty-seven patients required reoperations during follow-up. Proximal reoperation was necessary in 17 patients due to aortic regurgitation in 12, infective endocarditis in 3, hemolysis in 1, and false aneurysm in 1. Distal reoperation was done in 13 patients, consisted of total arch replacement in 7, descending aorta replacement in 1, replacement of the thoracoabdominal aorta in 3, replacement of infected elephant trunk in 1, and TEVAR in 1. Three patients needed reoperation due to tear in the brachiocephalic artery and resultant enlargement of the false lumen of the arch. Freedom from reoperation was 82.7 ± 3.6 % at 5 years and 73.4 ± 5.1 % at 10 years.
Discussion
Surgical results for acute aortic dissection have improved for a decade, however, not so much as the dramatic evolution of other fields in cardiac surgery, which was driven by OPCAB, valve repair, TAVR, and stent grafting. Population based study in the US 3,013 patients demonstrated that in hospital mortality has improved, but it was still over 20 % in 2003 [7]. Main reasons for this dawdling have been attributed to aortic rupture and organ malperfusion secondary to aortic or branch stenosis. Incidence of the malperfusion has been reported as 20–40 % and the patients’ outcome became worse than those without malperfusion [8–11]. The IRAD study demonstrated that the more aortic branches are involved, the higher mortality was recognized [12]. Centofanti et al. [13] developed a mathematical model consisting of five risk factor, such as age, coma, acute renal failure, and redo surgery, to predict early mortality for acute type A aortic dissection. They concluded when the predictive mortality is greater than 58 %, surgery is not considered to be mandatory. Geirsson et al. [9] pointed out that not only the early mortality and also late mortality was higher in patients with cerebral malperfusion. The German registry data (GERRADA) [11] disclosed that new postoperative neurological dysfunction was associated with malperfusion syndrome, supra-aortic vessel dissection and operation time. In their analysis, one third of the patients had no brain protection, which meant distal aorta clamping, and only 2 % had DHCA. Our previous study revealed that early mortality of the patients with preoperative brain malperfusion was 29 and 7 % in those without cerebral malperfusion [14]. Patients with coma never survived surgery in our experience.
Controversy regarding indication for aortic repair in preoperative comatose patients has existed. Patel et al. [15] proposed a strategy, where patients with stroke, acute abdomen, acute renal failure and leg ischemia had surgery after correction or subsiding of the peripheral arterial malperfusion syndrome. Their operative mortality after aortic repair was reported to be 9.5 % in 126 patients, however, 23 out of 70 patients (32.9 %) died of complications or aortic rupture while waiting for resolution of the malperfusion syndrome. Fukuda et al. [16] reported that three stroke patients successfully underwent aortic surgery after 27, 41, and 81 days from onset of aortic dissection, however, one died before surgery. On the contrary, Esterera et al. [17] reported that 80 % of patients with sustained stroke secondary to acute dissection who underwent aortic repair within 10 h had improvement in neurological status. Pocar et al. [18] reported that five comatose patients within 12 h of duration of consciousness disorder all survived surgery and four returned to normal life. Tsukube et al. [19] recommended earlier surgery because 86 % of patients regained the consciousness from preoperative coma when they underwent aortic repair within 5 h after onset of dissection. Bonser et al. [8] pointed the importance of early surgical reperfusion. Shiiya et al. [20] reported three cases in whom establishing selective cerebral perfusion before systemic perfusion. We had a patient, 72 year old female, with acute type A dissection of 6 h old. She was unconscious and left paraplegia on arrival. The CT and carotid echography showed a type A dissection and that there was no flow in the right common carotid artery. In the emergency room, a temporary bypass from the right femoral artery to the true lumen of the right common carotid artery using a roller pump was instituted. Then she was sent to the operating room and had hemiarch replacement. She woke-up next morning and discharged with mild left hemiparesis [21]. Sakaguchi et al. [22] reported a similar case, in whom earlier starting the antegrade cerebral perfusion at the beginning of cardiopulmonary bypass was done and he had no neurological deficit postoperatively.
Regarding arterial cannulation for the extracorporeal circulation, three quarters of patients had femoral cannulation, however, in 90 % of recent 30 cases we have used direct ascending aorta cannulation in the true lumen under guidance of direct or trans-esophageal echography. The axillary artery was used in only 6 % of whole patients. Main advantages of ascending aorta cannulation were (1) quicker access to the aorta, (2) large amount of the antegrade blood flow to the true lumen was almost always possible by using echo guidance, and (3) seldom occurrence of vascular injuries. Reece et al. [23] and Kamiya et al. [24] also reported a safeness of the direct ascending aorta cannulation in acute type A dissection. However, sometimes the organ malperfusion was detected during cardiopulmonary bypass by monitoring the direct blood pressure in the extremities and rSO2. In such circumstances, we have used multiple arterial cannulation in 20 patients, usually adding the femoral or axillary cannulae. Shiiya et al. [20] also recommended multiple arterial inflow strategy when organ malperfusion existed or occurred. Recently, cannulation in the axillary artery has become popular for treating patients with acute type A aortic dissection [25], as well as patients with a shaggy ascending aorta, because this cannulation can provide antegrade blood flow in the aortic arch. Nevertheless, there still some concerns remaining for malperfusion in the brachiocephalic artery, for atheromatous or ulcerative lesions at the orifices of the aortic arch vessels, and for injury of the axillary artery [26].
Antegrade cerebral perfusion is now considered to be the most reliable brain protection method, and has been widely used in the field of aortic surgery [27–29]. However, the procedures vary among surgeons. We always use three cannulae, which are inserted from inside of the arch without snaring [4]. Urbansky et al. [30] has used only one cannula to perfuse the whole brain, and reported a low incidence of postoperative stroke. Many surgeons perfuse only the brachiocephalic and left common carotid artery, and not the left subclavian artery [28]. However, the incompleteness of the brain Wills circle has been reported to be as high as 20–30 % in the normal population [31], and the vertebral arteries were sometimes hypoplastic or stenotic, especially in elderly patients. In addition, the left subclavian artery is often a supplier of the collateral vessels to the spinal cord.
We still use simple deep hypothermic circulatory arrest with retrograde cerebral perfusion in patients who underwent hemiarch repair but the duration of circulatory arrest was limited within 30 min [32]. The neurological outcome of these patients was similar to patients who had ACP in this study. Previously we reported the higher incidence of postoperative TND in patients who had total arch replacement using DHCA compared with ACP [33]. Since then, we have almost exclusively used ACP for patients who underwent total arch replacement. The GERAADA data demonstrated that for circulatory arrest time less than 30 min, neurological results of DHCA and ACP were similar [34].
TAR with elephant trunk insertion has been tried in anticipation of thrombosis of the remaining false lumen in the distal aorta and should be recommended [35]. Elephant trunk insertion technique first proposed by Borst et al. [36] has some advantages; to reinforce from inside and reduce risks of bleeding or new intimal tear at the distal anastomosis, and facilitation of multiple stage treatment of extensive aortic dissection. However, it was not possible for every patient because of preoperative morbidities of the patients. Twenty-three patients with retrograde dissection underwent TAR with elephant trunk insertion to exclude intimal tear. Recent report by Tsagakis et al. [37] regarding frozen elephant trunk insertion acute type A dissection is promising. In our policy, for the young patients, Marfan patients, or patients with completely dissected arch vessels, tear in the arch or in the descending aorta, and those who hemodynamically stable preoperatively we performed TAR [28].
Usage of a four-branch graft has several advantages over the “island” aortic cuff technique when used to reconstruct the arch vessels [4, 28]. The individual anastomosis of each arch vessel can provide a secure anastomosis. In addition, by dividing the arch cuff into three buttons, more liberal exposure of the aortic arch can be obtained. We had three patients who had tear in the brachiocephalic artery which led to reoperation due to dilatation of the residual false lumen of the arch.
The temperature of hypothermic CA during the distal anastomosis is particularly crucial for protecting vital organs. Since the primary goal of core cooling is to achieve a brain temperature compatible with the maximum suppression of metabolism, the lowest temperatures that can be safely achieved for optimal brain protection are used [16]. On the other hand, deep hypothermia tends to be associated with either coagulopathy or lung injury, which is to be avoided. The optimal temperature used during antegrade ACP has been reported to be between 20 and 28 °C [4, 29]. Kamiya et al. [38] reported that the temperature during hypothermic circulatory arrest could be safely increased to 28 °C with a high ACP flow rate, and that the incidence of neurological events was not increased. We set the tympanic temperature between 20 and 23 °C, thus resulting in optimal CA and ACP times (42.4 ± 27.8 and 97.3 ± 31.4 min respectively). As for the rectal temperature, we aimed to keep it below 30 °C just prior to CA, because we had one patient whose rectal temperature before CA was in excess of 30 °C, who developed necrosis of the entire colon, presumably because of the presence of the calcified stenosis of the mesenteric artery with poor visceral circulation.
Monitoring brain oxygenation by rSO2 and blood pressure in the both radial arteries during CPB is particularly important [39]. Earlier detection of the brain malperfusion is prerequisite for normal recovery. Also during re-warming, we increased the ACP flow from 10 to 15 mL/min/m2 to maintain the preoperative values of rSO2, however, the total flow was always maintained below 1,200 mL/min to avoid brain edema.
Limitations of the study are related to its retrospective nature. The operative techniques or strategies are refined over time during this period. These operations were performed by chief surgeon and additionally a couple of surgeons, even though the operative strategy was standardized.
Conclusions
The strategy of surgery and brain protection for acute type A aortic dissection was herein presented. The outcome of patients who had preoperative neurological disorder was worse. However, our approach has contributed to low hospital mortality and morbidities, thus leading to a favorable long-term outcome as a whole.
References
Sakata R, Fujii Y, Kuwano H. Thoracic and cardiovascular surgery in Japan during 2010: annual report by the Japanese Association for Thoracic Surgery. Committee for Scientific Affairs. Gen Thorac Cardiovasc Surg. 2012;60(10):680–708.
Sakata R, Kuwano H, Yokomise H. Hospital volume and outcomes of cardiothoracic surgery in Japan: 2005–2009 national survey. Gen Thorac Cardiovasc Surg. 2012;60:625–38.
Kazui T, Osada H, Fujita H. An attempt to analyze the relation between hospital surgical volume and clinical outcome. Gen Thorac Cardiovasc Surg. 2007;55(12):483–92.
Okada K, Omura A, Kano H, Sakamoto T, Tanaka A, Inoue T, Okita Y. Recent advancements of total aortic arch replacement. J Thorac Cardiovasc Surg. 2012;144(1):139–45.
Ueda Y, Miki S, Kusuhara K, Okita Y, Tahata T, Yamanaka K. Surgical treatment of aneurysm or dissection involving the ascending aorta and aortic arch, utilizing circulatory arrest and retrograde cerebral perfusion. J Cardiovasc Surg (Torino). 1990;31(5):553–8.
Ergin MA, Uysal S, Reich DL, Apaydin A, Lansman SL, McCullough JN, Griepp RB. Temporary neurological dysfunction after deep hypothermic circulatory arrest: a clinical marker of long-term functional deficit. Ann Thorac Surg. 1999;67(6):1887–90.
Knipp BS, Deeb GM, Prager RL, Williams CY, Upchurch Jr GR, Patel HJ. A contemporary analysis of outcomes for operative repair of type A aortic dissection in the United States. Surgery. 2007;142(4):524–8.
Bonser RS, Ranasinghe AM, Loubani M, Evans JD, Thalji NM, Bachet JE, Carrel TP, Czerny M, Di Bartolomeo R, Grabenwöger M, Lonn L, Mestres CA, Schepens MA, Weigang E. Evidence, lack of evidence, controversy, and debate in the provision and performance of the surgery of acute type A aortic dissection. J Am Coll Cardiol. 2011;58(24):2455–74.
Geirsson A, Szeto WY, Pochettino A, McGarvey ML, Keane MG, Woo YJ, Augoustides JG, Bavaria JE. Significance of malperfusion syndromes prior to contemporary surgical repair for acute type A dissection: outcomes and need for additional revascularizations. Eur J Cardiothorac Surg. 2007;32(2):255–62.
Girdauskas E, Kuntze T, Borger MA, Falk V, Mohr FM. Surgical risk of preoperative malperfusion in acute type A aortic dissection. J Thorac Cardiovasc Surg. 2009;138(6):1363–9.
Conzelmann LO, Hoffmann I, Blettner M, Kallenbach K, Karck M, Dapunt O, Borger MA, Weigang E, on behalf of the GERAADA Investigators. Analysis of risk factors for neurological dysfunction in patients with acute aortic dissection type A: data from the German Registry for Acute Aortic Dissection Type A (GERAADA). Eur J Cardiothorac Surg. 2012;42(3):557–65.
Bossone E, Rampoldi V, Nienaber CA, International Registry of Acute Aortic Dissection (IRAD) Investigators, et al. Usefulness of pulse deficit to predict in-hospital complications and mortality in patients with acutetype A aortic dissection. Am J Cardiol. 2002;89:851–5.
Centofanti P, Flocco R, Ceresa F, Attisani M, La Torre M, Weltert L, Calafiore AM. Is surgery always mandatory for type A aortic dissection? Ann Thorac Surg. 2006;82(5):1658–63.
Tanaka H, Okada K, Yamashita T, Morimoto Y, Kawanishi Y, Okita Y. Surgical results of acute aortic dissection complicated with cerebral malperfusion. Ann Thorac Surg. 2003;126(1):290–1.
Patel HJ, Williams DM, Dasika NL, Suzuki Y, Deeb GM. Operative delay for peripheral malperfusion syndrome in acute type A aortic dissection: a long-term analysis. J Thorac Cardiovasc Surg. 2008;135(6):1288–95.
Fukuda I, Imazuru T. Intentional delay of surgery for acute type A dissection with stroke. J Thorac Cardiovasc Surg. 2003;126(1):290–1.
Estrera AL, Garami Z, Miller CC, Porat EE, Achouh PE, Dhareshwar J, Meada R, Azizzadeh A, Safi HJ. Acute type A aortic dissection complicated by stroke: can immediate repair be performed safely? J Thorac Cardiovasc Surg. 2006;132(6):1404–8.
Pocar M, Passolunghi D, Moneta A, Mattioli R, Donatelli F. Coma might not preclude emergency operation in acute aortic dissection. Ann Thorac Surg. 2006;81(4):1348–51.
Tsukube T, Hayashi T, Kawahira T, Haraguchi T, Matsukawa R, Kozawa S, Ogawa K, Okita Y. Neurological outcomes after immediate aortic repair for acute type A aortic dissection complicated by coma. Circulation. 2011;124(11 Suppl):S163–7.
Shiiya N, Matsuzaki K, Kunihara T, Murashita T, Matsui Y. Management of vital organ malperfusion in acute aortic dissection: proposal of a mechanism—specific approach. Gen Thorac Cardiovasc Surg. 2007;55(3):85–90.
Munakata H, Okada K, Kano H, Izumi S, Hino Y, Matsumori M, Okita Y. Controlled earlier reperfusion for brain ischemia caused by acute type A aortic dissection. Ann Thorac Surg. 2009;87(4):e27–8.
Sakaguchi G, Komiya T, Tamura N, Obata S, Masuyama S, Kimura C, Kobayashi T. Cerebral malperfusion in acute type A dissection: direct innominate artery cannulation. J Thorac Cardiovasc Surg. 2005;129(5):1190–1.
Reece TB, Tribble CG, Smith RL, Singh RR, Stiles BM, Peeler BB, Kern JA, Kron IL. Central cannulation is safe in acute aortic dissection repair. J Thorac Cardiovasc Surg. 2007;133(2):428–34.
Kamiya H, Kallenbach K, Halmer D, Ozsöz M, Ilg K, Lichtenberg A, Karck M. Comparison of ascending aorta versus femoral artery cannulation for acute aortic dissection type A. Circulation. 2009;120(11 Suppl):S282–6.
Strauch JT, Spielvogel D, Lauten A, Lansman SL, McMurtry K, Bodian CA, Griepp RB. Axillary artery cannulation: routine use in ascending aorta and aortic arch replacement. Ann Thorac Surg. 2004;78(1):103–8.
Fukuda I, Fujimori S, Daitoku K, Yanaoka H, Inamura T. Flow velocity and turbulence in the transverse aorta of a proximally directed aortic cannula: hydrodynamic study in a transparent model. Ann Thorac Surg. 2009;87(6):1866–71.
Bachet J, Guilmet D, Goudot B, Dreyfus GD, Delentdecker P, Brodaty D, Dubois C. Antegrade cerebral perfusion with cold blood: a 13-year experience. Ann Thorac Surg. 1999;67(6):1874–8.
Kazui T, Washiyama N, Muhammad BA, Terada H, Yamashita K, Takinami M, Tamiya Y. Extended total arch replacement for acute type a aortic dissection: experience with seventy patients. J Thorac Cardiovasc Surg. 2000;119(3):558–65.
Ogino H, Sasaki H, Minatoya K, Matsuda H, Tanaka H, Watanuki H, Ando M, Kitamura S. Evolving arch surgery using integrated antegrade selective cerebral perfusion: impact of axillary artery perfusion. J Thorac Cardiovasc Surg. 2008;136(3):641–8.
Urbanski PP, Lenos A, Lindemann Y, Weigang E, Zacher M, Diegeler A. Carotid artery cannulation in aortic surgery. J Thorac Cardiovasc Surg. 2006;132(6):1398–403.
Merkkola P, Tulla H, Ronkainen A, Soppi V, Oksala A, Koivisto T, Hippeläinen M. Incomplete circle of Willis and right axillary artery perfusion. Ann Thorac Surg. 2006;82(1):74–9.
Svensson LG, Crawford ES, Hess KR, Coselli JS, Raskin S, Shenaq SA, Safi HJ. Deep hypothermia with circulatory arrest. Determinants of stroke and early mortality in 656 patients. J Thorac Cardiovasc Surg. 1993;106(1):19–28.
Okita Y, Minatoya K, Tagusari O, Ando M, Nagatsuka K, Kitamura S. Prospective comparative study of brain protection in total aortic arch replacement: deep hypothermic circulatory arrest with retrograde cerebral perfusion or selective antegrade cerebral perfusion. Ann Thorac Surg. 2001;72(1):72–9.
Krüger T, Weigang E, Hoffmann I, Blettner M, Aebert H, GERAADA Investigators. Cerebral protection during surgery for acute aortic dissection type A: results of the German Registry for Acute Aortic Dissection Type A (GERAADA). Circulation. 2011;124(4):434–43.
Hanafusa Y, Ogino H, Sasaki H, Minatoya K, Ando M, Okita Y, Kitamura S. Total arch replacement with elephant trunk procedure for retrograde dissection. Ann Thorac Surg. 2002;74(5):S1836–9.
Borst HG, Walterbusch G, Schaps D. Extensive aortic replacement using “elephant trunk” prosthesis. Thorac Cardiovasc Surg. 1983;31:37–40.
Tsagakis K, Pacini D, Di Bartolomeo R, Gorlitzer M, Weiss G, Grabenwoger M, Mestres CA, Benedik J, Cerny S, Jakob H. Multicenter early experience with extended aortic repair in acute aortic dissection: is simultaneous descending stent grafting justified? J Thorac Cardiovasc Surg. 2010;140(6 Suppl):S116–20.
Kamiya H, Hagl C, Kropivnitskaya I, Böthig D, Kallenbach K, Khaladj N, Martens A, Haverich A, Karck M. The safety of moderate hypothermic lower body circulatory arrest with selective cerebral perfusion: a propensity score analysis. J Thorac Cardiovasc Surg. 2007;133(2):501–9.
Olsson C, Thelin S. Regional cerebral saturation monitoring with near-infrared spectroscopy during selective antegrade cerebral perfusion: diagnostic performance and relationship to postoperative stroke. J Thorac Cardiovasc Surg. 2006;131(2):371–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Okita, Y. et al. (2014). Brain Protection in Surgery for Acute Type A Aortic Dissection. In: Bonser, R., Pagano, D., Haverich, A., Mascaro, J. (eds) Controversies in Aortic Dissection and Aneurysmal Disease. Springer, London. https://doi.org/10.1007/978-1-4471-5622-2_26
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5622-2_26
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5621-5
Online ISBN: 978-1-4471-5622-2
eBook Packages: MedicineMedicine (R0)