Abstract
Introduction
The female gender has been shown as high-risk factor for mortality and morbidity. We sought to assess the influence of female gender on coronary artery bypass graft (CABG) surgery from our own experience.
Methods
This is a retrospective analysis of prospectively collected database from a single centre. Patients were grouped according to gender and potential differences in pre-operative, intra-operative and post-operative factors were explored. Significant high-risk factors were then fitted in a multivariate model to account for differences in predicting gender influence on surgical outcomes.
Results
Two thousand eight hundred and four consecutive patients underwent isolated first-time CABG between February 2000 and December 2008; 562 (20 %) patients were females. Pre-operatively, females were more likely to have significant comorbidities (age, congestive cardiac failure, hypercholesterolemia, hypertension, ischemic heart disease, peripheral vascular disease, pre-op arrhythmias, small body surface area and poor ejection fraction (p < 0.001)) consistent with higher Euroscore (p > 0.0001) and more urgent surgery (p < 0.002). Intra-operatively, they showed less extent pattern of disease requiring less bypass and cross-clamp time (p < 0.001). Observed surgical mortality was significantly higher in females (3.6 vs. 2.1 %, p < 0.042); however, after adjusting for propensity score and significant factors identified in multivariate models, females only independently predicted a higher wound infection, lower neurological complications, lower rate of re-sternotomy, longer hospital stay and post-surgery stay (p < 0.01).
Conclusions
Despite higher risk profile and higher observed surgical mortality, early outcomes in females were similar to their matched males’ counterpart in isolated CABG surgery. Females were associated with higher incidence of wound infections but lower rate of neurological complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The impact of gender as an independent risk factor for morbidity and mortality after CABG is well documented in large cohort databases. Most reports in CABG suggest that female gender is an incremental risk factor for adverse outcome [1–4].
Of deaths, 18 % in men and 13 % in women in the UK are caused by coronary artery disease (CAD) and that translates into 88000 deaths a year, 49500 for men and 38500 for women [5].
By and large, coronary heart disease (CHD) in females is a disease of the elderly women because at the time a woman develops CHD she is approx 10 years older than her male counterpart is and at the time a woman develops MI she is approx 20 years older than her male counterpart. Moreover, when one refers to age above 75, the mortality from CHD increases by a factor of 9 in women [5].
Furthermore, from the “effect on sex on use of investigations” by Caroline Daly, ESC 2005, it was reported that females are less likely to have angiography and subsequently less likely to undergo surgical treatment for CHD [6].
Furthermore, Khan et al. [7] also suggested that female gender is associated with higher incidence of urgent procedures and smaller vessel size; females tend to be treated less frequently with GPIIb/IIIa and also receive less frequently IMA conduits.
The intent of this study is to examine outcomes by gender after CABG and create matched population for the most significant risk factors. This would allow us to examine the outcomes influenced by gender.
Subjects and methods
Patients
This study was a retrospective, single-centre, cohort study including 2804 consecutive patients undergoing first-time isolated CABG at a tertiary cardiac unit in St. James’s Hospital, Dublin, Republic of Ireland from January 2000 to December 2008.
All data were collected prospectively (Patient Analysis and Tracking System, Dendrite Clinical, UK) in the departmental database through the input of a dedicated database manager.
The analysis was conducted on 2804 CABG patients. Patients were stratified (based on gender) into two groups; 562 (20 %) were females, and these were compared with their male counterparts.
For each patient, demographic and clinical data including medical history, peri-operative, intra-operative data and post-operative intensive care unit (ICU) complications were extracted from the CABG database. Preoperative clinical factors analysed included urgency of procedure, coronary risk factors, diabetes mellitus (DM), hypertension, lipidemia, smoking, myocardial infarction (MI), prior percutaneous coronary intervention (PCI), heart failure, cerebrovascular accident (CVA), renal failure (RF), peripheral vascular disease (PVD), coronary disease severity, severity of left main stem (LMS) and LV function. The data collected on procedural details were cardiopulmonary bypass, aortic cross-clamp time and number of grafts used.
Our Institutional Review Board approved both this study and the departmental database. Individual patient consent was obtained for entry into the database.
Outcomes
The main outcome measured was in-hospital mortality. The other outcomes that were analysed included overall post-op complications, length of ventilation post-op >24 h, MRSA infection post-op, post-op arrhythmias, re-operation for bleeding/tamponade, re-operation for sternal dehiscence, pulmonary complications, neurological complications, wound infection, renal complications, gastrointestinal (GI) complications, multi-organ failure, intensive care re-admission, intensive care death, surgical mortality (<30 days of discharge), total hospital stay (days), cardiac surgery total length of stay (LOS) (days), and post-operative stay (days).
Definitions
Body surface area was calculated by the method of Dubois and Dubois. Operative priority was determined according to standard criteria [8]. Urgent operations were procedures performed in patients whose accelerated symptoms prompted urgent admission for evaluation and who were judged to be too unstable for discharge before surgery. Emergency operations are done within 24-h of catheterization. Elective operation means that medical factors indicate the need for an operation through a readmission at a later date. In-hospital mortality refers to all mortalities within the same admission post cardiac surgery regardless of their LOS. Operative mortality was any death occurring within 30 days of surgery.
Congestive cardiac failure (CCF) was determined by the presence of pulmonary opacities/oedema on chest X-rays. Peri-operative myocardial infraction (MI) was either a new Q wave or the elevation of the myocardial fraction of creatinine kinase (CK) in association with persistent ST changes or a new conduction abnormality.
Low cardiac output syndrome was diagnosed when the cardiac index was less than 2.5 l/min−1/m2 and inotropic support was needed for longer than 20 min.
Intra-operative complications included dissection, haemorrhage, arrhythmia, cardiac laceration, cardiac dilation, air embolism, myocardial infarction, aortic tear, cardiac arrest, valve trauma and unsatisfactory graft harvest.
Neurological complications depict not only any neurological deficit lasting >24 h, but also acute delirium state, even if the deficit resolved before discharge.
Wound infections included sternal and vein harvested site.
Renal complications refer to post-operative abnormal Creatinine that was managed conservatively or required dialysis.
Gastrointestinal (GI) complications refer to constipation-ileus, severe GI bleeding, cholecystitis, hepatitis, pancreatitis, bowel obstruction and bowel ischemia.
Infective complications refer to wound infections requiring intervention and sepsis. Pulmonary complications refer to post-operative chest infection, pleural effusion requiring drainage, adult respiratory distress syndrome, re-intubation and tracheostomy insertion.
Cardiopulmonary bypass
All cases were performed through a median sternotomy. Standard techniques of cardiopulmonary bypass (CPB) were employed in all patients. Following full anticoagulation with heparin given at a dose of 300 IU/kg to maintain an activated clotting time of 400–600 s, CPB was instituted using ascending aortic cannulation and a two-stage right atrial venous cannulation. A roller pump (jostra HL 20) and hollow-fibre membrane oxygenator (Optima, Cobe Cardiovascular Inc.) were used. The extracorporeal circuit was primed with 1400 ml of Hartmann’s solution and 5000 IU heparin. CPB was maintained with non-pulsatile flow with a minimum flow rate of 2.4 l/m2/min at normothermia with temperature allowed to drift to moderate hypothermia of 34 °C. Arterial line filtration (Sentoy, Cobe Cardiovascular Inc.) was used in all the cases. Shed blood was recycled using cardiotomy suction. Acid–base was managed with alpha-stat control. Myocardial protection was achieved using cold blood cardioplegia given antegradely, retrogradely or both, depending on the surgeon’s preference. On completion of all distal anastomoses, the aortic cross-clamp was removed and the proximal anastomoses performed with partial aortic clamping. Heparin was reversed with protamine at 1:1 ratio on weaning off cardiopulmonary bypass.
Statistical analysis
Patients were grouped according to gender, and potential differences in pre-operative and intra-operative factors were analysed.
Continuous variables are shown as mean and stand deviation (SD) or as 25th and 75th percentiles. Categorical variables are shown as a percentage with 95 % CI. Comparisons were made with Wilcoxon rank sum tests and Chi-square tests as appropriate. Standard statistical tests were used to calculate odds ratios with 95 % CI.
Univariate analysis (t test and Fisher’s exact test) was used to identify risk factors between male and female patients.
Multivariable logistic regression was then used to further develop independent predictors for gender. A propensity score based on these differences was calculated and used for adjustment in multivariate regression in predicting gender influence on surgical mortality and morbidity.
Logistic regression was used to assess the effect of gender on each outcome [expressed as odds ratio (OR), which approximates relative risk] after adjusting for differences in patient and disease characteristics (treatment selection bias).
Treatment selection bias was controlled, by constructing a propensity score. The propensity score was the probability that a patient would be a female patient, and was constructed from the variables listed in Table 1 (C statistic 0.71). Once the propensity score is constructed for each patient, there are three ways of using the score for comparisons: matching, stratification and multivariable adjustment. We have decided to use multivariable adjustment because matching would have reduced the study size and stratification can be difficult to interpret. The propensity score is then included along with the comparison variable (male or female) in multivariate analyses of outcome producing adjusted OR as shown in Table 3. The propensity score adjusts for the treatment selection bias, which is evident in Table 1, between one group versus another. Using a propensity score as the sole means for adjusting outcomes was preferable due to the low number of events in our study and provides better adjustment for those factors driving treatment selection; the overall effect is more complete risk adjustment. In all cases a p value, 0.05 was considered significant. All statistical analyses were performed retrospectively with SPSS for Windows Version 17.
Results
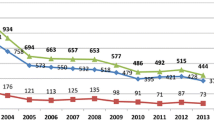
Altogether, 2804 consecutive patients underwent isolated CABG between February 2000 and December 2008; 562 (20 %) were females and that varied from 15 to 28 % throughout the years (Fig. 1).
The preoperative clinical characteristics of the patients in the two age groups (non-matched) are summarised in Table 1. There were differences between the two groups prior to matching. In comparison with males, females were more likely to be at least 3 years older overall. In terms of risk factors for CAD, females were found to have significant higher incidence of hypertension and that without a doubt translates into a higher rate of diastolic LV dysfunction in this group. Interestingly, there was a higher genetic link with CAD in the female group and also higher incidence of dyslipidemia compared to their male counterparts.
Furthermore, women were more likely to have more PVD (23.1 vs. 16.5 %, p < 0.001); however, that was not translated into higher incidence of previous cerebral or vascular events.
As regards to the left ventricular (LV) status, there were more males with fair or poor LV function (37.4 vs. 30.6 %, p = 0.007), although the number of previous myocardial infractions (MI) or the incidence of LMS disease did not differ between the two groups.
Likewise, angina/dyspnoea status, diabetes, renal failure, previous cardiovascular interventions or surgery, critical pre-op state, intravenous (IV) inotropes and intra-aortic balloon pump (IABP) prior to surgery, were variables similarly distributed between male and female patients.
Females showed less extent pattern of CAD (3VD: 70 vs. 80.4 %, p < 0.001) requiring less bypass grafts (69.4 vs. 81.2 %, p < 0.001) and therefore shorter cross-clamp time (p < 0.001).
BSA was different between genders as expected (1.71 vs. 1.96 m², p < 0.001). Lastly, overall females tend to have higher Euroscore, higher rate of preoperative CCF and more frequently urgent surgery.
On univariate analysis (Table 2), length of ventilation was significantly higher in the females’ group and that was reflected on significant higher rate of multi-organ failure in this group. Subsequently the observed surgical mortality was significantly higher in females (3.6 vs. 2.1 %, p = 0.042); however, the incidence of peri-operative morbidity in terms of neurological, pulmonary and GI complications showed no differences between the two groups.
Following adjustment for propensity score and significant factors identified in multivariate models (Table 3), females only independently predicted a higher wound infection rate (p < 0.006), lower neurological complications rate (p = 0.016), lower rate of re-sternotomy for bleeding (p = 0.008), longer duration of hospital stay (p = 0.003) and post-surgery stay (p = 0.012).
Discussion
The intent of this study is to examine outcomes by gender after CABG and create matched population for the most significant risk factors. Using data from the Health Care Utilization Project (HCUP) for 1998–2002, 1.2 million CABG admissions were analysed by Becker et al. [9]; they found that female CABG patients still experience significantly higher in-hospital mortality rates than their male counterparts. Some reports attributed these to differences in the demographic profiles of women at the time of operation [10, 11], or to a referral bias [12, 13]. In our series, women were older, smaller, had more diastolic LV dysfunction and had more comorbid conditions. The higher rate of hypertension in our studied population translates into a steeper pressure–volume relationship; this is supported by reports of gender differences in molecular remodelling in pressure overload hypertrophy [14, 15].
Our data also suggest that more women than men required urgent or emergency operations with advanced NYHA functional class and congestive heart failure. This may be related to late presentation, late referral or even both.
The risk for myocardial infarction differs between genders, as well as the pattern of coronary disease and myocardial remodelling. Vaccarino et al. [16] reported that myocardial infarction has the worse outcome when it occurred in younger women.
Extrapolating from this observation, the same group studied gender differences in mortality following CABG stratified by age. Paradoxically, studies have suggested that gender differences are greater in younger than in older patients [16–19]. This difference in risk decreases with age when women become “more like men”. As per those authors, women <50 years of age were three times more likely to die than men (3.4 vs. 1.1 %), and women 50–59 years of age were 2.4 times more likely to die than men (2.6 vs. 1.1 %). In the older age categories, the gender difference in in-hospital mortality was less marked for the interaction between gender and age. In our series, females were older (mean age 66.6 vs. 63.3 years) with corresponding higher observed mortality (3.6 vs. 2.1). The reasons for these observations are unknown. Is it due to yet-undetected high-risk factors in females? Wexler et al. [20] refer to lack of normal protective factors, ovarian dysfunction, abnormalities of the estrogen receptor, hormones that affect the coagulation system, lipid levels, and inflammatory mechanisms, psychological factors as well as referral bias, as the causative factors that have been postulated to occur in women with premature CAD.
Although incident of diabetes did not differ between the comparing populations in our series, as per Mehilli et al. [21], diabetes may have a greater adverse impact on women than on men.
In our cohort of patients, the females had a higher risk profile and higher Euroscore prior to surgery when compared with men. On the contrary, men were most likely to have poor LV, had similar incidence of LMS disease but more extensive pattern of CAD. In terms of revascularization completeness (number of grafts), there were differences between genders, with females ended up receiving less number of grafts (p < 0.001).
The relationship between vessel size and outcomes is inconsistent [22]. Body surface area was positively correlated with coronary artery luminal diameter and was a determinant of the risk of hospital mortality for men and women undergoing CABG. Furthermore, the correlation between body surface area (BSA) and coronary artery size was 0.9 [23], although other studies have found correlations as low as 0.1 [24, 25]. In our series, BSA was clearly a strong confounder for mortality. Significantly, more women have such low BSA than men have. However, after adjustment, both men and women of equal BSA possessed equal mortality risk.
Although most studies have documented a higher in-hospital or post-operative mortality in women compared with men, several investigators have concluded that when adjustment was made for differences in body size and clinical and angiographic variables, gender was not a predictor [11, 26] for adverse outcome. In contrast, other studies [27, 28] have continued to document a higher mortality in women that persisted in multivariable analysis. However, these studies have typically not adjusted results accordingly. In our series, without adjustments, females were more likely to require prolonged ventilated (6.9 vs. 4.5 %, p < 0.008), more likely to develop multi-organ failure (3 vs. 1.6 %, p < 0.036) and subsequently higher mortality. Furthermore, the cardiac surgery specific LOS >7 days was higher in the female group (50.7 vs. 40 %, p < 0.001). However, following adjustment, there was no mortality or morbidity differences.
Female gender was found to have higher rate of wound infections, which could be attributed in our series to their higher rate of prolonged total hospital stay or post-operative stay. This has been shown before in prospective settings as well [29, 30].
The lower rate of neurological complications associated with female gender in this study is not clear. Some suggest that it is perhaps due to the arbitrary distinction between these complications [23]. Others have argued that the higher incidence of peri-operative neurological complications in women cannot be explained by currently known risk factors [18].
Females were associated with lower likelihood of re-exploration for bleeding, and that may be due to the lower number of grafts overall and subsequently lower CPB and cross-clamp time.
Despite our incomplete understanding of the influence of smaller size and the increase in the gender difference in mortality in younger women that is far from being intuitively clear, several concepts have emerged such as gender differences in outcomes are greatest for in-hospital morbidity and mortality. These differences are diminished after adjustment for risk factors such as age and significant comorbidities.
Knowledge of the reasons for gender differences in outcomes after coronary revascularization can optimise therapy for all patients. The relative importance of factors in mediating these gender differences, particularly early mortality, requires studies that are adequately powered to conduct multivariate risk adjustment.
It is essential that clinical trials and registries report gender-specific outcomes, as it is likely that predictors of risk, including gender, will continue to evolve as procedure type and patient risk profiles change. It is not clear whether the differences are due to gender-related differences in the biology of the disease or in gender-related issues of treatment and access to care. Finally, we agree with a number of researchers that have concluded that it is likely that specific variable and not gender inherently, have led to the disparity in mortality outcomes between males and females.
Conclusion
This work highlighted the fact that despite higher risk profiles and higher observed surgical mortality, early outcomes in females were similar to their matched males’ counterpart in isolated CABG surgery. Females are at increased risk of wound infection and longer hospital stay and post-op stay, but at lower risk of neurological complications and re-sternotomy for bleeding.
Limitations
The limitations of our study arise primarily from its observational nature. For example, the decision to use a specific treatment or specific medication was not controlled. The data, however, were collected by a dedicated officer and, hence, are not subject to some lack of uniformity. Secondly, this is a hospital cohort; therefore, outcomes that occurred after discharge are not recorded.
In spite of these limitations, by using a large database, we were able to adjust for many important risk factors; therefore, the methodology of this study with the use of propensity matching is useful because it enabled us to eliminate the bias attributed to confounding factors.
References
Abramov D, Tamariz MG, Sever JY, Christakis GT, Bhatnagar G, Heenan AL, et al. The influence of gender on the outcome of coronary artery bypass surgery. Ann Thorac Surg. 2000;70:800–5 (discussion 806).
Mickleborough LL, Takagi Y, Maruyama H, Sun Z, Mohamed S. Is sex a factor in determining operative risk for aortocoronary bypass graft surgery? Circulation. 1995;92:II80–4.
Rahimtoola SH, Bennett AJ, Grunkemeier GL, Block P, Starr A. Survival at 15 to 18 years after coronary bypass surgery for angina in women. Circulation. 1993;88:II71–8.
Weintraub WS, Wenger NK, Jones EL, Craver JM, Guyton RA. Changing clinical characteristics of coronary surgery patients. Differences between men and women. Circulation. 1993;88:II79–86.
Scarborough P, Bhatnagar P, Wickramasinghe K, Smolina K, Mitchell C, Rayner M. Coronary heart disease statistics 2010. In: Group BHFHPR, editor. Oxford: Department of Public Health, University of Oxford; 2010. p. 156.
Stramba-Badiale M, Fox KM, Priori SG, Collins P, Daly C, Graham I, et al. Cardiovascular diseases in women: a statement from the policy conference of the European Society of Cardiology. Eur Heart J. 2006;27:994–1005.
Khan SS, Nessim S, Gray R, Czer LS, Chaux A, Matloff J. Increased mortality of women in coronary artery bypass surgery: evidence for referral bias. Ann Intern Med. 1990;112:561–7.
O’Connor GT, Plume SK, Olmstead EM, Coffin LH, Morton JR, Maloney CT, et al. A regional prospective study of in-hospital mortality associated with coronary artery bypass grafting. The Northern New England Cardiovascular Disease Study Group. JAMA. 1991;266:803–9.
Becker ER, Rahimi A. Disparities in race/ethnicity and gender in in-hospital mortality rates for coronary artery bypass surgery patients. J Natl Med Assoc. 2006;98:1729–39.
Christakis GT, Weisel RD, Buth KJ, Fremes SE, Rao V, Panagiotopoulos KP, et al. Is body size the cause for poor outcomes of coronary artery bypass operations in women? J Thorac Cardiovasc Surg. 1995;110:1344–56 (discussion 1348–56).
O’Connor GT, Morton JR, Diehl MJ, Olmstead EM, Coffin LH, Levy DG, et al. Differences between men and women in hospital mortality associated with coronary artery bypass graft surgery. The Northern New England Cardiovascular Disease Study Group. Circulation. 1993;88:2104–10.
Naylor CD, Levinton CM. Sex-related differences in coronary revascularization practices: the perspective from a Canadian queue management project. CMAJ. 1993;149:965–73.
Tobin JN, Wassertheil-Smoller S, Wexler JP, Steingart RM, Budner N, Lense L, et al. Sex bias in considering coronary bypass surgery. Ann Intern Med. 1987;107:19–25.
Liao Y, Cooper RS, Mensah GA, McGee DL. Left ventricular hypertrophy has a greater impact on survival in women than in men. Circulation. 1995;92:805–10.
Weinberg EO, Thienelt CD, Katz SE, Bartunek J, Tajima M, Rohrbach S, et al. Gender differences in molecular remodeling in pressure overload hypertrophy. J Am Coll Cardiol. 1999;34:264–273.
Vaccarino V, Abramson JL, Veledar E, Weintraub WS. Sex differences in hospital mortality after coronary artery bypass surgery: evidence for a higher mortality in younger women. Circulation. 2002;105:1176–81.
Cowley MJ, Mullin SM, Kelsey SF, Kent KM, Gruentzig AR, Detre KM, et al. Sex differences in early and long-term results of coronary angioplasty in the NHLBI PTCA Registry. Circulation. 1985;71:90–7.
Hogue CW, Barzilai B, Pieper KS, Coombs LP, DeLong ER, Kouchoukos NT, et al. Sex differences in neurological outcomes and mortality after cardiac surgery: a society of thoracic surgery national database report. Circulation. 2001;103:2133–7.
Regitz-Zagrosek V, Lehmkuhl E, Hocher B, Goesmann D, Lehmkuhl HB, Hausmann H, et al. Gender as a risk factor in young, not in old, women undergoing coronary artery bypass grafting. J Am Coll Cardiol. 2004;44:2413–4.
Wexler LF. Studies of acute coronary syndromes in women–lessons for everyone. N Engl J Med. 1999;341:275–6.
Mehilli J, Kastrati A, Dirschinger J, Bollwein H, Neumann FJ, Schomig A. Differences in prognostic factors and outcomes between women and men undergoing coronary artery stenting. JAMA. 2000;284:1799–805.
Mickleborough LL, Carson S, Ivanov J. Gender differences in quality of distal vessels: effect on results of coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;126:950–8.
Woods SE, Noble G, Smith JM, Hasselfeld K. The influence of gender in patients undergoing coronary artery bypass graft surgery: an eight-year prospective hospitalized cohort study. J Am Coll Surg. 2003;196:428–34.
Cantor WJ, Miller JM, Hellkamp AS, Kramer JM, Peterson ED, Hasselblad V, et al. Role of target vessel size and body surface area on outcomes after percutaneous coronary interventions in women. Am Heart J. 2002;144:297–302.
Sheifer SE, Canos MR, Weinfurt KP, Arora UK, Mendelsohn FO, Gersh BJ, et al. Sex differences in coronary artery size assessed by intravascular ultrasound. Am Heart J. 2000;139:649–53.
Loop FD, Golding LR, MacMillan JP, Cosgrove DM, Lytle BW, Sheldon WC. Coronary artery surgery in women compared with men: analyses of risks and long-term results. J Am Coll Cardiol. 1983;1:383–90.
Douglas JS, King SB, Jones EL, Craver JM, Bradford JM, Hatcher CR. Reduced efficacy of coronary bypass surgery in women. Circulation. 1981;64:II11–6.
Gardner TJ, Horneffer PJ, Gott VL, Watkins L Jr, Baumgartner WA, Borkon AM, et al. Coronary artery bypass grafting in women. A ten-year perspective. Ann Surg. 1985;201:780–4.
Bhatia JY, Pandey K, Rodrigues C, Mehta A, Joshi VR. Postoperative wound infection in patients undergoing coronary artery bypass graft surgery: a prospective study with evaluation of risk factors. Indian J Med Microbiol. 2003;21:246–51.
Bellchambers J, Harris JM, Cullinan P, Gaya H, Pepper JR. A prospective study of wound infection in coronary artery surgery. Eur J Cardiothorac Surg. 1999;15:45–50.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Al-Alao, B.S., Parissis, H., McGovern, E. et al. Gender influence in isolated coronary artery bypass graft surgery: a propensity match score analysis of early outcomes. Gen Thorac Cardiovasc Surg 60, 417–424 (2012). https://doi.org/10.1007/s11748-012-0082-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-012-0082-7




