Abstract
Purpose
Bypass surgery in patients undergoing cardiogenic shock caused by acute coronary syndrome is one of the most urgent and often performed cardiac operations. It remains unclear if patients gender independently influences the outcome. Literature reveals that females and males primarily differ from each other with regard to many important preoperative characteristics. Our objective was to compare the outcome and postoperative courses of both genders, using matched samples, eliminating these preoperative differences.
Methods
Between 2007 and 2015, 491 patients in cardiogenic shock underwent urgent bypass surgery in our institution. To assess the impact of gender on outcomes, we performed a propensity score matching to create two groups [males and females] which were matched for age, severity of shock, coronary artery disease morphology, and other comorbidities. Two groups were created: (1) 103 female and (2) 103 male patients. We analyzed the outcomes, complications and potential mortality predictors.
Results
Most of the patients had three-vessel disease (70.1%, n = 344) with proximal left anterior descending lesion (88%, n = 432). Our study showed no differences between female and male patients regarding choice of conduits, number of anastomosed vessels, and outcome. Acute kidney injury (AKI) occurred significantly more often in female patients and pericardial tamponade in their male counterparts. There were no differences regarding other major complications.
Conclusion
Gender does not appear to influence long-term outcomes in the study sample. Female gender is an independent risk factor for postoperative AKI. Other complications occurred with comparable rates in both genders. Exertion tolerance in the follow-up period was similar between genders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiogenic shock (CS) is a life-threatening state of reduced cardiac output; it results in hypotension and impaired end-organ perfusion caused by primary cardiac disorders [1]. Acute coronary syndrome (ACS) is the underlying pathology in about 80% of cases [2]. Occurring in about 5 to 10% of all ACS patients, CS is the main cause of early mortality in this group with an in-hospital mortality rate of up to 51% [1, 3]. This rate would be higher if the patients were treated only medically, but causal therapy with early revascularization or mechanical circulatory support has improved patient outcomes over the last few decades [4].
Risk profiles and mortality predictors have already been examined in other studies, it remains however unclear if patient gender independently influences patient outcome in this subset of patients. In previously published comparisons, important preoperative differences existed between females and males. Gender-related outcomes were compared in the Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock (SHOCK) trial and other studies. However, these concentrated on different treatment strategies, and their designs did not eliminate the differences in age and comorbidities between the genders [5, 6].
Our aim therefore was to exclude the most distinct preoperative differences between genders through propensity score matching and then to compare the outcomes between the two groups.
Methods
Selection of patients
We enrolled 491 consecutive patients (103 females, 388 males) in our retrospective study who developed acute heart failure (HF) due to ACS and underwent coronary artery bypass grafting (CABG) as an emergent procedure in our clinic from 2007 to 2015.
All of the included patients had ACS resulting from coronary artery disease (CAD). Patients with ischemia caused by other factors, such as anemia, severe aortic valve stenosis, tachycardia, myocarditis, intoxication, or shock were not included.
Patients with relevant valvular disease, mechanical complications of ACS, severe chronic HF, or those who underwent any concomitant procedures were excluded. In every included case, the acute HF began within 72 h after the onset of ACS. Implantation of intra-aortic balloon pump (IABP) or extracorporeal membrane oxygenation (ECMO) were not exclusion criteria.
Statistical methods
To compare the postoperative courses and outcomes of the male and female patients, we matched their propensity scores using the nearest-neighbor method without caliper and with a 1:1 ratio. Finally, we obtained a matched sample with 103 males and 103 female patients with comparable preoperative conditions.
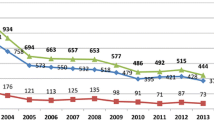
All of the variables used for such matching are listed in Fig.1, with their standardized mean differences before and after matching. Continuous variables are presented as means ± standard deviations for normal distributions and medians with quartiles for not-normal distributions. The matched datasets were considered as independent samples. For comparing the means between the groups, we used the t-test if the distributions were normal. For distributions that were not normal, we transformed the variables into normality using logarithmic or reciprocal transformations. In cases of unsuccessful transformation, non-parametric statistics were applied. Categorical variables were presented as absolute values and percentages. For comparing their distributions between the groups, the chi-squared test was used. For assessing the risk factors for in-hospital mortality, we performed a logistic regression analysis. The results are presented as odds ratios with a 95% confidence interval (CI). To present the effect of the hemoglobin decrease on the serum creatinine level (SCR) increase, a simple linear regression model was used. The results are presented as regression coefficient with 95% CI. The risk factors for long-term mortality were estimated with the proportional hazard model and are shown as hazard ratios with 95% CI. For the survival analysis, the Kaplan–Meier method was used. We compared the survival rates between the groups using the log-rank (Mantel–Cox) test. Overall, p values < 0.05 were considered statistically significant.
For the matching and statistical analyses, we used the R software v.3.4.3 (R Foundation for Statistical Computing, Vienna, Austria) in addition to the IBM SPSS Statistics version 25 (IBM Corp.) [7, 8].
Follow-up
Our clinic performs the follow-up routinely up to 6 months after surgery, and we included the relevant data in our analysis. Information about survival was received from the registration office. We sent out questionnaires to each of the 362 patients about repeat revascularization and subjective assessment of limitations in physical activity according to the New York Heart Association (NYHA) functional classification, receiving detailed answers from 213 patients (58.8%).
Definitions
Acute HF was defined as a rapid onset of symptoms or signs of HF as well as an acute aggravation of preexisting compensated HF [9]. We defined cardiogenic shock using the clinical criteria, such as hypoperfusion (reduced urine output < 30 ml/h, cool extremities, reduced consciousness level) and hypotension (systolic blood pressure < 90 mmHg or need for vasopressors or inotropes to maintain organ perfusion and blood pressure) over more than 30 min despite adequate filling status [1]. Since the cardiac index and the pulmonary capillary wedge pressure were not routinely measured, hemodynamic criteria were not considered. If the patient needed high doses of vasopressors or inotropes (norepinephrine > 0.2 μg/kg/min or dobutamine > 4 μg/kg/min) at any time, the CS was considered severe.
ACS was defined as a spectrum of conditions compatible with acute myocardial ischemia that are usually due to a sudden reduction in coronary blood flow [10].
According to the Risk, Injury, Failure, Loss of kidney function, and End-stage kidney disease (RIFLE) classification, AKI is “risk” in cases of reduced urine output (< 0.5 mL/kg/h) with an increase of SCR by 1.5 to 2 times. Acute kidney injury is “injury” in cases of reduced urine output (< 0.5 mL/kg/h) with an increase of SCR by 2 to 3 times, and is considered “failure” in cases of reduced urine output (< 0.3 mL/kg/h) with an increase of SCR by ≥ 3 times [11].
Complete revascularization was anatomically defined as revascularization of all coronary arteries with stenosis > 50% and diameter > 1.5 mm [12].
Results
Preoperative data
Most patients were male (79%, n = 388). The statistically significant age difference between male and female patients (66.9 ± 9.9 and 71.2 ± 9.7, respectively; p < 0.001) was offset by data preprocessing with the propensity score matching. The balance of other variables describing preoperative conditions was also distinctly improved by the matching process. We achieved very small standardized differences regarding shock severity, estimated glomerular filtration ratio (eGFR), and variables describing the morphology of CAD (Fig. 1). The preoperative characteristics of the analyzed sample are presented in Table 1.
Twenty-two (10.7%) of our matched patients presented with ST-elevation myocardial infarction (STEMI), whereas 133 (64.6%) were diagnosed as having Non-ST-elevation myocardial infarction (NSTEMI). Fifty-one (24.8%) of them did not meet the biochemical criteria of myocardial injury [13].
We emphasized the importance of CAD morphology and history of percutaneous coronary interventions (PCI). Eighty-four (40.8%) of our 206 matched patients had undergone a previous PCI. Most of these patients (82%, n = 69) had received an implanted stent (detailed characteristics in Table 2).
Surgical data
Almost all patients (96.5%, n = 474) underwent surgery via cardiopulmonary bypass (CPB). The times of surgery, CPB, and aortic cross-clamp did not differ between matched male and female patients.
There were no significant differences between female and male patients regarding the choice of conduits, number of anastomosed vessels, IABP, or ECMO implantation rates, the completeness of revascularization, and intraoperative mortality (Table 3).
Postoperative course
We observed a low-output syndrome in 20.4% (n = 100) of the patients. All of these patients required vasopressors or inotropes at the time of leaving the operating room. Seventy (14.3%) patients were additionally treated with IABP and four (0.8%) with ECMO.
Based on routine blood tests, we computed the SCR and hemoglobin, and hematocrit indices, which is the proportion between the highest (related to SCR) or the lowest (related to hemoglobin and hematocrit) obtained value to the value upon admission. The purpose was to demonstrate the mean amplitude of temporary value changes in a typical postoperative course after emergent cardiac surgery. The SCR increased temporarily after the surgery up to 1.6 ± 1.4 times (1.7 ± 1 times in female versus 1.47 ± 1.2 in male patients, p < 0.001). The hemoglobin index was 0.84 ± 0.18; this drop was significantly more relevant in male than in female patients (0.82 ± 0.19 versus 0.89 ± 0.14; p = 0.021). The same principle applied to the hematocrit (0.82 ± 0.17 in the whole sample; 0.8 ± 0.17 in male versus 0.87 ± 0.15 in female patients; p = 0.02). The absolute values of the lowest resulting hemoglobin and hematocrit levels in addition to the highest SCR did not differ between the genders.
We showed that any temporary increase of SCR > 1.5 times appears to be a common complication (33.6%; n = 165) and occurs much more frequently in female (47.6%; n = 49) than in male (28.2%; n = 29) patients (p = 0.004). The odds ratio with 95%CI for women was 2.0 (1.3 to 3.1, p = 0.002) in the sample before the matching and 1.932 (0.97 to 3.8, p = 0.062) within the matched sample.
According to the RIFLE classification of the AKI, an SCR index of 1.5 to 2 (“risk” level) times occurred with a similar frequency among female and male patients (18.4%, n = 19 versus 14.6%, n = 15; p = 0.45). A SCR index of ≥2 was seen in a significantly higher proportion of females (30[29.1%] versus 14 [13.6%]; p = 0.007]. The odds ratio with 95% CI for women was 1.4 (0.8 to 2.5, p = 0.183) in the unmatched sample and 2.6 (1.3 to 5.3, p = 0.008) after the matching.
Moreover, new-onset dialysis occurred more frequently in female patients, but this relationship (female versus male) was not statistically significant in our sample (p = 0.229). The lowest resulting absolute hemoglobin value (g/dl) was a strong predictor for any SCR increase in the postoperative course (odds ratio = 0.207, 95% CI: 0.34–0.073; p = 0.003), the hemoglobin index failed to show any significant influence. Thirty-day mortality was 10.7% (n = 11) among female patients versus 7.7% (n = 8) among male patients (p = 0.47). Postoperative data and complications are presented in Tables 4 and 5.
Follow-up
The mean follow-up time was 4.3 ± 3 years while the extrapolated mean survival time was 7.23 years. The 30-day, 1-year, and 3-year survival rates in the whole sample were 92%, 85%, and 82%, respectively. The comparison of cumulative survival between female and male patients is depicted in Fig.2. There were no significant differences (log-rank, p = 0.401).
We received our questionnaires back from 37 of 72 (51.4%) female patients and 47 of 77 (61%) male patients (p = 0.154). The subjectively assessed exertion tolerance had worsened within the follow-up time in 11 of 37 (29.7%) females and 18 of 47 (38.3%) males (p = 0.412). Also, the distribution of NYHA classes was similar for both genders (p = 0.801). Only 4 of 37 (10.8%) women and 5 of 47 (10.6%) men had NYHA-class III and no one had NYHA-class IV.
The data from our questionnaire also presented no differences between the analyzed groups (Table 6).
Mortality predictors
We identified several independent predictors of in-hospital and long-term mortality and have presented them in Table 7. STEMI was a predictor of in-hospital mortality, whereas patients who presented with NSTEMI were at higher risk of death within the long-term follow-up. Patients who did not meet the biochemical criteria of myocardial injury at the time of admission represented the lowest risk cohort for short- and long-term mortality. Variables describing CAD morphology, CPB time, and cross-clamp time did not influence the outcome. Mortality increases with age, shock severity, and renal function impairment. Any active infection during surgery and cardiopulmonary resuscitation are also important risk factors of short- and long-term mortalities. With regard to postoperative variables, gastrointestinal bleeding solely influenced short-term outcomes and stroke caused an increase in mortality in the follow-up period.
Discussion
In our study, mortality rates and limitations in exercise capacity after the surgery in patients with ACS-induced CS were similar for both genders. Women were more likely to develop postoperative AKI, whereas relevant pericardial effusion was more often seen in men. The rates of other major postoperative adverse events did not differ between genders.
The etiology of CS is more closely associated with the incidence of STEMI than NSTEMI. However, if identification and percutaneous treatment of culprit lesions are possible, emergent PCI is the method of choice in STEMI patients [14]. Our sample consists of patients who were selected due to the surgical nature of their treatment, hence a higher rate of patients presenting with NSTEMI.
Most patients with CAD and ACS were males. They were usually younger than the female patients, implying a better prognosis in hemodynamically stable conditions [15]. Also, in the context of surgical revascularization, the female gender is an independent mortality-related risk factor. The female gender mortality association is a distinct trend seen in many previous studies and is failing to decline over the last two decades, despite remarkable improvements in medical and surgical therapy [16]. On the other hand, many studies demonstrate in-hospital and long-term mortality to be equal for both genders in patients with ACS-induced CS [17, 18]. It is important to consider that in all of these trials, there are distinct preoperative differences between male and female patients. We confirmed equal mortality for all male and female patients in CS who underwent surgical coronary revascularization. In our study, this conclusion is confirmed by the propensity score matching, reducing preoperative differences regarding age and comorbidities to a completely insignificant level.
Mortality and the incidence of most postoperative complications were equal for both sexes. The surgery-related pericardial tamponade occurred more frequently in men than in women. This tendency has already been described in the literature, but no definite explanation for this disproportion in our sample has been offered [19].
It is of interest that over one-third of patients with ACS-induced CS had undergone various PCIs in their medical history, a surprisingly high proportion in comparison with the presented literature. Some studies have shown the ACS presentation, due to in-stent restenosis, to be associated with worse long-term prognosis and a higher recurrence incidence [20]. On the other hand, most of our patients had triple-vessel disease and could have developed critical stenoses also in other locations, not only within the stents.
It is known that women have an increased risk of developing AKI [21]. Ranucci and colleagues showed hemodilution during cardiopulmonary bypass to be an independent and strong risk factor for postoperative AKI [22]. Anemia during the postoperative course contributes to AKI development after cardiac surgery [23]. We observed this dependence, experiencing an accessory phenomenon in which men experienced more intensive hemodilution, but women suffering from AKI much more frequently. Mehta and colleagues described an opposite dependence, but in their study, the women were older than men and had significantly more comorbidities [24]. This indicates that gender independently influences the incidence of AKI.
In a propensity-matched cohort as seen in this study, there were no preoperative differences that could be ascribed to gender.
Regarding the limitations in the exercise capacity during the follow-up, there were no differences between genders. The low number of patients in NYHA classes III and IV after the surgery was also remarkable. However, 29.2% of the patients reported a subjective worsening of exertion tolerance after hospital discharge, compared with the time before ACS.
The reason behind the missing answers to our questionnaire is unknown, but we assume that it is similar for both genders. The incidence of repeat revascularization was comparable to that in the literature [25].
The identified risk factors, such as age, reduced eGFR, active infection, or shock severity associated with in-hospital and long-term mortality are not surprising. Any active infection during surgery is very important and often presents an underestimated factor that strongly reduces survival rates. CAD morphology did not seem to matter in patients with CS. This finding was quite unlike those from the stable patients from the EXCEL trial [26]. The duration of catecholamine support also showed no connections with outcomes.
The type of ACS influences the short- and long-term survival in a typical way. Patients with STEMI are at higher risk of short -term mortality, however failing to be significant in the long-term. This dependence is well-documented in the literature [27]. NSTEMI at presentation does not affect the short-term survival, but worsens the long-term prognosis. This pattern was also observed by other investigators [28].
Conclusions
Gender did not influence short- and long-term mortality in patients with ACS-induced CS. It also did not affect postoperative limitations in exercise capacity. CAD morphology did not influence outcomes in shock patients. Being a female was an independent risk factor for postoperative AKI. Even less intense hemodilution or anemia makes women more prone to AKI. Men are more likely to develop pericardial tamponade than women. However, it is a complication that seldom occurs.
Limitations
Our study was limited by its retrospective nature. Some preoperative data like precise information about former PCI procedures or stent-related stenoses are missing. The limitations in physical activity within the follow-up were subjectively assessed by patients, and the answer rate was relatively low (58.8%); therefore, the result of the questionnaire can only support conclusions based on hard data.
References
van Diepen S, Katz JN, Albert NM, et al. Contemporary management of cardiogenic shock: a scientific statement from the American Heart Association. Circulation. 2017;136:e232–68.
Thiele H, Ohman EM, Desch S, Eitel I, de Waha S. Management of cardiogenic shock. Eur Heart J. 2015;36:1223–30.
Tharmaratnam D, Nolan J, Jain A. Management of cardiogenic shock complicating acute coronary syndromes. Heart. 2013;99:1614–23.
Moosvi AR, Gheorghiade M, Goldstein S, Khaja F. Management of cardiogenic shock complicating acute myocardial infarction: The Henry Ford Hospital experience and review of the literature. Henry Ford Hosp Med J. 1991;39:240–4.
Wong SC, Sleeper LA, Monrad ES, et al. Absence of gender differences in clinical outcomes in patients with cardiogenic shock complicating acute myocardial infarction. A report from the SHOCK Trial Registry. J Am Coll Cardiol. 2001;38:1395–401.
Karlson BW, Herlitz J, Hartford M. Prognosis in myocardial infarction in relation to gender. Am Heart J. 1994;128:477–83.
Kassambara A, Kosinski M. Survminer: drawing survival curves using 'ggplot2'. R package version 0.4.2. 2018. https://cran.r-project.org/package=survminer.
R-Development-Core-Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2008. http://www.r-project.org/.
Kurmani S, Squire I. Acute heart failure: definition, classification and epidemiology. Curr Heart Fail Rep. 2017;14:385–92.
Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64:e139–228.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure – definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis. Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–12.
Leviner DB, Torregrossa G, Puskas JD. Incomplete revascularization: what the surgeon needs to know. Ann Cardiothorac Surg. 2018;7:463–9.
Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138:e618–e651.
Watson TJ, Ong PJL, Tcheng JE, editors. Primary angioplasty: a practical guide. Chapter 16. Role of coronary artery bypass surgery in acute myocardial infarction. Singapore: Springer. 2018.
Katircibasi MT, Kocum HT, Baltali M, et al. Effect of female gender on the outcome of coronary artery bypass surgery for left main coronary artery disease. Anadolu Kardiyol Derg. 2007;7:134–9.
Swaminathan RV, Feldman DN, Pashun RA, et al. Gender differences in in-hospital outcomes after coronary artery bypass grafting. Am J Cardiol. 2016;118:362–8.
Sadowski M, Gutkowski W, Raczynski G, Gierlotka M, Polonski L. Mortality in cardiogenic shock complicating acute myocardial infarction due to left main coronary artery disease: does gender matter? Przegl Lek. 2014;71:117–21.
Fengler K, Fuernau G, Desch S, et al. Gender differences in patients with cardiogenic shock complicating myocardial infarction: a substudy of the IABP-SHOCK II-trial. Clin Res Cardiol. 2015;104:71–8.
Weitzman LB, Tinker WP, Kronzon I, Cohen ML, Glassman E, Spencer FC. The incidence and natural history of pericardial effusion after cardiac surgery--an echocardiographic study. Circulation. 1984;69:506–11.
Assali AR, Moustapha A, Sdringola S, et al. Acute coronary syndrome may occur with in-stent restenosis and is associated with adverse outcomes (the PRESTO trial). Am J Cardiol. 2006;98:729–33.
Neugarten J, Sandilya S, Singh B, Golestaneh L. Sex and the Risk of AKI following cardio-thoracic surgery: A meta-analysis. Clin J Am Soc Nephrol. 2016;11:2113–22.
Ranucci M, Pavesi M, Mazza E, et al. Risk factors for renal dysfunction after coronary surgery: the role of cardiopulmonary bypass technique. Perfusion. 1994;9:319–26.
Ng RR, Chew ST, Liu W, Shen L, Ti LK. Identification of modifiable risk factors for acute kidney injury after coronary artery bypass graft surgery in an Asian population. J Thorac Cardiovasc Surg. 2014;147:1356–61.
Mehta RH, Castelvecchio S, Ballotta A, Frigiola A, Bossone E, Ranucci M. Association of gender and lowest hematocrit on cardiopulmonary bypass with acute kidney injury and operative mortality in patients undergoing cardiac surgery. Ann Thorac Surg. 2013;96:133–40.
Chikwe J, Lee T, Itagaki S, Adams DH, Egorova NN. Long-term outcomes after off-pump versus on-pump coronary artery bypass grafting by experienced surgeons. J Am Coll Cardiol. 2018;72:1478–86.
Gershlick AH, Kandzari DE, Banning A, et al. Outcomes after left main percutaneous coronary intervention versus coronary artery bypass grafting according to lesion site: results from the EXCEL trial. JACC Cardiovasc Interv. 2018;11:1224–33.
Marceau A, Samson J, Laflamme N, Rinfret S. Short and long-term mortality after STEMI versus Non-STEMI: A systematic review and meta-analysis. J Am Coll Cardiol. 2013;61:S8–S14.
Ren L, Ye H, Wang P, Cui Y, Cao S, Lv S. Comparison of long-term mortality of acute ST-segment elevation myocardial infarction and non-ST-segment elevation acute coronary syndrome patients after percutaneous coronary intervention. Int J Clin Exp Med. 2014;7:5588–92.
Funding
This work was not financially supported.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Our study was approved by the local Ethics Committee of the Heidelberg University, Germany. Number of the approval: S-570/2016. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Ethics statement regarding human and animal rights
The study was conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national). This article does not contain any studies with animal subjects performed by the any of the authors.
Informed consent
The consent for the follow-up is a routine at admission in our clinic. The consent for processing of retrospectively collected clinical data and for publication of the results is not required because the personal data were anonymized, and the article does not include images or data that may identify the person.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Szczechowicz, M.P., Mkalaluh, S., Torabi, S. et al. Gender and coronary artery bypass grafting in cardiogenic shock. Indian J Thorac Cardiovasc Surg 36, 580–590 (2020). https://doi.org/10.1007/s12055-020-00982-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-020-00982-5