Abstract
In the present study, the anti-inflammatory action of lysophosphatidylethanolamine (lysoPtdEtn), orally administered, in zymosan A-induced peritonitis was examined. Oral administration of 2-DHA-lysoPtdEtn (ED50, ~111 μg/kg) or 2-ARA-lysoPtdEtn (ED50, 221 μg/kg) was found to inhibit the plasma leakage in mice treated with zymosan A. In support of this, 2-polyunsaturated acyl-lysoPtdEtn diminished the formation of LTC4, a lipid mediator responsible for vascular permeability. Next, 2-DHA-lysoPtdEtn (ED50, 110 μg/kg) or 2-ARA-lysoPtdEtn (ED50, 123 μg/kg) effectively inhibited the leukocyte extravasation into the peritoneum. Consistent with this, each polyunsaturated-lysoPtdEtn diminished the formation of LTB4 and 12-HETE, potent chemotactic factors. Additionally, the level of pro-inflammatory mediator (IL-1 β, IL-6, TNF-α or NO) was lowered remarkably in contrast to the augmentation of anti-inflammatory interleukin IL-10. Furthermore, 2-(15-HETE)-lysoPtdEtn and 2-(17-HDHE)-lysoPtdEtn, 15-lipoxygenation product of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn, respectively, were more potent than corresponding lysoPtdEtn, suggesting the action of 2-acyl-lysoPtdEtn might be expressed through 15-lipoxygenation. In support of this, the formation of 15-HETE and LXA4 was upgraded in accordance with an increasing dose of 2-ARA-lysoPtdEtn. Separately, anti-inflammatory actions, 2-polyunsaturated acyl-lysoPtdEtns also drastically diminished leukocyte infiltration in a later phase of zymosan A-induced peritonitis, indicating that these lipids also possess pro-resolving activity. Taken together, it is suggested that polyunsaturated lysoPtdEtns and their lipoxygenation derivatives, could be classified as potent anti-inflammatory lipids.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammation is defined as a part of complex biological responses of vascular tissue toward exogenous harmful stimuli [1]. It becomes apparent that inflammation, normally results from an excessive inflammatory response or failure of resolution [2], is recognized as a causative in various diseases such as atherosclerosis, cancer, or asthma, and some neuropathological disorders such as Alzheimer’s disease or Parkinson’s disease. Additionally, lipid-derived mediators have proved to actively participate in the inflammation process and cooperate with others components in regulating the biological response to inflammation [3]. During the time course of inflammation, the lipid mediator could switch from a pro-inflammatory class such as prostaglandins and leukotrienes in the initial phase to biosynthesis of an anti-inflammatory and pro-resolving class including resolvin D series, resolvin E series, protectin D [4], maresin [5] in the resolution phase.
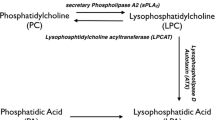
Lysophospholipid is a bioactive lipid class that plays important roles in the physical function and pathological conditions in the human body [6, 7]. Whereas the biological function of lysophosphatidylcholine (lysoPtCho), an abundant lysophospholipid in vivo, in inflammation it has been extensively studied and proved to be dependent upon the length and unsaturation degree of fatty acyl group [8, 9], the biological action of lysoPtdEtn, presents in human serum at a level of about several hundred ng mL−1, has been still unknown [10] except that the report that lysoPtdEtn expressed a potent anti-inflammatory activity in colitis induced by rectal administration of ethanol and trinitrobenzene sulfonic acid in rats [11]. Our recent works have proved that polyunsaturated-lysoPtCho, containing omega-3 or omega-6 fatty acid and its hydroxyl derivatives possess potent anti-inflammatory properties in vivo as well as in the in vitro model [8, 9, 12]. Anti-inflammatory activity of polyunsaturated lysoPtCho was suggested to be due to the combination effect of lysoPtCho itself and its metabolites. Moreover, 15-hydroxy derivative or 17-hydroxy derivative, derived from the sequential action of 15-LOX [13, 14] and GSH-peroxidase [15] on 1-ARA-lysoPtCho and 1-eicosapentaenoyl-lysoPtCho or 1-DHA-lysoPtCho, respectively, proved to possess more potent anti-inflammatory activity than their corresponding lysoPtCho suggesting that 15-lipoxygenase might be crucial for the anti-inflammatory effect of polyunsaturated lysoPtChos. However, the lysoPtCho form had been reported to be cytotoxic at relative small concentrations, in contrast to lysoPtdEtn which was less cytotoxic [16, 17]. Separately, it was reported that 18:0a/15S-HETE-PE potently inhibited cytokine generation in human monocytes, providing more evidence for anti-inflammatory activity of phosphatidylethanolamine (PtdEtn) in vitro [18]. However, it is still questionable whether polyunsaturated-lysoPtdEtn could express anti-inflammatory activity as observed with polyunsaturated acyl lysoPtCho. In this study we examined the anti-inflammatory actions of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn, their corresponding oxygenation products, 2-(15-HETE)-lysoPtdEtn and 2-(17-HpDHE)-lysoPtdEtn, respectively, to elucidate the mechanism responsible for their anti-inflammatory actions.
Materials and Methods
C18 (plasm)-22:6 PtEtn and C18 (plasm)-20:4 PtEtn, arachidonic acid (ARA), docosahexaenoic acid (DHA) (purity, 99%) were procured from Avanti Polar Lipids Inc. (Alabaster, Alabama, USA). All the enzyme were from the Sigma Company, unless otherwise indicated. Soybean lipoxygenase-1 (Type I-B), zymosan A (Z4250-1G) (Saccharomyces cerevisiae) were purchased from Sigma-Aldrich Corp. (St. Louis, MO, USA). 12/15-lipoxygenase (porcine leukocyte, 135.6 units/ml), 15-lipoxygenase-2 (human recombinant, 250 units/ml), 15-LOX inhibitor (PD 146176), EIA assay kits for prostaglandin E2 (PGE2), 15-HETE, leukotriene B4 (LTB4), leukotriene C4 (LTC4), and the nitrate/nitrite colorimetric assay kit were from Cayman Chemical (Ann Arbor, MI, USA). Lipoxin A4 (LXA4) and 12-HETE were from Oxford Biochemical Research Corp. (Box 522, Oxford, MI, USA) and Assay Designs Corp., respectively. The EIA assay kit for 12-HETE was supplied by Assay Design Inc. (Ann Arbor MI, USA). ELISA assay kits for cytokines (TNF-α, IL-1β, IL-4, IL-6 and IL-10) were obtained from eBioscience, Inc. (Science Center Drive, San Diego, USA).
Preparation of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn
2-DHA-lysoPtdEtn and 2-ARA-lysoPtdEtn were from the acidic hydrolysis of C18 (plasm)-22:6 PE and C18 (plasm)-20:4 PE, respectively according to a previous report with slight modification [19]. Briefly, PE was suspended in a mixture of 2.5 M HCl (0.8 ml), methanol (2 ml) and chloroform (1 ml) for 20 min at room temperature with vigorous stirring. Hydrolysis products were extracted from the reaction mixtures by the method of Bligh and Dyer and further purified by TLC on silica gel 60 plate, which was developed with a mobile solvent system (chloroform: methanol: H2O; 65:25:4). Eventually, the band containing lysoPtdEtn was scraped off, extracted with methanol and kept at −80 °C until used.
Preparation of 2-(15-HETE)-lysoPtdEtn and 2-(17-HDHE)-lysoPtdEtn
2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn (200 μM) was oxidized by soybean LOX-1B (4 KU/ml) in 5 ml of borax buffer (50 mM, pH 9.0) for 1 h. Then, hydroperoxide was subsequently reduced to the corresponding hydroxide by addition of SnCl2 (1 mM) with vigorous stirring for 10 min at room temperature. The hydroxide derivative product was extracted using the Bligh and Dyer method [9, 20] and further purified by RP-HPLC using Zorbrax eclipse XDB C18 column (5 μm, 50 × 4.6 mm, Agilent Technologies, USA) with an isocratic solvent system (ACN: water: formic acid; 60:40:0.1) [21]. The amount of 1-(15-HEPE)-lysoPtdEtn or 2-(17-HDHE)-lysoPtdEtn was determined by measuring absorbance of purified lipid at 234 nm using E 1m,1cm = 28,000, and the lipids were stored at −80 °C until used [18]
Determination of Kinetic Values in LOXs-Catalyzed Oxygenation of 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn
Oxygenation of 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn by LOXs was monitored via the increase in absorbance at 234 nm according to the formation of conjugated diene. In the kinetic study, lysoPtdEtns (0–20 μM) were incubated with soybean LOX-1B (2.5 units/ml), porcine leukocyte 12/15 LOX (1 unit/ml), or human 15-LOX-2 (1 unit/ml) in 50 mM borax buffer (pH 9.0), 50 mM phosphate buffer (pH 7.4) containing 5 mM EDTA and 0.03% Tween 20, or 50 mM Tris–HCl buffer (pH 7.2) containing 0.003% Tween 20, respectively. The kinetic parameters, Km and Vm, were determined by Linwear–Burk plot analysis as previously reported [9]. One unit of LOX activity was defined as the amount of LOX that can produce one nanomole of conjugated diene per min.
Identification of Oxygenation of 2-docosahexaenoyl-lysoPtdEtn or 2-ARA-lysoPtdEtn by Soybean 15-LOX Using LC/ESI-MS
Soybean 15-LOX-1B (10 units/ml) was incubated with either 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn (100 μM) in 500 μl of 5 mM borax buffer (pH 9.0). After 30 min incubation at room temperature, the reaction products (30 μl) were directly analyzed by LC/ESI-MS which was performed using a MSDI spectrometer (HP 1100 series LC/MSA, Hewlett Packard, USA), equipped with a Zorbrax eclipse XDB C18 column (5 μm, 50 × 4.6 mm, Agilent Technologies, Washington, USA). The LC–MS solution was utilized for data collection and manipulation. The oxidized product was eluted (0.5 ml/min) with an isocratic solvent system of 60% solvent B [0.1% formic acid/acetonitrile in solvent A (0.1% formic acid/methanol], and the eluent was monitored at 234 nm, full-scan mass spectra were obtained within the range of m/z 400–700, and the data acquisition was conducted in both negative and positive modes. The condition for EIS–MS analysis of HPLC peak included a capillary voltage of 200 V, a drying gas flow of 1.5 mL/min, and a temperature of 200 °C.
Animal Experiment
ICR mice (4–6 weeks of age, 29–30 g body weight) were procured from Koatech Co., Korea, and housed in cages (10 mice per cage) under viral antibody-free conditions. Mice were fed with standard food (Sangyang Co., Korea) that containing no less than 4.5% total fat with 0.26% omega-3 fatty acid and <0.01% ARA acid. All animal experiments were conducted according to the Guide for Care and Use of Laboratory Animals of the National Research Council (NRC, 1996), which was approved by the Committee of Animal Care and Experiment of Chungnam National University, Korea.
Zymosan A-Induced Peritonitis in ICR Mice
Peritonitis was stimulated by i.p. administration of zymosan A (1 mg/mouse) as described previously [22–24]. For the measurement of plasma leakage, mice were treated orally with 200 μl of each lysoPtdEtn taken from ethanol stock solution and diluted in PBS buffer (final ethanol concentration <0.5%), 60 min prior to i.p. administration (1 mg/mouse) of zymosan A, and 100 μl of 0.5% Evans Blue dye, dissolved in PBS, was intravenously injected just prior to zymosan A injection [25, 26]. Sixty minutes later, unless otherwise indicated, mice were killed using isoflurane inhalation, and peritoneal lavage was performed with 3 ml of ice cold PBS. Then, cells were centrifuged out of the lavage fluid. Finally, Evans blue dye extravasation amount was determined by measuring the absorbance of supernatants at 610 nm, and normalized with a standard curve [22, 23, 27]. Separately, in order to measure leukocyte infiltration, lipids were administered 60 min prior to i.p administration of zymosan A. Four hours after zymosan A injection, peritoneal lavage was taken, and total cells in the lavage fluid was enumerated using light microscopy with trypan blue staining [22, 28]. In an attempt to evaluate the effect of 15-LOX inhibitor (PD146176) [29] on the pharmacological activity of polyunsaturated lysoPtdEtns, mice were treated orally with 2-ARA-lysoPtdEtn or 2-docosahexaenoyl-lysoPtdEtn (50–150 μg/kg), followed by i.p. administration of PD146176, a specific 15-LOX inhibitor, 60 min prior to intra-peritoneal administration of zymosan A (1 mg/mice) and eventually, leukocyte infiltration was assessed as described above.
Determination of Inflammatory Lipid Mediators or Cytokine Level in Peritoneal Lavage Fluid
To determine the level of pro-inflammatory lipid mediators in exudates, 1 ml of peritoneal lavage fluid was transferred to micro-centrifuge tubes and centrifuged (15,000 rpm, 3 min). Supernatants were used directly for enzyme immunoassay (EIA) analysis of PGE2, LTB4, LTC4, 12-HETE, 15-HETE, or LXA4 level as described before [24, 30]. Whereas levels of pro-inflammatory (IL-1β, IL-6, TNF-α) or anti-inflammatory cytokines (IL-4, IL-10) were determined by ELISA assay according to the manufacturer’s instructions. Additionally, the content of nitric oxide (NO) in the lavage fluid was quantitated by a nitrate/nitrite colorimetric assay kit supplied by Cayman Chemical Company (Ann Arbor, MI, USA).
Statistical Analysis
Data were calculated and displayed as means ± SEM. Group comparisons were performed using one-way analysis of variance (ANOVA) followed by Neuman Keuls multiple comparison test or Student’s t test where appropriate; with P value ≤ 0.05 was considered as statistically significant (sufficient to reject the null hypothesis).
Results
Identification of Product from 15-LOX-catalyzed Oxygenation of 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn
The formation of 2-(15-HpETE)-lysoPtdEtn and 2-(17-HpDHE)-lysoPtdEtn, 15-LOX-catalyzed oxidation products of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn, respectively, was analyzed by LC–ESI–MS using both the positive and negative mode. Figure 1 shows that a peak with a retention time of 1.6 min (Inset, Fig. 1a) appeared as a predominant product possessing the mass spectrum of a compound corresponding to hydroperoxy derivative of 2-ARA-lysoPtdEtn (Fig. 1a); mass-to-charge ratio (m/z) at 532 (M–H)− in negative scan mode, and 500 (M + H–H2O–O)+, 516 (M + H–H2O)+, 534 (M + H)+, 556 (M + Na)+, and 572 (M + K)+ in positive scan mode (Fig. 1b). Likewise, as shown in Fig. 1c, d, the mass spectrum of the major peak (RT, 1.7 min) (Inset, Fig. 1c) including molecular ions indicative of hydroperoxy derivative of 2-DHA-lysoPtdEtn had been obtained; m/z at 556 (M–H)− in negative scan mode, and 524 (M + H–H2O–O)+, 540 (M + H–H2O)+, 558 (M + H)+, 580 (M + Na)+, and 596 (M + K)+ in positive scan mode [31]. Therefore, it was suggested that soybean LOX effectively converted 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn into their corresponding 15-hydroperoxy derivative products.
LC/ESI–MS analysis of products from soybean 15-LOX catalyzed oxidation of 2-ARA-lysoPtdEtn (a, b) or 2-DHA-lysoPtdEtn (c, d). The hydroperoxide derivative obtained from 30 min-incubation of soybean 15-LOX with 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn (100 μM) in 500 μl of 5 mM borax buffer (pH 9.0) was directly analyzed by LC/ESI-MS as described in “Materials and Methods”. The representative mass spectra of a major peak with retention time of 1.6 and 1.7 min (inset of a and b), respectively were obtained by the ESI–MS system using negative scan mode (a, b) and positive scan mode (c, d)
Determination of Kinetic Values in Oxygenation of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn by Various LOXs
As 15-lipoxygenation had been known to be required for anti-inflammatory action of polyunsaturated lysoPtCho [12], the oxygenation of 2-polyunsaturated acyl-lysoPtdEtn by different LOXs was examined. When 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn was incubated with 15-LOXs (soybean LOX-1, leukocyte 12/15-LOX or human recombinant 15-LOX-2), a time-dependent increase in absorbance at 234 nm was observed, indicating the formation of a conjugated diene (data not shown). Subsequently, the kinetic values for oxygenation of 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn by 15-LOX were determined from Lineweaver–Burk plot analysis, and compared to those for ARA or DHA. As displayed in Table 1, the most favorable substrate in case of soybean LOX-catalyzed oxygenation was found to be 2-DHA-lysoPtdEtn, showing catalytic efficacy (Vm/Km) value of 30.4 units/μg/μM, which was approximately ninefold higher than that of DHA (Vm/Km, 3.5 units/μg/μM). Meanwhile, 2-ARA-lysoPtdEtn demonstrated a Vm/Km value of 10.9 units/μg/μM, which was larger than that of ARA (Vm/Km, 7.4 units/μg/μM). Similarly, when the oxygenation of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn by human 15-LOX-2 was analyzed, the Vm/Km values for 2-DHA-lysoPtdEtn and 2-ARA-lysoPtdEtn were estimated to be 48.2 and 14.8 units/μg/μM, respectively, which were about 8- and 1.5-fold higher than that of DHA and ARA, respectively. Thus, it was demonstrated that 2-DHA-lysoPtdEtn and 2-ARA-lysoPtdEtn were more effective substrates than DHA and ARA, respectively, for human recombinant 15-LOX-2. Finally, in the oxygenation by leukocyte 12-LOX, the Vm/Km value for 2-ARA-lysoPtdEtn was estimated to be 10.3 units/μg/μM, which was found to be two times larger than that of ARA (Vm/Km, 4.5 units/μg/μM). Taken all together, it was suggested that 2-polyunsaturated acyl-lysoPtdEtn is a more effective substrate than the acid form in 12-LOX or 15-LOX-catalyzed oxygenation. Nonetheless, 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn were not oxygenated significantly by murine recombinant 12-lipoxygenase from platelets (data not shown).
Prevention by 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn Against Zymosan A-Induced Plasma Leakage
Increased vascular permeability caused by reversible opening of endothelial cells tight junction, followed by the leak of protein and fluids from the vascular compartment into the extravascular compartment, is one predominant event in acute inflammation. In order to see anti-inflammatory actions of 2-ARA-lysoPtdEtn or 2-docosahexaneoyl-lysoPtdEtn in acute inflammation, we investigated the effect of lysoPtdEtn, orally administered, on zymosan A-induced vascular permeability based on the extravasation of Evans Blue dye as marker. As shown in Fig. 2, both 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn, orally administered, 60 min prior to zymosan A treatment (i.p., 1 mg/mouse) dose-dependently decreased zymosan A-induced plasma leakage in ICR mice. Oral intake of 2-ARA-lysoPtdEtn at doses of 50 and 150 μg/kg suppressed the plasma leakage by 17 and 36%, respectively, while that of 2-DHA-lysoPtdEtn at doses of 50 and 150 μg/kg caused ~42 and ~58% reduction of plasma leakage, respectively. The 50% effective dose (EC50) for 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn was estimated to be about 221 and 111 μg/kg, respectively. By contrast, no remarkable inhibition of plasma was expressed by oral intake of DHA up to 150 μg/kg (data not shown), suggesting the structural importance of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn.
Prevention by 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn against zymosan A-induced plasma leakage. 2-ARA-lysoPtdEtn (filled) or 2-DHA-lysoPtdEtn (blank) (50 or 150 μg/kg), diluted in ice cold PBS, was administered orally to mice, 1 h prior i.p. administration of zymosan A (1 mg/mouse), followed by intravenous injection of Evans blue (5% in PBS, 100 μl/mouse). Two hours later, plasma leakage was determined by measuring the absorbance of cell free-supernatant of lavages at 610 nm, and calculating the amount of Evans blue using a standard curve of known concentrations of the dye. The value was expressed as the percentage of the sample value of the value of the zymosan A-treated group. Result are presented as means ± SEM (n = 5). #, P < 0.001 when compared to PBS-treated group; *, P < 0.05 and; **, P < 0.01 when compared to zymosan A-treated group
Effect of the 15-LOX Inhibitor, administrated i.p., on Anti-inflammatory Action of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn in Zymosan A-Induced Leukocyte Infiltration
Leukocyte extravasation is a subsequent event after the reversible opening of the endothelial cell tight junction at the onset of acute inflammation [32]. Therefore, in order to examine the ability of polyunsaturated lysoPtdEtn to regulate zymosan A-induced inflammation, the effect of 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn on zymosan A-induced leukocyte infiltration was investigated. As displayed in Fig. 3, 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn, orally administered, significantly (P < 0.05) prohibited the zymosan A-induced migration of leukocytes into the peritoneum in dose-dependent fashion; 2-ARA-lysoPtdEtn and 2-DHA at 150 μg/kg decreased total leukocyte infiltration by 56 and 60%, respectively, compared with the group challenged with zymosan A alone, suggesting that two lysoPtdEtn derivatives were potent inhibitors of leukocyte trafficking. The EC50 values for 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn were estimated to be about 123 and 110 μg/kg, respectively. However, such anti-inflammatory actions of 2-DHA-lysoPtdEtn or 2-ARA-lysoPtdEtn were completely reversed by concomitant treatment with PD146176, a specific 15-LOX inhibitor (Fig. 3), indicating that the action of 2-DHA-lysoPtdEtn or 2-ARA-lysoPtdEtn might be expressed mainly through the 15-LOX-induced oxygenation pathway.
Effect of 15-LOX inhibitor on anti-inflammatory action of 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn in zymosan A-induced leukocyte extravasation. Mice were orally given 2-ARA-lysoPtdEtn (filled) or 2-DHA-lysoPtdEtn (blank) (50 or 150 μg/kg) concurrently with or without PD146176 (i.p., 100 μg/mouse), 60 min prior i.p. administration of zymosan A (1 mg/mouse). Peritoneal lavages were collected after 4 h, and the total number of leukocyte was enumerated utilizing light microscopy after staining with trypan blue dye. Results are mean ± SEM. (n = 5). #, P < 0.001 when compared to PBS-treated group; *, P < 0.05; **, P < 0.01 when compared to zymosan A-treated group; †, P < 0.05, significant difference between treated groups
Suppressive Effect of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn on Zymosan A-Induced Formation of Pro-inflammatory Lipid Mediator in Peritoneum
In separate experiments, to investigate the mechanism responsible for the inhibitory effect of 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn on plasma leakage as well as leukocyte infiltration, the effect of 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn on zymosan A-induced formation of pro-inflammatory or anti-inflammatory lipid mediators was assessed. As displayed in Fig. 4a, oral administration of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn significantly reduced zymosan A-induced formation of LTC4 with EC50 values of about 132 and 84 μg/kg, respectively. Thus, 2-DHA-lysoPtdEtn was more potent than 2-ARA-lysoPtdEtn in suppressing the formation of LTC4, an important vascular permeability inducer. Furthermore, Fig. 4b indicated that the formation of LTB4, a potent chemo-attractant lipid, was also diminished by 2-ARA-lysoPtdEtn (EC50, 139 μg/kg) and 2-DHA-lysoPtdEtn (EC50, 211 μg/kg) in a dose-dependent manner, supporting the notion that the reduction of LTB4 formation might be related to the suppressive effect of 2-polyunsaturated acyl-lysoPtdEtn on zymosan A-induced leukocyte extravasation. Additionally, the amount of 12-HETE, another chemo-attractant lipid mediator was also dose-dependently reduced by 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn (Fig. 4c), supporting the idea that the decrease of 12-HETE level might at least partially account for the suppressive effect of 2-polyunsaturated acyl-lysoPtdEtn on vascular permeability. Especially, 2-DHA-lysoPtdEtn almost completely inhibited 12-HETE formation at dose of 150 μg/kg. However, no significant alternation of PGE2 level was observed after the treatment with 2-polyunsaturated acyl-lysoPtdEtn (not shown), suggesting that suppression of PGE2 might not be responsible for the anti-inflammatory action of 2-polyunsaturated acyl-lysoPtdEtn.
Suppressive effect of 2-ARA-lysoPtdEtn or 2-docosahexaenoyl-lysoPtdEtn on zymosan A-induced pro-inflammatory lipid mediator formation in mice. Mice were orally given 2-ARA-lysoPtdEtn (filled) or 2-DHA-lysoPtdEtn (blank) (15–150 μg/kg) 60 min prior to administration of zymosan A (i.p., 1 mg/mouse). Peritoneal lavages were collected at 4 h and the level of pro-inflammatory lipid mediator in cell-free supernatant was assessed by an EIA kit according to the manual. Each sample was determined in duplicate. Results are means ± SEM (n = 5). #, P < 0.001 when compared to the PBS-treated group; *, P < 0.05; **, P < 0.01 when compared to zymosan A-treated group
Effect of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn on Zymosan A-Induced Formation of Pro-inflammatory or Anti-inflammatory Cytokine
Production of both pro-inflammatory cytokines (e.g. IL-1, IL-6, TNF-α) and anti-inflammatory cytokines such as IL-10 is essential in the control of inflammation [1]. Here, we monitored a panel of cytokines in the exudate to assess whether 2-polyusaturated acyl-lysoPtdEtn could regulate their levels. Four hours after zymosan A treatment, most cytokine was dramatically up-regulated, compared to the control (Fig. 5). Of interest, 2-ARA-lysoPtdEtn and 2-docosahexaenoyl-lysoPtdEtn dose-dependently reduced the levels of pro-inflammatory cytokine including TNF-α, IL-1β or IL-6, while showing no significant effect on other pro-inflammatory cytokines such as IL-2 or IFN-γ (not shown). In the meantime, oral administration of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn caused a dose-dependent elevation of anti-inflammatory cytokine, IL-10. Noticeably, 2-DHA-lysoPtdEtn and 2-ARA-lysoPtdEtn (150 μg/kg) increased the IL-10 level by approximately four- and five-fold, respectively, compared to the zymosan A-challenged group (P < 0.05).
Effect of 2-ARA-lysoPtdEtn or 2-docosahexaenoyl-lysoPtdEtn on zymosan A-induced pro-inflammatory and anti-inflammatory cytokine formation. Mice were orally given 2-ARA-lysoPtdEtn (filled) or 2-DHA-lysoPtdEtn (blank) (15–150 μg/kg) 60 min prior administration of zymosan A (i.p., 1 mg/mouse). Peritoneal lavages were collected at 4 h, and the cytokine level in cell-free supernatant was assessed by ELISA assay kit according to manufactures’ protocol. Results are means ± SEM (n = 5). #, P < 0.001 when compared to PBS-treated group; *, P < 0.05; **, P < 0.01 when compared to the zymosan A-treated group
Suppressive Effect of 2-polyunsaturated Acyl-lysoPtdEtn on Zymosan A-Induced NO Production in Plasma Leakage
Nitric oxide (NO) plays a key role in the inflammation process especially including regulation of inflammatory cell transmigration into the inflamed site and up-regulation of vascular permeability In zymosan A-induced peritonitis, NO is produced by activated macrophages and eventually be oxidized within few second to nitrite or nitrate [33]. Therefore, to examine whether 2-polyusaturated acyl-lysoPtdEtn could attenuate the level of NO, we determined the amount of NO formation in exudate. As expected, 2-DHA-lysoPtdEtn as well as 2-ARA-lysoPtdEtn, orally administered, drastically suppressed zymosan A-induced NO production in ICR mice (Fig. 6). Interestingly, 2-DHA-lysoPtdEtn (50 μg/kg) almost completely suppressed the NO formation caused by zymosan A stimulation; 2-ARA-lysoPtdEtn at 50 and 150 μg/kg diminished the NO level by 60 and 70%, respectively. Taken all together, it was suggested that at least some part of inflammatory action of 2-polyunsaturated lysoPtdEtn was ascribed to the inhibition of NO production.
Suppressive effects of 2-ARA-lysoPtdEtn and 2-docosahexaenoyl-lysoPtdEtn on zymosan A-induced formation of NO in mice. Mice were orally given 2-ARA-lysoPtdEtn (filled) or 2-DHA-lysoPtdEtn (blank) (15–150 μg/kg), 60 min prior to administration of zymosan A (i.p., 1 mg/mouse). Peritoneal lavages were collected at 4 h and the NO level in cell-free supernatant was measured by colorimetric assay according to the manufacturer’s protocol. Results are means ± SEM (n = 5). #, P < 0.001 when compared to PBS-treated group; *, P < 0.05; **, P < 0.01 when compared to the zymosan A-treated group
Suppressive Effect of 2-(15-HETE)-lysoPtdEtn and 2-(17-HDHE)-lysoPtdEtn on Zymosan A-Induced Plasma Leakage and Leukocyte Infiltration
In a subsequent experiment, we elucidated which metabolic pathway is crucial for the anti-inflammatory action of 2-polyunsaturated acyl-lysoPtdEtn. Since 15-LOX activity, but not COX activity, was crucial for the anti-inflammatory action of 2-polyunsaturated lysoPtdEtn (Figs. 3, 4), we investigated the anti-inflammatory effect of 2-(15-HETE)-lysoPtdEtn and 2-(17-HDHE)-lysoPtdEtn, derived from 15-LOX-oxygenation of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn, respectively, on zymosan A-induced peritonitis. As demonstrated in Fig. 7a, plasma leakage induced by zymosan A was suppressed by 2-(15-HETE)-lysoPtdEtn (EC50, ~48 μg/kg) and 2-(17-HDHE)-lysoPtdEtn (EC50, 42 μg/kg) in a dose-dependent manner. Of notice, Fig. 7b indicated that EC50 of 2-(15-HETE)-lysoPtdEtn and 2-(17-HDHE)-lysoPtdEtn was estimated to be about ~42 and 28 μg/kg, respectively. Especially, 2-(15-HETE)-lysoPtdEtn and 2-(17-HDHE)-lysoPtdEtn, orally administered at a dose as low as 50 μg/kg could almost completely suppress leukocyte infiltration. In comparison, it was found that the suppression effect of 2-(15-HETE)-lysoPtdEtn and 2-(17-HDHE)-lysoPtdEtn on leukocyte infiltration was more potent than that of 2-ARA-lysoPtdEtn (EC50, ~123 μg/kg) and 2-DHA-lysoPtdEtn (EC50, ~110 μg/kg), respectively (P < 0.01), indicating that oxidized derivatives were more potent than the corresponding polyunsaturated acyl lysoPtdEtn in expressing anti-inflammatory action in vivo. Taken together, these data indicate that 15-LOX oxygenation products of 2-polyunsaturated acyl-lysoPtdEtn could be active metabolites directly responsible for the anti-inflammatory action in vivo.
Suppressive effect of hydroxyl derivatives of polyunsaturated acyl-lysoPtdEtn on zymosan A-induced plasma leakage or leukocyte infiltration. 2-(15-HETE)-lysoPtdEtn (filled) or 2-(17-HDHE)-lysoPtdEtn (blank) was orally administered to mice 60 min prior to the zymosan A challenge (1 mg/mouse; i.p.). Plasma leakage (a) and total leukocyte migration (b) was determined according to the methods described in Figs. 2 and 3, respectively. Results are means ± SEM (n = 5). #, P < 0.001 when compared to PBS-treated group; *, P < 0.05; **, P < 0.01, ***, P < 0.001 when compared to the zymosan A-treated group
Effect of 2-ARA-lysoPtdEtn on the Formation of 15-HETE and LXA4 in the Peritoneum of Mice
Previously, lysophospholipids administered to mice, were reported to be hydrolyzed by lipase activity [9] to release the hydrolysis product which in turn was converted to an active anti-inflammatory metabolite [12]. With this in mind, we examined the possible formation of 15-HETE and LXA4 from 2-ARA-lysoPtdEtn in peritoneal exudate after oral administration of 2-ARA-lysoPtdEtn. Figure 8 indicates that oral administration of 2-ARA-lysoPtdEtn causes an increase in the level of 15-HETE (Fig. 8a) and LXA4 (Fig. 8b) in the exudate; 2-ARA-lysoPtdEtn at 15, 50 and 150 μg/kg enhances 15-HETE level by approximately 3.5-, 5- and 9-fold, respectively, and the LXA4 level by about 2-, 4- and 5.5-fold, respectively. However, the formation of 15-HETE was not significant in the exudate from mice administered with 2-ARA-lysoPtd in combination with PD146176 (100 μg/mouse) (data not shown). Separately, the 4 h hydrolysis of the exudate sample in 1 N NaOH was carried out to see the possible reincorporation of the 15-HETE product into the phospholipids. As illustrated in Fig. 8a, the amount of 15-HETE in hydrolyzed samples, obtained from alkaline hydrolysis of peritoneal exudates was apparently greater than that in the corresponding non-hydrolyzed samples, suggesting that some part of 15-lipoxygenation products of 2-ARA-lysoPtdEtn, could exist as the lysophospholipid or phospholipid form. In contrast, there was no alteration of the 15-HETE level irrespective of alkaline hydrolysis in peritoneal samples from mice treated orally with 2-DHA-lysoPtdEtn up to 150 μg/kg (data not shown). From this, it was supposed that some part (<40%) of 15-HETE might be deposited in the lysophospholipid or phospholipid. The presence of lysophospholipid- and phospholipid-bound 15-HETE could provide a support for the 15-lipoxygenation of polyunsaturated acyl-lysoPtdEtn in vivo. Nonetheless, it is not excluded that free 15-HETE was reincorporated into the phospholipid.
Dose-dependent effect of 2-ARA-lysoPtdEtn on the level of 15-HETE or LXA4 before or after alkaline hydrolysis of the exudate from mice. Mice were orally treated with 2-ARA-lysoPtdEtn, 60 min prior to administration of zymosan A (i.p., 1 mg/mouse). The exudate samples were collected at 120 min after zymosan A treatment, and then 15-HETE (a) or LXA4 (b) in non-hydrolyzed (filled) or 1 N NaOH-hydrolyzed sample (blank) was extracted and determined by EIA kit according to manual. Results are means ± SEM (n = 5). #, P < 0.01 when compared to the PBS-treated group; *, P < 0.05; **, P < 0.01, ***, P < 0.001 when compared to the zymosan A-treated group; +, P < 0.05 was the significant difference between groups
Oral Administration of 2-Polyunsaturated Acyl-lysoPtdEtn Induced Resolution of Zymosan A Induced Peritonitis
In order to see whether 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn could attenuate the resolution of zymosan A-induced peritonitis, we examined the effect of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn on zymosan A-induced leukocyte infiltration in ICR mice. In our previous data [9], it was observed that the total number of leukocytes infiltrated reached a maximum approximately 12 h after zymosan A treatment. Therefore, 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn was administered 12 h after zymosan A treatment to see their effect on the resolution phase in zymosan A-induced peritonitis. As shown in Fig. 9, 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn, orally administered at the peak of inflammation (12 h post-zymosan A treatment), effectively decreased the total leukocyte infiltration at the time points of 15, 20 and 24 h, whereas 2-ARA-lysoPtdEtn produced ~23, 21 and 33% reduction of total leukocyte number, respectively, 2-DHA-lysoPtdEtn gave approximate 29, 33 and 44% reduction. In summary, it is suggested that 2-polyunsaturated acyl-lysoPtdEtn accelerates the resolution of zymosan A-induced peritonitis.
Induction of resolving zymosan A-induced peritonitis by 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn. Mice were i.p. administered with zymosan A (1 mg/mouse) alone (triangles ) or with either 2-ARA-lysoPtdEtn (open circles) or 2-DHA-lysoPtdEtn (closed circles) (12 h after zymosan A treatment). At the indicated periods, peritoneal lavage samples were collected and the total number of leukocyte infiltrated was enumerated according to the method described in Fig. 3. Results are means ± SEM (n = 5). *, P < 0.05; the 2-ARA-lysoPtdEtn-treated group vs. the zymosan A-treated group; †, P < 0.05, ††, P < 0.01, 2-DHA-lysoPtdEtn-treated group vs. zymosan A-treated group
Discussion
Nowadays, inflammation has been recognized as the central component of many prevalent diseases such as atherosclerosis, cancer, asthma, autoimmune disease, stroke, Alzheimer’s disease and Parkinson’s disease [1]. Interestingly, it now become apparent that inflammation is a dynamic process with the participation of new family of endogenous anti-inflammatory and pro-resolving lipid mediators such as resolvins, maresin and protectin derived from omega 3-polyunsaturated fatty acids [4, 5, 34]. These lipid mediators, actively biosynthesized in the resolution phase of acute inflammation, control the duration and magnitude of inflammation [4]. Whereas anti-inflammatory actions of lipid mediators, derived from polyunsaturated fatty acids and polyunsaturated lysoPtCho, have been well-established [3, 4, 8, 9, 12, 35], the biological function of polyunsaturated lysoPtdEtn derivatives in inflammation has not been clarified yet. Very recently, we found that oral administration of 1-DHA-lysoPtCho prevented zymosan A-induced peritonitis [13]. In our present study, it is proposed that 2-polyunsaturated acyl lysoPtdEtns also effectively suppresses acute inflammation induced by zymosan A.
It has been known that induction of vascular permeability and leukocyte infiltration are important events of biological response at the onset of acute inflammation [36]. In the present work, the anti-inflammatory action of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn was first substantiated by their effective prevention against zymosan A-induced plasma leakage with a potency similar to that of polyunsaturated lysoPtCho [12]. Such a potent effect is possibly associated with the suppressive effect of 2-acyl-lysoPtdEtn on the formation of LTC4 since early vascular permeability depends largely on cysteinyl-leukotriene (cysLT) released by resident peritoneal macrophages. Although vascular permeability is known to depend on PGE2 from multiple cellular origins in zymosan A-induced peritonitis [26, 37], the level of PGE2 was not altered by 2-polyunsaturated-lysoPtdEtn. Another mechanism possibly responsible for the anti-inflammatory action of polyunsaturated acyl lysoPtdEtns could be due to the decreased formation of NO, released from macrophages, which reversibly opens the endothelial cells tight junction leading to an enhancement of vascular permeability [33]. This might be partly supported by our present finding that the formation of NO in the peritoneum was reduced by 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn at relatively small doses.
In addition, the anti-inflammatory action of 2-polyunsaturated-lysoPtdEtn, represented by inhibition of leukocyte migration, could be related to the suppression of the formation of pro-inflammatory chemotactic lipid mediators. Support for this may come from the suppressive effect of 2-polyunsaturated-lysoPtdEtns on the formation of LTB4 [4] and 12-HETE [38, 39], two potent arachidonate-derived chemo-attractants responsible for leukocyte infiltration in the initial process of the inflammatory phase. Moreover, the levels of representative pro-inflammatory cytokines (TNF-α, IL-1β, IL-6), possessing chemo-attractant properties [1, 40] were significantly diminished by 2-polyunsaturated-lysoPtdEtns. Noteworthy is that 2-polyunsaturated acyl-lysoPtdEtn up-regulated IL-10, a potent anti-inflammatory cytokine, secreted by macrophage in acute inflammation, which showed a tonic inhibitory effect on the leukocyte migration and the formation of pro-inflammatory cytokine (TNF-α, IL-1β, IL-6) as well as chemokines (MCP-1, MIP-1α and MIP-2) in zymosan A peritonitis [41]. Additionally, IL-10 could block NF-kB activation by stabilization of IkBα [42, 43], and in turn, inhibit the induction of inducible nitric oxide synthetase (iNOS), resulting in decreased formation of nitric oxide (NO). Furthermore, activation of human monocyte and monocyte-derived dendritic cells by cysteinylated leukotrienes was down-regulated by IL-10 [44]. Collectively, IL-10 could extensively regulate zymosan A-induced peritonitis through both direct and indirect manners.
In previous studies we proved that 15-lipoxygenase activity was necessary for the anti-inflammatory function of 2-polyunsaturated acyl-lysoPtCho in zymosan A-induced peritonitis [8, 9]. Our present study also indicated that 15-lipoxygenase activity was crucial for the anti-inflammatory function of 2-polyunsaturated acyl-lysoPtdEtn, since PD146176, a specific inhibitor of 15-LOX, suppressed the effect of 2-polyunsaturated acyl-lysoPtdEtn on leukocyte infiltration. In support of this, 2-(15-HETE)-lysoPtdEtn and 2-(17-HDHE)-lysoPtdEtn were more potent as anti-inflammatory lipids than 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn, respectively, supporting the assumption that the hydroxyl derivatives might be more direct precursors for active metabolites accounting for the anti-inflammatory action of 2-polyunsaturated acyl-lysoPtdEtn in vivo.
A pathway for further metabolism for 2-polyunsaturated acyl-lysoPtdEtn might be a hydrolytic process since a lipase activity capable of hydrolyzing polyunsaturated lysophospholipids had been reported to be available in an in vivo system [9]. In support of this notion, the formation of 15-HETE in the peritoneum was augmented in accordance with an increasing dose of 2-ARA-lysoPtdEtn, and diminished by PD146176, a specific inhibitor for 15-LOX. Therefore, 15-HETE-lysoPtdEtn metabolite, generated from the oxygenation of 2-ARA-lysoPtdEtn, orally administered, by 15-LOX, could serve as a source for the 15-HETE supplement in vivo. Noteworthy, the 15-HETE level of 1 N NaOH-hydrolyzed sample was significantly higher than that of non-hydrolyzed sample, suggesting two possibilities; some part of 2-(15-HETE)-lysoPtdEtn was still not hydrolyzed by lipase activity or 15-HETE, released from 2-(15-HETE)-lysoPtdEtn, could be re-incorporated into the lipid or lysophospholipid by the lysophospholipid acyltransferase activity [45] in the in vivo condition. It had been previously reported that 15-HETE could be stored in the phospholipid, and the lipid after hydrolysis might be used as precursory substrate for LXA4 formation [46]. In this regard, the dose-dependent increase of LXA4 formation in the peritoneum after oral administration of 2-ARA-lysoPtdEtn may indicate that 15-HETE generated from 15-lipoxygenation of 2-ARA-lysoPtdEtn and subsequent enzymatic hydrolysis, was oxygenated by 5-LOX activity to produce 5-hydroperoxy, 15-hydroxyeicosatetraenoic acid, a direct precursor for LXA4 and LXB4 formation [47]. Likewise, it is quite possible that 2-DHA-lysoPtdEtn may be oxygenated to form 2-(17-hydroxyDHA)-lysoPtdEtn, which subsequently is hydrolyzed by a lipase activity to release 17-hydroxydocosahexaenoic acid (17-HDHE), a precursor for the formation of anti-inflammatory and proresolving lipid mediators such as protectin D [34] or resolvin D [32, 48]. Taken together, it is quite possible that the anti-inflammatory activity of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn in zymosan A-induced peritonitis is the consequence of bioactive oxygenated lipid mediators. Besides, an additional mechanism for anti-inflammatory activity of 2-polyunsaturated acyl-lysoPtdEtn was reported to be related to the inhibition of 5-LOX activity by 15-HETE [49], resulting in the reduction of LTB4 and LTC4 level, as well as the suppression of LTB4-evoked chemotaxis for leukocyte in acute inflammation [50]. Likewise, DHA [51] and 17-HDHE [52], generated from the metabolite of 2-DHA-lysoPtdEtn can indirectly or directly participate in the inhibition of 5-LOX activity, leading to the reduction of the leukotrienes level. As suggested from the present results, the anti-inflammatory action of 2-ARA-lysoPtdEtn in vivo might be at least partially ascribed to the effect of its oxygenated metabolites such as lipoxins (LXs). Previously, the anti-inflammatory activity of LXA4 through various mechanistic routes has been well-established. For instance, LXs inhibit leukocytes activation, chemotaxis, adhesion, transmigration, and pro-inflammatory mediator generation [53, 54]. Additionally, it also inhibits the increase in vascular permeability triggered by activated leukocytes [55, 56]. Additionally, LXA4 could diminish LTC4-induced vascular permeability [56]. Noteworthy, LXA4 formation could give an elevation of IL-10 level [57]. Meanwhile, the anti-inflammatory action of 2-DHA-lysoPtdEtn in vivo may be derived from the effect of its bioactive metabolites such as 17-HDHE or protectin D in vivo [27, 32]. 17-HDHE has been known to express the anti-inflammatory action through inhibition of the NF-κB pathway and down-regulation of 5-LOX expression in macrophages [52]. Besides, anti-inflammatory lipids such as protectin D1 or resolvin D [32, 48], presumably derived from the in vivo metabolism of 2-DHA-lysoPtdEtn, might be involved in its anti-inflammatory activity through suppression of leukocyte migration, down-regulation of pro-inflammatory cytokines, and inhibition of the NF-κB pathway. Since the anti-inflammatory effect of 2-DHA-lysoPtdEtn was almost completely reversed by a specific inhibitor of 15-LOX, it was suggested that maresin [5], formed via 12-LOX oxygenation pathway, might not be important for the anti-inflammatory action of 2-DHA-lysoPtdEtn [5]. Moreover, 2-DHA-lysoPtdEtn was not oxygenated by platelet 12-LOX (data not shown). Separately, the suppressive effects of 2-arachidonoyl-lysoPtdEtn and 2-DHA-lysoPtdEtn on leukocyte infiltration in the exudate in a later phase (12 h) of zymosan A-induced peritonitis may reflect their effects on pro-resolution through the removal of phagocytized cells [58]. Such a pro-resolving action of 2-polyunsaturated acyl-lysoPtdEtn may be related to the generation of bioactive metabolites such as LXA4, resolving or protectin, responsible for resolution of acute inflammation [59].
An alternative mechanism accountable for the anti-inflammatory action of 2-ARA-lysoPtdEtn or 2-DHA-lysoPtdEtn could be re-acylation of the corresponding oxygenation product; 15-HETE or 17-HDHE into phospholipids [18, 60]. In an earlier study, 18:0/15-HETE-phosphatidylethanolamine derivatives, generated from the re-acylation of 15-HETE into lysophospholipid, was reported to inhibit the release of pro-inflammatory cytokine from lipopolysaccharide-stimulated monocytes [18]. Another plausible mechanism for the anti-inflammatory actions of 2-polyunsaturated acyl-lysoPtdEtn in vivo may be from the inhibitory effect 15-HETE and 17-HDHE on 12-LOX activity, responsible for 12-HETE formation, as suggested from a strong inhibition of 12/15 LOX by 15-HETE and 17-HDHE [61]. In agreement with this, the present study has shown that oral administration of 2-ARA-lysoPtdEtn and 2-DHA-lysoPtdEtn, precursors for formation of 15-HETE and 17-HDHE, respectively, diminished the level of 12-HETE in the peritoneum dose-dependently. In turn, the reduction of 12-HETE could result in abrogation of pro-inflammatory cytokine levels and monocyte chemo-attractant protein (MCP-1) as had been reported previously [62–64]. Of note, the suppressive effect of 2-polyunsaturated acyl-lysoPtdEtns on zymosan A-induced 12-HETE formation in the present study was greater than that of 1-polyunsaturated acyl-lysoPtChos [9]. Taken together, the anti-inflammatory actions of 2-polyunsaturated acyl-lysoPtdEtn could be exerted through multiple mechanisms.
In conclusion, our present observations concerning the anti-inflammatory and pro-resolving activity of 2-polyunsaturated acyl-lysoPtdEtn may suggest that it can be a new anti-inflammatory lipid useful for the prevention as well as treatment of the zymosan A-induced peritonitis model. In future studies to expand its application, anti-inflammatory and pro-resolving activity of 2-polyunsaturated acyl-lysoPtdEtn is to be studied using other inflammation models. Furthermore, the structural design to obtain more stable derivatives of 2-polyunsaturated acyl-lysoPtdEtn should be also considered to broaden the practical use of 2-polyunsaturated acyl-lysoPtdEtn as an anti-inflammatory lipid agent.
Abbreviations
- 2-ARA-lysoPtdEtn:
-
1-Lyso-2-arachidonoyl-sn-glycero-3-phosphoethanolamine
- 2-DHA-lysoPtdEtn:
-
1-Lyso-2-docosahexaenoyl-sn-glycero-3-phosphoethanolamine
- 2-(15-HpETE)-lysoPtdEtn:
-
1-Lyso-2-15(S)-hydroperoxy-5,8,11,13-eicosatetraenoyl-sn-glycero-3-phosphoethanolamine
- 2-(15-HETE)-lysoPtdEtn:
-
1-Lyso-2-15(S)-hydroxy-5,8,11,13-eicosatetraenoyl-sn-glycero-3-phosphoethanolamine
- 2-(17-HDHE)-lysoPtdEtn:
-
1-Lyso-2-17(S)-hydroxy-4,7,10,13,15,19-docosahexaenoyl-sn-glycero-3-phosphoethanolamine
- 2-(17-HpDHE)-lysoPtdEtn:
-
1-Lyso-2-17-(S)-hydroperoxy-4,7,10,13,15,19-docosahexaenoyl-sn-glycero-3-phosphoethanolamine
- ARA:
-
Arachidonic acid
- DHA:
-
Docosahexaenoic acid
- 15-HETE:
-
15(S)-hydroxy-5,8,11,13-eicosatetraenoic acid
- 17-HDHE:
-
17-(S)-hydroxy-4,7,10,13,15,19-docosahexaenoic acid
- LTB4 :
-
Leukotriene B4
- LTC4 :
-
Leukotriene C4
- PGE2 :
-
Prostaglandin E2
- LXA4 :
-
Lipoxin A4
- ED50 :
-
50% Effective dose
- LOX:
-
Lipoxygenase
- TNF-α:
-
Tumor necrosis factor alpha
- IFN-γ:
-
Interferon gamma
- IL-1β:
-
Interleukin 1-beta
- IL-6:
-
Interleukin-6
References
Nathan C (2002) Points of control in inflammation. Nature 420:846–852
Gilroy DW, Lawrence T, Perretti M, Rossi AG (2004) Inflammatory resolution: new opportunities for drug discovery. Nat Rev Drug Discov 3:401–416
Serhan CN, Chiang N, Van Dyke TE (2008) Resolving inflammation: dual anti-inflammatory and pro-resolution lipid mediators. Nat Rev Immunol 8:349–361
Serhan CN, Savill J (2005) Resolution of inflammation: the beginning programs the end. Nat Immunol 6:1191–1197
Serhan CN, Yang R, Martinod K, Kasuga K, Pillai PS, Porter TF, Oh SF, Spite M (2009) Maresins: novel macrophage mediators with potent antiinflammatory and proresolving actions. J Exp Med 206:15–23
Schmitz G, Ruebsaamen K (2010) Metabolism and atherogenic disease association of lysophosphatidylcholine. Atherosclerosis 208:10–18
Ye XQ (2008) Lysophospholipid signaling in the function and pathology of the reproductive system. Hum Reprod Update 14:519–536
Huang LS, Hung ND, Sok DE, Kim MR (2010) Lysophosphatidylcholine containing docosahexaenoic acid at the sn-1 position is anti-inflammatory. Lipids 45:225–236
Hung ND, Kim MR, Sok DE (2011) Mechanisms for anti-inflammatory effects of 1-[15(S)-hydroxyeicosapentaenoyl] lysophosphatidylcholine, administered intraperitoneally, in zymosan A-induced peritonitis. Br J Pharmacol 162:1119–1135
Makide K, Kitamura H, Sato Y, Okutani M, Aoki J (2009) Emerging lysophospholipid mediators, lysophosphatidylserine, lysophosphatidylthreonine, lysophosphatidylethanolamine and lysophosphatidylglycerol. Prostaglandins Other Lipid Mediat 89:135–139
Sturm A, Zeeh J, Sudermann T, Rath H, Gerken G, Dignass AU (2002) Lisofylline and lysophospholipids ameliorate experimental colitis in rats. Digestion 66:23–29
Hung ND, Kim MR, Sok DE (2009) Anti-inflammatory action of arachidonoyl lysophosphatidylcholine or 15-hydroperoxy derivative in zymosan A-induced peritonitis. Prostaglandins Other Lipid Mediat 90:105–111
Huang LS, Kim MR, Sok DE (2007) Oxygenation of 1-docosahexaenoyl lysophosphatidylcholine by lipoxygenases; conjugated hydroperoxydiene and dihydroxytriene derivatives. Lipids 42:981–990
Huang LS, Kang JS, Kim MR, Sok DE (2008) Oxygenation of arachidonoyl lysophospholipids by lipoxygenases from soybean, porcine leukocyte, or rabbit reticulocyte. J Agric Food Chem 56:1224–1232
Huang LS, Kim MR, Sok DE (2009) Enzymatic reduction of polyunsaturated lysophosphatidylcholine hydroperoxides by glutathione peroxidase-1. Eur J Lipid Sci Tech 111:584–592
Olofsson KE, Andersson L, Nilsson J, Bjorkbacka H (2008) Nanomolar concentrations of lysophosphatidylcholine recruit monocytes and induce pro-inflammatory cytokine production in macrophages. Biochem Bioph Res Co 370:348–352
Wong JT, Tran K, Pierce GN, Chan ACOK, Choy PC (1998) Lysophosphatidylcholine stimulates the release of arachidonic acid in human endothelial cells. J Biol Chem 273:6830–6836
Morgan AH, Dioszeghy V, Maskrey BH, Thomas CP, Clark SR, Mathie SA, Lloyd CM, Kuhn H, Topley N, Coles BC, Taylor PR, Jones SA, O’Donnell VB (2009) Phosphatidylethanolamine-esterified eicosanoids in the mouse tissue localization and inflammation-dependent formation in th-2 disease. J Biol Chem 284:21185–21191
Tokumura A, Sinomiya J, Kishimoto S, Tanaka T, Kogure K, Sugiura T, Satouchi K, Waku K, Fukuzawa K (2002) Human platelets respond differentially to lysophosphatidic acids having a highly unsaturated fatty acyl group and alkyl ether-linked lysophosphatidic acids. Biochem J 365:617–628
Bligh EG, Dyer WJ (1959) A rapid method of total lipid extraction and purification. Can J Biochem Physiol 37:911–917
Yu S, Peng M, Ronis M, Badger T, Fang N (2010) Analysis of polar lipids in the serum from rats fed shiitake by liquid chromatography–mass spectrometry/mass spectrometry. J Agric Food Chem 58:12650–12656
Byrum RS, Goulet JL, Snouwaert JN, Griffiths RJ, Koller BH (1999) Determination of the contribution of cysteinyl leukotrienes and leukotriene b4 in acute inflammatory responses using 5-lipoxygenase- and leukotriene A4 hydrolase-deficient mice. J Immunol 163:6810–6819
Leite DFP, Echevarria-Lima J, Ferreira SC, Calixto JB, Rumjanek VM (2007) Abc transporter inhibition reduces zymosan-induced peritonitis. J Leukocyte Biol 82:630–637
Rao NL, Dunford PJ, Xue X, Jiang X, Lundeen KA, Coles F, Riley JP, Williams KN, Grice CA, Edwards JP, Karlsson L, Fourie AM (2007) Anti-inflammatory activity of a potent, selective leukotriene a4 hydrolase inhibitor in comparison with the 5-lipoxygenase inhibitor zileuton. J Pharmacol Exp Ther 321:1154–1160
Arita M, Bianchini F, Aliberti J, Sher A, Chiang N, Hong S, Yang R, Petasis NA, Serhan CN (2005) Stereochemical assignment, antiinflammatory properties, and receptor for the omega-3 lipid mediator resolvin E1. J Exp Med 201:713–722
Kolaczkowska E, Barteczko M, Plytycz B, Arnold B (2008) Role of lymphocytes in the course of murine zymosan-induced peritonitis. Inflamm Res 57:272–278
Sun YP, Oh SF, Uddin J, Yang R, Gotlinger K, Campbell E, Colgan SP, Petasis NA, Serhan CN (2007) Resolvin D1 and its aspirin-triggered 17r epimer. Stereochemical assignments, anti-inflammatory properties, and enzymatic inactivation. J Biol Chem 282:9323–9334
Bannenberg G, Moussignac RL, Gronert K, Devchand PR, Schmidt BA, Guilford WJ, Bauman JG, Subramanyam B, Perez HD, Parkinson JF, Serhan CN (2004) Lipoxins and novel 15-epi-lipoxin analogs display potent anti-inflammatory actions after oral administration. Brit J Pharmacol 143:43–52
Jeon SG, Moon HG, Kim YS, Choi JP, Shin TS, Hong SW, Tae YM, Kim SH, Zhu Z, Gho YS, Kim YK (2009) 15-lipoxygenase metabolites play an important role in the development of a T-helper type 1 allergic inflammation induced by double-stranded RNA. Clin Exp Allergy 39:908–917
Yuhki KI, Ushikubi F, Naraba H, Ueno A, Kato H, Kojima F, Narumiya S, Sugimoto Y, Matsushita M, Oh-Ishi S (2008) Prostaglandin I-2 plays a key role in zymosan-induced mouse pleurisy. J Pharmacol Exp Ther 325:601–609
Hui SP, Chiba H, Jin S, Nagasaka H, Kurosawa T (2010) Analyses for phosphatidylcholine hydroperoxides by lc/ms. J Chromatogr B 878:1677–1682
Serhan CN, Hong S, Gronert K, Colgan SP, Devchand PR, Mirick G, Moussignac RL (2002) Resolvins: a family of bioactive products of omega-3 fatty acid transformation circuits initiated by aspirin treatment that counter proinflammation signals. J Exp Med 196:1025–1037
Guzik TJ, Korbut R, Adamek-Guzik T (2003) Nitric oxide and superoxide in inflammation and immune regulation. J Physiol Pharmacol 54:469–487
Bazan NG (2009) Neuroprotectin D1-mediated anti-inflammatory and survival signaling in stroke, retinal degenerations, and Alzheimer’s disease. J Lipid Res 50(Suppl):S400–S405
Schwab JM, Chiang N, Arita M, Serhan CN (2007) Resolvin E1 and protectin D1 activate inflammation-resolution programmes. Nature 447:869–874
Medzhitov R (2008) Origin and physiological roles of inflammation. Nature 454:428–435
Kolaczkowska E, Shahzidi S, Seljelid R, van Rooijen N, Plytycz B (2002) Early vascular permeability in murine experimental peritonitis is co-mediated by resident peritoneal macrophages and mast cells: crucial involvement of macrophage-derived cysteinyl-leukotrienes. Inflammation 26:61–71
Goetzl EJ, Woods JM, Gorman RR (1977) Stimulation of human eosinophil and neutrophil polymorphonuclear leukocyte chemotaxis and random migration by 12-l-hydroxy-5,8,10,14-eicosatetraenoic acid. J Clin Invest 59:179–183
Kronke G, Katzenbeisser J, Uderhardt S, Zaiss MM, Scholtysek C, Schabbauer G, Zarbock A, Koenders MI, Axmann R, Zwerina J, Baenckler HW, van den Berg W, Voll RE, Kuhn H, Joosten LA, Schett G (2009) 12/15-lipoxygenase counteracts inflammation and tissue damage in arthritis. J Immunol 183(5):3383–3389
Van Assche G, Rutgeerts P (2005) Physiological basis for novel drug therapies used to treat the inflammatory bowel diseases—I. Immunology and therapeutic potential of antiadhesion molecule therapy in inflammatory bowel disease. Am J Physiol-Gastr L 288:G169–G174
Ajuebor MN, Das AM, Virag L, Flower RJ, Szabo C, Perretti M (1999) Role of resident peritoneal macrophages and mast cells in chemokine production and neutrophil migration in acute inflammation: Evidence for an inhibitory loop involving endogenous IL-10. J Immunol 162:1685–1691
Thelen M, Stein JV (2008) How chemokines invite leukocytes to dance. Nat Immunol 9:953–959
Malleo G, Mazzon E, Genovese T, Di Paola R, Caminiti R, Esposito E, Bramanti P, Cuzzocrea S (2008) Absence of endogenous interleukin-10 enhanced organ dysfunction and mortality associated to zymosan-induced multiple organ dysfunction syndrome. Cytokine 41:136–143
Woszczek G, Chen LY, Nagineni S, Shelhamer JH (2008) Il-10 inhibits cysteinyl leukotriene-induced activation of human monocytes and monocyte-derived dendritic cells. J Immunol 180:7597–7603
Brown WJ, Plutner H, Drecktrah D, Judson BL, Balch WE (2008) The lysophospholipid acyltransferase antagonist CI-976 inhibits a late step in copii vesicle budding. Traffic 9:786–797
Brezinski ME, Serhan CN (1990) Selective incorporation of (15s)-hydroxyeicosatetraenoic acid in phosphatidylinositol of human neutrophils—agonist-induced deacylation and transformation of stored hydroxyeicosanoids. Proc Natl Acad Sci USA 87:6248–6252
Schwab JM, Serhan CN (2006) Lipoxins and new lipid mediators in the resolution of inflammation. Curr Opin Pharmacol 6:414–420
Spite M, Norling LV, Summers L, Yang R, Cooper D, Petasis NA, Flower RJ, Perretti M, Serhan CN (2009) Resolvin D2 is a potent regulator of leukocytes and controls microbial sepsis. Nature 461(7268):1287–1291
Miller C, Yamaguchi RY, Ziboh VA (1989) Guinea pig epidermis generates putative anti-inflammatory metabolites from fish oil polyunsaturated fatty acids. Lipids 24:998–1003
Wu SH, Liao PY, Yin PL, Zhang YM, Dong L (2009) Elevated expressions of 15-lipoxygenase and lipoxin a(4) in children with acute poststreptococcal glomerulonephritis. Am J Pathol 174:115–122
Nauroth JM, Liu YC, Van Elswyk M, Bell R, Hall EB, Chung G, Arterburn LM (2010) Docosahexaenoic acid (DHA) and docosapentaenoic acid (DPAN-6) algal oils reduce inflammatory mediators in human peripheral mononuclear cells in vitro and paw edema in vivo. Lipids 45:375–384
Gonzalez-Periz A, Planaguma A, Gronert K, Miquel R, Lopez-Parra M, Titos E, Horrillo R, Ferre N, Deulofeu R, Arroyo V, Rodes J, Claria J (2006) Docosahexaenoic acid (DHA) blunts liver injury by conversion to protective lipid mediators: Protectin D1 and 17S-hydroxy-DHA. FASEB J 20:2537–2539
Maderna P, Godson C (2009) Lipoxins: revolutionary road. Br J Pharmacol 158:947–959
Filep JG, Zouki C, Petasis NA, Hachicha M, Serhan CN (1999) Anti-inflammatory actions of lipoxin A4 stable analogs are demonstrable in human whole blood: modulation of leukocyte adhesion molecules and inhibition of neutrophil-endothelial interactions. Blood 94:4132–4142
Takano T, Clish CB, Gronert K, Petasis N, Serhan CN (1998) Neutrophil-mediated changes in vascular permeability are inhibited by topical application of aspirin-triggered 15-epi-lipoxin A(4) and novel lipoxin B-4 stable analogues. J Clin Invest 101:819–826
Gronert K, Martinsson-Niskanen T, Ravasi S, Chiang N, Serhan CN (2001) Selectivity of recombinant human leukotriene D-4, leukotriene B-4, and lipoxin A(4) receptors with aspirin-triggered 15-epi-lxa(4) and regulation of vascular and inflammatory responses. Am J Pathol 158:3–9
Souza DG, Fagundes CT, Amaral FA, Cisalpino D, Sousa LP, Vieira AT, Pinho V, Nicoli JR, Vieira LQ, Fierro IM, Teixeira MM (2007) The required role of endogenously produced lipoxin A4 and annexin-1 for the production of IL-10 and inflammatory hyporesponsiveness in mice. J Immunol 179:8533–8543
Serhan CN (2008) Systems approach with inflammatory exudates uncovers novel anti-inflammatory and pro-resolving mediators. Prostag Leukotr Ess 79:157–163
Serhan CN (2007) Resolution phase of inflammation: novel endogenous anti-inflammatory and proresolving lipid mediators and pathways. Annu Rev Immunol 25:101–137
Matsumoto K, Morita I, Hibino H, Murota S (1993) Inhibitory effect of docosahexaenoic acid-containing phospholipids on 5-lipoxygenase in rat basophilic leukemia-cells. Prostag Leukotr Ess 49:861–866
Tsunomori M, Fujimoto Y, Muta E, Nishida H, Sakuma S, Fujita T (1996) 15-hydroperoxyeicosapentaenoic acid inhibits arachidonic acid metabolism in rabbit platelets more potently than eicosapentaenoic acid. Bba-Lipid Lipid Met 1300:171–176
Moreno JJ (2009) New aspects of the role of hydroxyeicosatetraenoic acids in cell growth and cancer development. Biochem Pharmacol 77:1–10
Chakrabarti SK, Cole BK, Wen YS, Keller SR, Nadler JL (2009) 12/15-Lipoxygenase products induce inflammation and impair insulin signaling in 3t3–l1 adipocytes. Obesity 17:1657–1663
Wen Y, Gu J, Chakrabarti SK, Aylor K, Marshall J, Takahashi Y, Yoshimoto T, Nadler JL (2007) The role of 12/15-lipoxygenase in the expression of interleukin-6 and tumor necrosis factor-alpha in macrophages. Endocrinology 148:1313–1322
Acknowledgments
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2010-0021372).
Conflict of interest
There is no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Hung, N.D., Kim, M.R. & Sok, DE. 2-Polyunsaturated Acyl Lysophosphatidylethanolamine Attenuates Inflammatory Response in Zymosan A-Induced Peritonitis in Mice. Lipids 46, 893–906 (2011). https://doi.org/10.1007/s11745-011-3589-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11745-011-3589-2