Abstract
Plasma concentration of lysophosphatidylcholine (LPC) was reported to decrease in patients with sepsis. However, the mechanisms of sepsis-induced decrease in plasma LPC levels are not currently well known. In mice subjected to cecal ligation and puncture (CLP), a model of polymicrobial peritoneal sepsis, we examined alterations in LPC-related metabolic parameters in plasma, i.e., the plasma concentration of LPC-related substances (i.e., phosphatidylcholine (PC) and lysophosphatidic acid (LPA)), and activities or levels in the plasma of some enzymes that can be involved in the regulation of plasma LPC concentration (i.e., secretory phospholipase A2 (sPLA2), lecithin:cholesterol acyltransferase (LCAT), acyl-CoA:lysophosphatidylcholine acyltransferase (LPCAT), and autotaxin (ATX)), as well as plasma albumin concentration. We found that levels of LPC and albumin and enzyme activities of LCAT, ATX, and sPLA2 were decreased, whereas levels of PC, LPA, and LPCAT1–3 were increased in the plasma of mice subjected to CLP. Bacterial peritonitis led to alterations in all the measured LPC-related metabolic parameters in the plasma, which could potentially contribute to sepsis-induced decrease in plasma LPC levels. These findings could lead to the novel biomarkers of sepsis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Lysophosphatidylcholine (LPC), an endogenous lysophospholipid, has various regulatory effects on immune cells [1–4]. Plasma concentration of LPC is about 100 μM, mostly bound to albumin [5]. As shown in Fig. 1, sources of plasma LPC include hydrolysis of phosphatidylcholine (PC) by secretory phospholipase A2 (sPLA2) or lecithin:cholesterol acyltransferase (LCAT) [6–10]. LPC, in turn, is hydrolyzed to lysophosphatidic acid (LPA) in the plasma by autotaxin (ATX) [11, 12]. LPA can also be synthesized from phosphatidic acid (PA) by sPLA2 [11, 13, 14]. In phospholipid remodeling pathway, LPC is converted to PC via reacylation by acyl-CoA:lysophosphatidylcholine acyltransferase (LPCAT) in various tissues [15–20].
Plasma LPC levels decrease in septic patients compared with healthy controls [21, 22]. Further, there is a positive association between the decrease in plasma LPC level and the lethality of septic patients [21, 23]. However, the mechanisms of sepsis-induced decrease in plasma LPC levels are not currently well known. Thus, the present study was designed to examine alterations of LPC-related metabolic parameters in the plasma of septic mice, to understand the mechanisms of sepsis-induced decrease in plasma LPC levels.
We found that levels of LPC and albumin and enzyme activities of LCAT, ATX, and sPLA2 were decreased, whereas levels of PC, LPA, and LPCAT1–3 were increased, in the plasma of mice subjected to cecal ligation and puncture (CLP), a model of polymicrobial peritoneal sepsis. These alterations could potentially contribute to sepsis-induced decrease in plasma LPC levels. Further, these findings could lead to the novel biomarkers of sepsis.
MATERIALS AND METHODS
Animals
Male ICR mice at the age of 5 weeks (26∼28 g body weight) were used. The procedures for animal experiments were approved by the Animal Experimentation Committee at Hallym University.
Animal Model of Sepsis
Cecal ligation and puncture (CLP) was done according to the previously reported method [24]. Mice were anesthetized with intra-peritoneal injection of pentobarbital (50 mg/kg), and a small abdominal midline incision was made and the cecum was exposed. The cecum was mobilized and ligated below the ileocecal valve, punctured through both surfaces twice with a 21-gauge needle, and the abdomen was closed. Up to 24 h post-CLP, the lethality was 4.3% (3/69). Sham procedure was the same as CLP, except for ligation and puncture of the cecum. The LPC, LPA, or vehicle groups (Fig. 5b) were treated subcutaneously with 10 mg/kg of 18:0 LPC, 18:0 LPA (Cayman Chemical Company, Ann Arbor, USA), or vehicle (PBS containing 2% BSA), respectively, two times at 12-h intervals beginning 2 h after CLP.
Measurements of LPC, PC, and LPA
Blood was collected sequentially from each mouse at 6, 12, and 24 h after CLP (n = 7 (sham), 12 (CLP) for LPC; n = 5 (sham), 7 (CLP) for PC; n = 4–5 (sham), 7–8 (CLP) for LPA) via retro-orbital plexus using heparinized capillary tubes. At 0 h, five (Fig. 2a, b) and four (Fig. 4a) naïve mice were used. Concentrations of LPC, PC, and LPA were measured with an enzyme colorimetric assay kit (Alfresa Pharma Corporation, Osaka, Japan), an enzymatic assay kit (Cayman Chemical Company, Ann Arbor, USA), and an enzyme-linked immunoassay kit (Echelon Bioscience Inc., Salt Lake City, USA), respectively.
Alteration of LPC-related metabolism in the plasma of mice subjected to CLP. Alteration in the level of LPC (a) and PC (b), and the decrease of enzymatic activity of LCAT (c) and sPLA2 (d) in the plasma of mice subjected to CLP. Plasma of each group (sham or CLP) was collected 0, 6, 12, and 24 h post-CLP (a, b). Enzymatic activities of the plasma LCAT (c) and sPLA2 (d) were measured at 24 h after CLP. Data are expressed as mean ± SEM (a n = 7 (sham), 12 (CLP); b n = 5 (sham), 7 (CLP), at 0 h (for a, b) five naïve mice were used; c and d, n = 5; *P < 0.05, **P < 0.01, ***P < 0.001; compared to sham).
Measurement of LPCAT
Blood was collected from retro-orbital plexus using heparinized capillary tubes at 0 and 24 h after CLP (n = 8–10). Concentration of LPCAT was measured with an enzyme-linked immunoassay kit (USCN, Huston, USA).
Measurements of Activities of LCAT, sPLA2, and ATX
Plasma was collected at 24 h after CLP (n = 5). Activities of LCAT, sPLA2, and ATX were measured with an enzymatic fluorometric assay kit (Calbiochem, Darmstadt, Germany), an enzymatic assay kit (Cayman Chemical Company, Ann Arbor, USA), and ATX activity assay kit (Echelon, Bioscience Inc., Salt Lake City, USA), respectively. In addition, ATX levels were measured with an enzyme colorimetric assay kit (USCN, Huston, USA) using blood collected from retro-orbital plexus with heparinized capillary tubes at 0, 6, 12, and 24 h after CLP (n = 5–7).
Measurement of Albumin
Plasma of mice was collected at 24 h after CLP (n = 10). Concentration of albumin was measured with an enzyme-linked immunoassay kit (Abcam, Cambridge, USA).
Quantitative Real-Time PCR (qRT-PCR)
Tissue samples (brain, heart, lung, liver, kidney, thymus, spleen, and adrenal grand) were collected at 24 h after CLP (n = 4). Total RNA was isolated with TRIzol reagent (Invitrogen, San Diego, USA), and cDNA was synthesized with 1.5 μg of total RNA using iScript cDNA symthesis kit (BIO-RAD, Contra Costa, USA) according to the manufacturer’s instructions. Real-time PCR was performed using 1 μl of cDNA in a 20-μl reaction volume with the Rotor Q system and Universal SYBR Green Supermix (BIO-RAD, Contra Costa, USA). The temperature profile of the reaction was 95 °C for 30 s, 40 cycles of denaturation at 95 °C for 15 s, and annealing and extension at 60 °C for 30 s. The relative messenger RNA (mRNA) levels were normalized by GAPDH. Primers were taken from special designed QuantiTect Primer Assays (Qiagen, Hilden, Germany) with the following catalog and NCBI reference sequence numbers: Mm_Lpcat1_1_SG QuantiTect Primer Assay (QT00164465, NM_145376.5) for LPCAT1, Mm_Lpcat2_1_SG QuantiTect Primer Assay (QT00105896, NM_173014) for LPCAT2, Mm_Lpcat3_1_SG QuantiTect Primer Assay (QT00156681, NM_145130) for LPCAT3, and Mm_Gapdh_3_SG QuantiTect Primer Assay (QT01658692, NM_008084) for GAPDH. All quantitative data were analyzed by Rotor gene software (Qiagen, Hilden, Germany).
Treatment of RAW 264.7 Macrophages with Heat-Killed Escherichia coli (E. coli)
RAW 264.7 macrophages were incubated with PBS (vehicle) or heat-killed E. coli (DH5α). After 24 h, media were removed and RNA samples were collected. E. coli were heat-killed by incubation in PBS (9 CFU/ml, 90 °C, 1 h).
Statistical Analysis
All the statistical data were analyzed by Graphpad Prism 5.0 (Graphpad software). They were evaluated either by two-tailed Student’s t test or ANOVA with post hoc Bonferroni test. P < 0.05 was considered to indicate statistical significance.
RESULTS
Changes in Plasma Concentrations of LPC and PC in Mice Subjected to CLP
Some metabolic pathways related to LPC are shown in Fig. 1. First, we measured plasma levels of LPC and PC at 6, 12, and 24 h after sham or CLP operation in mice (Fig. 2a, b). At 0 h, five naïve mice were used. It is to be noted that plasma LPC, but not PC, concentration in the sham group significantly decreased by 21% compared with naïve mice, suggesting that surgical injury decreases plasma LPC concentration. In the CLP group, plasma LPC concentration was significantly decreased by 18, 30, and 26%, at 6, 12, and 24 h post-CLP, respectively, compared with the sham-operated control group (Fig. 2a). In contrast, plasma PC concentration was significantly increased by 20% at 24 h post-CLP, compared with the sham group (Fig. 2b).
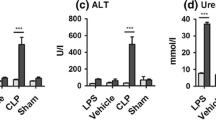
Effects of CLP on the Activities of LCAT and sPLA2 in Plasma
As we found alterations of LPC and PC concentration in the plasma of mice subjected to CLP (Fig. 2a, b), we next examined the activities of enzymes involved in the LPC synthesis, such as LCAT and sPLA2 (Fig. 1) at 24 h after CLP. As shown in Fig. 2c and d, activities of LCAT and sPLA2 in the plasma were decreased in mice subjected to CLP by 31 and 25%, respectively, at 24 h compared with the sham group. These data suggest that CLP-induced reduction in plasma LPC levels and increase in plasma PC levels (Fig. 2) could be, at least in part, due to the decreased plasma LCAT and sPLA2 activities.
CLP Induces an Increase in Plasma Levels of Lysophosphatidylcholine Acyltransferase (LPCAT)
LPCAT is involved in the conversion of LPC to PC (Fig. 1). Four types of LPCAT have been reported [15–18]. Plasma levels of LPCAT1, LPCAT2, LPCAT3, or LPCAT4 were measured at 24 h after CLP. Until now, the existence of LPCAT in the plasma has not been reported. It is to be noted that levels of all the four types of LPCAT are detectable in plasma; levels of LPCAT1 are most prominent, levels of LPCAT4 are barely detectible, and levels of LPCAT2 and LPCAT3 are in-between (Fig. 3a). Interestingly, we found that among the four types of LPCAT, levels of LPCAT1–3 were significantly increased in the plasma of mice subjected to CLP (fourfold, fivefold, and fourfold, respectively), compared with the sham group. These data suggest that the increased plasma LPCAT1–3 levels could also contribute to the decrease in LPC and the increase in PC levels in the plasma of CLP mice (Fig. 2).
Increase in the plasma levels of acyl-CoA:lysophosphatidylcholine acyltransferase (LPCAT) of mice subjected to CLP. a Plasma levels of LPCAT1–4 were measured at 24 h after CLP. Data are expressed as mean ± SEM (n = 8–10). b The expressions of mLPCAT1–3 in the brain, heart, lung, liver, kidney, thymus, spleen, and adrenal gland were analyzed by real-time PCR at 24 h after CLP. Data are expressed as mean ± SEM (n = 4). c The expressions of mLPCAT1–3 in RAW 264.7 macrophages incubated with PBS or heat-killed E. coli for 24 h (n = 6). *P < 0.05, **P < 0.01, ***P < 0.001).
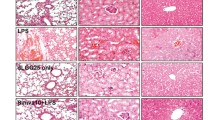
Effects of CLP on LPCAT mRNA Expression in Various Organs
As plasma LPCAT1–3 levels were increased in CLP mice (Fig. 3a), next we examined the source of the enhanced LPCAT expression by studying mLPCAT expression level in the various organs (brain, heart, lung, liver, kidney, thymus, spleen, and adrenal gland) of sham or CLP mice. As shown in Fig. 3b, in CLP mice, mLPCAT1 and mLPCAT3 expressions were increased in the liver and thymus but decreased in the adrenal gland, whereas mLPCAT2 expression was increased in the heart, liver, kidney and thymus. Among the eight organs we examined, the liver and thymus showed an increased expression of all the three mLPCAT1–3 (Fig. 3b).
Heat-Killed E. coli-Induced mLPCAT1 Expression in RAW 264.7 Macrophages
Next, we examined whether heat-killed E. coli induces mLPCAT expression in RAW 264.7 macrophages. As shown in Fig. 3c, mLPCAT1 expression was significantly increased by heat-killed E. coli. These data suggest that bacteria materials induce LPCAT expression and lead to increased plasma levels of mLPCAT1 in mice subjected to CLP.
Plasma LPA Level Increases in Mice Subjected to CLP
Next, we examined the plasma concentration of LPA, a metabolite of LPC, in mice subjected to CLP. As shown in Fig. 4a, the plasma concentration of LPA progressively increased time-dependently in CLP mice, reaching about tenfold increase (compared with 0 h when four naïve mice were used) at 24 h post-CLP. In contrast to LPC (Fig. 2a), sham operation did not affect plasma LPA concentration.
Alteration of LPA-related metabolism in the mice subjected to CLP. Increase of plasma LPA concentration in the mice subjected to CLP (a). Alterations of ATX level (b) and ATX activity (c and d) in mice subjected to CLP. Plasma LPA (a) and ATX (b) levels were measured at 6, 12, and 24 h after CLP by enzyme-linked immunoassay. At 0 h (for a, b), four naïve mice were used. ATX activities in the plasma (c) and the liver (d) were measured at 24 h after CLP. Data are expressed as mean ± SEM (n = 5–7 per group; *P < 0.05, ***P < 0.001).
Alteration in ATX Level and ATX Activity in CLP Mice
As ATX is involved in the conversion of LPC to LPA, ATX is an important regulator of plasma LPA concentration [11, 25–28]. Thus, we examined ATX activity to find whether it is increased in the plasma of mice subjected to CLP. As shown in Fig. 4b and c, however, plasma ATX level and activity were reduced by 13 and 40% at 24 h after CLP, respectively. However, ATX activity in the liver was significantly increased by 13% at 24 h after CLP (Fig. 4d).
Decrease in Plasma Albumin in Mice Subjected to CLP
LPC or ATX generally bind to albumin in plasma [5, 26, 29, 30]. Thus, altered plasma levels of LPC and ATX could be, at least in part, due to changes in the plasma albumin concentration. As the liver in the acute phase response, such as sepsis, is well known to switch from albumin to globulin synthesis, we examined whether plasma albumin levels are altered in mice subjected to CLP. As shown in Fig. 5a, plasma albumin level was decreased by 26% at 24 h after CLP, compared with the sham control group. These data suggest that reduction of plasma albumin level could substantially contribute to the decrease in LPC level or ATX level/activity in the plasma of mice subjected to CLP.
Alteration of plasma albumin level and no effect of LPC and LPA administration on plasma LPC level in mice subjected to CLP. Plasma albumin concentration was measured at 24 h after CLP by enzyme-linked immunoassay (a). No effect of LPC and LPA administrated subcutaneously on plasma LPC levels of mice subjected to CLP (b). Mice were treated subcutaneously with 10 mg/kg of LPC, LPA, or vehicle (PBS containing 2% BSA) two times at 12-h intervals beginning 2 h after CLP. All data are expressed as mean ± SEM (n = 7–10 per group; **P < 0.01, ***P < 0.001).
The Effect of LPC and LPA Administered Subcutaneously on Plasma LPC Levels in Mice Subjected to CLP
Next, we examined whether administration of the LPC or LPA could restore the decreased plasma LPC levels in mice subjected to CLP (Fig. 5b). Twice administrations of LPC or LPA at the dose of 10 mg/kg at 2 and 14 h after sham or CLP operation did not affect plasma LPC levels measured at 24 h post-sham or CLP operation.
DISCUSSION
In this study using mice subjected to CLP, we observed a significant decrease in plasma LPC levels (Fig. 2a), in line with the reports on human septic patients [21–23]. Interestingly, plasma levels of PC (Fig. 2b) and LPA (Fig. 4a) were significantly increased in mice subjected to CLP, which, as far as we know, have not been reported in septic animals or patients.
The increase in plasma LPA (Fig. 4a) is apparently contradictory to the increased LPCAT (Fig. 3), decreased LCAT (Fig. 2c), and decreased sPLA2 (Fig. 2d). Further, plasma ATX was decreased (Fig. 4b, c). Thus, these results suggest that the increase in plasma LPA levels at 24 h post-CLP does not depend on the plasma levels of these enzymes. The increase in ATX activity in the liver at 24 h post-CLP may be, at least in part, responsible for the plasma LPA increase at this time point. These results may reflect the limitation of the present study mostly focused on plasma levels of various enzymes.
Activity of LCAT, an enzyme involved in the conversion of PC to LPC (Fig. 1), was reportedly decreased in septic patients [31]. In line with this, mice subjected to CLP showed a decreased enzyme activity of plasma LCAT (Fig. 2c), which could contribute to the plasma LPC decrease in the same animals. Activity of plasma sPLA2, another enzyme involved in the conversion of PC to LPC (Fig. 1) has not yet been studied in sepsis. A significant decrease of sPLA2 activity at 24 h post-CLP (Fig. 2d) could also contribute to reduction of LPC in plasma of mice subjected to CLP.
Interestingly, plasma LPCAT1–3 levels were increased by CLP (Fig. 3a), with the accompanying enhancement of mRNA expression in some organs (Fig. 3c). Thus, the increase in plasma LPCAT1–3 could also contribute to the plasma LPC decrease in mice subjected to CLP. Further, heat-killed E. coli-induced mLPCAT1 expression in RAW 264.7 macrophages (Fig. 3c). As far as we know, this is the first report on the detection of plasma levels of LPCATs. Lipopolysaccharide-induced expression of LPCAT2 in mouse thioglycollate-induced macrophages has been reported [32]; however, this is the first report on the CLP-induced increase in plasma levels of LPCATs. Although the mechanisms of liberation of LPCATs, integral membrane proteins, to plasma remain to be clarified, plasma LPCAT1–3 could be useful biomarkers of sepsis.
ATX is the major enzyme synthesizing LPA in plasma [11, 28, 33, 34]. However, activity of plasma ATX was decreased at 24 h after CLP, while liver ATX activity was increased (Fig. 4). The opposite changes in ATX activity between plasma and liver at 24 h post-CLP remain to be explained. As ATX activity is inhibited by the high concentration of LPA [35], the more marked decrease in plasma ATX activity (40%) than plasma ATX level (13%) at 24 h after CLP (Fig. 4b, c) could be resulted from inhibition by high concentration (5 μM) of LPA (Fig. 4a).
Plasma albumin level decreased by 26% at 24 h after CLP compared with the sham group (Fig. 5a). Interestingly, the extent of the decrease in plasma LPC concentration at the same time point was exactly the same, i.e., 26% compared with the sham group (Fig. 2a), suggesting that the CLP-induced decrease in plasma albumin level could largely explain the CLP-induced decrease in plasma LPC level. However, for sepsis patients, the correlation between plasma albumin levels and plasma LPC levels was not reported to be evident [22]. Thus, the involvement of the various enzymes (LCAT, sPLA2, and LPCAT) in the CLP-induced decrease in plasma LPC levels cannot be excluded. For ATX, as it is also generally bound to plasma albumin, reduction of albumin (Fig. 5a) could also potentially contribute to the decrease of ATX level in plasma of mice subjected to CLP (Fig. 4c).
In summary, CLP induced an extensive change in the LPC-related parameters with nearly all the measured LPC-related parameters were changed. Novel findings in relation to CLP-induced changes include the increased plasma levels of PC, LPA, and LPCAT1–3, and the decreased enzyme activity of sPLA2. Although specific mechanisms need to be delineated for each of the phenomena, these alterations potentially could contribute to sepsis-induced decrease in plasma LPC levels. Furthermore, because early recognition and treatment are essential for the current therapy of sepsis, these novel CLP-induced plasma findings could lead to the development of useful biomarkers of sepsis.
References
Dial, E.J., D.M. Tran, J.J. Romero, M. Zayat, and L.M. Lichtenberger. 2010. A direct role for secretory phospholipase A2 and lysophosphatidylcholine in the mediation of LPS induced gastric injury. Shock 33(6): 634–638.
Schmid, B., M.J. Finnen, J.L. Harwood, and S.K. Jackson. 2003. Acylation of lysophosphatidylcholine plays a key role in the response of monocytes to lipopolysaccharide. European Journal of Biochemistry 270(13): 2782–2788.
Lin, P., E.J. Welch, X.-P. Gao, A.B. Malik, and R.D. Ye. 2005. Lysophosphatidylcholine modulates neutrophil oxidant production through elevation of cyclic AMP. Journal of Immunology 174(5): 2981–2989.
Yang, L.V., C.G. Radu, L. Wang, M. Riedinger, and O.N. Witte. 2005. Gi-independent macrophage chemotaxis to lysophosphatidylcholine via the immunoregulatory GPCR G2A. Blood 105(3): 1127–1134.
Thies, F., M.C. Delachambre, M. Bentejac, M. Lagarde, and J. Lecerf. 1992. Unsaturated fatty acids esterified in 2‐acyl‐1‐lysophosphatidylcholine bound to albumin are more efficiently taken up by the young rat brain than the unesterified form. Journal of Neurochemistry 59(3): 1110–1116.
Subramanian, V.S., J. Goyal, M. Miwa, J. Sugatami, M. Akiyama, M. Liu, and P.V. Subbaiah. 1999. Role of lecithin-cholesterol acyltransferase in the metabolism of oxidized phospholipids in plasma: Studies with platelet-activating factor-acetyl hydrolase- deficient plasma. Biochimica et Biophysica Acta 1439(1): 95–109.
Taniyama, Y., S. Shibata, S. Kita, K. Horikoshi, H. Fuse, H. Shirafuji, Y. Sumino, and M. Fujino. 1999. Cloning and expression of a novel lysophospholipase which structurally resembles lecithin cholesterol acyltransferase. Biochemical and Biophysical Research Communications 257(1): 50–56.
Slotboom, A.J., and G.H. De Haas. 1970. Hydrolysis of phosphoglycerides by purified lipase preparations II. Preparation of unsaturated 2-monoacyl choline phosphoglycerides. Chemistry and Physics of Lipids 4(1): 30–36.
McKean, M.L., J.B. Smith, and M.J. Silver. 1981. Formation of lysophosphatidylcholine by human platelets in response to thrombin. Support for the phospholipase A2 pathway for the liberation of arachidonic acid. Journal of Biological Chemistry 256(4): 1522–1524.
Mehta, D., S. Gupta, S.N. Gaur, S.V. Gangal, and K.P. Agrawal. 1990. Increased leukocyte phospholipase A2 activity and plasma lysophosphatidylcholine levels in asthma and rhinitis and their relationship to airway sensitivity to histamine. The American Review of Respiratory Disease 142(1): 157–161.
Eder, A.M., T. Sasagawa, M. Mao, J. Aoki, and G.B. Mills. 2000. Constitutive and lysophosphatidic acid (LPA)-induced LPA production: Role of phospholipase D and phospholipase A2. Clinical Cancer Research 6(6): 2482–2491.
Lee, S., and K.R. Lynch. 2005. Brown recluse spider (Loxosceles reclusa) venom phospholipase D (PLD) generates lysophosphatidic acid (LPA). Biochemical Journal 391(2): 317.
Fourcade, O., M.F. Simon, C. Viodé, N. Rugani, F. Leballe, A. Ragab, B. Fournié, L. Sarda, and H. Chap. 1995. Secretory phospholipase A2 generates the novel lipid mediator lysophosphatidic acid in membrane microvesicles shed from activated cells. Cell 80(6): 919–927.
Brown, W.J., K. Chambers, and A. Doody. 2003. Phospholipase A2 (PLA2) enzymes in membrane trafficking: Mediators of membrane shape and function. Traffic 4(4): 214–221.
Chen, X., B.A. Hyatt, M.L. Mucenski, R.J. Mason, and J.M. Shannon. 2006. Identification and characterization of a lysophosphatidylcholine acyltransferase in alveolar type II cells. Proceedings of the National Academy of Sciences 103(31): 11724–11729.
Nakanishi, H., H. Shindou, D. Hishikawa, T. Harayama, R. Ogasawara, A. Suwabe, R. Taguchi, and T. Shimizu. 2006. Cloning and characterization of mouse lung-type acyl-CoA:lysophosphatidylcholine acyltransferase 1 (LPCAT1). Expression in alveolar type II cells and possible involvement in surfactant production. The Journal of Biological Chemistry 281(29): 20140–20147.
Soupene, E., H. Fyrst, and F.A. Kuypers. 2008. Mammalian acyl-CoA:lysophosphatidylcholine acyltransferase enzymes. Proceedings of the National Academy of Sciences 105(1): 88–93.
Zhao, Y., Y.Q. Chen, T.M. Bonacci, D.S. Bredt, S. Li, W.R. Bensch, D.E. Moller, M. Kowala, R.J. Konrad, and G. Cao. 2008. Identification and characterization of a major liver lysophosphatidylcholine acyltransferase. Journal of Biological Chemistry 283(13): 8258–8265.
Bridges, J.P., M. Ikegami, L.L. Brilli, X. Chen, R.J. Mason, and J.M. Shannon. 2010. LPCAT1 regulates surfactant phospholipid synthesis and is required for transitioning to air breathing in mice. Journal of Clinical Investigation 120(5): 1736–1748.
Moessinger, C., L. Kuerschner, J. Spandl, A. Shevchenko, and C. Thiele. 2011. Human lysophosphatidylcholine acyltransferases 1 and 2 are located in lipid droplets where they catalyze the formation of phosphatidylcholine. The Journal of Biological Chemistry 286(24): 21330–21339.
Drobnik, W. 2003. Plasma ceramide and lysophosphatidylcholine inversely correlate with mortality in sepsis patients. Journal of Lipid Research 44(4): 754–761.
Cho, W.H., T. Park, Y.Y. Park, J.W. Huh, C.-M. Lim, Y. Koh, D.K. Song, and S.-B. Hong. 2011. Clinical significance of enzymatic lysophosphatidylcholine (LPC) assay data in patients with sepsis. European Journal of Clinical Microbiology and Infectious Diseases 31(8): 1805–1810.
Park, D.W., D.S. Kwak, Y.Y. Park, Y. Chang, J.W. Huh, C.M. Lim, Y. Koh, D.-K. Song, and S.-B. Hong. 2014. Impact of serial measurements of lysophosphatidylcholine on 28-day mortality prediction in patients admitted to the intensive care unit with severe sepsis or septic shock. Journal of Critical Care 29(5): 882.e885–882.e811.
Yan, J.-J., J.-S. Jung, J.-E. Lee, J. Lee, S.-O. Huh, H.-S. Kim, K.C. Jung, J.-Y. Cho, J.-S. Nam, H.-W. Suh, Y.-H. Kim, and D.K. Song. 2004. Therapeutic effects of lysophosphatidylcholine in experimental sepsis. Nature Medicine 10(2): 161–167.
Bächner, D., M. Ahrens, N. Betat, D. Schröder, and G. Gross. 1999. Developmental expression analysis of murine autotaxin (ATX). Mechanisms of Development 84(1–2): 121–125.
Tokumura, A. 2002. Identification of human plasma lysophospholipase D, a lysophosphatidic acid-producing enzyme, as autotaxin, a multifunctional phosphodiesterase. The Journal of Biological Chemistry 277(42): 39436–39442.
Tokumura, A. 2004. Metabolic pathways and physiological and pathological significances of lysolipid phosphate mediators. Journal of Cellular Biochemistry 92(5): 869–881.
Kanda, H., R. Newton, R. Klein, Y. Morita, M.D. Gunn, and S.D. Rosen. 2008. Autotaxin, an ectoenzyme that produces lysophosphatidic acid, promotes the entry of lymphocytes into secondary lymphoid organs. Natural Immunity 9(4): 415–423.
Moolenaar, W.H., and A. Perrakis. 2011. Insights into autotaxin: How to produce and present a lipid mediator. Nature Reviews Molecular Cell Biology 12(10): 674–679.
Fulkerson, Z., T. Wu, M. Sunkara, C.V. Kooi, A.J. Morris, and S.S. Smyth. 2011. Binding of autotaxin to integrins localizes lysophosphatidic acid production to platelets and mammalian cells. Journal of Biological Chemistry 286(40): 34654–34663.
Barlage, S., D. Fröhlich, A. Böttcher, M. Jauhiainen, H.P. Müller, F. Noetzel, G. Rothe, C. Schütt, R.P. Linke, K.J. Lackner, C. Ehnholm, and G. Schmitz. 2001. ApoE-containing high density lipoproteins and phospholipid transfer protein activity increase in patients with a systemic inflammatory response. Journal of Lipid Research 42(2): 281–290.
Shindou, H., D. Hishikawa, H. Nakanishi, T. Harayama, S. Ishii, R. Taguchi, and T. Shimizu. 2007. A single enzyme catalyzes both platelet-activating factor production and membrane biogenesis of inflammatory cells. Cloning and characterization of acetyl-CoA:LYSO-PAF acetyltransferase. The Journal of Biological Chemistry 282(9): 6532–6539.
Morishige, J., K. Touchika, T. Tanaka, K. Satouchi, K. Fukuzawa, and A. Tokumura. 2007. Production of bioactive lysophosphatidic acid by lysophospholipase D in hen egg white. Biochimica et Biophysica Acta 1771(4): 491–499.
Umezu-Goto, M. 2002. Autotaxin has lysophospholipase D activity leading to tumor cell growth and motility by lysophosphatidic acid production. Journal of Cell Biology 158(2): 227–233.
van Meeteren, L.A. 2005. Inhibition of autotaxin by lysophosphatidic acid and sphingosine 1-phosphate. Journal of Biological Chemistry 280(22): 21155–21161.
Acknowledgements
This work was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) (grant number 2015R1D1A1A01058532) and Hallym University Research Fund (grant number HRF-201606-011).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The procedures for animal experiments were approved by the Animal Experimentation Committee at Hallym University.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ahn, WG., Jung, JS., Kwon, H. et al. Alteration of Lysophosphatidylcholine-Related Metabolic Parameters in the Plasma of Mice with Experimental Sepsis. Inflammation 40, 537–545 (2017). https://doi.org/10.1007/s10753-016-0500-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-016-0500-6