Abstract
Intracerebral haemorrhage (ICH) is responsible for disproportionately high morbidity and mortality rates. The most used ICH classification system is based on the anatomical site. We used SMASH-U, an aetiological based classification system for ICH by predefined criteria: structural vascular lesions (S), medication (M), amyloid angiopathy (A), systemic disease (S), hypertension (H), or undetermined (U). We aimed to correlate SMASH-U classification of our patients to the intra-hospital mortality rates. We performed a single centre retrospective study at the Santa Maria Della Misericordia Hospital, Perugia (Italy) including consecutive patients between January 2009 and July 2017 assigned with 431 ICD-9 (International Classification of Diseases-9). We classified the included patients using SMASH-U criteria, and we analysed the association between SMASH-U aetiology and ICH risk factors to the outcome defined as intra-hospital mortality, using multivariable logistic regression analysis. The higher intra-hospital mortality rate was detected in the systemic disease (36.1%), medication (31.5%), and undetermined (29.4%) groups. At multivariable analysis, medication and systemic disease groups resulted associated with the outcome (odds ratio 3.47; 95% CI 1.15–10.46; P = 0.02 and 3.64; 95% CI 1.47–9.01; P = 0.005, respectively). Furthermore, age and high NIHSS at admission resulted significantly associated with intra-hospital mortality (odds ratio 1.01; 95% CI 1–1.03; P = 0.04 and 1.12; 95% CI 1.03–1.22; P = 0.008, respectively). In our retrospective study, the aetiology-oriented classification system SMASH-U showed to be potentially predictive of intra-hospital mortality of acute haemorrhagic stroke patients and it may support clinicians in the acute ICH management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intracerebral haemorrhage (ICH) is defined by the American Stroke Association as “the rapid development of neurological signs and symptoms attributable to the accumulation of blood within the brain parenchyma or ventricles not caused by trauma”; it accounts for 10–20% of all strokes and it is responsible for disproportionately high morbidity and mortality rates worldwide [1,2,3].
The case fatality rate has been reported to be 40% at one month and 54% in one year. Moreover, only 12–39% of survivors regain functional independence [1,2,3]. Over the past decade, ICH case fatality rates have not substantially altered and only high-income countries registered an improvement in ICH 30 days’ mortality [2, 4]. Current international guidelines on the management of ICH recommend that ICH must be treated as a medical emergency: physicians need to carry out rapidly baseline ICH severity score and neuroimaging with brain Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) [5].
The most used classification of ICH is based on the anatomical location of the ICH, as follows:
-
Deep ICH represents almost 70% of ICH cases and involves the basal ganglia and internal capsule (35–70%), brain stem (5–10%) and cerebellum (5–10%);
-
Lobar ICH is 15–30% of ICH and is located in cortical–subcortical areas and follows a ‘‘lobar’’ pattern across one or multiple lobes of the brain [6, 7].
Although location can provide insight into possible aetiology (e.g. hypertensive ICH for deep location), it does not necessarily predict patient outcome [8]. To overcome this latter limitation, the aetiological based SMASH-U classification was developed and includes the following sub-groups: structural vascular lesions (S), medication (M), amyloid angiopathy (A), systemic disease (S), hypertension (H) or undetermined (U). To date, this classification system is widely deemed to be predictive of patients’ outcome [9].
In our single-centre study, we aimed to correlate SMASH-U classification of our patients to the intra-hospital mortality rates.
Methods
This retrospective, single-centre, observational study included consecutive ICH patients admitted to the Departments of Internal and Vascular Medicine, Stroke Unit, Internal Medicine, Neurology, Neurosurgery, Endocrinology and Metabolic Diseases, Geriatrics, Oncology, Haematology and Intensive Care Units at the “Santa Maria Della Misericordia” Hospital in Perugia (Italy) between 1st January 2009 and 31st March 2017. Initial recruitment included all patients with the diagnostic code of 431 ICD-9-CM, either at admission or discharge. This diagnostic code identifies cases of haemorrhage within the brain parenchyma. Whenever re-bleeding was detected between 2009 and 2017, the most recent episode was used for classification purposes.
The 2010 American Stroke Association definition of ICH was adopted: the rapid development of neurological signs and symptoms attributable to the accumulation of blood within the brain parenchyma or ventricles not caused by trauma.
Exclusion criteria were: primary subdural/epidural hematoma, traumatic ICH or haemorrhage due to cancer (non-vascular origin), primary subarachnoid haemorrhage (with or without ICH), haemorrhagic transformation of cerebral infarction (with or without thrombolysis).
Data regarding ICH risk factors were collected for each patient including age, sex and history of hypertension (BP > 140/90 mmHg twice before the stroke or patient currently under antihypertensive treatment), myocardial infarction (MI), previous ICH (year and location), diabetes mellitus (DM) (glycaemia ≥ 126 mg/dl pre-prandial on at least 2 examinations, ≥ 200 mg/dl post-prandial, HbA1c ≥ 6.5% or currently under hypoglycaemic treatment), atrial fibrillation (AF), and/or systemic diseases (thrombocytopenia, coagulation disorders, renal failure, liver disease).
Drug history was investigated for each patient focusing on Vitamin K-Antagonists (VKAs), direct oral anticoagulants (DOACs), heparin and antiplatelet agents.
We used the original SMASH-U flow-chart to classify the most likely cause for each patient’s ICH and we selected the risk factors, as causal ones, that could be best proven, such as structural malformations, coagulation disorders, and anticoagulation to those that cannot. We used the same definition of “hypertensive aetiology” used by Meretoja et al. [9], that is: most recent pre-ICH blood pressure ≥ 160/100 mmHg, either on or off antihypertensive therapy or, when pre-ICH blood pressure was not known, either mention of pre-ICH elevated blood pressure by a patient, relative, or medical records together with a left ventricular hypertrophy as a biomarker of hypertension, or any pre-ICH use of blood pressure medication. We used the Boston criteria to define amyloid angiopathy [9, 10].
Unlike the SMASH-U study, we included arteriovenous malformations (AVMs), cavernomas and aneurysms, in the structural vascular lesions group, whenever present with intra-parenchymal ICH. Patients on treatment with VKAs (regardless of their INR values), DOACs or antiplatelets, were included in the medication group.
Regarding the SMASH-U groups, although many concomitant factors can lead to ICH, we have selected for classification the factor that we supposed to be the most likely and evincible aetiology. For instance, structural vascular lesions, coagulopathies, and systemic diseases (such as severe thrombocytopenia) were preferred over hypertension and amyloid angiopathy.
Intra-hospital mortality rates were recorded for each patient included.
We examined any association using the 2-tailed Fisher-exact test, the Pearson χ2-test for categorical variables, and the Student’s t test for continuous variables.
We analysed the association between SMASH-U aetiology and ICH risk factors to intra-hospital mortality, using multivariable logistic regression analysis.
We included the following variables of interest in the logistic regression model: structural lesions, medication, amyloid angiopathy, systemic disease, undetermined, (i.e. SMASH-U categories); hypertension, anticoagulation, antiplatelet, prior MI, DM, NIH Stroke Scale (NIHSS) at admission, age and AF.
We considered significant a P < 0.05.
Results
Between January 2009 and July 2017, we identified 1441 patients based on the 431 ICD-9 code, at either admission or discharge. During the retrieval of data, we excluded 715/1441: 546 for lack of information, 73 misdiagnosed with epi-subdural haemorrhages, 44 traumatic intracerebral haemorrhages, 19 ischemic strokes (IS), 14 IS with haemorrhagic infarction, 7 for bleedings in the pre-study period, 6 bleedings associated with neurosurgical interventions and 6 due to bleeding tumours (glioblastoma, metastasis, meningioma). We were not allowed to access to the data source of 546 on the total of patients (38%) as the clinical charts were no longer stored in the Hospital and due to the recent data regulation changes.
We included a total of 726 patients in the study. The mean age of our population was 72 ± 13.9 and 405 (55.7%) were males. Concerning the locations, 331 were recorded as lobar (46%), 296 deep (40%) and 99 cerebellar (14%) (Table 1).
Hypertension was present in 76.7% (n.557) of the patients, while previous cerebrovascular diseases were present as follows: 7.4% (n.54) history of IS, 7% (n.51) ICH and 8% (n.58) MI. Atrial fibrillation was present in 13.2% (n.96), whereas 15.1% (n.110) was diagnosed with type 2 DM.
Structural vascular lesions accounted for 9.6% (n.70) of patients with a mean age of 56.1 ± 17.5 years: 16 cavernomas, 10 aneurysms, 1 Sturge–Weber syndrome and 43 arteriovenous malformations (AVMs).
Medication represented 17.9% (n.130), with a mean age of 78.3 ± 8.8: 80 on VKAs, 15 on DOACs, 13 on heparins, 9 on double antiplatelet therapy, 3 on double antiplatelet therapy plus heparin and 10 on antiplatelet alone.
Probable amyloid angiopathy represented 4.3% (n.31) of patients with a mean age of 78.35 ± 6.8 years.
Systemic disease accounted for 9.9% (n.72) of patients with a mean age of 67.5 ± 14.9 years. The underlying diseases included 13 hepatopathy (7 HCV, 1 hepatocarcinoma, 4 alcohol-related disease and 1 HCV-HIV), 13 thrombocytopenia (2 myeloproliferative disease), 9 renal failure (8 end-stage kidney disease), 9 acute myeloid leukemia, 7 coagulopathy (3 VII-, 1 VIII- and 1 XII- factor deficiency), 4 chronic lymphoid leukemia, 2 multiple myeloma, 2 medullary aplasia, 3 neoplasms, 3 shocks, 1 systemic lupus erythematosus, 1 rheumatoid arthritis, 2 gestosis and 1 chronic myeloid leukemia, 1 reversible vasospasm syndrome and 1 mycotic aneurysm.
Hypertension accounted for 33.5% of cases (n. 243) with a mean age of 72.7 ± 12.4.
Undetermined included 24.8% (n.180) with a mean age of 73.6 ± 12.6.
The anatomical ICH sites, in relation to SMASH-U subgroups are listed in Table 1.
Intra-hospital mortality resulted 25.8% (n.187). Deceased patients were on average older (74.5 ± 12.7 vs 71.2 ± 14.3, P = 0.006).
The group of the deceased patients presented the following anatomical classification of the ICHs: 47.6% (n.89) lobar, 40.1% (n.75) deep and 12.3% (n.23) cerebellar. The deceased patients’ mean age was 74.5 ± 12.7, with a mean NIHSS at admission = 17 ± 8. Previous MI was reported for 12.3% (n.23) and 27.8% (n.52) had been previously prescribed antiplatelets (Table 2).
138/726 (19%) performed cerebral MRI.
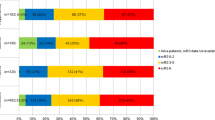
With SMASH-U classification, the inter-group mortality rate was for the structural vascular lesions 11.4% (8/70), medication 41/130 (31.5%), amyloid angiopathy 5/31 (16.1%), systemic disease group 26/72 (36.1%), hypertension 54/243 (22.2%) and undetermined 53/180 (29.4%) (Table 3).
On multivariable analysis, medication and systemic disease groups resulted significantly associated with intra-hospital mortality (odds ratio 3.47; 95% CI 1.15–10.46; P = 0.02 and 3.64; 95% CI 1.47–9.01; P = 0.005, respectively). Among the risk factors for ICH, age and high NIHSS at admission were also significantly associated with intra-hospital mortality (odds ratio 1.01; 95% CI 1–1.03; P = 0.04 and 1.12; 95% CI 1.03–1.22; P = 0.008, respectively) (Table 4).
Discussion
In our study, the highest mortality rates were detected for the systemic disease (36.1%), medication (31.5%), undetermined (29.4%), and hypertension (22.2%).
The high mortality rate observed in the systemic disease group is most likely a consequence of the poor outcome associated with the underlying pathology.
Regarding medication, the anticoagulant therapy increases the risk of in-hospital hematoma expansion (HE), and this latter factor could be responsible for the higher ICH mortality for patients in warfarin treatment [11,12,13,14,15]. The mortality in this group is lower than the rate registered in the original SMASH-U study population: one reason may be related to the most recent reversal therapies [16].
High blood pressure (BP) at the admission of ICH patients is associated with worse outcomes and higher mortality. Some studies found that hypertension is more likely to be related to large hematoma volume and HE [17,18,19], making hypertension a potential target for a better outcome, reducing the HE. However, current data does not support that intensive lowering BP improves mortality but it may better the functional outcome [20]. To date, the beneficial effect of early and intensive BP reduction for ICH outcome through HE prevention needs further clarification [21].
In our study, the undetermined group had a high mortality rate but in line with the original SMASH-U study, where it resulted in 30%, reinforcing the hypothesis that rapid aetiological diagnosis could improve the management and outcome of ICH patients [9].
As ICH prognosis remained stable over the last decades, despite an overall reduction in ICH incidence and an improvement of the prognosis in patients with ischemic stroke [22,23,24,25], we did not consider in the logistic model the year of admission. Additionally, we did not include in the logistic model the admission to the Stroke Unit as this may lead to bias, as the more severe patients were not routinely admitted to the Stroke Unit (for example patients who needed orotracheal intubation and intensive care were directly admitted to the Intensive Care Unit from the Emergency Department).
Since 2010, there has been a significant increase in the number of clinical studies in an attempt to better define the management of ICH. On this line, SMASH-U classification based on aetiology was developed in 2012 to enhance management [9]. Several studies found a significant reduction in the incidence of ICH over the past decade; however, mortality remains unchanged [22,23,24]. Management of acute ICH persists challenging: many promising interventions for acute ICH await further evidence from trials, while the prognosis of patients with ICH has not changed over recent times [25].
The relatively high number of structural vascular lesions, compared to the SMASH-U study (5%), could be due to the inclusion in our study of the Neurosurgery Department which is the referral centre of our region. Unexpectedly, 22.9% of these patients had deep hematomas and 8.6% were re-bleedings. The latter two findings suggest that there are limitations in the anatomical classification. In fact, without diagnostic work-ups, these cases might have been classified as typical ICHs due to hypertension (present in 50% of this group) (Table 1). In light of this, a complete aetiological work-up with CTA in Emergency Department, along with the clinical stratification of the severity of ICH could facilitate a more suitable diagnosis and faster addressing to the appropriate Department [26,27,28].
The medication group accounted for 17.9% (n.130), higher than what had been reported by the SMASH-U study. We could explain this higher percentage because we included all patients on anticoagulant treatment, regardless of INR values at admission, DOACs and antiplatelets, in the absence of alternative causes. The anticoagulant treatment with VKAs, regardless of INR levels at admission, could be regarded as a coagulopathy because it inhibits Vitamin K-dependent coagulation factors and INR levels may not be reliably predictive of any prior anticoagulation state [11]. The medication group is a target group for urgent treatment as the anticoagulant effects of VKAs and DOACs can be reversed [7, 11,12,13,14].
Amyloid angiopathy represented 4.3% (n.31) of our patients, which was significantly lower than the reported 20% of the original study [9]. On a total of 726 patients, only 138 (19%) performed cerebral MRI. Among this group, 20/31 (65%) had probable cerebral amyloid angiopathy based on MRI criteria, 11/20 (55%). Out of 27/31 (87%) also had a history of hypertension, representing a competing aetiology, highlighting how the amyloid angiopathy diagnosis could be challenging and sometimes overestimated.
Hypertension was significantly lower in our patients, 33.5% (n.253) vs 58% reported for the SMASH-U study. This difference might have been since, in our study, we classified hypertension as a risk factor and not, as in the SMASH-U study, a cause when no hypertensive disease was diagnosed and if a more probable aetiology was present (i.e. structural vascular lesions or coagulopathy).
Finally, the undetermined percentage was in line with that reported by the SMASH-U paper (24.8%). However, our percentage would have been higher if we had classified the patients with multiple risk factors in this category. Moreover, many of our patients could not be investigated for underlying causes due to early death. It is a quite high percentage and it could lead to the conclusion that it is a failure of the utility of the classification, and it highlights how difficult a rapid aetiological diagnosis is; nevertheless, the SMASH-U classification is the first to give input and promote an aetiological approach to acute ICH in clinicians. Therefore, it might be worth validating the scale in a prospective study.
There is more than one limitation within our study. First, we were not allowed, for the privacy policy, to access data from the outpatient setting and Emergency Department, so we did not record data about patients who died outside the hospital before admission or those who refused treatment. Second, this was a retrospective, single-centre study, so we only had access to medical records. As a consequence, we did not have access to follow-up; for this reason, we were limited to record intra-hospital mortality rates. For the same point, we were not able to record the data source of a quite high percentage (38%) of patients classified with the diagnostic code of 431 ICD-9-CM, as the clinical charts were no longer stored in our hospital. Third, the classification was applied on the most-likely-aetiology basis, deriving information from medical records: this approach could, with fair probability, have led to misclassification of some specific aetiologies.
Based on the results of our retrospective study, while considering all the previously mentioned limitations, in particular the potential aetiological misclassification, SMASH-U showed to be potentially predictive of intra-hospital mortality of ICH patients and it can be considered a useful tool, in clinical practice, to guide the management of acute haemorrhagic stroke patients.
A comparative study between the two classification systems (aetiology-based SMASH-U vs anatomically-based classification system) could help to clarify which system is the most suitable in terms of predictive value for the intra-hospital mortality of patients with ICH.
References
Katan M, Luft A (2018) Global burden of stroke. Semin Neurol 38(2):208–211 Epub 2018 May 23
Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V (2009 Apr) Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 8(4):355–369
Sacco S, Marini C, Toni DS, Olivieri L, Carolei A (2009) Incidence and 10-year survival of intracerebral hemorrhage in a population-based registry. Stroke 40(2):394–399
van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ (2010 Feb) Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol 9(2):167–176
Hemphill JC III, American Heart Association Stroke Council., Council on Cardiovascular, and Stroke Nursing., Council on Clinical Cardiology et al (2015) Guidelines for the management of spontaneous intracerebral hemorrhage: a Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 46(7):2032–2200
Flaherty ML, Woo D, Haverbusch M, Sekar P, Khoury J, Sauerbeck L et al (2005) Racial variations in location and risk of intracerebral hemorrhage. Stroke 36(5):934–937
Grysiewicz RA, Thomas K, Pandey DK (2008) Epidemiology of ischemic and hemorrhagic stroke: incidence, prevalence, mortality, and risk factors. Neurol Clin 26(4):871–895
Nag C, Das K, Ghosh M, Khandakar MR (2012) Prediction of clinical outcome in acute hemorrhagic stroke from a single CT scan on admission. N Am J Med Sci 4(10):463–467
Meretoja A, Strbian D, Putaala J, Curtze S, Haapaniemi E, Mustanoja S et al (2012) SMASH-U: a proposal for etiologic classification of intracerebral hemorrhage. Stroke 43(10):2592–2597
Knudsen KA, Rosand J, Karluk D, Greenberg SM (2001) Clinical diagnosis of cerebral amyloid angiopathy: validation of the Boston criteria. Neurology 56:537–539
James RF, Palys V, Lomboy JR, Lamm JR Jr, Simon SD (2013) The role of anticoagulants, antiplatelet agents, and their reversal strategies in the management of intracerebral hemorrhage. Neurosurg Focus 34(5):E6
Hemphill JC 3rd, Lam A (2017) Emergency neurological life support: intracerebral hemorrhage. Neurocrit Care 27(Suppl 1):89–101
Almegren M (2017) Reversal of direct oral anticoagulants. Vasc Health Risk Manag 13:287–292
Andresen K, Atar D, Gjertsen E, Ghanima W, Roseth S, Johansen OE (2018) Mechanisms of action and clinical use of specific reversal agents for non-vitamin K antagonist oral anticoagulants. Scand Cardiovasc J 52(3):156–162
Brouwers HB, Chang Y, Falcone GJ, Cai X, Ayres AM, Battey TW et al (2014) Predicting hematoma expansion after primary intracerebral hemorrhage. JAMA Neurol 71(2):158–164
Frontera JA, Lewin JJ 3rd, Rabinstein AA, Aisiku IP, Alexandrov AW, Cook AM et al (2016) Guideline for reversal of antithrombotics in intracranial hemorrhage: a statement for healthcare professionals from the neurocritical care society and society of critical care medicine. Neurocrit Care 24(1):6–46
Broderick JP, Diringer MN, Hill MD, Brun NC, Mayer SA, Steiner T, Skolnick BE, Davis SM (2007) Determinants of intracerebral hemorrhage growth: An exploratory analysis. Stroke 38:1072–1075
Wartenberg KE, Wang X, Muñoz-Venturelli P, Rabinstein AA, Lavados PM, Anderson CS et al (2017) Intensive care unit admission for patients in the INTERACT2 ICH blood pressure treatment trial: characteristics, predictors, and outcomes. Neurocrit Care 26(3):371–378
Sakamoto Y, Koga M, Yamagami H, Okuda S, Okada Y, Kimura K et al (2013) Systolic blood pressure after intravenous antihypertensive treatment and clinical outcomes in hyperacute intracerebral hemorrhage: The stroke acute management with urgent risk-factor assessment and improvement-intracerebral hemorrhage study. Stroke 44:1846–1851
Anderson CS, Heeley E, Huang Y, Wang J, Stapf C, Delcourt C et al (2013) Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med 368(25):2355–2365
Chen S, Zhao B, Wang W, Shi L, Reis C, Zhang J (2017) Predictors of hematoma expansion predictors after intracerebral hemorrhage. Oncotarget 8(51):89348–89363
Béjot Y, Grelat M, Delpont B, Durier J, Rouaud O, Osseby GV et al (2017) Temporal trends in early case-fatality rates in patients with intracerebral hemorrhage. Neurology 88(10):985–990
Zahuranec DB, Lisabeth LD, Sánchez BN, Smith MA, Brown DL, Garcia NM, Skolarus LE et al (2014) Intracerebral hemorrhage mortality is not changing despite declining incidence. Neurology 82(24):2180–2186
Béjot Y, Bailly H, Durier J, Giroud M (2016) Epidemiology of stroke in Europe and trends for the 21st century. Presse Med 45(12 Pt 2):e391–e398
Veltkamp R, Purrucker J (2017) Management of spontaneous intracerebral hemorrhage. Curr Neurol Neurosci Rep 17(10):80
Macellari F, Paciaroni M, Agnelli G, Caso V (2014) Neuroimaging in intracerebral hemorrhage. Stroke 45(3):903–908
Cheung CM, Tsoi TH, Hon SF, Au-Yeung M, Shiu KL, Lee CN, Huang CY (2008) Using the National Institutes of Health Stroke Scale (NIHSS) to predict the mortality and outcome of patients with intracerebral haemorrhage. Hong Kong Med J 14(5):367–370
D'Amore C, Paciaroni M, Silvestrelli G, Agnelli G, Santucci P, Lanari A et al (2013) Severity of acute intracerebral haemorrhage, elderly age and atrial fibrillation: independent predictors of poor outcome at three months. Eur J Intern Med 24(4):310–313
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest to disclose for the conduction of this study.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mosconi, M.G., Paciaroni, M., Agnelli, G. et al. SMASH-U classification: a tool for aetiology-oriented management of patients with acute haemorrhagic stroke. Intern Emerg Med 16, 109–114 (2021). https://doi.org/10.1007/s11739-020-02330-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-020-02330-2