Abstract
Background and objective
Intracerebral hemorrhage (ICH) is a serious medical condition with high mortality. However, factors leading to long-term mortality after ICH are largely unclear. The aim of this community-based study is to assess predictors of long-term mortality after spontaneous ICH.
Methods
We identified all patients admitted with spontaneous ICH to hospitals with a certified stroke unit in Brno, the second largest city in the Czech Republic (CR), in 2011, the year of the Czech Population and Housing Census. We reviewed their medical records for risk factors, radiographic parameters, and measures of post-stroke neurological deficit [National Institutes of Health Stroke Scale (NIHSS)]. Using the dates of death from the Czech National Mortality Register, we calculated mortality at 30 days, six months, one year, and three years after the ICH. Multivariate analysis with forward stepwise logistic regression was performed to determine independent predictors of mortality (p < 0.05).
Results
In 2011, 1086 patients with stroke were admitted to the four stroke-certified hospitals in Brno, CR. Of these, 134 had spontaneous ICH, with complete data available in 93 of them entering the final analysis. The mortality at 30 days, 6 months, 1 year, and 3 years post-ICH was 34%, 47%, 51%, and 63%, respectively. The mortality was highest in the first few days post-event, with 50% of patients dying in 255 days and average survival being 884 ± 90 days. Both NIHSS and modified ICH (MICH) score showed to be strong and reliable predictors of short- as well as long-term mortality; the risk of death post-ICH increased with older age and size of ICH. Other risk factors contributing to higher, primarily shorter-term mortality included history of cardiac failure, myocardial infarction, or atrial fibrillation.
Conclusions
In our community-based study, we found that severity of neurological deficit at admission (NIHSS), combined with age and size of ICH, well predicted short- as well as long-term mortality after spontaneous ICH. A history of cardiac failure, myocardial infarction, or atrial fibrillation at presentation were also predictors of mortality, underscoring the need for optimal cardiac management in patients with ICH.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite advances in treatment and diagnosis, intracerebral hemorrhage (ICH) remains a serious medical condition with one month case fatality rates as high as 40% [1], and survival rates at one year and five years of 46% and 21%, respectively [2]. Incidence of ICH has been reported to be 24.6 per 100,000, and to increase significantly with age, with patients 85 years and older having a nearly ten-fold higher annual risk of developing ICH than those 45–54 years old [1, 3]. Both the incidence and early case fatality have remained high and have not decreased significantly between 1980 and 2008 [1]. The morbidity of ICH is also high, with only 12–39% of patients achieving long-term functional independence [1]. ICH thus represents a growing public health challenge and financial burden, especially in countries with aging populations.
There is considerable variability in published data regarding the predictors of mortality following ICH. Moreover, data on long-term prognostic factors are limited. In this study, we explore short- and long-term predictors of mortality following ICH in patients hospitalized for ICH in Brno, Czech Republic (CR).
Methods
Study type and population
For this study, data from two Czech national administrative databases were used—the National Register of Hospitalized Patients (NRHOSP) and the Czech National Mortality Registry (CNMR). Both databases have been described previously [4, 5]. In short, in the NRHOSP data about all hospital admissions in the Czech Republic are being prospectively collected, the database has been previously validated the accuracy of the diagnostic codes for different stroke types. The CNMR collects information regarding all deaths in the Czech Republic [5].
For this community-based study, we searched the NRHOSP for all patients with discharge diagnosis of I61 [spontaneous (non-traumatic) ICH [International Classification of Diseases, Tenth Revision (ICD-10) code I61] admitted to any of the 4 hospitals with a certified stroke unit in Brno, Czech Republic (Hospital of the Merciful Brothers, Military Hospital Brno, St. Anne’s University Hospital, and the University Hospital Brno) between January 1, 2011, and December 31, 2011. All patients with a suspected stroke are required to be transported to a hospital with a certified stroke unit as per the guidelines applicable in the whole Czech Republic [6]. The year 2011 was selected due to the availability of accurate demographic data from the 2011 Czech Population and Housing Census; the population of the city of Brno, our catchment area, was 385,913 people that year. For each patient identified, we requested his or her complete discharge summary from the admitting hospital. The methodology of patient selection, case ascertainment, and clinical data collection in this study was described previously [7, 8]. In short, two neurologists independently reviewed the discharge summaries, and verified the discharge diagnosis of ICH using the standard WHO definition.
To identify the patients who died, regardless of cause, following a diagnosis of IS and to calculate all-cause mortality rates, we linked the data from the hospitalization registry (NRHOSP) with the data from the mortality registry (CNMR) and calculated 1-days, 6-months, 1-year, and 3-year all-cause mortality rates [5]. The exact cause of death was not accounted of in our analysis.
Clinical and radiological data collection
In summary, 16 clinical variables plus 15 radiological parameters were collected. Patients’ discharge summaries were reviewed, and risk factors and other relevant clinical variables were recorded. Functional outcome and severity of stroke were assessed by the National Institutes of Health Stroke Scale (NIHSS) and modified Rankin Scale (mRS) at both admission and discharge, as well as the pre-admission mRS to detect any baseline impairment.
Following radiologic parameters were obtained from the initial CT scans: volume of ICH and absolute/relative perihematomal edema volume (both measured by the ABC/2 method)[9,10,11], volume of intraventricular extension of ICH[11] and spontaneous intraventricular hemorrhage (IVH) volume[12], total volume of ICH (TV) [12], midline shift [11], hematoma location [11, 13], ventricular compression [11], presence of sulcal and basal cistern effacement [14], hydrocephalus score [14], and presence of foramen magnum herniation [15]. Finally, the modified ICH (MICH) score was calculated [16].
Statistics
Associations between mortality and patient parameters were calculated in the univariate analysis for the individual time points (30 days, six months, one and three years). Significant variables then entered the multivariate analysis in two models based on their mutual noncollinearity (Model A with NIHSS at admission and Model B with MICH score as leading factors) in which forward stepwise logistic regression was performed to determine independent predictors of mortality. Data are presented as mean values accompanied by standard deviation (SD) or as odds ratios (OR) with 95% confidence intervals (CI), assuming normal approximation of the binominal distribution. A p value ≤ 0.05 was considered statistically significant. Additionally, in the multivariate analysis, receiver operating characteristic (ROC) curves with area under curve (AUC) values are used to describe the data. The results then underwent a tenfold cross-validation to check for their accuracy and standardized accuracy (coefficient kappa).
Statement of ethics
This study was approved by the ethics committees of all participating hospitals (Hospital of the Merciful Brothers, Military Hospital Brno, St. Anne’s University Hospital, and the University Hospital Brno) and by the ethics committee of the Institute of Health Information and Statistics of the CR. Informed consent requirement has been waived by the above ethics committees, as this is a retrospective medical record review study. This study conforms with the guidelines outlined in the Declaration of Helsinki.
Results
In 2011, there were 1086 patients with stroke admitted to the four study hospitals in Brno, CR. Of these, 134 had spontaneous ICH, with available and complete data in 93 of them entering the final analysis (Table 1, Online Appendix). The mortality rate at 30 days, six months, one year, and three years post-ICH was 34%, 47%, 51%, and 63%, respectively. The mortality is highest in the first few days post-event, with 50% of patients dying in 255 days and average survival being 884 ± 90 days (Table 1).
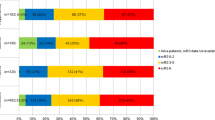
The associations between 16 clinical variables plus 15 radiological parameters and post-ICH mortality in the univariate analysis are summarized in Table 2. Results of the multivariate analysis are shown in Table 3 and Figs. 1, 2, 3.
Both NIHSS and MICH score showed to be strong and reliable predictors of short- as well as long-term mortality; the risk of death post-ICH increases with older age and size of ICH. Among the risk factors contributing to higher, primarily shorter-term mortality are also history of cardiac failure, myocardial infarction, or atrial fibrillation.
Discussion
In this community-based study, we assessed ICH mortality and its predictors in a geographically defined area of the city of Brno, CR. Our study has two major findings. Firstly, mortality at 30 days, six months, one year, and three years was 34%, 47%, 51%, and 63%, respectively. Such mortality rates are similar to those reported in several meta-analyses[1, 2] and our previous data on hemorrhagic stroke mortality in the CR [5]. The current data suggests that ICH mortality in the CR, three decades after the end of communism, was comparable or lower than that reported from other developed countries. Also, it suggests the high quality of care of stroke patients in the CR, a post-communist country in Central Europe with relatively scant data on stroke epidemiology.
Secondly, we identified predictors of both short- and long-term mortality after spontaneous ICH. We found that a patient’s functional neurological status, as assessed by the NIHSS at admission to hospital, was a consistent independent predictor of mortality at all time points. Our results are supported by numerous studies, in which the NIHSS proved to be a strong predictor of mortality during hospitalization [17], at 30 days [18, 19], three months [19], one year [20], and even at five years post event [18]. This finding points to the key role of neurological status immediately after stroke, well reflecting the underlying ICH severity, and its continuing impact on survival throughout the post-stroke period.
The MICH score (combining a subject´s functional performance assessed by NIHSS score, age, hematoma volume, infratentorial origin and intraventricular extension of bleed)[16] proved to be an equally potent predictor of both short- and long-term mortality. Our study thus contributes to the scant data on the predictive value of ICH score in the longer follow-up [21].
A history of cardiac failure, myocardial infarction, and atrial fibrillation independently predicted post-ICH survival at various time points. These results demonstrate the impact of concurrent heart disease on survival. A recent study noted that atrial fibrillation is present in 21.9% of spontaneous ICH cases.21 These patients, while receiving antithrombotic medication, had larger hematoma volume and higher three month mortality [22]. Others have noted that cardiac failure impacts post-ICH survival, increasing the risk of post-discharge mortality and hemorrhagic stroke recurrence within the first three years [23].
Consistent with previous studies, measuring largest diameter of ICH proved to add value to the prediction model; and given its simplicity and close relation to hematoma volume [9], this parameter may be particularly useful in an emergency setting [24]. Also, sulcal or cisternal effacement may indicate an increased intracranial pressure, and thus signal a developing hydrocephalus, which has previously been noted as an independent predictor of short-term mortality [14]. Further, hydrocephalus score serves as a good tool to assess and quantify hydrocephalus severity and thus better predict patient´s outcome [14].
Similar to other studies [9, 20, 25], age, too, independently predicted mortality. Combining the effect of age and NIHSS, the Essen ICH score showed a high prognostic accuracy for complete recuperation and death 100 days post stroke [26]. One study on ICH in the oldest-old patients (over 85 years), however, questioned the criterion of age as an independent predictor of mortality, stating that in the oldest of patients, a higher hematoma volume on admission leads to the graver outcome rather than age-related comorbidities [27]. Consequently, age might be a better predictor in comparatively younger patients, losing its forecasting utility in the eldermost.
The clinical relevance of our findings is accompanied by the quick and easy measurement of the aforementioned variables, which helps to streamline the process of assessing clinical severity and prognosis immediately after hemorrhagic stroke. Overall, our results indicate that both the NIHSS and MICH scores are excellent predictors of mortality and well describe the underlying ICH severity.
Our study has several limitations. First, it is a retrospective study with the spontaneous source of clinical/radiologic data being CT scans and admission or discharge reports of variable quality. However, the quality of the CT scans and discharge data was overall high, since all patients were treated in four large hospitals with stroke units (two of the four hospitals are university hospitals). Second, the cohort was relatively small and only patients with sufficiently detailed data were included [93 out of 134 patients (69%)], leading to a relatively lower power of our analysis due to reduced sample size and impacting on our ability to validly assess all potential predictors of mortality. However, there is generally a smaller sample size in ICH studies. Third, we could not include follow-up CT scans because these were missing for some patients, and therefore the effect of potential hematoma growth on outcome could not be explored [28]. Fourth, we did not collect data on eventual withdrawal or limitation of care; nonetheless, according to standard medical practice in the participating hospitals, the best possible intensive care is provided to patients with ICH.
Finally, in this study we analyzed only hospitalized cases of ICH. A previous study showed that over 7% of patients with ICH die prior to being admitted to hospital [29]. This most likely means that the mortality rates reported in this study are lower than the true rates. Also, the risk factor profile of patients surviving the hyperacute phase may be different from those who die before reaching hospital. Not including the latter in our analysis might have confounded the predictors of mortality identified in this study and likely limits the generalizability of our results to hospitalized ICH patients only. Inclusion of autopsy data would have mitigated this limitation, but these were not available to us. Nevertheless, we expect that all patients in the Brno area were presented to one of the cooperating hospitals, ie, no cases from the community were omitted other than due to ultra-early mortality, because all patients with a suspected stroke are required to be transported to a hospital with a certified stroke unit as per the guidelines applicable in the whole Czech Republic (and all 4 hospitals with certified stroke unit were included) [6].
The uniqueness of our study lies in its community-based character, in the assessment of broad range of clinical (16) and radiological (15) variables, and the reporting on three-year mortality after ICH and its predictors, thus becoming, to the best of our knowledge, the first study assessing long-term mortality after ICH in Central Europe. As mentioned above, due to the inclusive and community-based nature of our study, these mortality data should be representative of an urban and suburban population in a post-communist Central European city.
Conclusion
In this community-based study in Brno, CR, we found that severity of neurological deficit at admission, combined with age and size of ICH, well predicted short- and long-term mortality after spontaneous ICH. A history of cardiac failure, myocardial infarction, or atrial fibrillation at presentation were also predictors of mortality, underscoring the need for optimal cardiac management in patients with ICH.
References
van Asch CJ, Luitse MJ, Rinkel GJ et al (2010) Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. https://doi.org/10.1016/S1474-4422(09)70340-0
Poon MTC, Fonville AF, Salman RAS (2014) Long-term prognosis after intracerebral haemorrhage: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp-2013-306476
Sedova P, Brown RD, Zvolsky M et al (2017) Incidence of hospitalized stroke in the Czech Republic: the national registry of hospitalized patients. J Stroke Cerebrovasc Dis. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.11.006
Sedova P, Brown RD, Zvolsky M et al (2021) Incidence of stroke and ischemic stroke subtypes: a community-based study in Brno, Czech Republic. Cerebrovasc Dis. https://doi.org/10.1159/000512180
Bryndziar T, Sedova P, Brown RD et al (2020) Trends in one month and one year hemorrhagic stroke case fatality rates in the Czech Republic between 1998 and 2015. J Stroke Cerebrovasc Dis. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104762
Bryndová L, Bar M, Herzig R et al (2021) Concentrating stroke care provision in the Czech Republic: the establishment of Stroke Centres in 2011 has led to improved outcomes. Health Policy. https://doi.org/10.1016/j.healthpol.2021.01.011
Bryndziar T, Matyskova D, Sedova P et al (2022) Predictors of short- and long-term mortality in ischemic stroke: a community-based study in Brno, Czech Republic. Cerebrovasc Dis. https://doi.org/10.1159/000519937
Jackova J, Sedova P, Brown RD et al (2020) Risk factors in ischemic stroke subtypes: a community-based study in Brno, Czech Republic. J Stroke Cerebrovasc Dis. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104503
Broderick JP, Brott TG, Duldner JE et al (1993) Volume of intracerebral hemorrhage: A powerful and easy-to-use predictor of 30-day mortality. Stroke. https://doi.org/10.1161/01.STR.24.7.987
Gebel JM, Jauch EC, Brott TG et al (2002) Relative edema volume is a predictor of outcome in patients with hyperacute spontaneous intracerebral hemorrhage. Stroke. https://doi.org/10.1161/01.STR.0000035283.34109.EA
Nag C, Das K, Ghosh M, Khandakar MR (2012) Prediction of clinical outcome in acute hemorrhagic stroke from a single CT scan on admission. N Am J Med Sci. https://doi.org/10.4103/1947-2714.101986
Hallevi H, Dar NS, Barreto AD et al (2009) The IVH Score: a novel tool for estimating intraventricular hemorrhage volume: clinical and research implications. Crit Care Med. https://doi.org/10.1097/CCM.0b013e318198683a
Sreekrishnan A, Dearborn JL, Greer DM et al (2016) Intracerebral hemorrhage location and functional outcomes of patients: a systematic literature review and meta-analysis. Neurocrit Care. https://doi.org/10.1007/s12028-016-0276-4
Diringer MN, Edwards DF, Zazulia AR (1998) Hydrocephalus: a previously unrecognized predictor of poor outcome from supratentorial intracerebral hemorrhage. Stroke. https://doi.org/10.1161/01.STR.29.7.1352
Witsch J, Neugebauer H, Zweckberger K, Jüttler E (2013) Primary cerebellar haemorrhage: complications, treatment and outcome. Clin Neurol Neurosurg 115(7):863–869
Cheung RTF, Zou LY (2003) Use of the original, modified, or new intracerebral hemorrhage score to predict mortality and morbidity after intracerebral hemorrhage. Stroke. https://doi.org/10.1161/01.STR.0000078657.22835.B9
Satopää J, Mustanoja S, Meretoja A et al (2017) Comparison of all 19 published prognostic scores for intracerebral hemorrhage. J Neurol Sci. https://doi.org/10.1016/j.jns.2017.05.034
Cheung CM, Tsoi TH, Hon SFK et al (2008) Using the National Institutes of Health Stroke Scale (NIHSS) to predict the mortality and outcome of patients with intracerebral haemorrhage. Hong Kong Med J 14(5):367–370
Finocchi C, Balestrino M, Malfatto L et al (2018) National Institutes of Health Stroke Scale in patients with primary intracerebral hemorrhage. Neurol Sci. https://doi.org/10.1007/s10072-018-3495-y
Nilsson OG, Lindgren A, Brandt L, Säveland H (2002) Prediction of death in patients with primary intracerebral hemorrhage: a prospective study of a defined population. J Neurosurg. https://doi.org/10.3171/jns.2002.97.3.0531
Suo Y, Chen WQ, Pan YS et al (2018) The max-intracerebral hemorrhage score predicts long-term outcome of intracerebral hemorrhage. CNS Neurosci Ther 24:1149–1155. https://doi.org/10.1111/cns.12846
Roquer J, Vivanco-Hidalgo RM, Prats-Sánchez LL et al (2019) Interaction of atrial fibrillation and antithrombotics on outcome in intracerebral hemorrhage. Neurology. https://doi.org/10.1212/WNL.0000000000008462
Pana TA, Wood AD, Perdomo-Lampignano JA et al (2019) Impact of heart failure on stroke mortality and recurrence. Heart Asia. https://doi.org/10.1136/heartasia-2018-011139
Zis P, Leivadeas P, Michas D et al (2014) Predicting 30-day case fatality of primary inoperable intracerebral hemorrhage based on findings at the emergency department. J Stroke Cerebrovasc Dis. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.02.006
Jolink WMT, Klijn CJM, Brouwers PJAM et al (2015) Time trends in incidence, case fatality, and mortality of intracerebral hemorrhage. Neurology. https://doi.org/10.1212/WNL.0000000000002015
Weimar C, Benemann J, Diener HC (2006) Development and validation of the Essen intracerebral haemorrhage score. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp.2005.081117
Forti P, Maioli F, Domenico Spampinato M et al (2016) The effect of age on characteristics and mortality of intracerebral hemorrhage in the oldest-old. Cerebrovasc Dis. https://doi.org/10.1159/000448813
Delcourt C, Huang Y, Arima H et al (2012) Hematoma growth and outcomes in intracerebral hemorrhage: the INTERACT1 study. Neurology. https://doi.org/10.1212/WNL.0b013e318260cbba
Fogelholm R, Murros K, Rissanen A, Avikainen S (2005) Long term survival after primary intracerebral haemorrhage: a retrospective population based study. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp.2004.055145
Acknowledgements
We thank Michaela Volna and Jana Baluchova for their help with the data collection. We also express our gratitude toward Michaela Fricova who designed several graphs in our study.
Funding
PS and RM were supported by the Ministry of Health of the Czech Republic, grant nr. NW24-09–00215, by the IRENE COST Action (No. CA18118) funded by COST Association, by the IRIS-TEPUS Project (No. LTC20051) from the INTER-EXCELLENCE INTER-COST Program of the Ministry of Education, Youth and Sports of the Czech Republic, and by STROCZECH within CZECRIN Large Research Infrastructure (No. LM2018128) funded by the state budget of the Czech Republic. PS was supported by Ministry of Health, Czech Republic—conceptual development of research organization (FNBr, 65269705).
Author information
Authors and Affiliations
Contributions
Albert Sterba collected data, helped design and interpreted the statictical analysis, wrote the manuscript; Petra Sedova collected data, helped design and supervised the study, revised the manuscript; Robert D. Brown Jr. supervised the study, helped with the study design, revised the manuscript; Albert Stehlik collected data; Tomas Bryndziar took part in establishing the study methodology, revised the manuscript; Petra Cimflova assisted in correct assessment of radiological variables; Silvie Belaskova and Ingrid Kovacova performer statistical analysis; Josef Bednarik helped with the collection of data; Robert Mikulik helped design and supervised the study, revised the manuscript. All coauthors critically revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
The present study conforms to the guidelines issued in the Declaration of Helsinki. This study was approved by the Institutional Ethics Committees (Ethics Committees of St Anne’s University Hospital, University Hospital Brno, Hospital of Merciful Brothers, Military Hospital Brno, and Institute of Health Information and Statistics of the CR, RF. 36v/2014). Consent was waived by the IRB for this retrospective medical record review study, with no direct patient contact.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sterba, A., Sedova, P., Brown, R.D. et al. Predictors of spontaneous intracerebral hemorrhage mortality: a community-based study in Brno, Czech Republic. Acta Neurol Belg (2024). https://doi.org/10.1007/s13760-024-02612-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13760-024-02612-y