Abstract
Anemia is a risk factor related to morbidity and mortality in patients with chronic heart failure (HF). Less is known about its influence in patients in an early stage of HF. Our aim is to investigate the prognostic role of anemia in patients initially hospitalized for acute HF. We reviewed all consecutive patients admitted within a 18-month period with a main diagnosis of acute HF. We collected demographic, clinical and treatment data. Anemia is defined as Hemoglobin <12/13 g/dL upon admission in female/male patients, respectively. 719 patients were included (55.5% female), with a mean age of 78.7 ± 9 years. Anemia was present in 59.6% of patients upon admission, with a mean Hb of 10.4 ± 1.4 g/dL. Multivariate analysis confirms the relationship between the presence of anemia and older age, a previous diagnostic history of diabetes, and the presence of chronic kidney disease. In-hospital mortality is similar for anemic and non-anemic patients (6.8 vs 3.8%, p = n.s.) However, the difference is significant when one-year mortality is evaluated (31% in anemic patients vs 19% in non-anemic patients, p < 0.001). Cox regression analysis confirms the association between anemia and higher risk of one-year mortality, as well as with older age and a higher Charlson comorbidity index. Our study confirms that the presence of anemia is an independent factor for mid-term (1-year) mortality even in patients experiencing a first admission due to acute HF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anemia is a very frequent condition. Its prevalence among patients with heart failure (HF) has been found to range between 7 and 50%, depending on the cut-off value used to define its presence and on the HF population considered [1].The presence of anemia has been found to confer a significant impact on HF patient’s symptoms, quality of life and overall prognosis [2, 3].
The etiology of anemia in HF is usually multifactorial, and it is related to different mechanisms: iron deficiency due to reduced intestinal absorption or cytokine-related inflammatory changes, reduced erythropoietin production, concomitant chronic diseases such as kidney failure, or even hemodilution [4–6]. The prevalence of anemia and its effect on prognosis appear to be similar in HF associated with a reduced (HFrEF) and HF with a preserved (HFpEF) ejection fraction, with comparable risks of mortality, readmission, hospitalization rates and loss of functional capacity [7, 8]. Less is known, however, regarding the prognostic impact of anemia inpatients in the early stages of HF, namely those who have just experienced the first episode of acute decompensated HF leading to a first HF-related hospital admission [9, 10]. Our study aims at further investigating the putative role of anemia in the prognosis of these patients, focusing on its influence on 1-year mortality after this index admission as the main outcome.
Materials and methods
This retrospective study was performed at Bellvitge University Hospital, a 750-bed tertiary-care public hospital from Barcelona (Spain). We retrieved administrative data regarding all admissions to our hospital within a 18 month-period (July 2013–Dec 2014) with HF as primary discharge diagnosis, as identified by the ICD 9-CM codes 398.91, 402.91, 404.01, 404.03, 404.91, 404.93, 428.0, 428.1, 428.20, 428.21, 428.22, 428.23, 428.30, 428.31, 428.32, 428.33, 428.40, 428.41, 428.42, 428.43 and 428.9. Following this first selection, we reviewed all medical records of these patients to select only those who: (a) truly fulfilled clinical criteria for acute HF and (b) were experiencing the first ever admission due to a first episode of acute HF, excluding all those who had been discharged with a primary or secondary diagnosis of HF prior to the index admission. We also excluded from the analysis those patients younger than 50 years of age, patients in stage V chronic kidney disease (CKD) undergoing kidney replacement therapies, patients who had received a kidney or heart transplant, and patients who had been subject to prior blood transfusions with palliative intention. We also excluded those patients whose acute HF was secondary to an acute coronary syndrome, and those who had been discharged directly home within 24 h or transferred to other acute care hospitals from the Emergency Department (Fig. 1). All doubts regarding inclusion in the study were discussed within an investigators’ revision panel. The ethics committee of the Bellvitge University Hospital approved the overall protocol [PR2016/16].
HF presence was clinically ascertained according to the fulfilling of the Framingham criteria [11]. When echocardiographic data were available, we recorded EF values and coded HF as HFpEF type when the EF value was ≥50%. Collected data included demographic data (age, gender and place of residence), past medical history, and all clinical data related to HF signs and symptoms recorded at the time of admission. A basic blood chemistry panel was obtained, including kidney function (plasma creatinine values plus the estimated glomerular filtration rate calculated according to the abbreviated Modification of Diet in Renal Disease (MDRD) equation [12]), ionic, lipid and glycemic profiles were performed. The admission plasma concentration of NT-proBNP was not available in most patients, and for this reason, was excluded from the data collection procedures; that was also the case for iron metabolism markers, cobalamin and folate. A complete blood cell count was also obtained in all patients. Anemia was defined according to the World Health Organization (WHO) criteria (hemoglobin (Hb) <13 g/dL for males; Hb <12 g/dL for females); we categorized it as mild (Hb > 10 g/L), moderate (Hb 8–10 g/L) or severe (Hb <8 g/L) [13]. The Charlson Index (ChI) score was used to measure comorbidity [14]; this score ranges from 0 (no comorbidities) to a theoretical maximum of 33, depending on the presence of certain diseases with assigned values—HF is one of the components of the ChI, and since it was the main diagnosis for all patients, its assigned value was not incorporated in the calculation. Finally, we recorded the patients’ length of stay, their destinations at discharge and the HF-related medications prescribed upon discharge.
Follow-up
One-year mortality, measured as time-to-event data after the index admission discharge, is the main outcome of this study; 30-day mortality is a secondary outcome. Subjects were categorized as alive after 30 days and 12 months of follow-up, or censored when they died, whichever occurred first. Mortality status was determined by trained physician adjudicators on the basis of medical records from hospitalizations, emergency department visits, death certificates, and autopsy and coroner’s reports, when available. No patients were lost to follow-up.
Statistical analysis
Normally distributed continuous variables are reported as mean ± standard deviation (SD) and categorical variables are reported as proportions. The Student’s t test was used to compare continuous variables, with a previous Levene test for equality of variances, while either the Chi square statistic or Fisher’s exact test was used to compare categorical or dichotomous variables.
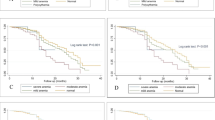
We performed logistic regression analysis to determine, at the multivariate level, the baseline factors associated with the presence of anemia at the time of admission. This procedure was used to estimate the unadjusted and adjusted odds ratio (OR) with 95% confidence intervals (CI 95%). Variables used in this logistic regression were those associated in the bivariate analysis. The final adjusted model was obtained using the backward stepwise method. We used the Cox regression model to evaluate the relationship (estimated as hazard ratios, HR) between the presence of anemia and all-cause mortality over time. Covariates used for adjustment of baseline variables were also evaluated in a stepwise Cox multivariable regression analysis, incorporating all of them with p < 0.05 in the univariate analysis. Finally, Kaplan–Meier survival curves and the log-rank test as a function of patients’ anemia category were calculated from baseline to time of censoring.
These analyses were completed with the Statistical Package for Social Sciences (SPSS) program (version 21.0, SPSS Inc., Chicago, IL, USA). Tests were 2-sided and p values <0.05 were considered statistically significant.
Results
A total of 719 patients were included in the study: mean age was 78.7 ± 9 years and 399 (55.5%) of them were female. Their mean ChI value (HF excluded) was 2.3 ± 1. Echocardiography was available during the index admission roughly in 50% of our patients (350); 210 of them (60%) were of the HFpEF type.
Anemia was present in 429 (59.6%) patients, 196 male (45.7%) and 233 female (54.3%). 133 anemic HF patients (31%) were already diagnosed with anemia before the index admission. Anemia was mostly normocytic (mean MCV 89. 9 ± 8.4 fL) and normochromic (mean MCH 29.1 ± 3.3 pg/mL). The mean Hb value of the anemic patients was 10.4 ± 1.4 g/dL; of them, 493 (68.5%) presented with mild anemia, whereas 111 (25.9%) had moderate and 24 (5.6%) severe anemia.
Baseline differences between anemic and non anemic patients are reported in Table 1: anemic patients are older, with a higher prevalence of diabetes, CKD, aortic stenosis and a prior diagnosis of anemia; the mean ChI score is also higher in this group. For those with echo data available, a significant relationship is found between anemia and the presence of HFpEF. The multivariate analysis confirms a significant and independent relationship between the presence of anemia and older age (OR 1.018 CI 95% 1.001–1.035) plus a prior diagnosis of diabetes (OR 1.556 CI 95% 1.110–2.181), and CKD (OR 2.364 CI 95% 1.587–3.521), with HFpEF losing the association at this level of the analysis.
Length of stay Hospital admission is longer for anemic patients (8.3 vs 7.5 days, Table 1), but compared to non-anemic patients the difference in length of stay does not reach statistical significance.
Mortality During the index admission, mortality is similar among anemic and non-anemic patients (6.8 vs 3.8%, p = 0.089) (Table 2). However, 30-day mortality is significantly higher in the group of anemic patients (11.9 vs 5.5%, p = 0.004). Regarding our main outcome data, mortality is also higher among anemic patients at one year of follow-up (31 vs 19%, p < 0.001). Figure 2 shows the cumulative risk of mortality during the year of follow-up for both categories of patients.
Table 3 shows the baseline and discharge data related to the patients’ vital status one year after discharge. Multivariate analysis confirms that the presence of anemia at the time of index admission is actually associated with a higher risk of one-year mortality (HR 1.778 CI 95% 1.178–2.685). Other factors independently associated with this risk are older age (HR 1063 CI 95% 1040–1086), a higher comorbidity measured by the ChI (HR 1110 CI 95% 1014–1216), and a previous diagnosis of dementia (HR 1970 CI 95% 1178–3087). Interestingly, the diagnosis of aortic stenosis is a protective factor for mortality, conferring a significant reduced risk of death when present (HR 0.365 CI 95% 0.160–0.830).
Discussion
Our study shows that anemia is not only a common finding among patients experiencing a first admission for acute HF, but also that its presence is an independent marker of mortality risk in this group of patients. The prevalence of anemia in similar HF populations reaches similar figures: a previous study of our group, based on a smaller number of patients but also selected when experiencing their first hospitalization for acute HF, shows a prevalence of anemia of 43% [10]. A recent Spanish study on a population of stable chronic HF patients (referred to an outpatient HF unit) reports a prevalence of “any kind of anemia” of 59.4% [15]. These prevalences are, however, lower than those found in other studies on patients with acute HF, ranging between 50% in OPTIMIZE-HF and ADHERE registry [16, 17] and 70% [18]; however, these studies include not only first admissions, but also patients with chronic HF and a history of repeated episodes of decompensation, for whom this higher prevalence of anemia is probably a marker of more advanced disease.
Anemia is easy to diagnose, and in some cases amenable to some kind of therapy: data from recent trials (FAIR-HF and CONFIRM-HF) [19, 20] prove the benefits of treating not only iron-deficiency anemia, but also iron deficiency alone in patients with chronic systolic HF. Furthermore, the new European Society of Cardiology guidelines stress the need to screen and treat for those conditions in such patients [21, 22]. Less is known regarding beneficial therapies for chronic disease-related anemia. Some trials have shown a lack of benefit in patients with HF and CKD-related anemia treated with erythropoietin, patients with HFpEF or patients with acute HF [23–25].
Our anemic HF patients are older and with more comorbid conditions; similar characteristics have been described in a recent metaanalysis [26]. A remarkable finding is that only one-third of our patients presenting with anemia upon admission have a mention of that diagnosis in their medical history. Although this might be related in some cases to a component of hemodilution, it also likely reflects the fact that mild anemia (Hb between 11 and 13 g/dL) is not always identified as such in medical records.
Regarding EF status, we find that HFpEF (and also higher EF values, when EF is analysed as a continuous variable) is more common in the presence of anemia, but this relationship loses statistical significance in the multivariable analysis. This lack of EF-specific association with a higher prevalence of anemia is also present in recent studies [18, 26].
The significant relationship between coexisting anemia and diabetes found in our study has also been described previously [27]. Most likely the coexistence of anemia and diabetes reflects the fact that the later plays the role of “chronic disease” leading to anemia. A previous study that categorizes the types of anemia in HF patients actually confirms that this association is significant only in patients whose anemia is classified as “chronic disease-related” [28].
Length of stay (LOS) in our study is longer for anemic patients, but does not reach a significant difference. In this line, the study by Caughey [18] describes a comparable LOS, with even longer stays in anemic patients with systolic heart failure (8.9 vs 7.5 days, p < 0.0001).
In-hospital mortality is higher for anemic patients, but the difference is not significantly different to that experienced by non-anemic patients. The overall in-hospital mortality of our cohort is 5.6%, which is between the 4.3% described among Medicare-patients [29] and the 6.4% of the population admitted for HF for the first time analysed by Tuppin et al. [30]. One-year mortality in our acute HF patients overall is 26.1%, with a significantly higher mortality rate in anemic patients (31%). The study by Tuppin et al. [30], also restricted to patients with HF experiencing a first hospitalization, reports a similar one-year mortality rate (29%), even though their study includes patients aged <50 years. The one-year mortality rate in anemic patients is higher than ours in the Caughey’s study (36% in HFpEF and 43% in HFrEF), but as already mentioned, this study includes all patients with acute HF, not restricted to those experiencing a first admission, and, therefore, likely to be in more advanced stages of the disease. From our data an association between the presence of anemia and a higher risk of one-year mortality in this group of patients with acute HF can be identified; this was neither the case in our previous study involving a smaller sample of acute HF patients admitted to the same hospital [10], nor in the other study focusing on new onset HF cases [9]. In patients with acute decompensated HF, this association has been suggested by Caughey et al., and also in Berry’s meta-analysis, both for HFpEF and HFrEF patients.
We also find that older age, comorbidity (measured by the ChI and history of dementia) are related to higher mortality. However, CKD, a well-known predictor of mortality, loses significance after the multivariate analysis. The protective role of aortic stenosis might seem counterintuitive, but further evaluation of our patients shows that about 50% of these patients underwent early valve repair surgery after diagnosis, thus eliminating the cause for their HF.
Our study has some limitations that have to be mentioned. It is a retrospective analysis and the information were taken from electronic medical records; full data about anemia evaluation and treatment (before or after the index hospitalization) was not completely available; data on NT-proBNP or anemia-related blood chemistry values was also scarce and echo data was restricted to half of the overall patients. On the other hand, this study is based on a sizeable number of comparable patients, carefully selected as presenting with their first-time ever clinical episode of acute HF (confirmed by a thorough medical record review), without missing cases in the year of follow-up.
Conclusions
Anemia is detected in more than half of patients hospitalized for the first time with acute HF. Furthermore, our study seems to confirm that the presence of anemia is a prognostic factor for 30-day and one-year mortality after discharge in such patients experiencing a first admission due to acute HF. The etiology of anemia in HF is usually multifactorial and related to different mechanisms; therefore, we suggest that anemia should be identified, correctly diagnosed and considered when possible a therapeutic target in all patients with acute HF.
References
Stamos TD, Silver MA (2010) Management of anemia in heart failure. Curr Opin Cardiol 25:148–154. doi:10.1097/HCO.0b013e3283357fe0
Cattadori G, Agostoni P, Corrà U, Sinagra G, Veglia F, Salvioni E, Bonomi A, La Gioia R, Scardovi AB, Ferraironi A, Emdin M, Metra M, Di Lenarda A, Limongelli G, Raimondo R, Re F, Guazzi M, Belardinelli R, Parati G, Caravita S, Magrì D, Lombardi C, Frigerio M, Oliva F, Girola D, Mezzani A, Farina S, Mapelli M, Scrutinio D, Pacileo G, Apostolo A, Iorio A, Paolillo S, Filardi PP, Gargiulo P, Bussotti M, Marchese G, Correale M, Badagliacca R, Sciomer S, Palermo P, Contini M, Giannuzzi P, Battaia E, Cicoira M, Clemenza F, Minà C, Binno S, Passino C, Piepoli MF (2016) Heart failure and anemia: effects on prognostic variables. Eur J Intern Med 37:56–63. doi:10.1016/j.ejim.2016.09.011
Triposkiadis F, Giamouzis G, Parissis J, Starling RC, Boudoulas H, Skoularigis J, Butler J, Filippatos G (2016) Reframing the association and signi fi cance of co-morbidities in heart failure. Eur J Heart Fail 30:744–758
Nanas JN, Matsouka C, Karageorgopoulos D, Leonti A, Tsolakis E, Drakos SG, Tsagalou EP, Maroulidis GD, Alexopoulos GP, Kanakakis JE, Anastasiou-Nana MI (2006) Etiology of anemia in patients with advanced heart failure. J Am Coll Cardiol 48:2485–2489. doi:10.1016/j.jacc.2006.08.034
Meara EO, Rouleau JL, White M, Roy K, Blondeau L, Ducharme A, Neagoe PE, Sirois MG, Lavoie J, Racine N, Liszkowski M, Madore F, Tardif JC, De Denus S (2014) Heart failure with anemia novel findings on the roles of renal disease, interleukins, and specific left ventricular remodeling processes. Circ Hear Fail 7:773–781. doi:10.1161/CIRCHEARTFAILURE.114.001100
Opasich C, Cazzola M, Scelsi L, De Feo S, Bosimini E, Lagioia R, Febo O, Ferrari R, Fucili A, Moratti R, Tramarin R, Tavazzi L (2005) Blunted erythropoietin production and defective iron supply for erythropoiesis as major causes of anaemia in patients with chronic heart failure. Eur Heart J 26:2232–2237. doi:10.1093/eurheartj/ehi388
Ather S, Chan W, Bozkurt B, Aguilar D, Ramasubbu K, Zachariah AA, Wehrens XHT, Deswal A (2012) Impact of noncardiac comorbidities on morbidity and mortality in a predominantly male population with heart failure and preserved versus reduced ejection fraction. J Am Coll Cardiol 59:998–1005. doi:10.1016/j.jacc.2011.11.040
Moe GW, Ezekowitz JA, O’Meara E, Lepage S, Howlett JG, Fremes S, Al-Hesayen A, Heckman GA, Abrams H, Ducharme A, Estrella-Holder E, Grzeslo A, Harkness K, Koshman SL, McDonald M, McKelvie R, Rajda M, Rao V, Swiggum E, Virani S, Zieroth S, Arnold JMO, Ashton T, D’Astous M, Chan M, De S, Dorian P, Giannetti N, Haddad H, Isaac DL, Kouz S, Leblanc MH, Liu P, Ross HJ, Sussex B, White M (2015) The 2014 Canadian cardiovascular society heart failure management guidelines focus update: anemia, biomarkers, and recent therapeutic trial implications. Can J Cardiol 31:3–16. doi:10.1016/j.cjca.2014.10.022
Kalra PR, Collier T, Cowie MR, Fox KF, Wood DA, Poole-Wilson PA, Coats AJS, Sutton GC (2003) Haemoglobin concentration and prognosis in new cases of heart failure. Lancet. doi:10.1016/S0140-6736(03)13912-8
Formiga F, Chivite D, Castañer O, Manito N, Ramón JM, Pujol R (2006) Anemia in new-onset congestive heart failure inpatients admitted for acute decompensation. Eur. J. Intern. Med. doi:10.1016/j.ejim.2005.11.015
McKee PA, Castelli WP, McNamara PM, Kannel WB (1971) The natural history of congestive heart failure: the Framingham study. N Engl J Med 285:1441–1446. doi:10.1056/NEJM197112232852601
Levey AS, Coresh J, Greene T, Marsh J, Stevens LA, Kusek JW, Van Lente F, Disease K (2007) Expressing the modification of diet in renal disease study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem 772:766–772. doi:10.1373/clinchem.2006.077180
WHO Scientific Group on Nutritional Anaemias (1968) World Health Organization., Nutritional anaemias: report of a WHO scientific group (meeting held in Geneva from 13 to 17 March 1967). http://whqlibdoc.who.int/trs/WHO_TRS_405_rus.pdf
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 40:373–383. doi:10.1016/0021-9681(87)90171-8
Díez-Ló Pez C, Lupó J, De Antonio M, Zamora E, Domingo M, Santesmases J, Troya M-I, Boldó M, Bayes-Genis A (2016) Hemoglobin Kinetics and Long-term Prognosis in Heart Failure Ciné tica de la hemoglobina y pronó stico a largo plazo en insuficiencia cardiaca. Rev Esp Cardiol. doi:10.1016/j.rec.2016.02.028
Young JB, Abraham WT, Albert NM, Gattis Stough W, Gheorghiade M, Greenberg BH, O’Connor CM, She L, Sun JL, Yancy CW, Fonarow GC (2008) Relation of low hemoglobin and anemia to morbidity and mortality in patients hospitalized with heart failure (Insight from the OPTIMIZE-HF Registry). Am J Cardiol. doi:10.1016/j.amjcard.2007.07.067
Galvao M, Kalman J, Demarco T, Fonarow GC, Galvin C, Ghali JK, Moskowitz RM (2006) Gender differences in in-hospital management and outcomes in patients with decompensated heart failure: analysis from the acute decompensated heart failure national registry (ADHERE). J Card Fail. doi:10.1016/j.cardfail.2005.09.005
Caughey MC, Avery CL, Ni H, Solomon SD, Matsushita K, Wruck LM, Rosamond WD, Loehr LR (2014) Outcomes of patients with anemia and acute decompensated heart failure with preserved versus reduced ejection fraction (from the ARIC Study Community Surveillance) HHS Public Access. Am J Cardiol 114:1850–1854. doi:10.1016/j.amjcard.2014.09.024
Anker SD, Colet JC, Filippatos G, Willenheimer R, Dickstein K, Drexler H, Luscher TF, Bart B, Banasiak W, Niegowska J, Kirwan BA, Mori C, von Eisenhart Rothe B, Pocock SJ, Poole-Wilson PA, Ponikowski P (2009) Ferric carboxymaltose in patients with heart failure and iron deficiency. N Engl J Med 361:2436–2448. doi:10.1056/NEJMoa0908355
Ponikowski P, Van Veldhuisen DJ, Comin-Colet J, Ertl G, Komajda M, Mareev V, McDonagh T, Parkhomenko A, Tavazzi L, Levesque V, Mori C, Roubert B, Filippatos G, Ruschitzka F, Anker SD (2015) Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symptomatic heart failure and iron deficiency. Eur Heart J 36:657–668. doi:10.1093/eurheartj/ehu385
Jankowska EA, Tkaczyszyn M, Suchocki T, Drozd M, von Haehling S, Doehner W, Banasiak W, Filippatos G, Anker SD, Ponikowski P (2016) Effects of intravenous iron therapy in iron-deficient patients with systolic heart failure: a meta-analysis of randomized controlled trials. Eur J Heart Fail. doi:10.1002/ejhf.473
Hfa A, Voors AA, Germany SDA, Uk JGFC, Uk AJSC, Harjola V, Germany VF, Poland EAJ, Uk PN, Germany BP, Uk JPR, Rosano GMC, Rutten FH (2016) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution:2129–2200. doi:10.1093/eurheartj/ehw128
Swedberg K, Young JB, Anand IS, Cheng S, Desai AS, Diaz R, Maggioni AP, McMurray JJV, O’Connor C, Pfeffer MA, Solomon SD, Sun Y, Tendera M, van Veldhuisen DJ (2013) RED-HF Committees, RED-HF Investigators, Treatment of anemia with darbepoetin alfa in systolic heart failure. N Engl J Med 368:1210–1219. doi:10.1056/NEJMoa1214865
Silverberg DS, Wexler D, Blum M, Tchebiner JZ, Sheps D, Keren G, Schwartz D, Baruch R, Yachnin T, Shaked M, Schwartz I, Steinbruch S, Iaina A (2003) The effect of correction of anaemia in diabetics and non-diabetics with severe resistant congestive heart failure and chronic renal failure by subcutaneous erythropoietin and intravenous iron. Nephrol Dial Transplant 18:141–146. doi:10.1093/ndt/18.1.141
Vullaganti S, Goldsmith J, Teruya S, Alvarez J, Helmke S, Maurer MS (2014) Cardiovascular effects of hemoglobin response in patients receiving epoetin alfa and oral iron in heart failure with a preserved ejection fraction. J Geriatr Cardiol 11:100–105. doi:10.3969/j.issn.1671-5411.2014.02.002
Berry C, Poppe KK, Gamble GD, Earle NJ, Ezekowitz JA, Squire IB, Mcmurray JJV, Mcalister FA, Komajda M, Swedberg K, Maggioni AP, Ahmed A, Whalley GA, Doughty RN, Tarantini L (2016) Prognostic significance of anaemia in patients with heart failure with preserved and reduced ejection fraction: results from the MAGGIC individual patient data meta-analysis. QJM 109:377–382. doi:10.1093/qjmed/hcv087
Lupón J, Urrutia A, González B, Herreros J, Altimir S, Coll R, Prats M, Rey-Joly C, Valle V (2005) Prognostic significance of hemoglobin levels in patients with heart failure. Rev. Española Cardiol. 58:48–53. http://www.ncbi.nlm.nih.gov/pubmed/15680131
Ezekowitz JA, McAlister FA, Armstrong PW (2003) Anemia is common in heart failure and is associated with poor outcomes: insights from a cohort of 12065 patients with new-onset heart failure. Circulation. doi:10.1161/01.CIR.0000052622.51963.FC
Bueno H, Ross JS, Wang Y, Chen J, Vidán MT, Normand S-LT, Curtis JP, Drye EE, Lichtman JH, Keenan PS, Kosiborod M, Krumholz HM, Krumholz Y (2010) Trends in length of stay and short-term outcomes among medicare patients hospitalized for heart failure: 1993–2008. JAMA 303:2141–2147. doi:10.1001/jama.2010.748
Tuppin P, Cuerq A, De Peretti C, Fagot-Campagna A, Danchin N, Juillière Y, Alla F, Allemand H, Bauters C, Drici MD, Hagège A, Jondeau G, Jourdain P, Leizorovicz A, Paccaud F (2014) Two-year outcome of patients after a first hospitalization for heart failure: a national observational study. Arch Cardiovasc Dis. doi:10.1016/j.acvd.2014.01.012
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This article does not contain any studies with animals performed by any of the authors. The ethics committee of the Bellvitge University Hospital approved the overall protocol.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Migone de Amicis, M., Chivite, D., Corbella, X. et al. Anemia is a mortality prognostic factor in patients initially hospitalized for acute heart failure. Intern Emerg Med 12, 749–756 (2017). https://doi.org/10.1007/s11739-017-1637-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-017-1637-5