Abstract
To establish whether C-reactive protein (CRP) is an independent predictor of all-cause mortality and hospitalization in chronic obstructive pulmonary disease (COPD), we followed 200 patients with COPD and 201 age- and gender -matched controls for a median time of 4.2 years (range, 0.2–5.1 years). Airflow obstruction was rated moderate if forced expiratory volume in one second (FEV1) was 50–69% of the predicted value, or severe if FEV1 was <50%. The CRP level was categorized as low (≤3 mg/L) or high (>3 mg/L). The hazard of death was estimated by a proportional hazard regression model, using controls with low CRP as the reference category. Fifty subjects died: 41 (21%) among the COPD and 9 (4%) among the controls (p < 0.0001). The hazard of death in moderate COPD was not significantly higher than in the reference category, independently of the CRP level. In severe COPD with a low CRP, the hazard of death is 3.4 times higher than in the reference category (p = 0.008); in severe COPD and a high CRP it is 9.6 times higher (p < 0.0001). The rate of hospitalization in COPD patients with a high CRP is 1.9 times higher than in those with a low CRP [95% confidence interval (CI), 1.2–3.2]. In severe COPD, it is 6.9 times higher than in moderate COPD (95% CI, 3.8–12.7). A high CRP level is a significant amplifier of the risk of death only in severe COPD. The degree of airflow obstruction is a strong independent predictor of COPD-related outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity, mortality, and disability in industrialized countries [1]. Chronic airflow obstruction, the functional hallmark of COPD, is associated with an inflammatory response of the lung to inhaled noxious particles and gases. COPD also features a systemic inflammatory component characterized by muscle wasting and weight loss [2, 3].
C-reactive protein (CRP) is a marker of systemic inflammation that can be measured in the plasma inexpensively. The CRP level is increased in stable COPD patients with respect to control smokers and non-smokers [4]. In advanced COPD, elevated CRP levels are associated with impaired energy metabolism and reduced exercise capacity [5]. Also, an increased CRP level may be predictive of adverse cardiac events [6] and of all-cause mortality in patients with mild to moderate COPD [7]. In a population-based survey, the CRP level was found to be an independent predictor of future adverse outcomes in subjects with airway obstruction [8].
The present study was undertaken to reappraise CRP as an independent predictor of all-cause mortality and hospitalization for COPD exacerbation. We followed over time a sample of patients with moderate to severe COPD, and an equal size sample of age- and gender -matched controls who took part in a multicenter cohort study on genetic susceptibility to the development of COPD.
Methods
Sample
The study sample included 200 patients with COPD and 201 controls that were part of a larger cohort enrolled in a case–control study aimed at assessing genetic susceptibility to the development of COPD [9–11].
The subjects, all Caucasian, were evaluated at the outpatient clinic of the CNR Institute of Clinical Physiology, Pisa, Italy, between November 1, 2001 and September 30, 2003. Potential candidates were enrolled through the help of family physicians in the city of Pisa and surroundings.
Criteria for case recruitment were (a) the firm clinical diagnosis of stable COPD, (b) airflow limitation as indicated by a post-bronchodilator ratio of forced expiratory volume in one second over forced vital capacity (FEV1/FVC) < 0.7 and FEV1 ≤70% of the predicted value [12], and (c) a smoking history ≥20 pack-years.
Patients were excluded from the study if they had an established diagnosis of asthma, established obstructive syndromes other than COPD or lung cancer, history of atopy, known alpha-1-antitrypsin deficiency, or a serum alpha-1-antitrypsin concentration <1.0 g/dL. Patients were also excluded if they had had a clinically confirmed acute exacerbation in the 4 weeks preceding the study entry.
By study design, controls were recruited to match COPD patients on age and gender. All the controls were current or former smokers with a smoking history ≥20 pack-years. Only individuals with no airflow obstruction were included in the control group (FEV1/FVC > 0.7; FVC and FEV1 > 80% of the predicted value). Individuals were excluded from the control group if they had a history of chronic lung disease or atopy, a family history of COPD, or had had an acute respiratory infection in the 4 weeks preceding the study entry.
Study protocol
The protocol was approved by the local ethics committee. Before entering the study, an informed written consent was obtained from all the subjects.
Detailed clinical history and physical examination were obtained in each participant. Comorbid conditions were defined as follows:
Systemic arterial hypertension was considered to be present if there was documented persistent elevation of arterial pressure (systolic >150 mmHg or diastolic >90 mmHg), or if the patient was receiving anti-hypertensive medication. Ischemic heart disease was considered to be present if one of the following criteria were met: (a) typical angina on exertion, (b) use of anti-anginal medication, and (c) any prior myocardial infarction documented by electrocardiogram and cardiac enzyme elevation. Left heart valvular disease was recorded if there was hemodynamic or echocardiographic evidence of mitral or aortic stenosis or incompetence. Heart failure was recorded if there was echocardiographic evidence of a left ventricular ejection fraction ≤40%. Chronic cor pulmonale was recorded if there was radiologic or echocardiographic evidence of dilatation of the right heart cavities. Right ventricle hypertrophy was considered to be present if the thickness of the right ventricle free wall exceeded 7 mm on 2-D echocardiography.
Cerebrovascular disorders included transitory ischemic attacks (TIA) and stroke and were recorded if documented any time prior to the enrollment in the study. Pulmonary embolism was recorded if there had been episodes of embolism, diagnosed by lung scintigraphy or computed tomographic angiography, that required anticoagulant therapy. Similarly, deep vein thrombosis was recorded if there had been episodes of venous thrombosis, documented by compression ultrasonography of the lower or upper extremities, requiring anticoagulant therapy.
Diabetes mellitus was considered to be present if the patient was on long-term therapy with insulin or oral hypoglycemic drugs. Hypercholesterolemia was recorded if the blood cholesterol was higher than 200 mg/dL and the HDL cholesterol lower than 40 mg/dL, or if the patient was on long-term statin therapy. Hypertriglyceridemia was recorded if triglyceride levels were higher than 150 mg/dL. Hypercholesterolemia and hypertriglyceridemia were grouped under the term dyslipidemia. Documented hyper- or hypothyroidism of any cause requiring appropriate medical treatment was recorded as thyroid dysfunction. Chronic hepatitis C was recorded if there were elevated serum aminotransferases for longer than 6 months, anti-HCV antibodies present in serum, and positive testing for HCV RNA by polymerase chain reaction.
Lung function studies included the measurement of FVC and FEV1 (before and after bronchodilator), and of single breath carbon monoxide lung diffusing capacity (DLCO). Spirometry, and DLCO measurements were performed according to ATS/ERS standards [13, 14].
Postero-anterior and lateral digital chest radiographs were obtained in all the subjects at the time of recruitment into the study and were examined by two pulmonologists for the presence of emphysema [15]. The diagnosis of emphysema on chest radiography was based on the identification of at least two of four explicit criteria that had been originally validated against lung pathology [16]. The COPD patients were also invited to complete a self-administered quality-of-life questionnaire [17].
Upon inclusion, a blood sample (stored in lithium heparin) was obtained from all the subjects for genomic studies. Plasma aliquots were stored at −80°C until further processing. The CRP level was measured with the high-sensitivity assay (Immulite, Diagnostic Products Corporation, Los Angeles, CA, USA).
Follow-up
The 401 sampled subjects were followed up until death or December 31, 2006, whichever occurred first. All the subjects were interviewed by phone at 6-month intervals. Whenever required, their family physicians were also called. Patients with COPD were evaluated clinically once a year at the outpatient clinic of our Institution. Critical events recorded by the physicians in charge of follow-up included hospital admissions for exacerbation of COPD, and death. The cause of death was established by reviewing clinical files, autopsy findings, or death certificates.
Statistical analysis
Continuous variables in the text and in the tables are reported as median with interquartile range (IQR). Differences between and within groups were tested for by Mood’s median test or Fisher exact test.
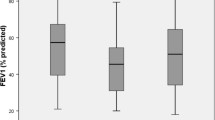
To model the hazard of death from any cause, we estimated a semi-parametric proportional hazard regression model. We considered time from study entry to death or censoring. The continuous variables CRP and FEV1 (as % predicted) were grouped into classes as follows: (a) CRP ≤ 3 mg/L (low CRP; N = 222), (b) CRP > 3 mg/L (high CRP; N = 179), (c) FEV1 < 50% (severe airflow obstruction; N = 78), (d) FEV1 between 50 and 69% (moderate obstruction; N = 122), and (e) FEV1 above 80% with FEV1/FVC > 0.7 (no obstruction; N = 201). They were introduced in the model along with their interaction by means of indicator variables.
Since cases and controls were matched on age and gender, we included a shared frailty term to account for the potential dependency within each matched pair. The frailty term, a multiplicative random effect for the baseline hazard associated with each matched pair, was assumed to follow a Gamma distribution with the mean equal to one and unknown variance [18].
The regression coefficients associated with the covariates were tested by likelihood ratio tests. Testing for homogeneity across matched pairs was performed by testing that the variance of the frailty term was equal to zero. To adjust for the boundary constraint, the variance being non-negative, we compared the likelihood ratio test statistic with the 50:50 mixture distribution of the Chi-square with one degree of freedom and the constant zero [19]. Though this procedure has been shown to be conservative [20], with our data it rejected the null hypothesis of homogeneity across matched pairs.
Among the 200 cases with moderate or severe COPD no matching was present. The incidence rate of hospitalization among the cases was modeled by Poisson regression. The estimates were adjusted for the different length of time of follow-up (exposure time) across the patients by introducing the logarithm of the exposure time as an offset variable in the model.
The dichotomous variable CRP was kept in both the proportional hazard and the Poisson regression model. All the remaining variables were included one at a time to check whether they might be confounders (change in the regression coefficient after inclusion greater than 10%), or effect modifiers (statistically significant interaction of the effect of CRP on the dependent variables). No confounders were found. The interaction between CRP and the severity of airflow obstruction was found to be significant in the proportional hazard regression. p values of less than 0.05 were considered statistically significant throughout. The statistical analysis was performed with Stata version 10 (StataCorp, College Station, TX).
Results
The baseline characteristics of the study sample are reported in Table 1.
The CRP concentration in the plasma was significantly higher in COPD patients than in age- and gender -matched controls (Table 1). Among the patients with COPD, there was no significant difference in CRP levels between those who were on inhaled corticosteroid therapy (median 3.0 mg/L, IQR 1.4–7.4), and those who were not (median 2.8 mg/L, IQR 1.2–6.5) (p = 0.883). Similarly, there was no significant difference in CRP levels between COPD patients who were on statin therapy (median 4.5 mg/L, IQR 1.8–9.2), and those who were not (median 2.8 mg/L, IQR 1.3–6.6) (p = 0.366).
The sample median follow-up time was 4.22 years (range, 0.18–5.13 years). During follow-up, 50 subjects died: 41 (21%) among the 200 patients with COPD and 9 (4%) among the 201 controls. Overall, the 401 subjects provided 1,626.7 person-years of follow-up.
The causes of death in the study sample are given in Table 2. Thirty-eight (76%) of 50 deaths were in-hospital deaths. COPD was considered the primary cause of death in 13 (32%) of 41 fatal events in the COPD group.
In univariate analysis, the COPD patients who died were significantly older and had more severe airflow obstruction than those who survived (Table 3). The COPD patients who died also had a significantly lower body mass index, a higher prevalence of emphysema and of chronic cor pulmonale, and a worse quality of life than those who survived (Table 3). There was no difference across the two groups as regards the baseline plasma concentration of CRP level (Table 3).
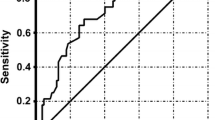
The results of the proportional hazard regression model are given in Table 4. In this analysis, the control subjects with low CRP levels are the reference category.
For the patients with moderate COPD, the hazard of death from any cause was not significantly higher with respect to the reference category, independently of the CRP concentration. In the patients with severe COPD and a low CRP level, the hazard of death was 3.4 times higher than in the reference category. High CRP level was an effect amplifier in the patients with severe COPD such that the hazard of death in this category was nearly tenfold higher than in the reference category.
Kaplan–Meier survivor curves in the patients with COPD are displayed in Fig. 1.
The cumulative rate of death from any cause as a function of CRP level and degree of airflow obstruction in 200 COPD patients. Red line high CRP level (>3 mg/L). Blue line low CRP level (≤3 mg/L). Severe COPD, high versus low CRP levels: log rank test, p value 0.0228. Moderate COPD, high versus low CRP levels: log rank test, p value 0.1190
In severe COPD and a high CRP level, the cumulative rate of death from any cause was significantly higher than in those with severe obstruction and a low CRP level. In moderate COPD, there was no significant difference in the mortality rate between the patients with high and those with low CRP levels.
The incidence rate of hospitalization for COPD exacerbation was 1.9-fold higher in the patients with a high CRP level than in those with a low CRP level (95% CI, 1.2–3.2, p = 0.012). In the patients with severe COPD, the incidence rate of hospitalization was 6.9-fold higher than in those with moderate COPD (95% CI, 3.8–12.7, p < 0.0001). The interaction between the covariates (CRP and FEV1) was not statistically significant.
Discussion
The primary objective of the present study was to establish whether an elevated CRP level is an independent predictor of all-cause mortality in established COPD. Differently from other investigations [6–8], we evaluated a sample of patients with moderate to severe COPD, and an equal-size sample of controls that were matched to COPD patients on age and gender. Cases and controls also featured very similar prevalence of comorbid conditions.
Our results can be summarized as follows: (a) the crude mortality rate in patients with moderate to severe COPD is remarkably higher than that of controls sharing similar comorbidities, (b) a high CRP level is a significant amplifier of the risk of death only in patients with severe COPD so that the hazard in this category is nearly tenfold that of controls with a low CRP level, (c) the severity of airflow obstruction, as reflected by FEV1, is a strong independent predictor of reduced survival in COPD, (d) among the cases, the rate of hospitalization for COPD exacerbation seems more dependent on the severity of airway obstruction than on the actual level of CRP.
With regard to the causes of death in our COPD sample, 13 (32%) of 41 were due to respiratory failure and 34% to cardiovascular events, assuming that “sudden death” is related to a major acute cardiovascular event. Cancer was the cause of death in 17% of all deaths in COPD patients. These figures are similar to those reported in the TORCH study [25], where 27% of the deaths were deemed to be due to cardiovascular causes, 35% to pulmonary causes, and 21% to cancer.
In the paper by Celli et al. [22], as many as 61% of the deaths are attributed to respiratory failure. That study comprised 635 patients with COPD from three different countries (Spain, Venezuela, and the United States), most of whom (71%) featured severe airflow obstruction [22].
In the study by Man et al. [7], the overall mortality rate among the COPD patients is of only 6.8% during a median period of 7.5 years of follow-up. The causes of death were lung cancer (31%), cardiovascular diseases (26%), and respiratory failure (8%). In the remaining 35%, the cause of death was due to other illnesses. In that study, the mean FEV1 was 78% of the predicted value [7]. Therefore, it is quite reasonable that respiratory failure was the cause of death in only a minority of the COPD patients.
In our sample, the COPD patients who died had more severe airflow obstruction than those who survived (FEV1 44 vs. 57% of the predicted value), so it not surprising that a substantial proportion of them died as a consequence of respiratory failure.
Our study has some limitations. First, our sample was smaller than that of other reports [6–8]. This precluded the possibility of investigating CRP levels as a predictor of cause-specific mortality in COPD. Second, our follow-up was shorter than that obtained by others [6–8]. Third, our analysis was based on a single determination of CRP level made at baseline. The latter limitation is shared by other broad outcome studies [6–8].
Dahl et al. [8] report that a CRP level above 3 mg/L is an independent predictor of future COPD-related hospitalization and death in a sample of 1,302 subjects with airway obstruction selected from the Copenhagen City Heart Study. The authors used a FEV1/FVC ratio of less than 0.7 as the single criterion to select subjects for the analysis, so it is unclear whether obstructive lung disorders other than COPD were included in the sample.
Also, the 6% mortality rate reported by Dahl, during a median duration of 8 years of follow-up, is far smaller than that observed in our COPD sample (21%) over a shorter period of follow-up.
In all likelihood, the subjects with airflow obstruction recruited into population-based studies differ from the COPD patients seen in the clinic. Therefore, the prognostic value of an elevated CRP level, as assessed in epidemiological surveys, may lose its strength when applied in clinical practice.
Our findings are in agreement with those reported by de Torres et al. [21] in 218 patients with moderate to very severe COPD who were followed up for a median time of 3 years. In that study, the all-cause mortality rate is 25%, which is very similar to that of our sample. The authors find that CRP levels are not associated with survival and that CRP does not add significant information to the risk assessment provided by other tools such as the multidimensional BODE index [22].
The interaction we observed between a high CRP level and severe airflow obstruction may suggest that systemic inflammation contributes to the determination of an adverse outcome in patients with advanced COPD. Such an interaction should be confirmed prospectively using serial measurements of the CRP levels.
Elevated values of CRP are not specific to COPD inas much as CRP increases in a variety of other inflammatory disorders. So, CRP may be an inadequate marker to assess the effect of any given therapeutic regimen on COPD-related outcomes.
For example, some investigators report that inhaled corticosteroids decrease CRP levels in patients with COPD [4, 23]. We were unable to confirm this finding, and so do others recently [24]. Anyway, there is no convincing evidence, at present, that inhaled corticosteroids are effective in reducing the all-cause mortality rate in COPD [25].
This should not be surprising, for COPD rarely occurs as a single clinical entity. As many as 81% of the COPD patients in our sample had at least one of cardiovascular, metabolic or endocrine comorbidity.
It is quite clear, therefore, that COPD patients may eventually die from conditions other than COPD. So, we believe that the issue of comorbidity must be taken into account while searching for new prognostic markers of COPD.
In summary, our data indicate that a high CRP level is a significant amplifier of the risk of death only in COPD patients with severe airflow obstruction. Carefully designed studies are, therefore, needed before endorsing CRP level as an outcome predictor in patients with established COPD.
References
Mannino DM, Homa DM, Akinbami LJ, Moorman JE, Gwynn C, Redd SC (2002) Chronic obstructive pulmonary disease surveillance—United States, 1971–2000. MMWR CDC Surveill Summ 51:1–16
Agusti AG, Sauleda J, Miralles C, Gomez C, Togores B, Sala E, Batle S, Busquets X (2002) Skeletal muscle apopotosis and wight loss in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 166:485–489
Vestbo J, Prescott E, Almdal T, Dahl M, Nordestgaard BG, Andersen T, Sørensen TIA, Lange P (2006) Body mass, fat-free mass, and prognosis in patients with COPD from a random population sample. Am J Respir Crit Care Med 173:79–83
Pinto-Plata VM, Mullerova H, Toso JF, Feudjo-Tepie M, Soriano JB, Vessey RS, Celli BR (2006) C-reactive protein in patients with COPD, control smokers and non-smokers. Thorax 61:23–28
Broekhuizen R, Wouters EF, Creutzberg EC, Schols AM (2006) Elevated CRP mark metabolic and functional impairment in advanced COPD. Thorax 61:17–22
Sin DD, Man SFP (2003) Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular diseases? Circulation 107:1514–1519
Man SFP, Connett JE, Anthonisen NR, Wise RA, Tashkin DP, Sin DD (2006) C-reactive protein and mortality in mild to moderate chronic obstructive pulmonary disease. Thorax 61:849–853
Dahl M, Vestbo J, Lange P, Bojesen SE, Tybjærg-Hansen A, Nordestgaard BG (2007) C-reactive protein as a predictor of prognosis in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 175:250–255
Chappell S, Daly L, Morgan K, Baranes TG, Roca J, Rabinovich R, Millar A, Donnelly SC, Keatings V, McNee W, Stolk J, Hiemstra PS, Miniati M, Monti S, O’Connor C, Kalsheker N (2006) Cryptic haplotypes of SERPIN A1 confer susceptibility to chronic obstructive pulmonary disease. Hum Mutat 27:103–109
Chappell S, Daly L, Morgan K, Guetta-Baranes T, Roca J, Rabinovich R, Millar A, Donnelly SC, Keatings V, McNee W, Stolk J, Hiemstra P, Miniati M, Monti S, O’Connor CM, Kalsheker N (2008) Genetic variants of microsomal epoxide hydrolase and glutamate-cysteine ligase in COPD. Eur Respir J 32:931–937
Haq I, Chappell S, Johnson SR, Lotya J, Daly L, Morgan K, Guetta-Baranes T, Roca J, Rabinovich R, Millar A, Donnelly SC, Keatings V, McNee W, Stolk J, Hiemstra P, Miniati M, Monti S, O’Connor CM, Kalsheker N (2010) Association of MMP-12 polymorphisms with severe and very severe COPD: a case control study of MMPs 1, 9 and 12 in a European population. BMC Med Genet 15:11–17
Crapo RO, Morris AH, Gardner RM (1981) Reference spirometric values using equipment and technique that meet ATS recommendations. Am Rev Respir Dis 123:659–664
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, Macintyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J (2005) ATS/ERS task force standardisation of spirometry. Eur Respir J 26:319–338
Macintyre N, Crapo RO, Viegi G, Johnson DC, van der Grinten CP, Brusasco V, Burgos F, Casaburi R, Coates A, Enright P, Gustafsson P, Hankinson J, Jensen R, McKay R, Miller MR, Navajas D, Pedersen OF, Pellegrino R, Wanger JI (2005) Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J 26:720–735
Miniati M, Monti S, Stolk J, Mirarchi G, Falaschi F, Rabinovich R, Canapini C, Roca J, Rabe KL (2008) Value of chest radiography in phenotyping chronic obstructive pulmonary disease. Eur Respir J 31:509–515
Sutinen S, Christoforidis AJ, Klugh GA, Pratt PC (1965) Roentgenologic criteria for the recognition of nonsymptomatic pulmonary emphysema. Correlation between roentgenologic findings, pulmonary pathology. Am Rev Respir Dis 91:69–76
Jones PW, Quirk FH, Baveystock CM, Littlejohn P (1992) A self-complete measure of heath status for chronic airflow limitation. The St. George’s respiratory questionnaire. Am Rev Respir Dis 145:1321–1327
Kalbfleisch JD, Prentice RL (2002) The statistical analysis of failure time data. Wiley, New York
Self SG, Liang KY (1987) Asymptotic properties of maximum likelihood estimators and likelihood ratio tests under nonstandard conditions. J Am Stat Assoc 82:605–610
Crainiceanu CM, Ruppert D (2004) Likelihood ratio tests in linear mixed models with one variance component. J R Stat Soc Ser B Stat Soc 66:165–185
de Torres JP, Pinto-Plata V, Casanova C, Mullerova H, Cordoba-Lanús E, Muros de Fuentes M, Aguirre-Jaime A, Celli BR (2008) C-reactive protein levels and survival in patients with moderate to very severe COPD. Chest 133:1336–1343
Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, Pinto-Plata V, Cabral HJ (2004) The body mass index, airflow obstruction, dyspnea and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 350:1005–1012
Sin DD, Lacy P, York E, Man SFP (2004) Effects of fluticasone on systemic markers of inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 170:760–765
Sin DD, Man SFP, Marciniuk DD, Ford G, FitzGerald M, Wong E et al (2008) Effects of fluticasone with or without salmeterol on systemic biomarkers of inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 177:1207–1214
Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, Yates JC, Vestbo J (2007) for the TORCH investigators Salmeterol and fluticasone propionate and survival in chronic obstructive poulmonary disease. N Engl J Med 356:775–789
Acknowledgments
The authors wish to thank Giosuè Catapano, Gianfranco Mirarchi, and Cristina Carli for excellent clinical and technical assistance. Permission was obtained from those who are acknowledged. This work was supported by the European Union fifth Framework Programme under the contract number QLG1-CT-2001-01012 (COPD GENE SCAN Project). The funding source had no role in the study design, the collection, analysis, or interpretation of data, the writing of the report, or the decision to submit the paper for publication.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miniati, M., Monti, S., Bottai, M. et al. Prognostic value of C-reactive protein in chronic obstructive pulmonary disease. Intern Emerg Med 6, 423–430 (2011). https://doi.org/10.1007/s11739-011-0520-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-011-0520-z