Abstract
The objectives of the study were to describe robotic-assisted surgery training programs currently being used by ACGME-accredited obstetrics and gynecology (OB/Gyn) residency programs and to explore residents’ attitudes towards their robotic surgery training curricula to evaluate resident desire for robotics training. We conducted a cross-sectional study of OB/Gyn residents for the 2015–2016 academic year. Participants completed a 31-item online questionnaire regarding their robotic-assisted surgical training and associated perspectives. Analyses of these data were primarily descriptive. In total, 98.9% of included respondents (N = 177) reported availability of a surgical robot at their training institution, and 35.0% of participants reported not having any structured robotics training program at their institution. The most commonly used training modalities included online modules (62.2%), dual-assist console (55.1%) and virtual reality simulation (50.3%). The most commonly reported barriers to completing a robots training were a lack of personal time (56.2%) and availability of the virtual reality simulator or access to the robotic equipment (29.2%). OB/Gyn residents desire robotics training and are exposed to a wide variety of training modalities. The ACGME should consider recommending the incorporation of a standardized formal robotics training program as part of the OB/Gyn residency curriculum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over 570,000 robotic-assisted procedures were performed in the United States in 2014 resulting in an increased interest in developing structured robotic training programs [1]. Modalities used in robotic surgery training curricula vary widely and include didactic sessions, skills labs, virtual reality simulation, cadaver training, case observation, and proctoring [2]. The American College of Obstetricians and Gynecologists (ACOG) recently released a statement in conjunction with the Society of Gynecologic Surgeons (SGS) addressing the growth of robotic surgery [3]. Within the statement, ACOG and SGS recommended that surgeons complete a didactic education program and hands-on training. However, there were no plans for formal training programs recommended, and the development of training programs was deferred to individual institutions. ACOG and SGS did note that surgeons must complete a didactic educational program offered by an accredited program, and practitioners must have hands-on training.
To date, there have been very few studies about formal robotic training programs incorporated into OB/Gyn residencies. In 2011, a cross-sectional survey of OB/Gyn residency directors revealed that although robotic surgical systems were available at 78% of the institutions, only 58% of programs had incorporated robotic surgical training as part of residency program [4]. Another study evaluating resident access to robotics training demonstrated that only 38% of residents had access to formal training despite 79% of respondents believing that their institution should provide such training [5]. The robotic training modalities reported in this study were limited to lectures, online modules, pelvic trainers, and animal laboratories; however, the time necessary to complete training was not stated. Furthermore, there has been little research about incorporation of more recent training technologies such as virtual reality simulation which has been shown to be an efficient way to acquire robotic skills or dual-assist console [6].
The objectives of this cross-sectional study were the following: (1) to describe the training programs currently being used by ACGME-accredited OB/Gyn residency programs for robotic-assisted surgery training including types of training modalities and resident exposure to robotics; (2) to explore residents’ attitudes towards their robotic surgery training curricula to evaluate resident desire for robotics training; and (3) to identify possible barriers to implantation of a robotics training program.
Methods
This was an IRB-exempt multi-institutional survey of postgraduate years (PGY) 1–4 residents in all ACGME-accredited OB/Gyn residency programs enrolled for the 2015–2016 academic year. An online survey tool was used to create a 31-question questionnaire, to assess resident exposure to robotic-assisted surgical training programs, types of training modalities being utilized, and resident attitudes towards their training experience. The survey was distributed to all program coordinators of accredited OB/Gyn residency programs for the 2015–2016 academic year via email. Program coordinators could then forward the survey to their enrolled residents. Periodic email reminders containing the link to the survey were sent to the residency program coordinator. Exclusion criteria included prior training in a surgical resident program outside of OB/Gyn such as urology, general surgery, neurosurgery or plastic surgery.
The data collected included demographic information, quantification of robotic surgical exposure, role as primary surgeon (as defined as completing 50% of the case) and comfort level with different robotics tasks. Exposure to the following training modalities was also recorded: formal didactics, online modules, dry laboratory, laparoscopic training, virtual reality simulator, cadaver/animal labs, live case observation, and dual-assist console usage. Additional data were collected to explore residents’ perceptions and attitudes towards their robotics training experience using Likert scale questions.
Analyses of these data were primarily descriptive. Demographic characteristics of respondents were compared using Chi square. Response rates were presented descriptively as percentages. A number of training modalities were reported as both the mean and range. All data manipulation and analyses were conducted in SAS software, Version 9.4 (SAS Institute Inc, Cary, NC).
Results
Demographics
There were 186 surveys completed. This represents approximately 3.8% of the population of OB/Gyn residents in the United States during the 2015–2016 academic year; however, given the distribution method of the survey the true sample size is unknown. Nine surveys were excluded from the analysis due to missing demographic data, PGY > 4, or prior residency experience. A majority of respondents were females (82.6%) in either their PGY-2 (27.5%) or PGY-3 (32.0%) (Table 1). The most commonly reported residency type was university programs (57.3%) located in the Northeast (38.8%) or Midwest (33.1%). Over 98% of respondents reported that there was a surgical robot available at their institution.
Structured robotics training program
Approximately, 65% of respondents were required to complete a structured robotics training program prior to sitting at the surgical console. The mean number of training modalities being utilized in formal training programs was 1.6 (range 1–8). Online modules (79.7%) were the most commonly utilized training modalities in formal training programs followed closely by dual-assist console (72.1%) and virtual reality simulation (65.0%). Additionally, 72.1% of participants reported receiving hands-on training on set-up, docking and troubleshooting the robot. Animal/cadaver labs were the least commonly utilized modalities (11.2%).
Of the respondents required to complete formal didactics as part of their robotic-assisted surgical training, 46.3% of respondents reported they had 2–5 h of didactics while 13.0% of respondents had at least 10 h of formal didactics. Virtual reality simulators were used by 65% of the respondents, the most common of which is the da Vinci® Skill Simulator (59.9%). Approximately, 67% of participants reported requiring at least 6 h to complete their mandatory virtual reality simulation modules. Despite a majority of respondents participating in a structured robotics training program, 50.3% of respondents reported that they did not have formal evaluations as a component of their training program. The most commonly utilized evaluation method was scoring of virtual reality modules (17.3%) followed by written evaluation of observed surgical techniques completed by attendings (12.1%).
Robotics-assisted surgical exposure
Of the 177 respondents with complete data 172 (97.2%) reported observing at least one robotic surgery at this point of their residency training while 65% of participants observed at least ten robotic procedures. Twenty-one (11.7%) respondents had never assisted during a robotic surgery while 85 (47.8%) reported assisting for at least ten robotic surgical procedures to date. To this point in training, a majority of residents (60.1%) reported that they had never been the primary surgeon for a robotic case. Approximately, 21% of respondents had completed five or fewer cases as primary surgeon. Residents reported exposure to robotic-assisted surgery in a wide range of clinical rotations with the most common rotations being gynecologic oncology (92.2%), benign gynecology (83.8%) and urogyneocology/pelvic floor reconstruction (45.3%).
Resident perceptions of their robotics training
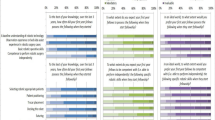
Respondents with an available formal robotics surgical training procedure were asked to identify the most useful and least useful training modalities (Fig. 1). Approximately, 50% of respondents identified dual-assist console as the most useful training modality, while 50.9% of participants selected online modules as the least useful training modalities. Over 74% of respondents identified a barrier to completion of a robotics training program. Of participants who identified a barrier, 71 respondents (55.9%) reported only one barrier to their training, while 11 respondents (8.6%) selected three or more barriers to training. The most commonly identified barrier was personal time available to complete training components followed by availability of the simulator/robot (Fig. 2).
Most respondents (68.2%) felt that robotics training is at least “probably important” as part of residency training, and 77.5% either agreed or strongly agreed that they would like to receive formal training in robotics surgery. Approximately, 26% of respondents felt that robotic-assisted surgical cases decreased resident participation in learning surgical procedures. With regard to the use of robotics in clinical practice following residency training, 25.4% of respondents either strongly disagreed or disagreed with the statement “I plan to use surgical robotics in my future practice” while 42.2% agreed or strongly agreed with this statement.
Discussion
The purpose of this study was to describe both the current training programs being utilized in OB/Gyn residents and to assess resident attitudes towards this training. This study found that 98.9% of respondents had access to a robot console at their training institution which is greatly improved from a prior survey in 2011 in which access to robotic surgical systems in OB/Gyn residencies was reported at 58% [4]. Furthermore, 65.0% of respondents were required to complete a structured robotics training program prior to being allowed activity at the surgical console compared to 16% in a 2010 study [5]. Importantly, in the current study, 68% of participants agreed that robotics training is a critical part of residency training, and 78% desired structured robotics training. These results are consistent with prior studies with reported ranges of 57–79% in residents from both OB/Gyn and general surgery programs [5, 7].
This study illustrated the wide variety of robotic-assisted surgical training modalities currently being utilized in OB/Gyn residency training programs. Dual-assist console and virtual reality simulation were noted by the respondents to be the most useful training modalities and these responses are congruent with the data evaluating the subjective utility of these training modalities [3, 8]. Several prospective studies have shown the effect of virtual reality robotic surgical simulation in improving trainees’ abilities in the operating room [9, 10]. There are less data regarding the objective utility of the dual-assist console and expert-guided mentorship in a dry laboratory setting as several recent studies did not show any significant difference in performance time during the teaching of training drills to medical students [11, 12]. However, benefits of the use of the dual console may allow for more rapid involvement of the residents in surgical cases and may be more time efficient [13].
Though the current study addresses a topic with limited data, there are several weaknesses that should be recognized. First, while we likely have a low response rate, we are unable to confirm how many participants ultimately received the survey due to the two-step distribution made necessary due to the lack of accessible, centralized resident contact information. Additionally, it is possible that our results were affected by respondent bias, in which residents with an interest in robotics or a formal robotics training program may have been more motivated to complete the survey. However, the demographic data illustrate the variety of respondents in terms of program type, gender, geographic location, and postgraduate year reflective of the overall OB/Gyn resident population. It is important to note that despite this study excluding residents receiving training in other surgical subspecialties, our results are similar to prior studies regarding formal robotics training in different surgical specialties [4, 5, 14]. Future efforts to improve response rates could include partnering with the Council on Resident Education in Obstetrics and Gynecology of ACOG for survey administration and providing incentives for responses.
Given that a majority of residents report access to a surgical robot, it is essential to implement a standardize robotics training for all OB/Gyn residency programs. Previous research has shown that a comprehensive training for robotic surgery was associated with high reliability and significant educational benefit [6, 15]. In one such study, 55 participants from general surgery, urology and gynecology were enrolled in a 2-month curriculum that included the following: online didactics, hands-on tutorials, and nine inanimate tasks modified from the Fundamentals of Laparoscopic Surgery program [15]. Approximately, 96% of participants enrolled in the curriculum successfully completed all components in 9–17 h and reached proficiency after a mean of 72 repetitions. A more recent study of implementation of a standard robotics curriculum in general surgery combined trainee-directed and expert-directed learning utilizing a wide variety of training modalities [16]. Ultimately, all participants (N = 20) completed the curriculum and 65% of participants reported sitting at the surgeon console. Similar to our study, these authors found that the major barrier to completion of the robotics curriculum was resident time availability.
While more research is needed in evaluating proficiency and establishing benchmark performance standards in the current robotic training programs proposed in the literature, our findings confirm that there is a desire for formal robotics training as reported by residents. Additionally, while over 97% of residents report at least observing a robotic surgery, less than 66% of these residents reported any formal robotics training. Given these findings, we recommend consideration of implementation of a standard robotics training program. The development of structured curriculum should consist of clear objectives and goals, a wide variety of training modalities, and be completed in a reasonable timeframe [6]. As time and access were identified as major barriers to robotic training, residency programs should consider incorporating robotic training into protected didactics time. Furthermore, the formalized curriculum should be intermittently evaluated and modified as more research becomes available about validated proficiency benchmarks, training learning curves, and efficiency of training.
References
Lee J (2015) Modern healthcare [internet]: crain communications. http://www.modernhealthcare.com/article/20150113/NEWS/301139973. Accessed 13 April 2016
Robotic Surgery in Gynecology (2015) ACOG committee opinion no. 628. American College of Obstetricians and Gynecologists. Obstet Gynecol 125(3):760–7
Schreuder HWR, Wolswijk R, Zweemer RP et al (2012) Training and learning robotic surgery, time for a more structured approach: a systematic review. BJOG 119:137–149
Gobern JM, Novak CM, Lockrow EG (2011) Survey of robotic surgery training in obstetrics and gynecology residency. JMIG 18:755–760
Smith AL, Schneider KM, Berens PD (2010) Survey of obstetrics and gynecology residents training and opinions on robotic surgery. J Robot Surg 4:23
Vetter MH, Green I, Martino M, Fowler J, Salani R (2015) Incorporating resident/fellow training into a robotic surgery program. J Surg Oncol 112(7):684–689
Patel YR, Donias HW, Boyd DW, Pandea RU, Amodeo JL, Karamanoukian RL, D’Ancona G, Karamanoukain HL (2003) Are you ready to become a robo-surgeon? Am Surg 69:599–603
Thiel DD, Patel VR, Larson T, Lannen A, Leveillee RJ (2013) Assessment of robotic simulation by trainees in residency programs of the Southeastern Section of the American Urologic Association. J Surg Educ 70(5):571–577
Vogell A, Gujral H, Wright KN, Wright VW, Ruthazer R (2015) Impact of a robotic simulation program on resident surgical performance. AJOG 213:874–875
Sheth SS, Fader AN, Tergas AI, Kushnir CL, Green IC (2014) Virtual reality robotic surgical simulation: an analysis of gynecology trainees. J Surg Educ 71:125–132
Crusco S, Jackson T, Advincula A (2014) Comparing the da Vinci si single console and dual console in teaching novice surgeon suturing techniques. JSLS 18(e2014):00218
Liang MI, McCann GA, Rath KS, Backes FJ, Cansino C, Salani R (2014) Training the next generation of robotic surgeons using guided mentorship: a randomized controlled trial. JMIG 21(6):1075–1079
Fernandes E, Elli E, Guilianotti P (2014) The role of the dual console in robotic surgical training. Surg 155(1):1–4
Farviar BS, Flannagan M, Leitman IM (2015) General surgery residents’ perception of robot-assisted procedures during surgical training. J Surg Educ 72:235–242
Arain NA, Dulan G, Hogg DC, Rege RV, Powers CE, Tesfay ST, Hynan LS, Scott DJ (2012) Comprehensive proficiency-based inanimate training for robotic surgery: reliability, feasibility and educational benefit. Surg Endosc 26(10):2740–2745
Winder JS, Juza RM, Saski J, Rogers AM, Pauli EM, Haluck RS, Estes SJ, Lyn-Sue JR (2016) Implementing a robotics curriculum at an academic general surgery training program: our initial experience. J Robot Surg 10(3):209–213
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Vetter, Hade, Fowler, Salani and Ms. Palettas declare they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Vetter, M.H., Palettas, M., Hade, E. et al. Time to consider integration of a formal robotic-assisted surgical training program into obstetrics/gynecology residency curricula. J Robotic Surg 12, 517–521 (2018). https://doi.org/10.1007/s11701-017-0775-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-017-0775-0