Abstract
To describe OB/GYN fellowship directors’ (FDs) observations, expectations, and preferences of incoming fellow’s robotic surgery preparedness. Cross-sectional study. OB/GYN FDs in gynecologic oncology, minimally invasive gynecologic surgery, female pelvic medicine and reconstructive surgery, and reproductive endocrinology and infertility in the United States. 60 FDs answered the questionnaire. Participants completed an online questionnaire about their preferences and expectations of robotic surgery experience for incoming fellows. FDs observed that many incoming first-year fellows had a baseline understanding of robotic technology (60%) and robotic bedside assist experience (53%). However, few could perform more advanced robotic tasks; with FDs indicating fellows could infrequently robotically suture (18%), or perform the entire hysterectomy (15%). FDs reported higher composite observation than expectation scores (34.3 versus 22.2, p < 0.0001), and higher preference than expectation scores (34.0 versus 22.2, p < 0.0001). The composite expectation score of high-volume divisions was greater than of low-volume divisions (23.7 versus 14.0, p = 0.04). Among the domains identified, FDs most strongly preferred their fellows be able to bedside assist, have a basic understanding of robotic technology, and have basic robotic operative skills. While incoming fellows have more robotic skill than their FDs expect, few are deemed competent to independently operate the robot. Higher volume robotic surgery divisions have higher expectations of the robotic skills of their incoming fellows compared to low-volume divisions; however, FDs neither expected nor preferred their incoming fellows to be fully competent in all aspects of robotic surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
In 2005, the Food and Drug Administration approved use of the Da Vinci Surgical System for gynecological surgery, and since then, there has been a rapid uptake of the technology, with robotic hysterectomies increasing from 0.5 to 9.5% from 2007 to 2010 [1]. Many procedures in OB/GYN practice utilize robotic technology including hysterectomy, sacrocolpopexy, adnexal surgery, myomectomy, and cancer surgery [2]. Purported benefits of the robotic platform include ease of use, the ability to perform more technically demanding cases that would have otherwise required laparotomy, and improved surgeon ergonomics and visualization [3]. The increasing prevalence of robotic surgery has corresponded with increased integration of robotic surgical training into gynecologic subspecialty practice [4].
Few studies have been conducted to assess gynecologic resident training in robotic surgery. A survey of residents conducted in 2010 found that while 78% of institutions have the capacity for robotic surgery, only 58% have incorporated formal training as part of their residency [5]. A 2009 survey of OB/GYN residents found that while 70% participated in robotic surgery in the last 12 months and 44% planned to practice robotic surgery in their careers, only 3.6% felt equipped to practice robotic surgery independently [6]. Nationwide residents have inconsistent exposure to robotic technology and experience on the console. A recent study examining graduating OB/GYN resident surgical volume found a 74-fold difference in robotic case volume between the top and bottom 10% of graduating residents [7]. A multi-center retrospective cohort study at four academic institutions and found that only 58.9% of robotic cases had resident involvement, compared with 88.6% of other surgical approaches [8].
There are few guidelines regarding resident robotic surgery training and fellowship program directors’ opinions regarding the robotic training of incoming fellows remain unknown. The purpose of this study is to describe the expectations and preferences of OB/GYN subspecialty fellowship directors (FDs) on the robotic surgery preparedness of incoming fellows. Fellowship directors’ opinions could be used to improve robotic surgery curricula for residents desiring competency in this surgical modality.
Methods
This was an Institutional Review Board-approved (IRB 13-0057) prospective, cross-sectional study using a survey of OB/GYN subspecialty FDs in fields of gynecologic oncology (GYN ONC), minimally invasive gynecologic surgery (MIGS), female pelvic medicine and reconstructive surgery (FPMRS), and reproductive endocrinology and infertility (REI). The American Board of Obstetrics and Gynecology website was used to identify GYN ONC, and REI fellowship directors; the Accreditation Council for Graduate Medical Education and the American Association of Gynecologic Laparoscopists websites were used to identify FPMRS and MIGS fellowship directors, respectively. We identified 175 accredited programs and sent those programs an open, anonymous, electronic survey to the listed contact person listed. Participation was voluntary and the survey window was open for responses between February 2014 and April 2014. Participants received one paper and three email reminders.
The multi-item survey was developed, piloted, and modified based on expert opinion and feedback from FDs and faculty at our institution. It was modeled after previously validated surveys in medical training, but altered to incorporate robotic surgery and gynecologic procedures. The authors consulted with an expert in epidemiology and survey design during its development. To establish content validity, focus groups with individuals across specialties and with varying robotic surgery experience were held and the survey was subsequently pilot tested to ensure construct validity. FDs were surveyed regarding 1) incoming fellows observed experience, 2) their expectations of incoming fellows, and 3) their preferences of incoming fellows. FDs were instructed that observations were the “experiences or skills your first-year fellows have upon starting fellowship”; expectations were “the minimum experience or skill level that you expect your fellows to have upon starting fellowship” and preferences were “the experiences or skills that you, in an ideal world, would prefer your fellows have upon starting fellowship”. The FDs were queried on 16 components of robotic surgery including bedside assisting, patient selection, robotic suturing, and operating at the console. Each of the 16 variables used a 5-item Likert-like scale, with 0 corresponding to “not at all preferred” or “not at all expected”, to 4-corresponding to “invaluable” or “mandatory” for the preference and expectation scores respectively. A copy of the survey is included in supplementary materials (Appendix 1). The composite score ranged from 0 to 64. The rankings of each of the 16 variables were summed to calculate a score for the observation, preference, and expectation domains of the survey. Responses were excluded if robotic surgery was not performed in their division, or if more than 50% of the survey questions or the surgical volume questions were unanswered. Fellowship programs were categorized as either low or high volume if the total number of robotic cases performed within the division were less or greater than 30 cases annually, respectively. The 30-case threshold for high volume was selected based on several colorectal studies that used this annual case volume as a cutoff [9, 10].
Power analysis examined the standardized difference between scores (Cohen’s d effect size) detectable by paired T test at 5% significance level and 80% power. As the sample size was predetermined, with a maximal sample size of 175, the power analysis reviewed that moderate-effect sizes were detectable, ranging from 0.25 for a 75% response rate to 0.43 for a 25% response rate. Thus, with a 25% response rate, the study would have 80% power to detect 0.43 standard deviation difference in scores at a 5% significance. Statistical analysis was performed using SAS 9.3. (SAS Institute, Cary, NC). Variables were compared by Chi-square, Fisher exact test, T test, analysis of variance, Wilcoxon rank-sum test, Kruskal–Wallis test, and Wilcoxon signed rank test as appropriate. Scores were calculated across the following domains: observation, preference, and expectation. Comparisons between domain scores were made by paired T tests. Comparisons across groups for the same domain were made by ANOVA (subspecialty) or two-sample T test. A two-tailed P value of ≤ 0.05 was deemed statistically significant.
Results
Sixty of 175 fellowship directors completed the survey for a response rate of 34%. Three respondents reported no robotic surgery within their division and were excluded from analysis, leaving 57 analyzable surveys. Table 1 lists demographics for FD respondents. FDs from all subspecialties responded to the survey. Seventy-four percent of FDs personally had robotic surgery privileges, and 84% came from departments with greater than 30 robotic surgeries annually. FDs reported that 66 and 30% of their fellows were very or somewhat interested in robotic surgery training respectively. Seventy-five percent of facilities had a dual-console robotic system and 88% reported robotic simulation training. Sixty-five percent of fellowships were 3 years in duration and conducted robotic research in their division (56%). FDs felt that the most appropriate time for robotic surgery training was residency (77%) and fellowship (75%) (Table 1).
Fellowship directors reported higher composite observation than expectation scores (34.3 versus 22.2, p < 0.0001), and higher preference than expectation scores (34.0 versus 22.2, p < 0.0001). Composite observation and preference scores were not statistically different. The composite expectation score differed across subspecialty groups, with GYN ONC having the highest score and REI the lowest. The composite expectation score of high-volume divisions was greater than of low-volume divisions (23.7 versus 14.0, p = 0.041). The composite observation and preference score did not differ across subspecialty groups or when stratified by low- and high-volume divisions. Gender of the FDs did not impact any of the domain scores (Table 2).
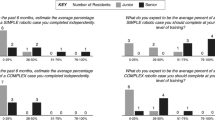
FDs observed that many incoming first-year fellows “always” or “often” had a baseline understanding of robotic technology (60%), and robotic bedside assist experience (53%). Fewer FDs felt that first-year fellows “always” or “often” had basic robotic operative skills (37%) or competence to perform robotic surgery independently (7%). When asked about their incoming fellows’ competency in specific components of robotic surgery, FDs felt that their trainees could “always” or “often” position the patient (29%), place trocars (21%), dock the robot (23%), and select appropriate robotic patients (40%). Fewer fellows could perform more advanced robotic tasks; with FDs indicating that fellows could often or always robotically suture (18%), perform parts of the hysterectomy (30%), or perform the entire hysterectomy (15%) (Fig. 1).
Few (2%) of FDs expected their incoming fellows to be able to independently perform robotic surgery. FDs felt it “mandatory” or “very much expected” for incoming fellows have a baseline understanding of technology (39%), able to observe or bedside assist (23%), or have basic robotic operative skills (11%). (Fig. 1) Similarly, a minority of FDs felt that it was “mandatory” or “very much expected” for their incoming fellows to be able to select appropriate patients (21%), position patients (16%), perform parts of the hysterectomy (14%), place trocars (11%), dock the robot (9%), and suture or perform the entire hysterectomy (9%). When asked “in an ideal world, to what extent would you prefer first-year fellows possess the following”, FDs were most interested in their fellows having observation or bedside assist experience (53%) or a baseline understanding of robotic technology (53%), followed by basic robotic operative skills (40%). (Fig. 1) The more advanced the robotic skill, the less FDs preferred them (Fig. 1).
Discussion
Robotic training in the U.S. is variable and there is limited understanding of robotic training across OB/GYN residency programs. While residents are starting fellowship with more robotic skill than their FDs expect, few are deemed competent to independently operate the robot. Higher volume subspecialties have higher robotic surgery expectations, as do FDs who come from high-volume robotic surgery divisions. Among the domains identified, FDs most strongly preferred their fellows be able to bedside assist, have a basic understanding of robotic technology, and have basic operative skills. FDs neither expected nor preferred their incoming fellows to be fully competent in all aspects of robotic surgery.
These results are consistent with the existing literature regarding the timing of robotic training. A survey of gynecologic robotic surgeons revealed that 51% of generalists and 56% of subspecialists believed that only orientation to robotic surgery should be required for residency graduation. In that survey, generalists favored residency, while subspecialists favored fellowship when asked about the ideal timing to learn to use the robot [11]. Fellowships affords additional opportunity to obtain robotic training. In another survey of OB/GYN residents, 20% of those planning additional post-graduate training in robotics sough to do so via fellowship [6]. Additionally, the percentage of residents pursing fellowship is increasing, from 7.0% in 2000 to 19.5% in 2012. [12].
Strengths of this study include the survey population, which was a diverse national representation of fellowship directors; and a survey that captured many domains relevant to robotic surgery. The survey was specific to gynecology, and afforded detailed analysis by specific components of a hysterectomy, as well as general components of robotic surgery. Fellowship directors can comment on the skills of incoming fellows in a way that may be less biased than residency program directors. Limitations of this study include response bias secondary to a 34% response rate, and the inability to verify self-reported data. It is possible that FDs interested in robotic surgery were more likely to respond to the survey. We intentionally allowed survey responses from FDs who did not personally have robotic privileges. We did not want to exclude these programs, and assumed that since all accredited programs have formative evaluations, these FDs would be able to answer questions regarding their fellows’ robotics experience. However, the fact that 26% of survey respondents did not have personal robotic privileges is a potential limitation of the study. Additionally, only subspecialists were surveyed, which limits the generalizability of the results to residents pursuing fellowship.
While this study highlights incoming fellows’ strengths, it also identifies areas for improvement in robotic surgery training. Residency program directors have a growing list of skills expected of their graduates, and not all graduates will incorporate robotic technology into their practice. Identifying trainees that have particular interest in robotic surgery would allow for more targeted training. Specific proposed strategies for improving robotic surgery education include tracking in residency [13,14,15], prioritizing robotic console time for trainees interested in robotics, and implementing a standardized gynecologic robotic curricula [16]. Such a curriculum is not available nationally, although several institutions have published experiences with their robotic curricula [16,17,18]. In addition to implementing a structured robotic training program, residency education leaders could target other barriers for simulation training including increasing time allocated for simulation, increasing the availability of the simulator, and limiting training to residents planning on using the robotic in their practice [19].
Understanding FDs expectations and preferences on robotic surgery will provide critical insight into the educational objectives for graduating residents and can be used to tailor their training, so they are maximally prepared to start fellowship.
Data availability
Available upon request.
References
Wright JD, Ananth CV, Lewin SN, Burke WM, Lu YS, Neugut AI et al (2013) Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA 309(7):689–698
Liu H, Lu D, Wang L, Shi G, Song H, Clarke J (2012) Robotic surgery for benign gynaecological disease. Cochrane Database Syst Rev (2):CD008978
Visco AG, Advincula AP (2008) Robotic gynecologic surgery. Obstet Gynecol 112(6):1369–1384
Fatehchehr S, Rostaminia G, Gardner MO, Ramunno E, Doyle NM (2014) Robotic surgery training in gynecologic fellowship programs in the United States. JSLS 18(3)
Gobern JM, Novak CM, Lockrow EG (2011) Survey of robotic surgery training in obstetrics and gynecology residency. J Minim Invasive Gynecol 18(6):755–760
Smith AL, Schneider KM, Berens PD (2010) Survey of obstetrics and gynecology residents’ training and opinions on robotic surgery. J Robot Surg 4(1):23–27
Hall EF, Raker CA, Hampton BS (2020) Variability in gynecologic case volume of obstetrician-gynecologist residents graduating from 2009 to 2017. Am J Obstet Gynecol 222(6):617.e1-617.e8
Jeppson PC, Rahimi S, Gattoc L, Westermann LB, Cichowski S, Raker C et al (2015) Impact of robotic technology on hysterectomy route and associated implications for resident education. Am J Obstet Gynecol 212(2):196.1e1-1961.e16
Rashidi L, Neighorn C, Bastawrous A (2017) Outcome comparisons between high-volume robotic and laparoscopic surgeons in a large healthcare system. Am J Surg 213(5):901–905
Bastawrous A, Baer C, Rashidi L, Neighorn C (2018) Higher robotic colorectal surgery volume improves outcomes. Am J Surg 215(5):874–878
Pickett SD, James RL, Mahajan ST (2013) Teaching robotic surgery skills: comparing the methods of generalists and subspecialists. Int J Med Robot 9(4):472–476
Rayburn WF, Gant NF, Gilstrap LC, Elwell EC, Williams SB (2012) Pursuit of accredited subspecialties by graduating residents in obstetrics and gynecology, 2000–2012. Obstet Gynecol 120(3):619–625
Hariton E, Freret TS, Nitecki R, Hinchcliff E, Stagg A (2018) Program director perceptions of subspecialty tracking in obstetrics and gynecology residency. J Grad Med Educ 10(6):665–670
Magrina JF (2014) Isn’t it time to separate the O from the G? J Minim Invasive Gynecol 21(4):501–503
Brown HL, Carson SA, Lawrence HC 3rd (2018) The first national summit on women’s health: the future of obstetrics and gynecology training. Obstet Gynecol 132(3):755–762
Geller EJ, Schuler KM, Boggess JF (2011) Robotic surgical training program in gynecology: how to train residents and fellows. J Minim Invasive Gynecol 18(2):224–229
Newcomb LK, Bradley MS, Truong T, Tang M, Comstock B, Li YJ et al (2018) Correlation of virtual reality simulation and dry lab robotic technical skills. J Minim Invasive Gynecol 25(4):689–696
Vogell A, Gujral H, Wright KN, Wright VW, Ruthazer R (2015) Impact of a robotic simulation program on resident surgical performance. Am J Obstet Gynecol 213(6):874–875
Vetter MH, Palettas M, Hade E, Fowler J, Salani R (2018) Time to consider integration of a formal robotic-assisted surgical training program into obstetrics/gynecology residency curricula. J Robot Surg 12(3):517–521
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hall, E.F., Bregar, A.J., Robison, K. et al. Ready for the robot? A cross-sectional survey of OB/GYN fellowship directors’ experience and expectations of their incoming fellow’s robotic surgical skills. J Robotic Surg 15, 723–729 (2021). https://doi.org/10.1007/s11701-020-01160-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-020-01160-w