Abstract
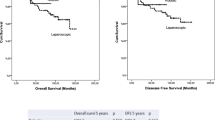
The aim of our study was to compare short-term outcomes of robotic and laparoscopic sphincter-saving total mesorectal excision (TME) in male patients with mid-low rectal cancer (RC) after neadjuvant chemoradiotherapy (NCRT). The study was conducted as a retrospective review of a prospectively maintained database, and we analyzed 14 robotic and 65 laparoscopic sphincter saving TME (R-TME and L-TME, respectively) performed by one surgeon between 2005 and 2013. Patient characteristics, perioperative recovery, postoperative complications and and pathology results were compared between the two groups. The patient characteristics did not differ significantly between the two groups. Median operating time was longer in the R-TME than in the L-TME group (182 min versus 140 min). Only two conversions occurred in the L-TME group. No difference was found between groups regarding perioperative recovery and postoperative complication rates. The median number of harvested lymph nodes was higher in the RTME than in the L-TME group (32 versus 23, p = 0.008). The median circumferential margin (CRM) was 10 mm in the R-TME group, 6.5 mm in the L-TME group (p = 0.047. The median distal resection margin (DRM) was 27.5 mm in the R-TME, 15 mm in the L-TME group (p = 0.014). Macroscopic grading of the specimen in the R-TME group was complete in all patients. In the L-TME group, grading was complete in 52 (80 %) and incomplete in 13 (20 %) cases (p = 0.109). R-TME is a safe and feasible procedure that facilitates performing of TME in male patients with mid-low RC after NCRT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Over the last two decades, the management of rectal cancer (RC) has evolved with fall in local recurrence rates and improvement in disease-free survival. This can be attributed to improved radiological staging, neoadjuvant-adjuvant chemoradiotherapy, and surgical technique [1–4]. Neoadjuvant long-course chemoradiotherapy downstages tumor, achieves complete response rates in 15–20 % patients depending on the waiting period, and may improve sphincter preservation rate [5, 6]. However, operating patients who have mid or low RC after neoadjuvant chemoradiotherapy (NCRT) is challenging with minimal invasive surgery. Additionally, laparoscopic resection of RC is a more technically demanding and has a steep learning curve because it is performed in the narrow pelvic cavity [7, 8]. Results of the United Kingdom Medical Research Council Conventional vs Laparoscopic-Assisted Surgery in Colorectal Cancer (MRC-CLASICC) showed that laparoscopic surgery for RC was associated with high rates of conversion, circumferential resection margin (CRM) positivity, and urinary/sexual dysfunction especially in male patients. Additionally, converted individuals had the most complications from surgery [9]. Considering the particular advantage of the robot in pelvic procedures, it is belived that the robotic system will overcome the limitations of laparoscopy in the narrow pelvis and could result in a benefit to the patient in the meaning of improved oncologic and functional outcomes. However, most of the published studies comparing robotic versus laparoscopic surgery for mid or low RC do not specifically focused on male mid or low RC patients received NCRT [10–14]. We therefore designed a study to compare perioperative and oncological short-term outcomes of laparoscopic and robotic resections for mid or low RC in male patients after NCRT.
Patients and methods
A retrospective analysis was carried out based on a RC database collected prospectively between January 2005 and December 2013. Fourteen robotic rectal resections with TME (R-TME) were compared to the 65 laparoscopic rectal resections with TME (L-TME) from the 306 patients who underwent minimally invasive TME performed from 2005 to 2013. Robotic procedures were performed from January 2013 to December 2013. Robotic and laparoscopic resections were performed by a single surgeon (OA) at two different centers (Istanbul University Faculty of Medicine, Department of General Surgery, Istanbul, Turkey and Liv Hospital, Department of General Surgery, Istanbul, Turkey).
Patients with male gender, mid or low RC, cT3-4, N(−)/(+) lesions without distant metastasis, having sphincter-saving TME after NCRT were inclusion criteria of the study. RC was defined as pathologically demonstrated adenocarcinoma located in the rectum, 10 cm or less from the anal verge with the rigid sigmoidoscope. The low rectum was defined as 0–5 cm from the anal verge, the mid rectum as 6–10 cm, and the upper rectum as 11–15 cm. All patients were carefully assessed preoperatively. Patient characteristics, body mass index (BMI), and American Society of Anesthesiologists (ASA) scores [15] were evaluated. The preoperative staging included chest X-ray, assessment of carcinoembryonic antigen (CEA) levels, total colonic examination with flexible or virtual colonoscopic technique, abdominal computed tomography (CT), pelvic-phased array magnetic resonance imaging (MRI), and/or endorectal ultrasound. Patients with clinical T3, T4 or node-positive disease (stage II and III) initially treated with either neoadjuvant long-course chemoradiotherapy [45–50.4 Gy pelvic irradiation with concomitant 5-fluorouracil (5-FU) and leucoverin (FUFA)], or short-course radiotherapy (25 Gy pelvic irradiation). Short-course radiotherapy was preferred in a selected group of patients without any risk of lateral margin positivity. The waiting period was 4–8 weeks for long-course radiotherapy, and 1–4 weeks for short-course radiotherapy. After completion of surgery, all patients treated with neoadjuvant protocol and diagnosed with pT3 and/or any N positivity were treated with four courses of FUFA. Mechanical bowel preparation was carried out by the administration of both oral and rectal sodium phosphate preparations the day before surgery. All patients received preoperative antibiotic prophylaxis as a combination of single doses of 1.5 g cefuroxime axetil and 500 mg metronidazole administered intravenously. Prophylaxis for deep vein thrombosis was carried out via the administration of low molecular weight heparin and the application of anti-embolic stockings. According to the protocol of our department, the prophylaxis continued until the end of the 30th day following the discharge.
Our technique of L-TME has been described before [16–18]. With the patient placed supine in the lithotomy position, 5 trocars were positioned. High ligation of the inferior mesenteric artery and vein was carried out, and sharp pelvic dissection was performed. The distal rectum was transected using a laparoscopic linear stapler intracorporeally. Anastomosis was carried out intracorporeally using a circular stapler. For ultra-low anterior resections, hand-sewn coloanal anastomosis was performed.
For the R-TME, we used total robotic dissection with single-stage double-phase, full robotic technique. In brief, totally robotic dissection procedure performed without changing the position of the robotic cart. Instead, only the robotic arms were repositioned between 2 phases: (1) vascular ligation, and sigmoid colon to splenic flexure mobilization; and (2) pelvic total mesorectal excision. All robotic procedures were performed using a four-arm Da Vinci-S Surgical System (Intuitive Surgical, Sunnyvale, CA). Six ports were used, including one 12-mm camera port, four 8-mm robotic working ports, and one 12-mm port for the assistant (Fig. 1a, b). The robotic cart is positioned on the patient’s left side along the imaginary line between the anterosuperior iliac spine and the umbilicus at a 60° angle. In the colonic phase, the inferior mesenteric artery and vein were divided, followed by medial-tolateral dissection, including splenic flexure mobilization. Robotic arms 2 and 3 were changed from R2-I to R2-II and from R3-I to R3-II (Fig. 1a, b) for pelvic dissection. The pelvic phase involved dissection of the TME plane until circumferential dissection of the rectum was complete. Once the TME is completed, the distal rectum is divided by the assistant using a reticulating 30-mm linear stapler through the 12-mm laparoscopic port. The specimen is extracted through a minilaparotomy. In patients with low rectal tumors without sphincter involvement, ISR and a hand-sewn coloanal or double staple technique anastomosis was created.
a Trocarpositions in robotic total mesorectal excision for rectal cancer. R1, R2, and R3: 8-mm trocarsconnected to robotic arms; Assistant port, 12-mm trocar; C: 12-mm trocar for robotic camera. b Placment of robotic arms at first (I) and second (II) phase. The position of robotic arms 2 and 3 were changed from I to II between two phases of procedure
Perioperative outcomes included operation time, conversion to an open procedure, the time to first passage of flatus, the time to a resumed a soft diet, and the length of hospital stay. Conversion was defined as any unplanned laparotomy at any time during surgery, regardless of the incision length. Postoperative complications were defined as adverse events that occurred within 30 days after surgery. All pathology specimens were examined to determine tumor size, the number of lymph nodes harvested, microscopic proximal, distal and circumferantial resection margins (PRM, DRM and CRM, respectively), and the integrity of the mesorectum. Surrogates of oncologic outcome were then compared between L-TME and R-TME groups.
Statistical analysis
All statistical analyses were performed using SPSS software, version 18.0 (SPSS, Chicago, IL). Categorical variables were analyzed using the ×2 or Fisher’s exact test, and continuous variables were analyzed using the Student’s t test/Mann–Whitney U rank tests. P values <0.05 were considered statistically significant.
Results
Between January 2005 and December 2013, minimal invasive surgery was applied in 306 patients with RC by a single surgeon. Seventy-nine patients met the study inclusion criteria; 65 had L-TME and 14 had R-TME. Characteristics of the entire study population are presented in Table 1. No significant difference in age, BMI, and ASA score was observed between the two groups.
Table 2 summarizes perioperative outcomes. There was no conversion noted in RTME group whereas two patients in the L-TME group were converted to open surgery. The median operation time was significantly longer in the R-TME group than in the L-TME group (p < 0.05). The median time to the first passing of flatus was 2 days in the R-TME group (range 1–5 days) and 1 day in the L-TME group (range 1–11 days) (p = 0.4); the median time to resume a soft diet was 2 days (range 1–5 days) in the R-TME group and 2 days (range 1–12 days) in the L-TME group (p = 0.9). There was no difference with regard to the length of hospital stay [5 days (range 4–10 days) in R-TME group vs 6 days (range 4–32 days) in LTME group].
The overall complication rate was 14.3 % for the R-TME group and 24.6 % for the LTME group (p = 0.502) (Table 3). There were one (7.1 %) anastomotic leak in the R-TME group and 6 (9.2 %) in the L-TME group. All patients with leakage was treated conservatively, by maintaining pelvic drainage until the infection that was present had resolved clinically. In the L-TME group, three wound infections, two ileostomy-related complications, and two urinary tract infections occurred. Detailed evaluation of postoperative complications is summarized in Table 3.
Pathological findings are presented in Table 4. Tumor size and specimen length were similar in both groups. The median number of harvested lymph nodes was 32 (range17–56) in the R-TME group and 23 (range 4–67) in the L-TME group (p = 0.008). The median PRM did not differ significantly between the two groups. The median DRM was 27.5 mm (range 5–60 mm) for R-TME and 15 mm (range 10–70 mm) for L-TME (p = 0.014). The median CRM (CRM) were 10 mm (range 1–30 mm) in the R-TME group and 6.5 mm (range 0–35 mm) in the L-TME group (p = 0.047). The CRM was positive in a one patient in R-TME group (1 mm) and 3 patients in L-TME group (1 mm in a one and 0 mm in two patients). Macroscopic grading of the specimen in the R-TME group was complete in all patients. In the L-TME group, grading was complete in 52 (80 %) cases and incomplete in 13 (20 %) cases. The difference between two groups was not found statistcally significant.
Discussion
Achieving a TME is a key oncological principle when resecting the rectum for mid or low cancer, and particularly challenging when attempted laparoscopically in male patients after NCRT. This is because performing a L-TME with meticulous and precise dissection of the mesorectum in a previously irradiated rectum down to the pelvic floor within the confines of a narrow pelvis requires a series of complex moves, which are not only operator but also assistant/cameraman dependent and demands a high level of experience and has a significant learning curve [16]. In addition, laparoscopic instruments are known to have several limitations such as inability to perform high precision suturing, poor ergonomics, and fixed tips with limited dexterity. Robotic rectal resection has been suggested as a means of overcoming the difficulties of the laparoscopic approach and improving the adoption of minimally invasive rectal surgery. Some of the benefits of the robotic system include a stable, high-definition, 3D image, a finer dissection with articulated tools, and better ergonomics for the surgeon [10–14]. All these aspects may contribute to improve quality of TME. Here we compared our short-term outcomes of R-TME and L-TME in a challenging patient population.
Operative time has been previously noted as a potential drawback of robotic surgery. Operating time was higher in the R-TME group compared with the L-TME group; however it was acceptable. In previous studies [10–12], the high heterogeneity and inconsistency in the analysis of operating time depended on the inclusion of different colorectal surgical procedures such as anterior resection and abdomino-perineal resection of the rectum in robotic series. However, Baik et al. [10] have reported shorter operating time for robotic RC resections using a hybrid technique. Operating time may also depend on the experience, skill of the surgeon, and technique used, whether fully robotic or the hybrid technique.
Conversion in laparoscopic RC surgery has been associated with suboptimal postoperative outcome [19–21]. In the present series, none of the R-TME patients and two of the L-TME patients was converted to laparotomy. Despite the challenges posed by the more complex surgical cases, our conversion rate for whole patient population was extremely low. The low number of conversions in our series partly reflects the technical skills of the surgeon but mainly demonstrates the advantages of robotic surgery described earlier, which make a very technically challenging procedure relatively easy. Recent meta-analysis of Xiong et al. [22] showed that the conversion rate was significantly lower in the robotic rectal resection group than in the laparoscopic rectal resection group (6/554 versus 35/675). The most frequent reason for conversion is difficulty in pelvic dissection the most important variable for assesing the quality of TME. Rottoli et al. [23] suggested that patients undergoing conversion after laparoscopic rectal resection showed a trend toward overall higher recurrence rates. Chan et al. [24] analyzed 470 colorectal resections and detected that converted patients were more likely to develop local recurrence in addition to showing a reduced disease-free survival rate. A German multi-center observational trial found a higher local recurrence rate in patients who required conversion to open surgery [25]. Thorpe et al. [26], analyzing 131 laparoscopic TME included in the CLASICC trial, identified male sex as a risk factor for conversion. Thus, use of robotic system in male patients with mid or low RC may reduce conversion rates and may have an impact on improving patient oncological outcome. Regarding, time to passing first flatus, time to resume a soft diet and length of hospital stay, both minimally invasive approaches resulted in a very fast recovery. We found no differences between the robotic and laparoscopic groups in the perioperative evolution of patients. This finding agrees with all the analyzed studies but one: Baik et al. [10] reported significant reduction in the time needed to reintroduce a soft diet after robotic surgery, in spite of no difference between the groups in the time to first passing flatus. Moreover, that study found shorter hospital stay in the robotic group [10].
With respect to overall complication rate, the incidence reported for the robotic groups varied from 10.7 % [27] to 30.6 % [28]. For the laparoscopic groups, these data varied from 12.2 % [12] to 20 % [11]. However, no significant differences were found between groups, either by studies or by meta-analysis of pooled data [23, 29]. In the present study, we found no significant differences in terms of complications between laparoscopic and robotic TME, although there were numerically fewer complications in the robotic group. In our study, the overall complication rate was 14.3 % in the R-TME group and 24.6 % in the L-TME group. These results were similar with the literature. Results of Xiong et al. meta-analaysis emphasized that the area, location of the tumor, and TNM stage had no influence on complication, but neoadjuvant chemoradiotherapy might affect the postoperative outcomes. Current study demonstrated that R-TME reduced overall complications in male patients with mid or low RC received NCRT. The most important variable for assessing the quality of TME is precise pelvic dissection. This variable can primarily be measured by CRM and DRM, the completeness of the mesorectum, the recurrence rate, and overall survival rates. The CRM is one of the strongest predictors of surgical quality for TME [30, 31]. Standardized TME procedures performed by experienced surgeons reduce the possibility of obtaining CRM-positive specimens [18]. A positive CRM is defined as a direct tumor extension within 1 or 2 mm of the radial, nonperitonealized surface of the resection specimen [32, 33]. Previous studies have generally used a threshold of <1 mm to define CRM involvement. However, a margin of >2 mm between the tumor tissue and the CRM has been reported to be associated with decreased local recurrence and decreased rates of distant metastases [33, 34]. Although higher positivity of the CRM did not translate into an increased incidence of local recurrence at 3 year follow-up in the MRC-CLASICC trial, the difference in CRM involvement was thought to reflect the greater technical difficulties associated with laparoscopic RC surgery [9]. In addition, the high rate of CRM positivity reported in the Colorectal Cancer Laparoscopic or Open Resection (COLOR) II trial also raised concerns regarding the feasibility of the laparoscopic approach for RC [35]. Therefore, the precise dissection afforded by R-TME might be expected to improve the pathological outcomes. Three studies have evaluated the outcomes of robotic and laparoscopic surgery for mid and low RC [10–12]. However, these studies also included patients who did not receive preoperative radiotherapy. In the prospective study by Baik et al. [10], the CRM involvement was not found statistically different between laparoscopic and robotic low anterior resection groups. On the contrary, recent meta-analysis showed that the rate of positive CRM was lower in R-TME group than in LTME group [22]. In our study, the overall rate of CRM involvement was observed in 3 patients in the L-TME group and 1 patients in the R-TME group. The median CRM length was higher in R-TME group than in the L-TME group, the difference for CRM length between the two groups was found statistically significant. Robotic surgery allowed us to achieve a complete and oncologically adequate resection of the specimen without CRM involvement compared to the laparoscopic group.
Our results demonstrate that the R-TME can be carried out safely with a high success rate and following oncological principles. In this study, the number of harvested lymph nodes and the length of DRM in patients receiving R-TME were higher in patients receiving LTME. The main reason for high length of DRM in R-TME group was most of the patients in R-TME group received ISR as transection of rectum with a laparoscopic stapler technically not feasible for low or mid RC with our R-TME approach. In our practice, we placed two robotic arms right lower quadrant in order to achive single-stage technique without reposition of robotic cart. However, location of the robotic arms at right lower quadrant did not allow placing laparoscopic stapler with adequate angulation for transection of the rectum. We belive that robot offers significant advantages of precise pelvic dissection, but because of robotic stapler device has not been available yet, patients with low or mid RC receive R-TME with ISR most of the time for safe transection of the rectum. The quality of the specimen is considered a parameter for the evaluation of prognosis [36]. Therefore, in our study, macroscopic evaluation of TME completeness was evaluated as an additional parameter for evaluation of the oncologic safety of the procedure. The macroscopic grading of the specimen in L-TME group was complete in 52 (80 %) cases and incomplete in 13 patients (20 %), in the R-TME group the grading was complete in all cases (100 %). The difference between the direction and strength of the applied tractions by the robotic instruments and those of the conventional laparoscopic instruments could be a factor influencing the quality of the specimen and, typically, the mesorectal fascia integrity. The meta-analysis by Xiong et al. [22] reported that among the eight included studies only two of them [10, 37] evaluated the completeness of mesorectum. Baik et al. [10] pointed out that the macroscopic completeness of TME can represent the quality of dissection more precisely than positivity of the CRM, because involvement of the CRM is also influenced by tumor location in relation to the fascia propria of the rectum. They [10, 38] suggested that the macroscopic evaluation of TME completeness should be an additional parameter for assessing surgical quality especially in cases with CRM involvement to ensure the oncologic safety of the procedure.
This study had important limitations. First, it was a retrospective study of prospectively collected data from a single surgeon highly experienced in performing laparoscopic colorectal resection, and there was a definite difference between the two operative techniques with regard to the surgeon’s expertise. Second, the number of performed procedures is quite low because of the restricted study population and this study was not a randomized trial so we included a special group of patients to study in order to obtain homogenization between the groups and achieve reliable results. However, a prospective randomized study is needed to demonstrate that robotic TME with SSP truly is a feasible procedure for very low rectal cancer.
In conclusion, robotic surgery for mid and low RC after NCRT can be performed safely in male patients. The very low conversion rate for this procedure is the main advantage over the L-TME. The results of this study showed that R-TME associated with better short-term oncological outcomes than the L-TME. Therefore, R-TME may be a promising alternative to L-TME in the treatment of RC. However, further prospective randomized trials are needed to clarify our initial findings and to assess the long-term oncological and functional outcomes of robot-assisted surgery for mid or low RC.
References
Daniels IR, Fisher SE, Heald RJ, Moran BJ (2007) Accurate staging, selective preoperative therapy, and optimal surgery improves outcome in rectal cancer: a review of the recent evidence. Colorectal Dis 9:290–301
Kapiteijn E, Putter H, van de Velde CJ, Cooperative investigators of the Dutch ColoRectal Cancer Group (2002) Impact of the introduction and training of total mesorectal excision on recurrence and survival in rectal cancer in The Netherlands. Br J Surg 89:1142–1149
Martling A, Holm T, Rutqvist LE et al (2005) Impact of a surgical training program on rectal cancer outcomes in Stockholm. Br J Surg 92:225–229
Wibe A, Møller B, Norstein J et al (2002) Norwegian Rectal Cancer Group. A national strategic change in treatment policy for rectal cancer–implementation of total mesorectal excision as routine treatment in Norway. A national audit. Dis Colon Rectum 45:857–866
Minsky BD, Cohen AM, Kemeny N et al (1993) The efficacy of preoperative 5-fluorouracil, high-dose leucovorin, and sequential radiation therapy for unresectable rectal cancer. Cancer 71:3486–3492
Theodoropoulos G, Wise WE, Padmanabhan A et al (2002) T-level downstaging and complete pathologic response after preoperative chemoradiation for advanced rectal cancer result in decreased recurrence and improved disease-free survival. Dis Colon Rectum 45:895–903
Staudacher C, Vignali A (2010) Laparoscopic surgery for rectal cancer: the state of the art. World J Gastrointest Surg 2:275–282
Poon JT, Law WL (2009) Laparoscopic resection for rectal cancer: a review. Ann Surg Oncol 16:3038–3047
Guillou PJ, Quirke P, Thorpe P et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomized controlled trial. Lancet 365:1718–1726
Baik SH, Kwon HY, Kim JS et al (2009) Robotic versus laparoscopic low anterior resection of rectal cancer: short-term outcome of a prospective comparative study. Ann Surg Oncol 16:1480–1487
Bianchi PP, Ceriani C, Locatelli A et al (2010) Robotic versus laparoscopic total mesorectal excision for rectal cancer: a comparative analysis of oncological safety and short-term outcomes. Surg Endosc 24:2888–2894
Park JS, Choi GS, Lim KH, Jang YS, Jun SH (2010) Robotic-assisted versus laparoscopic surgery for low rectal cancer: case-matched analysis of short-term outcomes. Ann Surg Oncol 17:3195–3202
Saklani AP, Lim DR, Hur H et al (2013) Robotic versus laparoscopic surgery for mid-low rectal cancer after neoadjuvant chemoradiation therapy: comparison of oncologic outcomes. Int J Colorectal Dis 28:1689–1698
Fernandez R, Anaya DA, Li LT et al (2013) Laparoscopic versus robotic rectal resection for rectal cancer in a veteran population. Am J Surg 206:509–517
Owens WD, Felts JA, Spitznagel EL Jr (1978) ASA physical status classifications: a study of consistency of ratings. Anesthesiology 49:239–243
Balik E, Asoglu O, Saglam S et al (2010) Effects of surgical laparoscopic experience on the short-term postoperative outcome of rectal cancer: results of a high volume single center institution. Surg Laparosc Endosc Percutan Tech 20:93–99
Asoglu O, Balik E, Kunduz E et al (2013) Laparoscopic surgery for rectal cancer: outcomes in 513 patients. World J Surg 37:883–892
Asoglu O, Kunduz E, Rahmi Serin K et al (2014) Standardized laparoscopic sphincter preserving total mesorectal excision for rectal cancer: long-term oncologic outcome in 217 unselected consecutive patients. Surg Laparosc Endosc Percutan Tech 24:145–152
Leroy J, Jamali F, Forbes L et al (2004) Laparoscopic total mesorectal excision (TME) for rectal cancer surgery: long-term outcomes. Surg Endosc 18:281–289
Morino M, Parini U, Giraudo G et al (2003) Laparoscopic total mesorectal excision: a consecutive series of 100 patients. Ann Surg 237:335–342
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ (2010) Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 97:1638–1645
Xiong B, Ma L, Zhang C, Cheng YJ (2014) Robotic versus laparoscopic total mesorectal excision for rectal cancer: a meta-analysis. Surg Res 188:404–414
Rottoli M, Bona S, Rosati R et al (2009) Laparoscopic rectal resection for cancer: effects of conversion on short-term outcome and survival. Ann Surg Oncol 16:1279–1286
Chan AC, Poon JT, Fan JK, Lo SH, Law WL (2008) Impact of conversion on the long-term outcome in laparoscopic resection of colorectal cancer. Surg Endosc 22:2625–2630
Ptok H, Steinert R, Meyer F et al (2006) Long-term oncological results after laparoscopic, converted, and primary open procedures for rectal carcinoma. Results of a multicenter observational study. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 77:709–717
Thorpe H, Jayne DG, Guillou PJ, Quirke P, Copeland J, Brown JM (2008) Medical research council conventional versus laparoscopic-assisted surgery in colorectal cancer trial G. Patient factors influencing conversion from laparoscopically assisted to open surgery for colorectal cancer. Br J Surg 95:199–205
Maeso S, Reza M, Mayol J et al (2010) Efficacy of the Da Vinci surgical system in abdominal surgery compared with that of laparoscopy. Ann Surg 252:254–262
Patriti A, Ceccarelli G, Batoli A et al (2009) Short and medium term outcome of robotassisted and traditional laparoscopic rectal resection. JSLS 13:176–183
Ortiz-Oshiro E, Sánchez-Egido I, Moreno-Sierra J, Pérez CF, Díaz JS, Fernández-Represa JÁ (2012) Robotic assistance may reduce conversion to open in rectal carcinoma laparoscopic surgery: systematic review and meta-analysis. Int J Med Robot 8:360–370
Kelly SB, Mills SJ, Bradburn DM, On behalf of the Northern Region Colorectal Cancer Audit Group et al (2011) Effect of the circumferential resection margin on survival following rectal cancer surgery. Br J Surg 98:573–581
Huang MJ, Liang JL, Wang H et al (2011) Laparoscopic-assisted versus open surgery for rectal cancer: a meta-analysis of randomized controlled trials on oncologic adequacy of resection and long-term oncologic outcomes. Int J Colorectal Dis 26:415–421
Quirke P, Dixon MF (1988) The prediction of local recurrence in rectal adenocarcinoma by histopathological examination. Int J Colorectal Dis 3:127–131
Nagtegaal ID, Marijnen CA, Kranenbarg EK, Pathology Review Committee et al (2002) Cooperative Clinical Investigators Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma: not one millimeter but two millimeters is the limit. Am J Surg Pathol 26:350–357
Anderson C, Uman G, Pigazzi A (2008) Oncologic outcomes of laparoscopic surgery for rectal cancer: a systematic review and meta-analysis of the literature. Eur J Surg Oncol 34:1135–1142
van der Pas MH, Haglind E, Cuesta MA, Colorectal Cancer Laparoscopic or Open Resection II (COLOR II) Study Group et al (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–218
Nagtegaal ID, van de Velde CJ, van der Worp E, Kapiteijn E, Quirke P, van Krieken JH (2002) Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol 20:1729–1734
Kim JY, Kim NK, Lee KY, Hur H, Min BS, Kim JH (2012) A comparative study of voiding and sexual function after total mesorectal excision with autonomic nerve preservation for rectal cancer: laparoscopic versus robotic surgery. Ann Surg Oncol 19:2485–2493
Kwak JM, Kim SH, Kim J, Son DN, Baek SJ, Cho JS (2011) Robotic vs laparoscopic resection of rectal cancer: short-term outcomes of a case-control study. Dis Colon Rectum 54:151–156
Conflict of interest
Author Oktar Asoglu, Author Fatma Ayca Gultekin, Author Burcin Batman, Author Serden Ay, Author Kursat Rahmi Serin, Author Yersu Kapran, and Author Sezer Saglam declare that they have no conflicts of interest or financialties to disclose.
Ethical standard
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Serin, K.R., Gultekin, F.A., Batman, B. et al. Robotic versus laparoscopic surgery for mid or low rectal cancer in male patients after neoadjuvant chemoradiation therapy: comparison of short-term outcomes. J Robotic Surg 9, 187–194 (2015). https://doi.org/10.1007/s11701-015-0514-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-015-0514-3