Abstract
Background
Long-term outcome of patients with conversion following laparoscopic resection of colorectal cancer has seldom been reported. This study aimed to evaluate the impact of conversion on the operative outcome and survival of patients who underwent laparoscopic resection for colorectal malignancy.
Methods
An analysis of a prospectively collected database of 470 patients who underwent laparoscopic colectomy between May 2000 and December 2006 was performed. The operative results and long-term outcomes of patients with conversion were compared with those with successful laparoscopic operations.
Results
The overall conversion rate to open surgery was 8.7% (41 patients). There was no difference in age, comorbid illness, location of tumor, and stage of disease between the laparoscopic and conversion groups. The most common reasons for conversion include adhesions (34.1%), tumor invasion into adjacent structures (17.1%), bulky tumor (9.8%), and uncontrolled hemorrhage (9.8%). A male preponderance was observed in the conversion group. Tumor size was significantly larger in the conversion group compared with the laparoscopic group (5 versus 4 cm, P = 0.002). Although there was no difference in the operative time between the two groups, increased perioperative blood loss (461.9 vs. 191.2 ml, P < 0.001), increased postoperative complication rate (56.1% versus 16.7%, P = 0.001) and prolonged median hospital stay (10 versus 6 days, P < 0.001) were associated with the conversion group. Consequently, patients in the conversion group were more likely to develop local recurrence (9.8% versus 2.8%, P < 0.001) with a significantly reduced cumulative cancer-free survival.
Conclusion
The disease-free survival and the local recurrence were significantly worse by the presence of conversion in laparoscopic resection for colorectal malignancy. Adoption of a standardized operative strategy may improve the perioperative outcome after conversion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The role of laparoscopic colectomy in the management of colorectal cancer (CRC) has become well established in recent years. The short-term benefits in operative outcome in terms of faster recovery of bowel function, less postoperative pain, and reduced hospital stay have been demonstrated in multicenter randomized controlled trials [1,2]. Although laparoscopic colectomy is the preferred approach for treating CRC by many surgeons, conversion to open procedure is sometimes necessary due to technical difficulties such as the presence of a bulky tumor, adhesions or adjacent organ invasion. Conversion is also sometimes inevitable in cases of intraoperative complications. The need for conversion subjects patients to adverse factors such as prolonged operating time, increased blood loss, and the need for blood transfusion. However, only a small number of studies have addressed the issue of conversion in laparoscopic surgery with respect to its impact on the long-term outcome in patients with CRC [1, 3]. The objective of this study was to evaluate if conversion would confer a negative impact on the long-term survival of patients who had laparoscopic resection of colorectal cancer.
Patients and methods
This is a study on the prospectively collected data of 470 patients who underwent laparoscopic resections of colorectal cancer between May 2000 and December 2006 in the Department of Surgery, University of Hong Kong Medical Centre. Patient demographics, operative details including blood loss and duration of operation, reasons for conversion, postoperative outcomes including morbidity and mortality, and length of hospital stay were reviewed. All resections were performed by colorectal surgeons with an interest in laparoscopic surgery. Most patients underwent preoperative bowel preparation including fluid diet and polyethylene glycol electrolyte solution 1 day before operation unless there were contraindications against bowel preparation. Intravenous antibiotic prophylaxis was given on induction of anesthesia for operation. Intracorporeal dissection was performed, mainly with ultrasonic dissector. Mobilization of the large bowel and division of major vessels were performed intracorporeally. From the latter half of 2004, a standardized medial to lateral approach was utilized in colon and rectal mobilization. For mid and low rectal cancer, total mesorectal excision was performed. Following bowel mobilization and vessel division, the tumor-bearing segment was retrieved through an incision with wound protection, except for abdominoperineal resection in which cases the specimens were retrieved through the perineal wound. Bowel anastomosis was performed extracorporeally for right hemicolectomies and intracorporeally using circular staplers with a double-stapled technique for most left-sided and rectal lesions. Conversion was defined as: (1) the need to perform conventional laparotomy in order to accomplish the procedure or (2) premature abdominal incision for colorectal dissection or vascular control. Diversion stoma was carried out when anastomosis was preformed within 5 cm from anal verge or if the anastomosis was considered hazardous. Morbidities were defined as complications that required additional treatment or prolonged hospital stay. Operative mortality was defined as death within 30 days after operation. All morbidities and mortalities were recorded prospectively. Local recurrence was defined in colon cancer as tumor recurrence at the tumor bed in the vicinity of the previous anastomotic site. In cases of rectal cancer, local recurrence was considered to be present when the relapse of the disease was present in the pelvis. All resected specimens were examined by surgeons after operation and then sent for histological examination. Tumor size, proximal, and distal resection margin was measured by surgeons from the fresh specimen. The International Union against Cancer/American Joint Committee on Cancer (UICC/AJCC) colorectal cancer staging system was adopted for tumor staging, and advanced tumor was defined as T3 or T4 stage tumor. Statistical analysis was performed using Statistical Package for Social Sciences (SPSS, Version 15.0, Chicago, IL, USA). Student’s t-test was used for analysis of continuous variables and the chi-square test was used for analysis of categorical variables. Survival was analyzed with the Kaplan–Meier method and comparison was made with the log-rank test. Only patients with stage I–III disease were included in survival analysis. In the analysis of disease-free survival, the patients with postoperative mortality were excluded. A P-value of less than 0.05 was considered statistically significant.
Results
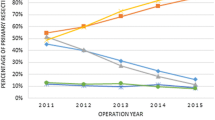
Four hundred and seventy patients (268 males) were included in the study with a median follow-up of 30.8 months. The median age was 69 years. Conversions to open surgery occurred in 41 patients (8.7%). Patient demographics, tumor characteristics including location and stage, history of previous abdominal surgery and adjuvant treatment for CRC are presented in Table 1. There was no difference in age, comorbid illness, stage of disease, incidence of previous abdominal surgery, and use of neoadjuvant chemoradiation between patients with successfully performed laparoscopic resection and those with conversion, except that there was a male preponderance in the conversion group. The common reasons for conversion are presented in Table 2; they included adhesions (34.1%), local invasion into adjacent structures (17.1%), intraoperative hemorrhage (9.8%), and bulky tumor (9.8%). The conversion rates between laparoscopic resection for rectal cancer and colon cancer were similar (7.2% versus 12.3%, P = 0.16). There was a noticeable decline in the conversion rate over the years as the experience of the operating surgeons improved. The conversion rate from 2000 to 2003 was 10.4% while the conversion rate from 2004 to February 2007 was 5.8%. As shown in Table 3, patients in the conversion group had a significantly larger tumor size than those in the laparoscopic group (4.0 versus 5.0 cm, P < 0.001). However, there was no significant difference in the stages of the tumors, although there was a trend for more patients with advanced T-stage tumors in the conversion group. Nonetheless, tumor clearance was not jeopardized with the need for conversion, as demonstrated by a similar number of lymph nodes harvested and length of resection margins between the two groups of patients. Conversion was associated with a significant increase in operative blood loss (191.2 versus 461.9 ml, P < 0.001), postoperative complication rate (56.1% versus 16.8%, P < 0.001) and prolonged hospital stay (10 versus 6 days, P < 0.001). The postoperative complications in the two groups of patients are compared in Table 4. One patient in the laparoscopic group died 22 days after the operation because of postoperative bleeding duodenal ulcer, which required reoperation for hemostasis. One patient in the conversion group who had pre-existing cirrhosis died of liver failure and pneumonia 30 days after the operation. Despite the association with increased blood loss and postoperative complication, conversion did not result in increased operative mortality. However, patients in the conversion group had a significantly higher chance to develop local recurrence than those in the laparoscopic group (9.8% versus 2.8%; Table 5). The pattern of recurrence is shown in Table 5. Of the 12 patients who developed local recurrence in the laparoscopic group, all patients except two had cancer in the rectum or rectosigmoid junction, whereas all local recurrences in the conversion group were found in patients who had rectal cancer. The two patients who had colonic cancer in the laparoscopic group developed recurrence in the tumor bed in the vicinity of the anastomosis. The mean time to local recurrence for the laparoscopic and conversion groups was 28.0 and 28.9 months, respectively (P = 0.78). Excluding patients with stage IV disease, it was shown that patients in the conversion group had worse cumulative disease-free survival than those in the laparoscopic group (Fig. 1). There was also a trend towards reduced overall survival for patients in the conversion group but the difference did not reach statistical significance (Fig. 2).
Discussion
Laparoscopic colectomy is a technically challenging procedure that usually involves mobilization of bowel in different quadrants of the peritoneal cavity, dissection and ligation of sizable vessels which could result in severe hemorrhage if inadvertently damaged, and construction of an anastomosis. The learning curve is steep and experience of an average of 40–60 cases is needed to achieve mastery of the skills [4, 5]. Despite the improved surgical technique and advancement in laparoscopic instrumentation, conversion still occurred in 10–29% of the patients who underwent laparoscopic colectomy [3, 6–9]. However, conversion should not be viewed as a complication but as a solution to overcome the limitation of laparoscopic surgery. A number of studies had addressed the impact of conversion on the short-term outcome of laparoscopic colectomy [8, 10, 11]. Increased postoperative morbidity and prolonged hospital stay were the main adverse outcomes identified in these studies [11, 12]. The present study also showed a higher incidence of postoperative complications and prolonged hospital stay in the conversion group. In the study by Marusch et al. [12], both overall and surgically-related complication rate were higher in the conversion group compared with the group with successful laparoscopic procedures. A meta-analysis of 28 nonrandomized studies showed that prolonged operative time and length of hospital stay were associated with conversion [6]. Over half of our patients with conversion developed complications. The significant proportion of complications in the conversion group could be attributed to the prolonged operation or significant operative blood loss, which may increase the body stress response and dampen the host immune response, leading to increase susceptibility to develop postoperative complications. A study by Kiran et al. also showed that open colectomy was associated with increased blood loss and blood transfusion requirement when compared with laparoscopic colectomy [13]. Despite the increased operative blood loss encountered in the conversion group, there was no significant difference in the operative time between the two groups of patients. This was a reflection of early and prompt decision for conversion as a common practice among our colorectal surgeons and was consistent with the suggestion by Agachan et al. that, when the decision for conversion was taken early on, the duration of the procedure was not significantly prolonged [14]. However, the clinical significance of early versus late conversion needs to be elucidated in future trials.
One common pitfall in most studies that have evaluated the consequence of conversion was that they usually contained a heterogeneous group of conditions and the impact of conversion on long-term survival of cancer patients was often not evaluated. The present study represented one of the few studies that evaluated the prognostic influence of conversion on laparoscopic resection of colorectal cancers. Patients in the conversion group had higher incidence of local recurrence and correspondingly worsened disease-free survival. This partly may be contributed by the higher percentage of advanced (T3 and T4) tumors in the conversion group, though this did not reach statistical significance. In a recent retrospective study of 377 laparoscopic colorectal resections, Moloo et al. found that patients with stage IV disease had a higher chance of conversion than those with stage I–III disease [3]. This result indicated the local extent of the disease which attributed to difficulty in mobilizing the tumor-bearing segment. Another study by Tekkis et al. found that the conversion rate in T3–4 tumors was remarkably higher than those with T1–2 tumors [9]. The present study also showed similar findings in which the median gross tumor size was significantly larger in the conversion group than those in the laparoscopic group. Patients with T3–4 tumor had almost four times the risk to undergo conversion than those with T0–2 tumors (11.4% versus 3.1%). In contrast to Moloo et al.’s study in which exposure was the most common reason for conversion [3], difficulty in dealing with adhesions and advanced bulky tumors was the main culprit in our study. We demonstrated a lower local recurrence and a better disease-free survival in patients with laparoscopically completed operation. In contrast to Moloo et al.’s study, our study did not show any difference in overall survival between the two groups of patients. This is probably due to the short follow-up, and any genuine survival difference may yet to show up with longer duration of follow-up.
Our conversion rate of 8.7% compared favorably with that in other series. To further reduce the conversion rate, patient selection would become an important issue. The use of a conversion model could prove to be an effective method to predict the risk of conversion. The Cleveland Clinic Foundation (CCF) laparoscopic conversion rate model, which incorporates both preoperative and intraoperative clinical parameters, was shown to have a high discriminatory power of patients with high risk of conversion [9]. Another conversion model developed by Schlachta et al. was also shown to be capable of stratifying patients into various risk groups [7]. However, a common pitfall of these conversion models is their wide applicability to both benign and malignant conditions. The design of a specific conversion model for colorectal cancers may prove to be a useful tool for patient selection. Another clinical measure that could improve the outcome of conversion is the adoption of a standardized operative strategy. A structured operative approach permits early recognition of risk for conversion, and could potentially eliminate inefficient surgical maneuvers, which could avoid unnecessary bowel handling and reduce the chance of cancer cell spillage. Recent studies showed that an acceptable conversion rate and postoperative outcome could be achieved when a standardized approach was adopted [15, 16].
Our study has several limitations. First, it was a nonrandomized study subject to selection bias. The decision for laparoscopic colectomy was made at the discretion of the surgeon based on experience. Second, our relatively small number of converted cases may not be sufficient to demonstrate all the significant differences in clinical outcomes between the two groups of patients. Furthermore, our study only compared the long-term outcome in patients with laparoscopic surgery and conversion but did not compare those who received open surgery for colorectal cancer. It is uncertain if the survival outcome in patients with conversion would be worse than those who had open colectomies. A further prospective trial comparing all three groups of treatments is needed to elucidate this issue.
Conclusion
Increased postoperative morbidity and prolonged hospital stay were the main adverse short-term outcomes associated with open conversion in laparoscopic resection of colorectal cancers. Although there was no difference in overall survival between patients who had conversion and those who had successful laparoscopic resection, patients in the former group had higher chance to develop local recurrence and had worsened disease-free survival. A cohort trial with longer duration of follow-up is needed to ascertain the prognostic influence of conversion.
References
Guillou PJ, Quirke P, Thorpe H et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365(9472):1718–1726
Veldkamp R, Kuhry E, Hop WC et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6(7):477–484
Moloo H, Mamazza J, Poulin EC et al (2004) Laparoscopic resections for colorectal cancer: does conversion survival? Surg Endosc 18(5):732–735
Bennett CL, Stryker SJ, Ferreira MR et al (1997) The learning curve for laparoscopic colorectal surgery. Preliminary results from a prospective analysis of 1194 laparoscopic-assisted colectomies. Arch Surg 132(1):41–44; discussion 45
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242(1):83–91
Gervaz P, Pikarsky A, Utech M et al (2001) Converted laparoscopic colorectal surgery. Surg Endosc 15(8):827–832
Schlachta CM, Mamazza J, Seshadri PA et al (2000) Predicting conversion to open surgery in laparoscopic colorectal resections. A simple clinical model. Surg Endosc 14(12):1114–1117
Gonzalez R, Smith CD, Mason E et al (2006) Consequences of conversion in laparoscopic colorectal surgery. Dis Colon Rectum 49(2):197–204
Tekkis PP, Senagore AJ, Delaney CP (2005) Conversion rates in laparoscopic colorectal surgery: a predictive model with, 1253 patients. Surg Endosc 19(1):47–54
Casillas S, Delaney CP, Senagore AJ et al (2004) Does conversion of a laparoscopic colectomy adversely affect patient outcome?. Dis Colon Rectum 47(10):1680–1685
Belizon A, Sardinha CT, Sher ME (2006) Converted laparoscopic colectomy: what are the consequences? Surg Endosc 20(6):947–951
Marusch F, Gastinger I, Schneider C et al (2001) Importance of conversion for results obtained with laparoscopic colorectal surgery. Dis Colon Rectum 44(2):207–214; discussion 214–6
Kiran RP, Delaney CP, Senagore AJ et al (2004) Operative blood loss and use of blood products after laparoscopic and conventional open colorectal operations. Arch Surg 139(1):39–42
Agachan F, Joo JS, Sher M et al (1997) Laparoscopic colorectal surgery. Do we get faster? Surg Endosc 11(4):331–335
Senagore AJ, Delaney CP, Brady KM, Fazio VW (2004) Standardized approach to laparoscopic right colectomy: outcomes in 70 consecutive cases. J Am Coll Surg 199(5):675–679
Senagore AJ, Duepree HJ, Delaney CP et al (2003) Results of a standardized technique and postoperative care plan for laparoscopic sigmoid colectomy: a 30-month experience. Dis Colon Rectum 46(4):503–509
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chan, A.C.Y., Poon, J.T.C., Fan, J.K.M. et al. Impact of conversion on the long-term outcome in laparoscopic resection of colorectal cancer. Surg Endosc 22, 2625–2630 (2008). https://doi.org/10.1007/s00464-008-9813-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-9813-3