Abstract
Background
Obesity is a common disease in the elderly population, and bariatric surgery is the most effective intervention to achieve significant and sustainable weight loss. Many bariatric programs have established an arbitrary cutoff at the age of 60 to 65 years. The aim of this study was to evaluate the safety and short-term outcomes of Roux-en-Y gastric bypass (RYGB) in patients older than 60 years.
Patients and Methods
We conducted a retrospective cohort study of patients who underwent RYGB from 2004 to 2019 in a single center. Logistic and linear multivariate regressions were made to compare complications and short-term outcomes between patients aged > 60 years and < 60 years. The statistical significance was set at p ≤ 0.05.
Results
From 849 patients who underwent a primary RYGB, 57 were > 60 years of age. Overall, early and late complications were similar in both groups, except for unexpected intensive care unit (ICU) admission which was more frequent in the > 60 years group. Excess body weight loss (%EWL) and percentage total weight loss (%TWL) at 1 year in patients > 60 years old were 76.6 ± 21.8% and 30.73 ± 6.8%, respectively. Figures for the same parameters in the control group were 81.7 ± 19.9% (p = 0.09) and 34.3 ± 7.2 (p = 0.001), respectively.
Conclusions
In our experience, an age > 60 is not related to higher rates of overall early and late complications after RYGB. Comorbidity remission rates are similar to those in younger patients. Elderly patients had lower total weight loss at 1 year, but the %EWL was similar in both groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is one of the leading causes of morbidity and mortality in the world. The prevalence of obesity in Mexico is high, affecting more than 30% of the adult population [1]. It has also been described that the Hispanic population has a higher risk for cardiovascular diseases, hypertension (HTN), and type 2 diabetes (T2D) [2]. Despite this, life expectancy has increased in Mexico, being 80.5 years for women and 77.9 years for men who have any type of health insurance and 77.65 and 73.73 years for women and men without health insurance, respectively [3]. The incidence of obesity has increased in the elderly Mexican population in the last years.
The role of bariatric surgery in the elderly is still under debate, and there is no consensus, nor specific recommendations for the management of obesity in this age group. Previous studies have shown that bariatric surgery in the older population is related to higher overall complications and mortality rates [4,5,6]. The Obesity Surgery Mortality Risk Score (OSM-RS) recognizes age > 45 years as one of the risk factors related to mortality [5]. In a retrospective study from the National Surgical Quality Improvement Program (NSQIP), an age > 65 years was related to higher overall and medical complications rates, as well as to higher mortality [7]. Due to these findings, many bariatric programs have established an arbitrary cutoff at 60 to 65 years to perform bariatric surgery. The Bariatric Surgery Center Network (BSCN) of the American College of Surgeons (ACS) recommends that bariatric surgery in patients > 60 years should be performed in high-volume or level I centers [8].
By contrast, several studies have shown acceptable overall complications and mortality rates in elderly patients, ranging from 13 to 14.7% and 0.05 to 0.7%, respectively [9,10,11].
The aims of this study were (1) to comparatively analyze the rate of short-term complications in patients with an age above and below 60 years who underwent Roux-en-Y gastric bypass (RYGB), (2) to comparatively evaluate the short-term weight loss in both groups, and (3) to analyze the impact of RYGB in the resolution of obesity-related comorbidities in patients above 60 years.
Patients and Methods
A retrospective analysis from a prospectively maintained database of 849 patients who underwent RYGB for morbid obesity at our institution from March 2004 to February 2019 was made. All bariatric procedures were performed after a complete multidisciplinary evaluation according to the national guidelines. The type of surgical procedure was selected based on the surgeon and patient preferences. Before surgery, all patients signed an informed consent for their operation and the de-identified data analysis. The study was approved by the institutional review board.
The patients were divided into two groups: patients 60 years or older and patients < 60 years of age. Preoperative recorded data included age, gender, weight, height, body mass index (BMI), body composition, and obesity-related comorbidities. Intraoperative data included operative time, estimated blood loss, and complications.
Body composition and bioelectrical impedance analysis (BIA) was assessed with the Total Body Composition Analyzer Model TBF-310 (Tanita Corporation of America Inc., Arlington Heights, IL).
Postoperative data included complications, total weight loss (TWL) in kg, percentage of total body weight loss (%TWL), percentage of the excess of body weight loss (%EWL), and remission of comorbidities.
Weight parameters were defined as follows [12]:
Remission of comorbidities was defined as follows [12]:
Type 2 Diabetes
Complete remission: Normal measures of glucose metabolism (Hb1Ac < 6% and fasting blood glucose (FBG) < 100 mg/dL) in the absence of antidiabetic medications.
Partial remission: Sub-diabetic hyperglycemia (Hb1Ac 6–6.4% and FBG 100–125 mg/dL) in the absence of antidiabetic medications.
Improvement: Significant reduction in HbA1c and FBG, without meeting the criteria for remission, OR decrease in antidiabetic medications (discontinuing insulin or at least one oral medication or half reduction in dose).
Unchanged: The absence of remission or improvement as previously described.
Hypertension
Complete remission: Blood pressure (BP) values corresponding to normotension (< 120/80 mmHg) in the absence of antihypertensive medication.
Improvement and/or partial remission: BP values corresponding to prehypertension (120–140/80–89) in the absence of antihypertensive medication OR decrease in dosage or number of antihypertensive medication OR decrease in systolic or diastolic BP on same medication dose.
Unchanged: The absence of remission or improvement as previously described.
Hyperlipidemia
Remission: Normal lipid panel in the absence of lipid lowering medications, as follows: LDL-cholesterol < 100 mg/dL, HDL-cholesterol ≥ 40 mg/dL or < 60 mg/dL, total cholesterol < 200 mg/dL, and triglycerides < 150 mg/dL.
Improvement: The decrease in number or dose of lipid lowering agents with equivalent control of dyslipidemia OR improved control of lipids on equivalent medication.
Complications
Complications were reported in 3 different ways: (1) early (< 30 days) and late (≥ 30 days); (2) minor and major, as recommended by Brethauer et al. [12], where major complications included those that resulted in a prolonged hospital stay (7 days), administration of anticoagulant, reoperation, or re-intervention, and minor, all other complications; and (3) according to the Clavien-Dindo classification of surgical complications [13].
Operative Technique
Roux-en-Y Gastric Bypass
Using 4 laparoscopic trocars and a Nathanson liver retractor, a gastric pouch close to 30 cc was created using a 32-Fr. gastric calibration tube in all cases. Limb lengths changed over time. In the first 790 patients (March 2004 to July 2017), the biliopancreatic (BP) limb had 50 cm in length and the alimentary limb 100 cm, whereas in the remaining 59 (July 2017 to February 2019), the BP limb was 100 cm and the alimentary limb 100 cm. A ~ 10 mm hand-sewn gastrojejunostomy was made in all cases, and both the mesenteric and Petersen spaces were closed with non-absorbable sutures.
Statistical Analysis
Statistical analysis was performed using the IBM® SPSS® Statistics software version 24.0 (IBM Corp., Armonk, NY, USA). Distribution shape, kurtosis, and skewness were reviewed in all included variables separately. Descriptive and inferential statistics were used based on the inherent scaling of the analyzed variables. Independent samples t test and Mann-Whitney U test were used for quantitative variables as a parametric and nonparametric test, respectively. Pearson’s chi-square test and Fisher’s exact test were used for categorical dichotomous variables, and Kendall’s tau-b was used for ordinal variables. Multivariate analysis was performed by means of binomial logistic and linear regression analysis for assessing the risk factors and the weight of interaction and confusing variables for early and late complications, as well as to determine the factors related to weight loss. Statistical significance was set at p ≤ 0.05 or 5% (alpha error) for a two-tailed hypothesis test.
Results
There were 496 (58.4%) women and 353 (41.6%) men. The group of patients > 60 years comprised 57 (6.7%) patients, whereas 792 (93.3%) were < 60 years. Mean baseline weight and fat free mass (FFM) were significantly lower in patients > 60 years of age. Regarding comorbidities, T2D, HTN, obstructive sleep apnea syndrome (OSAS), and decreased glomerular filtration rate (< 60 mL/min/1.73 m2) were significantly more frequent in the study group as shown in Table 1.
Early and late complications rates were similar for both groups, except for unexpected intensive care unit (ICU) admission (3.5% vs 0.4%, p = 0.039; OR = 9.5, CI 95% 1.53–58.4). In the group of patients > 60 years, two patients were admitted to the ICU, one was due to respiratory instability and lower limb swelling. Deep vein thrombosis, pulmonary thromboembolism, and/or acute heart failure were ruled out and the patient improved with conservative management. The second patient was a patient who presented a gastrojejunostomy leak. In the group of patients < 60 years, 3 patients were admitted to the ICU, one was due to intraperitoneal bleeding that required re-intervention, other due to intraluminal bleeding, and one because of an inadvertent small bowel perforation that required surgical re-intervention.
A comparison of the frequency of complications is shown in Table 2. In the group of > 60 years, in addition to the complications that required ICU, there was one patient who developed nosocomial pneumonia. In the group of patients < 60 years, one patient also developed nosocomial pneumonia, 4 patients presented a leak that required surgical re-intervention in 2, and 16 patients had gastrointestinal bleeding. In 13 patients, bleeding resolved spontaneously and 3 underwent surgical re-intervention.
No mortalities occurred in any group. There were no cases of deep venous thrombosis, porto-mesenteric thrombosis or pulmonary thromboembolism, and wound or urinary tract infections.
Using the multivariate binary logistic regression analysis, FFM, T2D, HTN, or the combination of T2D and HTN did not reach statistical significance for unexpected transfer to the ICU.
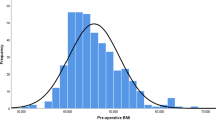
A complete 1-year follow-up was obtained in 586 (69%) patients, 47 (82.5%) from the > 60 years group and 539 (68%) from the < 60 years group. Late complications, including anastomotic stricture, marginal ulcer, small bowel obstruction, and anemia, during the first year after RYGB were similar for both groups. No malnutrition or severe hypoalbuminemia was reported. Weight parameters at 1 year are shown in Fig. 1. A sub-analysis of %TWL and %EWL according to the gender in patients of the study group showed no difference. For women, mean ± SD %TWL was 31.6% ± 6.9 and mean ± SD %EWL was 80.4% ± 24, whereas for men, these were 28.8% ± 6.3 (p = 0.2, Student’s t test) and 67.8% ± 11.9 (p = 0.02, Student’s t test), respectively.
Regarding body composition, patients > 60 years showed lower FFM at baseline. However, the decrease in the estimated FFM after RYGB was similar in both groups at 3, 6, and 12 months. On the other hand, patients < 60 years lost a higher proportion of body fat percentage (BF%) than patients > 60 years of age during follow-up (Fig. 2).
Multiple linear regression analysis was performed to assess variables related with weight loss at 12 months. Higher preoperative weight, BMI, and FFM were related to a higher WL (p < 0.0001), %TWL (p < 0.0001), and %EWL at 1 year (p < 0.0001). However, an age > 60 years and presence of T2D were not significantly related.
A comparison of comorbidity resolution rates at 1 year among groups is shown in Table 3. Remission of T2D, hyperlipidemia, and HTN was similar in both groups.
A sub-analysis of patients between 60 and 70 years and > 70 years was performed. Overall, early and late complication rates, remission of comorbid conditions, and weight loss were similar between groups at 1 year (Table 4).
Discussion
Bariatric surgery in patients aged ˃ 60 years represents nearly 10% of all bariatric procedures, and it has been growing over the past decade [10]. According to the national registers, there are more than 14 million people over the age of 60 in Mexico, and considering that more than 50% of the Mexican population over 50 years old is overweight and 28.7% has obesity, there are nearly four million elderly individuals with obesity, and a number of patients may be candidates for bariatric surgery [14]. In our series, 6.7% of the primary bariatric operations were performed on patients over 60 years of age.
In 2012, a national survey of health and nutrition (ENSANUT) showed that 40% of Mexican individuals aged 60 years or older have HTN, whereas 24.3% and 20.4% have T2D and hyperlipidemia, respectively [15]. Related to this, it has been reported that elderly patients have a risk two times higher to be hospitalized due to chronic diseases, comorbidities, and limited overall health condition when compared with the younger population [16]. Other studies have also shown higher rates of HTN (78.5–84%), T2D (49.5–58.9%), osteoarthritis (62.6%), GERD (52.3%), chronic obstructive pulmonary disease (23.4%), and chronic kidney disease (6.3%) in patients over 60 years who underwent bariatric surgery [10, 17]. Our results are consistent with these findings, as we found that in patients > 60 years of age, the frequencies of arterial HTN, T2D, and decreased GFR were 70%, 45%, and 16%, respectively, whereas for younger patients, these were 34%, 27%, and less than 1%, respectively. This could be related to the chronic nature of these diseases and obesity. However, the rate of another metabolic disease such as hyperlipidemia was similar for both groups.
A recent systematic review that analyzed the impact of bariatric surgery in patients over 60 years old showed a T2D remission rate of 54.5%, 42.5% for HTN, and 41.2% for hyperlipidemia, respectively [9]. Similar to this, a previous study showed that patients over 60 years old who underwent bariatric surgery had a greater reduction in the total amount of medications at 1 year compared with younger patients, including anti-reflux, lipid-lowering, cardiovascular, and T2D medications [18], showing the positive effect of bariatric surgery in this group of age. Our results are consistent with these findings. Complete remission of T2D, HTN, and hyperlipidemia 1 year after RYGB in patients > 60 years occurred in 64%, 64.5%, and 90% of patients, respectively. On the other hand, the reported remission rate of T2D in patients younger than 60 years undergoing bariatric surgery is around 70% [19,20,21], similar to our findings.
Most scores used for predicting T2D remission such as the ABCD [22] and DiaRem [23] include age as a prognostic factor for remission. Specifically, the DiaRem score considers an age above 60 years as one of the leading factors for non-remission (HR = 1.78) when compared with patients < 40 years of age [23]. Although we recognize that patients > 60 years may have longer duration of T2D with the consequent increase of pancreatic beta cell dysfunction, our results were different.
On the other hand, a relationship between age, surgical morbidity, and mortality has been suggested. Livingston et al. reported a mortality rate of 3.5% for patients over 55 years of age, whereas for younger patients, this was 1.1%. Half of the patients died due to medical-related complications [4]. In 2007, DeMaria et al. published the Obesity Surgery Mortality Risk Score (OSM-RS). In their original study, the mortality of patients over 45 years old who underwent RYGB was higher. However, no mortality was reported in patients aged > 65 years old [5]. It is important to highlight that many open bariatric procedures were included.
Based on the presumable high rate of complications, a longer hospital stay, and higher mortality, many centers have settled an arbitrary cutoff point of 60 to 70 years for bariatric surgery [10, 24]. However, this has been recently debated. A systematic review of bariatric surgery in elderly patients showed a mortality rate of 0.01% and a pooled overall complication rate of 14.7%, ranging from 1.33 to 47%, which is similar to the reported rates in younger patients [9]. Also, Parmar et al. found no difference regarding early and late complications in a study of 10 septuagenarians compared with 10 patients younger than 60 years [25].
According to our results, older patients did not show a higher risk for overall, early, and late complications. When we analyzed the indications to transfer to the ICU in the group of patients > 60 years, we can see that there was a leak of the gastrojejunostomy that required surgical re-exploration in one patient, and another patient was admitted for surveillance, in whom major complications were ruled out and the patient was discharged from the ICU in 24 h.
In our series, the remaining early and late complications had similar rates in patients > 60 years old and younger. In addition, no mortality occurred in any group. A large retrospective study of the National Surgical Quality Improvement Program (NSQIP) in the USA also showed that patients over 65 years old have similar rates of surgical-related complications than younger patients and a higher rate of medical complications [7]. In this study, medical complications in patients aged > 65 years and younger occurred in 6% and 4%.
In terms of weight loss, similar to previous reports [18, 26], our results showed that patients aged > 60 years had lower weight loss at 1 year. However, only two patients (4.3%) over 60 years old remained with a BMI above 35 kg/m2, and one patient (2.1%) did not reach an EWL > 50% at 1 year. Lower weight loss may be related to several factors, such as less physical activity, lower metabolic capacity, a different pattern of fat distribution, reduced lipolytic activity, and the presence of sarcopenia [9, 18, 27]. Contrary to this, a retrospective study of patients > 70 years showed no difference regarding TWL and EWL at 6, 12, and 24 months, in comparison with younger patients [25].
Despite a lower weight loss, in our series, there were no differences regarding the rates of remission of T2D, HTN, and hyperlipidemia between patients > 60 years and < 60 years of age, and FFM was similarly preserved in both groups. It was interesting to see that the %EWL at 1 year in patients aged > 60 years in our series was 76.63% which is higher than the 53.8% EWL reported in a previous systematic review [9]. Patients < 60 years showed a higher decrease in BF%. This may be related to the higher preoperative weight in this group. In a similar way, a previous study comparing patients with different ages found complete remission of T2D in 60% and of HTN in 50% in older patients, without significant differences between aged and younger patients [25].
Among the limitations in our study, we recognize its retrospective nature, a limited follow-up, a limited sample size of patients over 60 years old, a suboptimal methodology to asses body composition and bioelectrical impedance, and the fact that mean age in the study group was 64.4 ± 3.7 being all patients within the 60 to 70 years range. Other limitations were the difference in preoperative weight and the number of patients with super-obesity, which may affect weight loss parameters, as well as the %BF between groups.
Conclusions
RYGB is safe, yields effective weight loss, and achieves proper comorbidity remission rates at 1 year, in patients > 60 years. We consider that bariatric surgery should not be denied in this group of patients only because of age. Proper patient selection is crucial to avoid a higher rate of complications.
References
Palloni A, Beltrán-Sánchez H, Novak B, et al. Adult obesity, disease and longevity in Mexico. Salud Publica Mex. 2015;57(Suppl 1):S22–30.
Shaw PM, Chandra V, Escobar GA, et al. Controversies and evidence for cardiovascular disease in the diverse Hispanic population. J Vasc Surg. 2018;67(3):960–9.
Garcia de Alba-Garcia JE, Salcedo-Rocha AL, Milke-Najar ME. 2015 life tables of population user of Jalisco’s Instituto Mexicano del Seguro Social services. Rev Med Inst Mex Seguro Soc. 2018;56(3):261–72.
Livingston EH, Huerta S, Arthur D, et al. Male gender is a predictor of morbidity and age a predictor of mortality for patients undergoing gastric bypass surgery. Ann Surg. 2002;236(5):576–82.
DeMaria EJ, Portenier D, Wolfe L. Obesity surgery mortality risk score: proposal for a clinically useful score to predict mortality risk in patients undergoing gastric bypass. Surg Obes Relat Dis. 2007;3(2):134–40.
Haskins IN, Ju T, Whitlock AE, et al. Older age confers a higher risk of 30-day morbidity and mortality following laparoscopic bariatric surgery: an analysis of the metabolic and bariatric surgery quality improvement program. Obes Surg. 2018;28(9):2745–52.
Qin C, Luo B, Aggarwal A, et al. Advanced age as an independent predictor of perioperative risk after laparoscopic sleeve gastrectomy (LSG). Obes Surg. 2015;25(3):406–12.
Bariatric Surgery Center Network (BSCN) - ACS Division of Research and Optimal Patient Care. Accreditation Program Manual. 2010; Available from: https://www.cms.gov/Medicare/Coverage/DeterminationProcess/downloads/id160c.pdf
Victorzon M, Giordano S. Bariatric surgery in elderly patients: a systematic review. Clin Interv Aging. 2015;1627
Gebhart A, Young MT, Nguyen NT. Bariatric surgery in the elderly: 2009–2013. Surg Obes Relat Dis. 2015;11(2):393–8.
Robert M, Pasquer A, Espalieu P, et al. Gastric bypass for obesity in the elderly: is it as appropriate as for young and middle-aged populations? Obes Surg. 2014;24(10):1662–9.
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25(4):587–606.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications. Ann Surg. 2004;240(2):205–13.
Rivas-Marino G, Negin J, Salinas-Rodríguez A, et al. Prevalence of overweight and obesity in older Mexican adults and its association with physical activity and related factors: an analysis of the study on global ageing and adult health. Am J Hum Biol. 2015;27(3):326–33.
Manrique-Espinoza B, Salinas-Rodríguez A, Moreno-Tamayo KM, et al. Health conditions and functional status of older adults in Mexico. Salud Publica Mex. 2013;55(Suppl 2):S323–31.
González-González C, Sánchez-García S, Juárez-Cedillo T, et al. Health care utilization in the elderly Mexican population: expenditures and determinants. BMC Public Health. 2011;11(1):192.
Hassinger TE, Mehaffey JH, Johnston LE, et al. Roux-en-Y gastric bypass is safe in elderly patients: a propensity-score matched analysis. Surg Obes Relat Dis. 2018;14(8):1133–8.
Kaplan U, Penner S, Farrokhyar F, et al. Bariatric surgery in the elderly is associated with similar surgical risks and significant long-term health benefits. Obes Surg. 2018;28(8):2165–70.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366(17):1577–85.
Sjöström L, Peltonen M, Jacobson P, et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA. 2014;311(22):2297.
Pournaras DJ, Osborne A, Hawkins SC, et al. Remission of type 2 diabetes after gastric bypass and banding. Ann Surg. 2010;252(6):966–71.
Lee W-J, Hur KY, Lakadawala M, et al. Predicting success of metabolic surgery: age, body mass index, C-peptide, and duration score. Surg Obes Relat Dis. 2013;9(3):379–84.
Still CD, Wood GC, Benotti P, et al. Preoperative prediction of type 2 diabetes remission after Roux-en-Y gastric bypass surgery: a retrospective cohort study. Lancet Diabetes Endocrinol. 2014;2(1):38–45.
Varela JE, Wilson SE, Nguyen NT. Outcomes of bariatric surgery in the elderly. Am Surg. 2006;72(10):865–9.
Parmar C, Mahawar KK, Carr WRJ, et al. Bariatric surgery in septuagenarians: a comparison with <60 year olds. Obes Surg. 2017;27(12):3165–9.
Contreras JE, Santander C, Court I, et al. Correlation between age and weight loss after bariatric surgery. Obes Surg. 2013;23(8):1286–9.
Batsis JA, Villareal DT. Sarcopenic obesity in older adults: aetiology, epidemiology and treatment strategies. Nat Rev Endocrinol. 2018;14(9):513–37.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Statement
The institutional review board approved this study. This article does not contain any studies with human participants or animals performed by any of the authors.
Consent Statements
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ponce de León-Ballesteros, G., Sánchez-Aguilar, H.A., Velázquez-Fernández, D. et al. Roux-en-Y Gastric Bypass in Patients >60 Years of Age: Morbidity and Short-Term Outcomes. OBES SURG 30, 5033–5040 (2020). https://doi.org/10.1007/s11695-020-04957-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04957-8