Abstract
Objective
To evaluate whether the baseline Dietary Inflammatory Index (DII®) was associated with weight loss and body composition change after bariatric surgery.
Methodology
This longitudinal study included 132 women with obesity (BMI ≥ 35 kg/m2, 43.0 ± 9.7 years), followed up for 6 months after bariatric surgery. The DII® was calculated from dietary data collected using 24-h dietary recall interviews. Anthropometric variables, socio demographic variables, health-related habits, history of disease, as well as gastrointestinal symptoms, both in the preoperative period (baseline) and 6 months after bariatric surgery were collected from the patients’ medical records.
Results
Individuals with a more pro-inflammatory diet (DII > 0.35 median value) preoperatively experienced smaller weight loss (− 22.7% vs. − 25.3%, p = 0.02) and fat mass loss (− 31.9 vs. − 36.2%, p = 0.026), with no difference in lean mass (p = 0.14). In a linear regression model, the baseline DII score was negatively associated with percentage change in weight and fat mass and positively associated with weight and fat mass in the sixth month after surgery. In addition, a pro-inflammatory baseline DII score was correlated with a lower intake of fruit (r = − 0.26, p = 0.006), vegetables (r = − 0.47, p = 0.001), and legumes (r = − 0.21, p = 0.003) in the postoperative period.
Conclusion
In this longitudinal study, a pro-inflammatory diet at baseline was associated with smaller reductions in weight and body fat and poorer dietary quality (reduced consumption of fruits, vegetables, and legumes) 6 months after bariatric surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a chronic disease defined as excessive fat accumulation and is related to the development of various chronic diseases [1]. It is estimated that in the world, there are 641 million individuals with obesity, being 375 million women. [2]. Currently, bariatric surgery is the most effective treatment for reducing morbidity and mortality in patients with severe obesity [3]. Roux-en-Y gastric bypass (RYGB) is the most commonly used technique worldwide and is associated with a low rate of complications and mortality [4].
Preoperative predictors that may influence weight loss include baseline weight [including relative weight expressed as body mass index (BMI)], diabetes mellitus, advanced age, and a family history of obesity [5,6,7]. It is also well known that the individual’s dietary pattern is an important factor in the incidence of obesity and chronic diseases [8, 9], and it is known to be related to chronic subclinical inflammation [10,11,12,13]. In addition, specific dietary components may modulate the pro-inflammatory state associated with weight loss in people with obesity [10, 14].
The dietary inflammatory index (DII®), a validated instrument developed to characterize an individual’s diet according to its inflammatory properties [15], may be related to weight change after bariatric surgery. Higher DII scores, indicating a more pro-inflammatory diet, have been associated with greater weight gain/year, higher BMI, and greater risk of developing obesity [16, 17]. However, no study has e valuated whether the inflammatory potential of diet can influence weight loss and body composition after bariatric surgery.
The objective of this study was to evaluate whether baseline (i.e., preoperative) DII® predicts changes in body weight and fat 6 months after bariatric surgery.
Methodology
Study Population
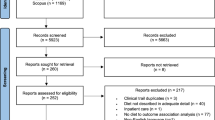
A total of 132 women with a BMI of ≥ 35 kg/m2 were enrolled into the present study. All participants underwent surgical treatment for obesity at the Hospital das Clínicas at the Universidade Federal de Minas Gerais, Medical School and treated by the Equipe de Terapia Nutricional da Obesidade Grave (ETNO). All participants attended the outpatient clinic from 2006 to 2015 and met these inclusion criteria: completion of data collection from the first consultation, completion of the consultation corresponding to 6 months after surgery, and reported daily caloric intake within pre-defined values (500–4000 kcal/day) to rule out gross under- or over-estimation. In addition, the 24-h recall was considered only when the ingestion corresponded to the patient’s routine habits.
The study was performed through an analysis of the medical records that was authorized by the ETNO runner, thus informed consent individual does not apply. The study was approved by the Research Ethics Committee of the Universidade Federal de Minas Gerais (UFMG) (No. 1.966.953/2017) and was therefore carried out in accordance with the ethical standards established in the Declaration of Helsinki (1964).
Food Consumption and DII Computation
The at pre and at post-operative diets were evaluated using a 24-h dietary recall (24HR) each time point, not necessarily restricting to the last 24HR intake. Computation of micronutrient, macronutrient, and total caloric intake was performed using Dietpro® software version 5.8, using the Brazilian food composition table [18] in combination with the USDA database [19], which was used to provide missing data.
The design and development of DII have been described previously [15]. Briefly, the DII was calculated using a scoring algorithm based on a review of 1943 articles that showed the association of 45 food parameters with six inflammatory biomarkers (IL-1b, IL-4, IL-6, IL-10, tumor necrosis factor-α, and C-reactive protein (CRP). Articles were positively marked (+ 1) if the effect was considered pro-inflammatory, negatively (− 1) in the case of an anti-inflammatory effect, or zero, if the parameters did not produce a significant change in the biomarkers to obtain literature-derived inflammatory effect score for each food parameter. The 24HR-derived food and nutrient consumption was first adjusted for total energy (i.e., per 1000 kcal) and then standardized to a globally representative energy-adjusted dietary database, which was constructed based on dietary intake from 11 populations living in different regions of the world. From this, the energy-adjusted standardized dietary intake (expressed as z scores of the referent database and then as centered proportions) was then multiplied by the literature-derived inflammatory effect score for each DII component. Individual scores were then summed to determine the overall E-DII score for each individual, with positive scores representing a more pro-inflammatory diet and negative values representing more anti-inflammatory diets.
In order to calculate the DII in this study, the following food parameters, obtained through analyzing the24HR were utilized: energy consumption, carbohydrate, protein, total fat, cholesterol, saturated fat, monounsaturated fat, polyunsaturated fat, omega 3, omega 6, niacin, vitamin A, vitamin C, vitamin D, vitamin E, iron, selenium, magnesium, zinc, beta carotene, and fiber.
Anthropometric Evaluation and Body Composition
The participant’s weight was measured on a platform-type scale with a capacity of 300 kg and the height was determined using a stadiometer attached to the scale (Filizola Electrónica 300 kg, São Paulo, Brazil), as previously described [20, 21]. BMI was calculated and the participants were classified by weight-status [22]. Weight loss was expressed as the change in BMI, as an addition, the percentage of excess weight loss was calculated by the formula % EWL = (initial weight − weight in the 6th month/initial weight − ideal weight) × 100. Percentage change was calculated by the formula % change = (post-surgery variable − pre-surgery variable/pre-surgery variable) × 100. Percentage change was calculated by the formula % change = (post-surgery variable − pre-surgery variable/pre-surgery variable) × 100.
Body composition was evaluated by means of bioelectrical impedance (BIA) (model Biodynamics 310e, brand TBW, São Paulo, Brazil), according to the protocol indicated by the manufacturer.
Other Variables
Data were collected from patients’ records on sociodemographic variables, health status and health-related behaviors (physical activity, use of medications, nutritional treatment prior to surgery, and use of medication for weight loss), supplements (multivitamin, vitamin B12 injections), and gastrointestinal symptoms (nausea, vomiting).
Statistical Analyses
Results from descriptive analysis are presented as mean (standard deviation), median (minimum-maximum), or percentage. The normality of the distribution was tested using the Shapiro-Wilk test. Comparative analyses were performed by paired t test and Student’s t test, and the Pearson correlation was computed for all continuous variables.
To evaluate the variables of interest according to the most pro and anti-inflammatory DII, the present study sample was categorized as most anti-inflammatory or most pro-inflammatory diet, according to the DII median (0.3 points). The use of a median cutoff point has been used previously [11, 23] as a way of creating risk groups in epidemiological studies [24].
In the final multiple linear regression model, the backward elimination method was used, with the least significant variables being removed from the model. The procedure was repeated until all of the variables present in the model reached statistical significance (p ≤ 0.20). All statistical analyses were conducted using SPSS® version 20.0, and the level of significance adopted for rejection of the null hypothesis was α = 0.05.
Results
Characteristics of study participants pre-operative and 6 months after bariatric surgery are shown in Table 1. Among the women evaluated in this study, 87.1% (n = 115) had already undergone some type of nutritional treatment before undergoing bariatric surgery, with 74.2% (n = 98) used medication for weight loss.
The participants lost, on average, 31.8 kg (± 12.6) and 12.2 kg/m2, corresponding to 44.6% (± 14.3) of the excess weight loss. Weight, BMI, fat, and lean mass 6 months after bariatric surgery were significantly lower in comparison to baseline values (p < 0.005, data not shown).
Regarding the baseline DII, the median was 0.35, with a minimum value of − 3.43 (more anti-inflammatory) and a maximum value of 4.08 (more pro-inflammatory). A more baseline pro-inflammatory diet was correlated with a lower intake of fruit (r = − 0.26, p = 0.006), vegetables (r = − 0.47, p < 0.001), and legumes (r = − 0.21, p = 0.003) in the postoperative period (Fig. 1).
Those individuals who consumed a more pro-inflammatory diet in the preoperative period had a lower percentage of change in weight (− 22.7% vs. − 25.3% p = 0.024) and fat mass (− 31.9% vs. − 36.2% p = 0.026) when compared to a more anti-inflammatory diet (Fig. 2).
In a linear regression model, the baseline DII and baseline weight were negatively associated with the percentage of weight change (F = 3.0, p = 0.02), explaining 8.6% of its variation (Table 2) as well as positively associated with postoperative weight (6-month follow-up) (F = 11.6, p < 0.001), explaining 7.8% of its variation (Table 3), independent of adjusting variables. The baseline DII was also negatively associated with legume intake, which was positively associated with the change in fat mass even after adjusting for age and postoperative caloric intake (F = 3.4, p = 0.01), explaining 9.7% of variation (Table 2). However, this model lost statistical significance when the baseline weight was included. Finally, baseline DII and baseline weight also were positively associated with postoperative fat mass (F = 8.4, p < 0.001), explaining 7.4% of variation (Table 3).
Discussion
To our knowledge, this paper provides the first evidence that a baseline pro-inflammatory diet may predict change in weight and body fat mass after bariatric surgery. However, previous studies have demonstrated the relationship between pro-inflammatory DII scores and obesity. In a multicenter cross-sectional study, the most pro-inflammatory DII was associated with higher BMI values in a cardio metabolic risk population [16]. In a cohort study, a pro-inflammatory diet was directly associated with the risk of being overweight and obese, in addition to promoting greater weight gain. Therefore, the authors suggest that diet-induced inflammation may contribute to maintaining or increasing obesity [17].
Weight [including relative weight expressed as body mass index (BMI)], presence of diabetes mellitus, age, and a family history of obesity are considered important predictors of weight loss after bariatric surgery [5,6,7]. However, previous studies do not describe how the baseline dietary pattern could be associated with post-surgical results. In fact, several dietary patterns have been directly related to metabolic improvement and reduction in adiposity [25,26,27]. Together, the results indicate the importance of the analysis of food patterns and nutritional monitoring from the preoperative phase of the patient people with obesity in order to identify food predictors for the postoperative period.
Another finding from our study was the relationship between the pro-inflammatory baseline diet with lower consumption of fruits, legumes, and vegetables in the postoperative period, indicating the importance of the pro-inflammatory characteristic of the diet 6 months after the surgery. Fruits, vegetables, and legumes have antioxidant, fiber, and protein components that are inversely related to oxidative stress and inflammation [23, 28, 29]. They also provide greater satiety and delayed gastric emptying [30, 31]. The consumption of legumes is associated with greater weight loss [32, 33].
The dietary pattern of people with obesity is characterized by the consumption of calorie-density and nutrient-sparse foods, all of which are known to be pro-inflammatory [12, 13]. As a corollary, their diets are characterized by low intake of legumes, vegetables, whole grains, fruits, fish, and a high intake of processed meat (e.g., sausages), sugar-sweetened drinks, processed foods, and saturated fat [34, 35]. Bariatric surgery patients also have lower intake of fruits, vegetables, and grains, despite improvement in diet quality after surgery [36, 37].
It is important to remember that after bariatric surgery, the food standards differ from those of the normal population. That is, the intake of 60 g of protein per day or 1.5 g of protein per kg of the ideal weight [38] is recommended, along with a caloric intake of 1000 to 1200 kcal/day [39], and supplementation of multivitamins and minerals is compulsory after surgery [40, 41]. In this context, the implementation of better eating habits should be continuously encouraged, beginning in the preoperative period, which optimizes the improvement in the quality of the most anti-inflammatory diet and, consequently, the expected clinical-nutritional results.
It is important to note that there was no difference in the percentage of change in lean mass in relation to the baseline DII. This result indicates that the ratio of DII to weight loss is related to loss of fat mass and not to lean mass. This point is important to note, because the loss of lean mass is associated with a reduction in the baseline metabolic rate, making weight loss and weight maintenance more difficult [42].
In addition to adiposity, the DII is associated with inflammatory markers. In a study conducted in Belgium, Shivappa et al. [43] found an association between pro-inflammatory DII and high concentrations of IL-6, homocysteine, and leukocytes. Furthermore, in the Seasonal Variation of Blood Cholesterol Study (SEASONS) in the USA, the pro-inflammatory DII was associated with higher concentrations of CRP [44]. As we can observe, diet and chronic subclinical inflammation characteristics of people with obesity are interconnected, forming a vicious cycle [8, 45]. Thus, having a baseline pro-inflammatory DII may be associated with maintaining dietary patterns with pro-inflammatory characteristics, potentiating sustained chronic subclinical inflammation and making it difficult to lose weight and fat mass after surgery.
In summary, this is the first study to show that the DII is a tool capable of evaluating the inflammatory potential of dietary patterns on the clinical-nutritional results in bariatric subjects. However, it does have its limitations, as the number of study participants does not allow for large statistical controls, but we know that there are several factors that are associated with changes in body composition. Despite previous training in the standardization of anthropometric measures and dietary assessment, the possibility of interpersonal variability should be considered. Specifically, the use of a single 24HR food recall represents more current data than usual [46], although this food questionnaire has been exhaustively used to study association between food intake, dietary indexes, and cardiometabolic risk factors [9, 14, 47].
Conclusion
In this longitudinal study, a pro-inflammatory diet in the preoperative period was associated with smaller weight and body fat loss and poor diet quality (reduced consumption of fruits, vegetables and legumes), 6 months after bariatric surgery. In addition, our results indicate the importance of diet quality, with emphasis on its inflammatory profile, as well as the importance of nutritional monitoring in the preoperative period.
References
Yamashita JM, de Moura-Grec PG, de Freitas AR, et al. Assessment of oral conditions and quality of life in morbid obese and normal weight individuals: a cross-sectional study. PLoS One. 2015;10(7):e0129687.
NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387(10026):1377–96.
Tirado R, Masdeu MJ, Vigil L, et al. Impact of bariatric surgery on heme oxygenase-1, inflammation, and insulin resistance in morbid obesity with obstructive sleep apnea. Obes Surg. 2017:1–9.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25(10):1822–32.
Fox B, Chen E, Suzo A et al. Dietary and psych predictors of weight loss after gastric bypass. J Surg Res 2015, 197(2), 283–290.
Al-Khyatt W, Ryall R, Leeder P, et al. Predictors of inadequate weight loss after laparoscopic gastric bypass for morbid obesity. Obes Surg. 2017;27(6):1446–52.
Steinbeisser M, McCracken J, Kharbutli B. Laparoscopic sleeve gastrectomy: preoperative weight loss and other factors as predictors of postoperative success. Obes Surg. 2017;27(6):1508–13.
Bressan J, Hermsdorff HH, Zulet MA, et al. Impacto hormonal e inflamatório de diferentes composições dietéticas: ênfase em padrões alimentares e fatores dietéticos específicos. Arq Bras Endocrinol Metabol. 2009;53(5):572–81.
Freire RH, Borges MC, Alvarez-Leite JI, et al. Food quality, physical activity, and nutritional follow-up as determinant of weight regain after Roux-en-Y gastric bypass. Nutrition. 2012;28(1):53–8.
Hermsdorff HHM, Zulet MÁ, Puchau B, et al. Fruit and vegetable consumption and proinflammatory gene expression from peripheral blood mononuclear cells in young adults: a translational study. Nutr Metab. 2010;7(1):42.
Hermsdorff HH, Mansego ML, Campion J, et al. TNF-alpha promoter methylation in peripheral white blood cells: relationship with circulating TNFα, truncal fat and n-6 PUFA intake in young women. Cytokine. 2013;64(1):265–71.
Kong LC, Holmes BA, Cotillard A, et al. Dietary patterns differently associate with inflammation and gut microbiota in overweight and obese subjects. PLoS One. 2014;9(10):e109434.
Mazidi M, Kengne AP. Nutrient patterns and their relationship with general and central obesity in US adults. Eur J Clin Investig. 2017;
Hermsdorff HHM, Zulet MÁ, Abete I, et al. Discriminated benefits of a Mediterranean dietary pattern within a hypocaloric diet program on plasma RBP4 concentrations and other inflammatory markers in obese subjects. Endocrine. 2009;36(3):445–51.
Shivappa N, Steck SE, Hurley TG, et al. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014;17(8):1689–96.
Ruiz-Canela M, Zazpe I, Shivappa N, et al. Dietary inflammatory index and anthropometric measures of obesity in a population sample at high cardiovascular risk from the PREDIMED (PREvencion con DIetaMEDiterranea) trial. Br J Nutr. 2015;113(6):984–95.
Ramallal R, Toledo E, Martínez JA, et al. Inflammatory potential of diet, weight gain, and incidence of overweight/obesity: the SUN cohort. Obesity. 2017;25(6):997–1005.
Lima DM et al. Tabela brasileira de composição de alimentos-TACO: versão IV. NEPA-UNICAMP: Campinas; 2011.
USDA United States Department of Agriculture. Food Composition Databases [Accessed on 20 May 2017]. Disponívelem: https://ndb.nal.usda.gov/ndb/.
Jelliffe, D. B., & World Health Organization. Evaluación del estado de nutrición de la comunidad (con especial referencia a las encuestas en las regiones en desarrollo). 1968.
World Health Organization. Physical status: The use of and interpretation of anthropometry, Report of a WHO Expert Committee. 1995.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation presented at the World Health Organization, June 3–5, 1997, Geneva, Switzerland. Geneva, Switzerland: WHO. 1997.
Carraro JCC, Hermsdorff HHM, Mansego ML, et al. Higher fruit intake is related to TNF-α hypomethylation and better glucose tolerance in healthy subjects. J Nutrigenet Nutrigenomics. 2016;9(2–4):95–105.
Willett WC. Nutritional epidemiology. 2nd ed. New York: Oxford University Press; 1998.
Hermsdorff HHM, Puchau B, Volp ACP, et al. Dietary total antioxidant capacity is inversely related to central adiposity as well as to metabolic and oxidative stress markers in healthy young adults. Nutr Metab. 2011;8(1):59.
García-Fernández E, Rico-Cabanas L, Rosgaard N, et al. Mediterranean diet and cardiodiabesity: a review. Nutrients. 2014;6(9):3474–500.
Soltani S, Shirani F, Chitsazi MJ, et al. The effect of dietary approaches to stop hypertension (DASH) diet on weight and body composition in adults: a systematic review and meta-analysis of randomized controlled clinical trials. Obes Rev. 2016;17(5):442–54.
Cocate PG, Natali AJ, de Oliveira A. Fruit and vegetable intake and related nutrients are associated with oxidative stress markers in middle-aged men. Nutrition. 2014;30(6):660–5.
Rocha DM, Lopes LL, da Silva A, et al. Orange juice modulates proinflammatory cytokines after high-fat saturated meal consumption. Food Funct. 2017;8:4396–403.
Venn BJ, Mann JI. Cereal grains, legumes and diabetes. Eur J Clin Nutr. 2004;58(11):1443–61.
Cavallo DN, Horino M, McCarthy WJ. Adult intake of minimally processed fruits and vegetables: associations with cardiometabolic disease risk factors. J Acad Nutr Diet. 2016;116(9):1387–94.
Hermsdorff HHM, Zulet MÁ, Abete I, et al. A legume-based hypocaloric diet reduces proinflammatory status and improves metabolic features in overweight/obese subjects. Eur J Nutr. 2011;50(1):61–9.
Kim SJ, de Souza RJ, Choo VL. Effects of dietary pulse consumption on body weight: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2016;103(5):1213–23.
Jastrzebska-Mierzynska M, Ostrowska L, Dadan J. Dietary habits of obese patients qualified for bariatric procedures. RocznikiPaństwowegoZakładuHigieny2014, 65(1).
Wirth J, di Giuseppe R, Boeing H, et al. A Mediterranean-style diet, its components and the risk of heart failure: a prospective population-based study in a non-Mediterranean country. Eur J Clin Nutr. 2016;70(9):1015–21.
Johnson LK, Andersen LF, Hofsø D, et al. Dietary changes in obese patients undergoing gastric bypass or lifestyle intervention: a clinical trial. Br J Nutr. 2013;110(1):127–34.
Soares FL, De Sousa LB, Corradi-Perini C, et al. Food quality in the late postoperative period of bariatric surgery: an evaluation using the bariatric food pyramid. Obes Surg. 2014;24(9):1481–6.
Heber D, Greenway FL, Kaplan LM, et al. Endocrine and nutritional management of the post-bariatric surgery patient: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(11):4823–43.
Flancbaum L, Choban PS, Bradley LR, et al. Changes in measured resting energy expenditure after Roux-en-Y gastric bypass for clinically severe obesity. Surgery. 1997;122(5):943–9.
Shankar P, Boylan M, Sriram K. Micronutrient deficiencies after bariatric surgery. Nutrition. 2010;26(11):1031–7.
Bordalo LA, Teixeira TFS, Bressan J, et al. Cirurgia bariátrica: como e por que suplementar. Rev Assoc Méd Bras. 2011;57(1):113–20.
Dagan SS, Tovim TB, Keidar A, et al. Inadequate protein intake after laparoscopic sleeve gastrectomy surgery is associated with a greater fat free mass loss. Surg Obes Relat Dis. 2017;13(1):101–9.
Shivappa N, Hébert JR, Rietzschel ER, et al. Associations between dietary inflammatory index and inflammatory markers in the Asklepios study. Br J Nutr. 2015;113(4):665–71.
Shivappa N, Steck SE, Hurley TG, et al. A population-based dietary inflammatory index predicts levels of C-reactive protein in the seasonal variation of blood cholesterol study (SEASONS). Public Health Nutr. 2014;17(8):1825–33.
Hermsdorff HHM, Zulet MÁ, Puchau B, et al. Central adiposity rather than total adiposity measurements are specifically involved in the inflammatory status from healthy young adults. Inflammation. 2011;34(3):161–70.
Hébert JR, Hurley TG, Steck SE, et al. Considering the value of dietary assessment data in informing nutrition-related health policy. Adv Nutr. 2014;5(4):447–55.
Shivappa N, Steck SE, Hussey JR, et al. Inflammatory potential of diet and all-cause, cardiovascular, and cancer mortality in National Health and Nutrition Examination Survey III Study. Eur J Nutr. 2017;56(2):683–92.
Acknowledgments
We thank the participants of this study and the Equipe de Terapia Nutricional da Obesidade Grave (ETNO) of the Hospital das Clínicas – UFMG for excellent technical assistance. HHM Hermsdorff and JIA Leite are CNPq Research Productivity Fellows.
Funding
PA Andrade was provided Master’s grant from CAPES (MEC/Brazil), and this study received financial support from the FAPEMIG (State of Minas-Gerais, Brazil). Drs. Shivappa and Hébert were supported by grant number R44DK103377 from the United States National Institute of Diabetes and Digestive and Kidney Diseases.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Declaration
JRH owns controlling interest in Connecting Health Innovations LLC (CHI), a company planning to license the right to his invention of the dietary inflammatory index (DII) from the University of South Carolina in order to develop computer and smart phone applications for patient counseling and dietary intervention in clinical settings. NS is an employee of CHI. The subject matter of this paper will not have any direct bearing on that work, nor has that activity exerted any influence on this project.
Conflict of Interest
The authors declared no conflict of interest. However, we do wish to disclose that Dr. James R. Hébert owns controlling interest in Connecting Health Innovations LLC (CHI), a company planning to license the right to his invention of the dietary inflammatory index (DII) from the University of South Carolina in order to develop computer and smart phone applications for patient counseling and dietary intervention in clinical settings. Dr. Nitin Shivappa is an employee of CHI.
Rights and permissions
About this article
Cite this article
Andrade, P.A., Hermsdorff, H.H.M., Leite, J.I.A. et al. Baseline Pro-inflammatory Diet Is Inversely Associated with Change in Weight and Body Fat 6 Months Following-up to Bariatric Surgery. OBES SURG 29, 457–463 (2019). https://doi.org/10.1007/s11695-018-3530-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3530-3