Abstract
Gastrojejunostomy anastomotic strictures are a complication of Roux-en-Y gastric bypass surgery without an established treatment guideline. A systematic review and meta-analysis were performed to determine the safety and efficacy of endoscopic dilation in their management. PubMed, Web of Science, and Cochrane Central (1994–2017) were searched. Data was analyzed with random effects meta-analysis and mixed effects meta-regression. Twenty-one observational studies (896 patients) were included. The stricture rate for laparoscopic patients was 6% (95% CI, 5–9%). Only 38% (95% CI, 30–47%) required greater than one dilation. Symptom improvement occurred in 97% (95% CI, 94–98%). The complication rate was 4% (95% CI, 3–6%). Endoscopic dilation of GJA strictures is safe, effective, and sustaining. This study can guide endoscopists in the treatment of a common bariatric surgical complication.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Roux-en-Y (RNY) gastric bypass is a common bariatric procedure during which a surgeon aims to create an anastomosis that is a tight seal, but free of tension, with an adequate blood supply, and a luminal restriction that supports weight loss. Despite this intent, gastrojejunostomy anastomotic (GJA) strictures are a common complication in the early postoperative period. RNY gastric bypass patients suffer from symptoms and incur direct and indirect costs for medical care related to GJA strictures. There is no reported safe and effective management strategy identified. To date, there is only one meta-analysis describing endoscopic dilation of RNY GJA strictures [1]. Systematic review and meta-analysis were performed to understand the safety and effectiveness of endoscopic dilation in treating bariatric RNY gastric bypass patients with GJA strictures.
Methods
The present study was conducted according to the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions [2] and the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) reporting guidelines for observational studies [3].
Selection Criteria
Participants
Studies with patients who met institutional qualification for bariatric surgery, underwent RNY gastric bypass, were symptomatic (i.e., nausea, vomiting, oral intolerance, abdominal pain, and dysphagia) and diagnosed with GJA strictures by upper endoscopy were included. Laparoscopic RNY surgeries were targeted by selecting studies between 1994 and 2017; however, studies that included open technique were not excluded.
Endoscopic Intervention
Studies with detailed descriptions of endoscopic dilation of GJA strictures, including diameter of dilation, number of dilation sessions, timing of diagnosis or intervention, and the type of dilator used were included. Both Savary-Gilliard and balloon dilation were accepted; however, combinations of interventions were excluded.
Outcomes
Studies that addressed patient symptomatic improvement after dilation as well as those that needed surgical revision for either complications of dilation or for failure of improvement were included. Studies were not excluded based on follow-up period.
Study Design
Randomized controlled trials, cohort studies, and case-control studies were included, but meeting abstracts, case reports, editorials, and reviews were excluded.
Database Search
Database searches targeting articles that addressed the clinical question were performed using PubMed, Web of Science, and Cochrane Central during July and August 2017. The PubMed search phrase used was “Gastric Bypass”[Mesh] OR “Anastomosis, Roux-en-Y”[Mesh] OR “gastric bypass”[Text Word] OR Roux-en-Y[Text Word] OR Anastomosis[Text Word]) AND (“Constriction, Pathologic”[Mesh] OR stenosis[Text Word] OR stricture[Text Word]) AND (“Dilatation”[Mesh] OR “Endoscopy, Gastrointestinal”[Mesh] OR dilation[Text Word] OR dilatation[Text Word] OR endoscopic[Text Word] OR endoscopy[Text Word]) with limits English language, 1994–present, and Adult 19 +. The Web of Science search phrase used was (“gastric bypass” OR Roux-en-Y OR Anastomosis) and (stenosis OR stricture) and (dilation OR dilatation OR endoscopic OR endoscopy) with limits 1994–2017. The Cochrane Central search used Mesh and text words listed above and publication year 1994–2017 (Supplementary Material A). Citations were saved in a citation management software (EndNote) and duplicates were removed.
Selection Process
Two authors (A.B. and A.A. or D.E.) independently reviewed all collected titles/abstracts and decided yes/no/uncertain regarding relevance to the study. All investigators then met to resolve differences and determine final selection of abstracts for full-text retrieval. Two authors (A.B. and A.A. or D.E. or R.H.) then independently reviewed the selected full-text articles and decided yes/no/uncertain. Authors again met to resolve differences and identify the final set of articles for inclusion and data retrieval. Following final article selection, clinical trial registries (metaRegister of Controlled Trials, ClinicalTrials.gov, Australian Clinical Trials Registry, UK Clinical Trials, and WHO Portal) were searched, and citation lists of six key studies used and three relevant review articles were reviewed for possibly missed articles of relevance (i.e., snowballing).
Assessment of Study Quality
The quality of all studies was assessed by two authors (A.B. and D.E.) using the Newcastle-Ottawa Scale (NOS) for Cohort Studies [4].
Data Extraction
Four authors (A.B., R.H., M.F., and A.C.) independently extracted and input data into a standardized Excel data sheet containing the following: (1) patient characteristics: demographics (age, sex, and BMI), number of laparoscopic and open RNY patients with and without anastomotic strictures, number of patients with anastomotic ulcers, and description of stenosis; (2) intervention characteristics: timing of diagnosis/intervention, type of dilator used, use of fluoroscopy or steroids, diameters of dilator used on first session and during the total treatment period, number of dilation sessions, and time between dilation sessions; and (3) outcomes: symptom improvement, surgical revision, complications of dilation, duration of follow-up, and percentage of excess weight loss (% EWL) or change in BMI for stricture and non-stricture patients.
Data Missing
Data was collected in its reported form and converted to the most common unit whenever possible. Data that could not be attained or converted was imputed for analysis. A descriptive summary or weighted estimates of the remaining available data was made. Data was retrieved only from articles; authors of studies were not contacted to confirm or obtain data.
Statistical Analysis
All analysis was conducted with R statistical software [5], including the meta [6] and metafor packages [7]. Missing observations were imputed using the mice R package [8].
Descriptive statistics for number of: female and male patients; mean: age, BMI, and timing of diagnosis/intervention; minimum and maximum: dilator diameter on first endoscopy, dilator diameter during total treatment period, time between dilation sessions, and duration of follow-up; and maximum: number of dilation sessions were summarized using weighted means, standard errors, and range (minimum, maximum).
Meta-analysis and meta-regression were implemented by fitting random effects and mixed effects regression models to account for both within and between study variations. The restricted maximum likelihood, inverse variance, and Clopper-Pearson confidence interval methods were used. Test statistics for estimating heterogeneity included the τ2, I2, H2, and R2. Chi-square test (p value < 0.05) and a test of significance of coefficients was conducted to test for the significance of the residual heterogeneity. Both the logit transformed proportions, with continuity correction of 0.5 for studies with zero cell frequencies, and the Freeman-Tukey double arcsine transformed proportions of the outcome were compared [9]. Results were reported as odds ratios and their 95% confidence intervals.
Publication bias and sensitivity analysis were conducted using the rank correlation test and the regression test for funnel plot asymmetry [10, 11].
Results
Study Characteristics
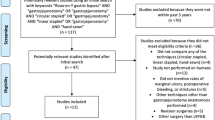
The initial electronic search retrieved 2452 articles after duplicates were removed, which were screened by title and abstract (Fig. 1). Of those, 59 were selected for full-article review. Upon final review, 21 articles met inclusion criteria and were chosen for data extraction and analysis [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32]. The gray literature search and snowballing revealed no additional relevant studies. No randomized controlled trials were identified. Over 50% of studies had an NOS score of ≥ 6 (Supplementary Material B).
Patient Characteristics
Results were pooled for 896 stricture patients (635 laparoscopic, 62 open, and 201 unreported) with available data summarized in Table 1. A weighted summary of the observed data available revealed a weighted mean of mean age 41.37 ± 2.28 (range 38.40–46.00; n = 566) and mean BMI 47.30 ± 3.20 (range 43.79–55.20; n = 485). Studies tended to have a higher number of female stricture patients with a weighted mean number of females 39.80 ± 17.90 (range 11.00–71.00 patients; n = 559) compared to a weighted mean number of males 25.40 ± 27.10 (range 1.00–75.00 patients; n = 559). The remaining studies did not separate demographic data for stricture and non-stricture patients. All patients were symptomatic, but five studies also used imaging in evaluation prior to endoscopy [16, 17, 23,24,25]. Eight studies mentioned stricture diameters (data not shown), but the majority reported that the diameter was less than 10 mm or that the scope was unable to pass (8.5–10 mm endoscope) [16,17,18, 24, 26, 27, 29, 32]. Not all studies reported the number of laparoscopic versus open RNY patients with anastomotic strictures, but for the data available (n = 578), there was an anastomotic stricture rate for laparoscopic patients of 6% (95% CI, 5–9%; I2 = 92%; p < 0.01; Fig. 2a).
Intervention
The weighted mean for mean timing of diagnosis or intervention of the observed data available was 67.06 ± 54.82 days after surgery (range 30.00–539.00; n = 802). The minimum and maximum timing reported in any study was 3.00 and 4921.00 days after surgery. Only 51 of 896 patients received the Savary-Gilliard dilation while the clear majority received the through-the-scope (TTS) balloon dilation [28]. Only one study (26 patients) used steroid injections to supplement dilation [17], and three studies (106 patients) dilated under fluoroscopy [17, 26, 28]. The weighted mean minimum and maximum diameter of the dilator used on the first endoscopy was 9.45 ± 2.62 mm (range 6.00–15.00; n = 396) and 16.39 ± 2.57 mm (range 10.00–20.00; n = 372) respectively. The weighted mean minimum and maximum diameter of the dilator used during the total treatment period was 9.37 ± 2.33 mm (range 6.00–15.00; n = 590) and 17.71 ± 2.63 mm (range 12.00–25.00; n = 630) respectively. The weighted mean minimum and maximum weeks between endoscopic dilations was 1.64 ± 1.18 mm (range 0.40–7.00; n = 245) and 6.04 ± 6.58 mm (range 2.00–25.00; n = 245) respectively. The weighted mean maximum sessions of dilation for the observed data available was 4.43 ± 1.20 sessions (range 3.00–7.00; n = 787).
Only 38% (95% CI, 30–47%; I2 = 81%; p < 0.01; Fig. 3a) of patients required greater than one dilation session during their treatment period. BMI (OR, 0.86; 95% CI, 0.77–0.97; p = 0.01), minimum dilator diameter on first endoscopy (MiDF) (OR, 0.79; 95% CI, 0.70–0.89; p < 0.001), and during the total treatment period (MiDT) (OR, 0.85; 95% CI, 0.76–0.95; p = 0.01) negatively predicted the need for repeat dilation. After adjusting for multiple variables, MiDF was still predictive of outcome. (OR, 0.86; 95% CI, 0.75–0.98; p = 0.03; Fig. 3b).
a Forest plot describing the rate of patients requiring greater than one endoscopic dilation session during the total treatment period (proportion 0.38; 95% CI, 0.30–0.47). b Bubble chart showing the relationship between the proportion of patients requiring greater than one endoscopic dilation and the minimum dilator diameter (mm) used on the first endoscopy. Sizes of circles are proportional to the study cohort size. A solid regression line is plotted with dotted lines indicating the 95% CI (OR, 0.86; 95% CI, 0.75–0.98; p = 0.03)
Outcomes
The weighted mean for mean duration of follow-up of the observed data available was 25.29 ± 7.31 months (range 14.40–37.00; n = 188). The minimum and maximum follow-up duration reported in any study was 0.90 and 146.00 months. Meta-analysis showed that 97% (95% CI, 94–98%; I2 = 67%; p < 0.01; Fig. 4a) of patients’ symptoms responded safely to endoscopic dilation compared to 3% (95% CI, 2–6%; I2 = 67%; p < 0.01; Fig. 4c) that failed to respond (n = 15) or suffered a complication (n = 8) and required surgery. For symptom improvement, maximum dilator diameter on the first endoscopy (MxDF) was a strong positive predictor (OR, 1.45; 95% CI, 1.21–1.70; p < 0.001) while MiDT was a strong negative predictor (OR, 0.78; 95% CI, 0.63–0.97; p = 0.02). However, after adjusting for multiple variables in meta-regression, only MxDF was a strong predictor (OR, 1.36; 95% CI, 1.11–1.70; p = 0.004; Fig. 4b). The same predictors, in opposing direction, were true for requirement of surgical revision (MxDF: OR, 0.69; 95% CI, 0.57–0.83; p < 0.001; MiDT: OR, 1.28; 95% CI, 1.04–1.59; p = 0.02) with MxDF as a strong predictor after adjusting for multiple variables (OR, 0.74; 95% CI, 0.60–0.90; p = 0.004).
a Forest plot describing the high rate of symptom improvement with endoscopic dilation (proportion 0.97; 95% CI, 0.94–0.98). b Bubble chart showing the relationship between the proportion of patients with symptom improvement and the maximum dilator diameter (mm) on the first endoscopy. Sizes of circles are proportional to the study cohort size. A solid regression line is plotted with dotted lines indicating the 95% CI (OR, 1.36; 95% CI, 1.11–1.70; p = 0.004). c Forest plot describing the low rate of surgery after endoscopic dilation (proportion 0.03; 95% CI, 0.02–0.06)
There was an overall low-complication rate (4%; 95% CI, 3–6%; I2 = 7.1%; p = 0.86; Fig. 5a). There were 21 (91%) patients with perforation, one with hemorrhage, and one with a subepithelial hematoma. Eight patients underwent surgery for perforations; however, three of these patients did not require revision. The remaining complications were managed conservatively. There was no strong predictor of complication using logit transformation; however, MiDF trended toward significance (OR, 0.86; 95% CI 0.74–1.00; p = 0.05). On the other hand, using Freeman-Tukey transformation, MiDF was a strong negative predictor of complication (OR, 0.99; 95% CI 0.98–1.00; p = 0.04; Fig. 5b). There was an anastomotic ulcer rate in all stricture patients of 6% (95% CI, 3–12%; I2 = 70%; p < 0.01; Fig. 2b). Presence of an anastomotic ulcer at the time of diagnosis of anastomotic stricture did not predict complications during endoscopic dilation.
a Forest plot showing the low-complication rate of endoscopic dilation (proportion 0.04; 95% CI, 0.03–0.06). b Bubble chart showing the relationship between the proportion of patients with complication and the minimum dilator diameter (mm) on first endoscopy. Sizes of circles are proportional to the study cohort size. A solid regression line is plotted with dotted lines indicating the 95% CI (OR, 0.86; 95% CI 0.74–1.00; p = 0.05)
Six studies reported that the percentage of % EWL was not different between stricture and non-stricture patients within their studies [16, 19, 26,27,28, 30]; however, there was not enough pooled data for analysis.
Sensitivity Analysis
Sensitivity analysis detected potential bias with asymmetry (p < 0.05) in the funnel plots for ulcer rate and the outcomes of symptom improvement or surgery after dilation. Stricture rate, patient need for greater than one dilation session, and complication rate showed no bias with the absence of significant asymmetry in the funnel plots (Supplementary Material C).
Discussion
Based on the current available literature, endoscopic dilation of GJA strictures is safe and effective with low-complication rates and high rates of symptom improvement after one dilation. Endoscopic dilation response is maintained long-term as GJA stricture patients are followed on average for 2 years.
Laparoscopic procedures are predominant in this review due to the defined selection criteria; thus, comparisons between laparoscopic and open procedures were not made. The overall reported stricture rate in laparoscopic patients is low with the absence of a publication bias. By design, all stricture patients included were symptomatic. Diagnosis of GJA strictures and endoscopic intervention occurs early, on average 2 months after surgery, when RNY patients transition from soft to solid food. Anastomotic strictures can be classified as membranous due to extended fasting; cicatricial from chronic inflammation related to foreign body material, ulceration, and anastomotic leak; and granular from ischemic tissue necrosis related to anastomotic tension, smoking, marginal ulceration, and lack of apposition [33, 34]. Membranous strictures respond well to endoscopic dilation [33, 34]. This is likely the most common stricture type with over 60% of patients responding to one dilation session.
TTS balloon dilation is far more common than wire-guided bougie dilation as it allows for direct targeting of the surgical anastomotic stricture. Larger dilator diameter selection promotes positive outcomes. Early response to endoscopic therapy is predicted by a larger MiDF without publication bias. Likewise, a larger MxDF promotes overall symptom improvement and lessens the need for surgery. It is safe to choose a 2–6-week interval between dilations.
The overall complication rate is low (4%) without publication bias, and most complications are conservatively managed with few requiring surgical revision. Although the rate is low, 91% of complications are perforations. This rate is higher than the perforation rate seen in esophageal dilations for eosinophilic esophagitis (< 1%) [35, 36]. The complication rate found in this meta-analysis is more comparable to that associated with dilation of Crohn’s disease strictures (4% complication rate and 3% perforation rate), in which 65% of patients had anastomotic strictures [37]. Thus, anastomotic strictures may carry higher risk of perforation than intrinsic strictures.
Complication, interestingly not predicted by an associated ulcer, is predicted by smaller MiDF. The reason is likely related to the small size of the stricture itself. As a stricture becomes smaller in diameter, the squared area decreases dramatically. Thus, when dilating a small stricture incrementally there is higher risk with each increment compared to when dilating a larger stricture. For instance, a 5-mm diameter stricture (78.50 mm2) dilated to 7 mm (153.86 mm2) is a 96% increase in the squared area; whereas, a 9-mm diameter stricture (254.34 mm2) dilated to 11 mm (379.94 mm2) is only a 33% increase in the square area. Although larger dilator diameters on the first endoscopy promote symptom improvement and lessen the need for repeat sessions, when facing a small GJA stricture, the endoscopist should begin with the smallest dilator and use extra caution with each incremental increase as this is the time at the highest risk of perforation.
Despite that the main objective of bariatric surgery is weight loss, there was only six comparative (one matched) studies reporting % EWL, but at various follow-up intervals. In the future, researchers should pay attention to % EWL in stricture and non-stricture patients and how it is affected by endoscopic dilation.
There are several limitations to this systematic review and meta-analysis that reflect the restrictions of the included studies. First, all the studies included are observational cohort studies. Significant heterogeneity (p < 0.05) was present in meta-analysis, except for complication rate, indicating that multiple effect sizes are likely present, potentially due to variability in populations, interventions, and reporting parameters of the studies. Random effects and mixed effects regression models were fitted to account for both within and between study variations given the observational nature of the studies. Data was imputed when not available in the meta-regression analysis. Lastly, sensitivity analysis showed potential for publication bias for ulcer rate and outcomes of symptom improvement or surgery after dilation, but not for stricture rate, complication rate, and patients receiving only one endoscopic dilation. Reporting parameters for the former data varied between studies, and therefore data extraction may over or underestimate incidence or treatment effects.
The strengths of this systematic review and meta-analysis are the large number of included studies, its detailed data extraction, the rating of the quality of the cohort studies, and statistical methods used to account for heterogeneity and bias in the studies. No other systematic review and meta-analysis currently exists that provides a comprehensive guide on endoscopic treatment of GJA strictures.
Conclusion
Endoscopic dilation of GJA strictures, typically occurring in the early post-operative period, is safe and effective with most patients responding to one dilation session. Strictures should be objectively measured before each dilation. With small strictures, the smallest dilator diameter should be selected and incrementally increased with caution. Dilations may be safely repeated every 2–6 weeks based on symptom resolution. Objective stricture measurement can also aid in evaluating the need for adjunctive therapy, such as steroid injection, in refractory strictures when following patients prospectively. If a complication, like perforation, occurs, it can generally be managed conservatively. Further studies are needed to standardize the approach to assessment, treatment, and follow-up of GJA strictures. This systematic review and meta-analysis provides a guide to endoscopists in treatment of a common bariatric surgical complication.
References
Campos JM, Mello FS, Ferraz AA, et al. Endoscopic dilation of gastrojejunal anastomosis after gastric bypass. Arq Bras Cir Dig. 2012;25(4):283–9.
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration. Wiley Online Library; 2008. Available from: http://www.cochrane.org/handbook.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
Wells G, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale for assessing the quality of nonrandomized studies. 2014. Accessed April 22, 2018. Available from: www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
R Core Team. A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2018.
Schwarzer G. Meta: an R package for meta-analysis. R News. 2007;7(3):40–5.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3):1–48. Available from: http://www.jstatsoft.org/v36/i03
van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2010;45(3):1–67.
Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Stat. 1950;21:607–11.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Ahmad J, Martin J, Ikramuddin S, et al. Endoscopic balloon dilation of gastroenteric anastomotic stricture after laparoscopic gastric bypass. Endoscopy. 2003;35(9):725–8.
Alasfar F, Sabnis AA, Liu RC, et al. Stricture rate after laparoscopic roux-en-Y gastric bypass with a 21-mm circular stapler: the Cleveland Clinic experience. Med Princ Pract. 2009;18(5):364–7.
Barba CA, Butensky MS, Lorenzo M, et al. Endoscopic dilation of gastroesophageal anastomosis stricture after gastric bypass. Surg Endosc. 2003;17(3):416–20.
Caro L, Sanchez C, Rodriguez P, et al. Endoscopic balloon dilation of anastomotic strictures occurring after laparoscopic gastric bypass for morbid obesity. Dig Dis. 2008;26(4):314–7.
Carrodeguas L, Szomstein S, Zundel N, et al. Gastrojejunal anastomotic strictures following laparoscopic Roux-en-Y gastric bypass surgery: analysis of 1291 patients. Surg Obes Relat Dis. 2006;2(2):92–7.
Catalano MF, Chua TY, Rudic G. Endoscopic balloon dilation of stomal stenosis following gastric bypass. Obes Surg. 2007;17(3):298–303.
Da Costa M, Mata A, Espinos J, et al. Endoscopic dilation of gastrojejunal anastomotic strictures after laparoscopic gastric bypass. Predictors of initial failure. Obes Surg. 2011;21(1):36–41.
Dolce CJ, Dunnican WJ, Kushnir L, et al. Gastrojejunal strictures after Roux-en-Y gastric bypass with a 21-mm circular stapler. JSLS. 2009;13(3):306–11.
Espinel J, De-la-Cruz JL, Pinedo E, et al. Stenosis in laparoscopic gastric bypass: management by endoscopic dilation without fluoroscopic guidance. Rev Esp Engerm Dig. 2011;103(10):508–10.
Frutos MD, Lujan J, Garcia A, et al. Gastrojejunal anastomotic stenosis in laparoscopic gastric bypass with a circular stapler (21 mm): incidence, treatment and long-term follow-up. Obes Surg. 2009;19(12):1631–5.
Go MR, Muscarella 2nd P, Needleman BJ, et al. Endoscopic management of stomal stenosis after Roux-en-Y gastric bypass. Surg Endosc. 2004;18(1):56–9.
Huang CS, Forse RA, Jacobson BC, et al. Endoscopic findings and their clinical correlations in patients with symptoms after gastric bypass surgery. Gastrointest Endosc. 2003;58(6):859–66.
Lee JK, Van Dam J, Morton JM, et al. Endoscopy is accurate, safe, and effective in the assessment and management of complications following gastric bypass surgery. Am J Gastroenterol. 2009;104(3):575–82.
Mathew A, Veliuona MA, DePalma FJ, et al. Gastrojejunal stricture after gastric bypass and efficacy of endoscopic intervention. Dig Dis Sci. 2009;54(9):1971–8.
Nguyen NT, Stevens CM, Wolfe BM. Incidence and outcome of anastomotic stricture after laparoscopic gastric bypass. J Gastrointest Surg. 2003;7(8):997–1003.
Peifer KJ, Shiels AJ, Azar R, et al. Successful endoscopic management of gastrojejunal anastomotic strictures after Roux-en-Y gastric bypass. Gastrointest Endosc. 2007;66(2):248–52.
Ribeiro-Parenti L, Arapis K, Chosidow D, et al. Gastrojejunostomy stricture rate: comparison between antecolic and retrocolic laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2015;11(5):1076–84.
Rondan A, Nijhawan S, Majid S, et al. Low anastomotic stricture rate after Roux-en-Y gastric bypass using a 21-mm circular stapling device. Obes Surg. 2012;22(9):1491–5.
Ryskina KL, Miller KM, Aisenberg J, et al. Routine management of stricture after gastric bypass and predictors of subsequent weight loss. Surg Endosc. 2010;24(3):554–60.
Schwartz ML, Drew RL, Roiger RW, et al. Stenosis of the gastroenterostomy after laparoscopic gastric bypass. Obes Surg. 2004;14(4):484–91.
Ukleja A, Afonso BB, Pimentel R, et al. Outcome of endoscopic balloon dilation of strictures after laparoscopic gastric bypass. Surg Endosc. 2008;22(8):1746–50.
Yimcharoen P, Heneghan H, Chand B, et al. Successful management of gastrojejunal strictures after gastric bypass: is timing important? Surg Obes Relat Dis. 2012;8(2):151–7.
Kataoka M, Masaoka A, Hayashi S, et al. Problems associated with the EEA stapling technique for esophagojejunostomy after total gastrectomy. Ann Surg. 1989;209(1):99–104.
Moole H, Jacob K, Duvvuri A, et al. Role of endoscopic esophageal dilation in managing eosinophilic esophagitis: a systematic review and meta-analysis. Medicine. 2017;96(14):e5877.
Dougherty M, Runge TM, Eluri S, et al. Esophageal dilation with either bougie or balloon technique as a treatment for eosinophilic esophagitis: a systematic review and meta-analysis. Gastrointest Endosc. 2017;86(4):581–91.
Navaneethan U, Lourdusamy V, Njei B, et al. Endoscopic balloon dilation in the management of strictures in Crohn’s disease: a systematic review and meta-analysis of non-randomized trials. Surg Endosc. 2016;30(12):5434–43.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Statement
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent Statement
For this type of study formal consent is not required.
Electronic supplementary material
ESM 1
(DOCX 431562 kb)
Rights and permissions
About this article
Cite this article
Baumann, A.J., Mramba, L.K., Hawkins, R.B. et al. Endoscopic Dilation of Bariatric RNY Anastomotic Strictures: a Systematic Review and Meta-analysis. OBES SURG 28, 4053–4063 (2018). https://doi.org/10.1007/s11695-018-3491-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3491-6