Abstract
Obesity is a global epidemic and will soon become the number one priority in healthcare management. Bariatric surgery causes a significant improvement in obesity and its related complications. Pre-operative esophago-gastro-duodenoscopy (EGD) is done by several bariatric surgical teams across the world but is still not mandatory.
Aim
To study the percentage of symptomatic and asymptomatic pathological EGD findings in obese patients undergoing bariatric surgery and to analyze whether these findings influence the eventual choice of bariatric surgery.
Materials and Methods
All patients posted for bariatric surgery at our institute from January 2015 to March 2017 had a pre-operative EGD done by the same team of endoscopists.
Results
In this study, totally, 675 patients were assessed prior to routine bariatric surgery. 78.52% of all pre-operative patients had an abnormal EGD. The most common endoscopic abnormalities found were hiatus hernia (52.44%), gastritis (46.22%), presence of Helicobacter (H.) pylori (46.67%), reflux esophagitis (16.89%), Barrett’s esophagus (1.78%), gastric erosions (13.19%), and polyps (7.41%). Fifty patients had upper gastrointestinal polyps: 41 in the stomach, 3 in the esophagus, and 6 in the duodenum, mostly benign hyperplastic or inflammatory polyps. Two patients had gastrointestinal stromal tumor (GIST), 6 leiomyoma, and 6 neuroendocrine tumors (NET). Of those with endoscopic evidence of gastroesophageal reflux disease (GERD), 70 (60.03%) of patients were asymptomatic. The pre-operative EGD findings resulted in a change of the planned surgical procedure in 67 (9.93%) patients.
Conclusion
Our study suggests that a large percentage of patients undergoing bariatric surgery have pathologically significant endoscopic findings of which a significant number are asymptomatic; this can lead to a change in the planned bariatric procedure in a section of patients; hence, we believe that EGD should be made mandatory as a pre-operative investigation in all bariatric surgery patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a major health problem worldwide and has reached epidemic proportions. It is a complex chronic disease which results in increased morbidity and mortality including GERD and esophageal motility disorders [1, 2].
Treating morbid obesity is difficult and despite losing weight initially, majority of patients face the long-term challenge of maintaining weight loss [3]. Therapies currently accepted for treating obesity include dietary modification, physical exercise, pharmacological or endoscopic treatment, and finally bariatric surgical therapy.
There is an ingrained relationship between the endoscopist and bariatric surgery. The endoscopist’s role lies not only in pre- and post-operative management but also in the primary treatment of obesity. It is our surmise that an esophago-gastro-duodenoscopy (EGD) be done as part of the pre-operative workup. Conditions such as GERD, hiatus hernia, reflux esophagitis, Barrett’s esophagus, H. pylori infection, ulcers, polyps, gastric outlet obstruction, NETs, GIST, and Dieulafoy’s lesions can greatly influence the type of bariatric surgery and resultant long-term outcomes [4]. For example, if severe reflux disease or hiatus hernia is detected, sleeve gastrectomy (SG) maybe contraindicated [4]. Exclusion of the remnant stomach in a gastric bypass makes surveillance EGD difficult if not impossible, and this can pose a dilemma in countries endemic for gastric cancer [4].
Aim
The aim of this study was to determine the percentage of symptomatic and asymptomatic pathological EGD findings in obese patients undergoing bariatric surgery and to analyze whether these findings influence the eventual choice of bariatric surgery. We also compared the presence of gastroesophageal reflux disease (GERD) and H. pylori positivity in our obese patient population with that seen in non-obese patients from literature.
Materials and Methods
All patients posted for routine bariatric surgery between January 2015 and March 2017 underwent EGD as part of their pre-operative workup. Written informed consent was obtained from all patients. Approval from the hospital ethics committee was taken. The study included 675 patients who presented to our hospital for bariatric surgery. The patients’ demographics, body mass index (BMI), and co morbidities were recorded. History of symptoms suggestive of GERD such as reflux, acidity, or pre-operative use of medication such as antacids, proton pump inhibitors, or motility drugs was evaluated.
EGD was performed by the same team of endoscopists to maintain uniformity in result reporting.
Literature and community-based data was used from non-obese patients for comparison of GERD incidence and H. pylori presence.
The diagnosis of esophagitis was based on the criteria described in the Los Angeles Classification [5].
Los Angeles Classification (Table 1)
The gastroesophageal junction was assessed using a retroflexed view with gastric inflation. The gastroesophageal sphincter incompetency (GSI) was graded from I to IV according to the Hill classification [6].
Hill Classification (Fig. 1)
The presence of hyperemia and edema were considered as evidence of endoscopic gastritis or duodenitis.
The presence or absence of H. pylori was investigated systematically by biopsy of a mucosal sample from the antrum and subjecting it to a rapid urease test (RUT).
Any polyps, nodules, or tumors were biopsied or excised and sent for histopathology.
A retrospective analysis of data based on a prospectively loaded database was performed.
Results
Totally, 675 patients were assessed in this study. Majority of patients (75%) were between 30 and 60 years with mean 45 ± 9.09 (30–60) and 73% had a BMI between 30 and 60 with mean 43.94 ± 6.9 (30.02–59.77).
The remainder of patients 15% < 30 years of age with mean 21.93 ± 4.59 (14–29) and 10% > 60 years of age with mean 69.42 ± 7.26 (61–84). Also 3.5% had BMI < 30 with mean 28 ± 1.55 (25.6–29.8) and 23.5% had BMI > 60 with mean 66.64 ± 7.10 (60.21–89.31).
Three hundred eighty-three (56.74%) of the patients were female and 292 (43.26%) were male.
Two hundred seventy (40%) were hypertensive, 217 (32.15%) were diabetic, and 141 (20.89%) had dyslipidemia.
Two hundred thirty-four (34.67%) of the patients had pre-operative symptoms of GERD of which 149 (63.67%) were on medications for the same.
For those with reflux esophagitis on endoscopy 73 (64.03%) patients were asymptomatic.
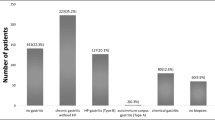
Five hundred thirty (78.52%) of all pre-operative patients had an abnormal EGD (Fig. 1, abnormal EGD findings). 354/675 (52.44%) of patients had a hiatus hernia on EGD according to the Hill Classification.
114/675 (16.89%) of patients had endoscopic findings suggestive of reflux esophagitis according to the LA Classification.
12/675 (1.78%) had pre-operative biopsy proven Barrett’s esophagus.
312/675 (46.22%) of the patients had gastritis and 89/675 (13.19%) had gastric erosions. 23/675 (3.4%) had duodenitis with 6/675 (0.8%) having duodenal ulcers.
Totally, 315/675 (46.67%) were H. pylori positive.
50/675 patients had upper gastrointestinal polyps: 41 in the stomach, 3 in the esophagus, and 6 in the duodenum. Most of these were benign hyperplastic polyps. Two patients had GIST, 6 had leiomyoma, and 6 had neuroendocrine tumors (NET).
73/114 (64.03%) of those with reflux esophagitis were asymptomatic pre-operatively. 40/56 (71.43%) of patients with Grade A esophagitis, 17/33 (51.52%) with Grade B esophagitis, and 16/25 (64%) with Grade C were asymptomatic.
Totally, 67/675 (9.93%) had their surgical management altered because of their pre-operative EGD findings.
Four hundred eleven (60.89%) underwent a Roux-en-Y gastric bypass (RYGB), 9 (1.33%) underwent a banded RYGB (BRYGB) with remnant gastrectomy, 163 (24.15%) LSG, 26 (3.85%) LSG with duodenojenunal bypass (DJB), and 66 (9.78%) single anastomosis gastric bypass (SAGB).
Five of the 12 patients in our study having Barrett’s esophagus on EGD who were supposed to have a LSG had their surgical plan altered to a RYGB. Fifty-one patients had their surgery plan changed from a LSG to RYGB due to severe esophagitis or hiatus hernia while in 11 patients the surgical plan was altered to include a remnant Gastrectomy with a RYGB or a LSG to include excision of the GIST or NET.
Six had their surgery canceled as they were not willing to undergo the procedure offered by us.
Discussion
The role of EGD in the pre-operative assessment of bariatric patients is controversial as there is no uniformity amongst surgeons on its cost effectiveness and utility.
Multiple published studies have demonstrated that routine EGD before surgery can identify a variety of conditions including hiatal hernia, esophagitis, ulcers, and tumors [7, 8]. In our study, 530 (78.52%) of all pre-operative patients had an abnormal EGD.
Corroborating data in the literature shows that the most frequent endoscopic findings are gastritis, hiatal hernia, esophagitis, and gastroduodenal ulcers [9, 10].
Comparison of findings in literature and findings in this study (Table 2).
GERD
Obesity itself is a risk factor for GERD, which is present in 30 to 60% of patients undergoing bariatric surgery [15]. In a study by Bhumika et al., 55.5% of patients with GERD were obese. They thus concluded that an increasing BMI has a statistically significant relationship with increased occurrence of GERD [16]. Another meta-analysis by Nilsson et al. indicated that obesity was associated with a significant 1.5–2 fold increase in the risk of GERD symptoms and erosive esophagitis [17].
In our study, 234/675 (34.67%) of patients had symptoms of GERD pre-operatively. Of these, 149/234 (63.67%) were on histamine type 2 receptor blockers or other antacids.
73/114 (64.03%) of those with reflux esophagitis on EGD were asymptomatic pre-operatively; what was noteworthy was that 16/25 (64%) of those with Grade C oesophagitis were asymptomatic. Majority of patients with abnormalities in all previous studies were asymptomatic as well [7, 8].
Barrett’s Esophagus
In a meta-analysis of 19 studies, including 5802 patients, the prevalence of Barrett’s esophagus was found in 2.1% [18] which was similar to the 1.78% of patients in our study.
These findings take on significance now that LSG has become the most commonly performed procedure world over.
Prager et al. performed a study following up patients undergoing LSG with pH manometry, EGD, and questionnaires; they found 45.5% with de novo hiatal hernias and an increase in Barrett’s esophagus from 0 (pre-operatively) to 14% on follow-up. Thus, they concluded that LSG should be considered a relative contraindication in patients with pre-operative hiatus hernia, GERD, and Barrett’s esophagus [19].
In a study by Genco et al., 17.2% patients were found on follow-up endoscopy post-LSG to have newly diagnosed non-dysplastic Barrett’s esophagus [20]. Therefore, concluding that in patients with pre-op Barrett’s esophagus, LSG should not be done [21]. Patients with Barrett’s esophagus need to be screened for the progression to high-grade dysplasia and later possibly adenocarcinoma. Regression of Barrett’s esophagus following a gastric bypass has been reported in literature [22].
We believe the pre-operative detection of hiatus hernia with flap valve grading and endoscopic evidence of reflux esophagitis plays an important role in deciding the type of surgery to be performed. In our center, all patients with a Hill classification of 3 to 4 and/or a Grade C or D esophagitis according to the LA Classification or those with Barrett’s esophagus were posted for a RYGB instead of either an SAGB or a LSG. RYGB is known to reduce both acid and bile reflux. Therefore, in our study, five of the 12 patients having Barrett’s esophagus on EGD who were supposed to have a LSG had their surgical plan altered to a RYGB, the rest were already posted for a RYGB so no alteration in surgery decision was required. Fifty-one patients had their surgery plan changed from a LSG to RYGB due to severe esophagitis or hiatus hernia on pre-op EGD.
Worldwide endoscopic findings resulted in an alteration of the surgical approach or delay in surgery for 1 to 9% of patients [23].
The effects of bariatric interventions on GERD appear to be variable. Roux-en-Y gastric bypass (RYGB) has been shown in multiple series to reduce GERD symptoms at rates that approach or exceed 90% [24]. Reflux symptoms may be worsened in patients who have undergone LSG [25]. RYGB is hence considered a better operative choice for patients with significant pre-operative diagnosis of GERD. Dupree et al. found that most patients undergoing RYGB have a resolution or improvement in symptoms of GERD [26].
Gastritis
In a study by Rasmussen et al., 47.92% of patients had gastritis, and Kakar et al. reported a rate of 25.4%; in our study, 312/675 (46.22%) of the patients had gastritis and 89/675 (13.19%) had gastric erosions. 23/675 (3.4%) had duodenitis with 6/675 (0.8%) having duodenal ulcers. Gomez et al. were the only ones to report much lower rates of gastritis 9.1%.
H. pylori
In Rasmussen’s study, H. pylori was present in 54.44% of patients who had stomach ulcers [22].
In a study by Adlekha et al. from Kerela in India, the prevalence of H. pylori was found to be as high as 62% [27].
A meta-analysis published by James et al. in 2017 studied prevalence of H. pylori all over the world published in multiple studies and found the prevalence in India to be as high as 50–60% [28]. In our study, we found 315/675 (46.67%) patients were H. pylori positive and were treated pre-operatively as well as put on surveillance in the post-op period for marginal ulcers in case the patient had a RYGB/SAGB .
H. pylori can be a predisposing factor for gastric cancer, hence its early detection and treatment is of paramount importance [29]. In countries endemic for stomach carcinoma like Korea and Japan, the post-operative diagnosis and surveillance of H. pylori-related ulcer disease, gastritis, and carcinoma becomes much more difficult as the gastric remnant is no longer easily accessible to EGD after RYGB/SAGB [30].
A higher prevalence of H. pylori has been reported in those with obesity being observed in 23 to 70% of bariatric patient as shown in studies by Rosenthal et al. and Mohanty et al [31, 32]. It has been incriminated as an important cause of marginal ulceration [33] thereby underlining the importance of detection and treatment of H. pylori to prevent complications post-bariatric surgery.
In our study, 50 (7.41%) patients had polyps, which were biopsied. Most of these were either inflammatory polyps or benign hyperplastic polyps.
14/675 patients had asymptomatic tumors in the stomach or duodenum.
On histopathology, six patients were found to have neuroendocrine tumors (NET) Grade 1/2. Three of these NETs were found in the stomach and three in the first part of the duodenum. All these patients were then investigated further with serum chromogranin and serum metanephrine levels and PET scans to determine the presence of absence of tumors elsewhere. Patients with stomach NET had a RYGB with remnant gastrectomy as the surgical procedure of choice or LSG. The duodenal NETs were either completely excised endoscopically prior to surgery or the patients underwent a RYGB with remnant gastrectomy and removal of the 1st part of duodenum (D1 removal). Two patients who were diagnosed as GIST had a RYGB with remnant gastrectomy or a fundectomy with a RYGB depending on location of tumor. Six patients had a leiomyoma and underwent either a LSG excising the area of the stomach having the tumor or a RYGB with fundectomy.
In patients undergoing RYGB or SAGB, it becomes difficult to view the remnant stomach at a later stage; hence, if diagnosis of a pre-malignant condition, is made it is imperative to either remove the tumor prior to surgery or that portion of the stomach or duodenum along with the bariatric procedure to avoid difficult in surveillance of the tumor at a later stage.
Schirmer et al. studied 560 patients who underwent RYGB; 26 patients (4.9%) had endoscopic findings that changed or altered the operative procedure. However, no surgeries were cancelled [34] In our study, six had their surgery cancelled as they were not willing to undergo the procedure offered by us.
According to the American Society for Metabolic and Bariatric Surgery (ASMBS) guidelines published in 2008, clinically significant gastrointestinal symptoms should be evaluated before bariatric surgery with imaging studies, upper gastrointestinal series, or endoscopy, and routine screening for the presence of Helicobacter pylori before bariatric surgery may be considered in high-prevalence areas (Fig. 2) [35].
In 2015, the Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy (ASGE) in conjunction with the ASMBS prepared a document describing the role of endoscopy in bariatric surgery [36]. This document suggested that the decision to perform a pre-operative endoscopy should be individualized depending on the type of bariatric surgery planned (Fig. 3).
Evidence-based guidelines presented at the 12th International Congress of the European Association for Endoscopic Surgery (E.A.E.S.) in Barcelona, Spain, recommended pre-operative endoscopy to be included as a routine in pre-operative workup in patients considering a bariatric surgery after a consensus panel discussion [37].
Conclusion
On the basis of our study, where 78.52% of all patients had a pathologically relevant EGD with GERD, hiatal hernia, H. pylori, and gastritis being the most common findings of this study, we believe that EGD should be made mandatory as a pre-operative investigation in all bariatric patients. It helps not only in the diagnosis of asymptomatic upper gastrointestinal pathology but also in diagnosing conditions like NET, GIST, and Barrett’s esophagus that may result in change of the planned surgical procedure in nearly 10% of the patients. A pre-operative EGD can go a long way in choosing the right procedure for the patient and preventing a lot of post-operative morbidity.
References
Guh DP, Zhang W, Bansback N, et al. The incidence of co-morbidities related to obesity and over-weight: a systematic review and meta-analysis. BMC Public Health. 2009;25:88.
Muñoz R, Ibáñez L, Salinas J, et al. Importance of routine pre-operative upper GI endoscopy: why all patients should be evaluated? Obes Surg. 2009;19:427–31.
Wadden TA, Frey DL. A multicenter evaluation of a proprietary weight loss program for the treatment of marked obesity: a five-year follow-up. International Journal of Eating Disorders. 22(2):203–12.
Rosenthal RJ. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases. Surg Obesity Rel Dis. 2012;8:8–19.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles Classification. Gut. 1999;45:172–80.
Hill AD, Kozarek RA, Kraemer SJM, et al. The gastroesophageal flap valve: in vitro and in vivo observations. Gastrointest Endosc. 1996;44:541–7.
Korenkov M, Sauerland S, Shah S, et al. Is routine preoperative upper endoscopy in gastric banding patients really necessary? Obes Surg. 2006;16:45–7.
Zeni TM, Frantzides CT, Mahr C, et al. Value of preoperative upper endoscopy in patients undergoing laparoscopic gastric bypass. Obes Surg. 2006;16:142–6.
Anderson MA, Gan SI, Fanelli RD, et al. ASGE guideline: role of endoscopy in the bariatric surgery patient. Gastrointest Endosc. 2008;68:1–10.
Sharaf RN, Weinshel EH, Bini EJ, et al. Endoscopy plays an important preoperative role in bariatric surgery. Obes Surg. 2004; Nov-Dec;14(10):1367–72.
Kakar K, Singhal V, Khaitan L. Preoperative upper endoscopy should be standard of care for patients undergoing bariatric surgery. SAGES 2014
Victoria Gomez MD, Rajat Bhalla MD, et al. Routine screening endoscopy before bariatric surgery: is it necessary? Bariatric Surgery Practice Patient Care. 2014;9(4):143–9.
Rodriguez Diez, Maria D. et al. Upper endoscopy findings in obese morbid patients candidates for bariatric surgery. Gastroenterol Hepatol 2015; 38(7): 426–430.
Bennett S et al. The role of routine preoperative upper endoscopy in bariatric sx: a systematic review and meta analysis. Surg Obes Relat Dis. 2016;12(5):1116–23.
Di Francesco V, Baggio E, Mastromauro M, et al. Obesity and gastro- esophageal acid reflux: physiopathological mechanisms and role of gastric bariatric surgery. Obes Surg. 2004;14:1095–102.
Bhumika V, Arvind B, Pragati M, et al. Gastroesophageal Reflux disease and its association with BMI: Clinical and Endoscopic Study. J Clin Diagn Res. 2017;11(4):OC01–4.
El-Serag H. The association between obesity and GERD : a review of the epidemiological evidence. Dig Dis Sci. 2008 Sep;53(9):2307–12.
Bennett S, Gostimir M, Shorr R, et al. The role of routine preoperative upper endoscopy in bariatric surgery : a systematic review and meta-analysis. Surg Obes Relat Dis. 2016;12(5):1116–25.
Felsenreich D, Kefurt R, Schermann M, et al. Reflux, sleeve dilation, and Barrett’s esophagus after laparoscopic sleeve gastrectomy: long-term follow-up. Obes Surg. 2017; https://doi.org/10.1007/s11695-017-2748-9.
Genco A, Soricelli E, Casella G, et al. Gastroesophageal reflux disease and Barrett’s esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication. Surg Obes Relat Dis. 2017;13:568–74.
Cobey F, Oelschlager B. Complete regression of Barrett’s esophagus after Roux-en-Y gastric bypass. Obes Surg. 2005;15(5):710–2.
Rasmussen JJ, Fuller W, Ali MR. Marginal ulceration after laparoscopic gastric bypass: an analysis of predisposing factors in 260 patients. Surg Endosc. 2007;21(7):1090–4.
Loewen M, Giovanni J, Barba C. Screening endoscopy before bariatric surgery: a series of 448 patients. Surg Obes Relat Dis. 2008;4:709–12.
Foster A, Richards WO, McDowell J, et al. Gastrointestinal symptoms are more intense in morbidly obese patients. Surg Endosc. 2003;17:1766–8.
Howard DD, Caban AM, Cendan JC, et al. Gastroesophageal reflux after sleeve gastrectomy in morbidly obese patients. Surg Obes Relat Dis. 2011;7:709–13.
DuPree CE, Blair K, et al. Laparoscopic sleeve gastrectomy in patients with preexisting gastroesophageal reflux disease, a national analysis. JAMA Surgery. 2014;149(4):328–34.
Adlekha C et al. Prevalence of H. Pylori infection among patients undergoing upper gastrointestinal endoscopy in a Medical College Hospital in Kerela, India. Ann Med Health Sci Res. 2013;3(4):559–63.
Hooi KY, Wong WS, Kaplan GG, et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology. 2017;153(2):420–9.
Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection—the Maastricht IV/ Florence Consensus. Gut. 2012;61:646–64.
Papasavas PK, Gagne DJ, Donnelly PE, et al. Prevalence of Helicobacter pylori infection and value of preoperative testing and treatment in patients undergoing laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2008;4(3):383–8.
Erim T, Cruz-Correa MR, Szomstein S, et al. Prevalence of Helicobacter pylori seropositivity among patients undergoing bariatric surgery: a preliminary study. World J Surg. 2008;32:2021–5.
Verma S, Sharma D, Kanwar P, et al. Prevalence of helicobacter pylori infection in bariatric patients: a histologic assessment. Surg Obes Relat Dis. 2013;9:679–85.
Schirmer B, Erenoglu C, Miller A. Flexible endoscopy in the management of patients undergoing Roux-en-Y gastric bypass. Obes Surg. 2002;12:634–8.
Sharaf RN, Weinshel EH, Bini EJ, et al. Endoscopy plays an important preoperative role in bariatric surgery. Obes Surg. 2004;14:1367–72.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient – 2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic and Bariatric Surgery. Obesity. 2013;21:S1–S27.
ASGE Standards of Practice Committee. The role of endoscopy in the bariatric surgery patient. Surg Endosc. 2015 May;29(5):1007–17.
Sauerland S, Angrisani L, Belachew M, et al. Obesity surgery. Evidence-based guidelines of the European Association for Endoscopic Surgery (E.A.E.S.). Surg Endosc. 2005;19:200–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflict of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human and Animal Rights
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
D’Silva, M., Bhasker, A.G., Kantharia, N.S. et al. High-Percentage Pathological Findings in Obese Patients Suggest that Esophago-gastro-duodenoscopy Should Be Made Mandatory Prior to Bariatric Surgery. OBES SURG 28, 2753–2759 (2018). https://doi.org/10.1007/s11695-018-3230-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3230-z