Abstract
Background
Marginal ulceration after Roux-en-Y gastric bypass (RYGB) is diagnosed in 1% to 16% of patients. The factors predisposing patients to marginal ulceration are still unclear.
Methods
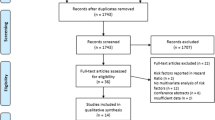
A total of 260 patients who underwent laparoscopic RYGB were retrospectively reviewed. Data regarding demographics, comorbidities, body mass index (BMI), Helicobacter pylori infection, gastrojejunal (GJ) anastomotic leaks, postoperative bleeding, operative time, type of suture material, and marginal ulcer formation were collected. Fisher’s exact test was used for statistical analysis of discrete variables, and Student’s t-test was used for continuous variables. Statistical significance was set at an alpha of 0.05.
Results
The overall marginal ulceration rate was 7%. Demographic data (age, gender distribution, BMI) did not differ significantly between patients who experienced marginal ulceration and those who did not (p > 0.05). Similarly, technical factors (choice of permanent or absorbable suture for the GJ anastomosis, attending as primary surgeon, robotic GJ, operative time, postoperative hematocrit drop) were not statistically different between the two groups (p > 0.05). Finally, the prevalence of comorbidities (diabetes, hypertension, obstructive sleep apnea, musculoskeletal complaints, dyslipidemia, gastroesophageal reflux disease [GERD] and peptic ulcer disease [PUD]) did not differ significantly between the two groups (p > 0.05). However, preoperative H. pylori infection, although adequately treated, was twice as common among the patients who had marginal ulceration (32%) as among those who did not (12%) (p = 0.02). All the patients who experienced marginal ulcers had complete resolution of symptoms with proton pump inhibitors and sucralfate. No reoperations were required for marginal ulceration.
Conclusion
Helicobacter pylori may potentiate marginal ulcer formation. The authors hypothesize that H. pylori damages the mucosal barrier in a way that persists postoperatively, which may precipitate marginal ulceration even when the organism has been medically eradicated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obesity is an epidemic on the rise in the United States and the world [28, 38, 39]. Currently, the most effective means of weight loss and long-term weight loss maintenance is bariatric surgery [19, 25, 37]. In the United States, Roux-en-Y gastric bypass (RYGB) is the most commonly performed bariatric operation [1, 11, 32]. Whether open or laparoscopic, RYGB has been associated with excellent surgical outcomes and low complication rates [1].
Marginal ulceration remains a morbid complication of RYGB, occurring in 1% to 16% of patients [9, 17, 30, 31]. Although the mechanisms underlying the development of marginal ulceration have not been completely elucidated, the etiology of this complication is likely to be multifactorial. We set out to identify patient or technique-specific factors that may predispose to marginal ulcer formation after laparoscopic RYGB.
Materials and methods
Between January 2004 and July 2005, 260 patients underwent laparoscopic RYGB at the University of California, Davis Medical Center. These patients had surgery consecutively, and no patient was excluded from the analysis.
Our technique for laparoscopic RYGB includes a side-to-side GIA-stapled jejunojejunostomy with a retrocolic, retrogastric alimentary limb and closure of all mesenteric defects. The gastrojejunostomy (GJ) is a two-layer anastomosis. The inner layer consists of a GIA-stapled side-to-side posterior row with a running sewn gastroenterotomy closure, whereas the outer layer is hand-sewn circumferentially. The GJ is routinely tested for leak with endoscopic insufflation.
Data were collected under approval from the institutional review board. For each patient, we collected data regarding demographics (age, gender, preoperative body mass index [BMI]), the presence of medical comorbidities (diabetes mellitus, hypertension, obstructive sleep apnea, musculoskeletal complaints, dyslipidemia, gastroesophageal reflux disease [GERD], peptic ulcer disease [PUD]), technical factors (choice of permanent or absorbable suture for the inner layer of the GJ, attending as primary surgeon, robotic GJ, operative time, postoperative hematocrit drop), and preoperative Helicobacter pylori infection.
Helicobacter pylori was diagnosed by a commercial enzyme-linked immunoassay (ELISA) serum assay (Diamedix Inc, Miami, FL, USA) with a sensitivity of 98% and a specificity of 94%. Marginal ulcers were diagnosed by upper endoscopy (EGD). Postoperative EGD was performed for all patients with epigastric pain, persistent nausea and vomiting, or gastrointestinal hemorrhage. At the time of the study, all the patients were postoperatively prescribed 3 months of H2-blocker therapy.
Fisher’s exact test was used for statistical analysis of discrete variables, and Student’s t-test was used for continuous variables. Statistical significance was set at an alpha of 0.05 for all analyses.
Results
Among the 260 patients, the average age was 42 years and the average BMI was 44 kg/m2. The patients were predominantly female (90%). There were no significant differences in demographics between the two study groups (marginal ulceration vs no marginal ulceration) (Table 1).
The overall mean follow-up period was 10.2 months. The mean follow-up period was 10 months for the no marginal ulceration group and 12 months for the marginal ulceration group (p = 0.2, nonsignificant difference). Overall, marginal ulcers developed in 19 (7%) of the 260 patients. The mean time to onset of marginal ulceration symptoms after surgery was 4.3 months (range, 1–12 months) (Fig. 1). Epigastric pain was the most common presenting symptom, occurring in 89% of the patients and as the only symptom in 47% of these patients. Nausea, with or without vomiting, developed in 42% of patients, whereas only 21% experienced bleeding from their ulcers.
The comorbidity profile of our population is summarized in Fig 2. There were no statistical differences in the prevalence of any comorbidity between the two groups (Table 1). Notably, there was no difference in the prevalence of GERD (p = 0.8), GERD requiring medical treatment (p = 0.1), or history of PUD (p = 1.0).
Technical factors also were similar between the two groups. The mean operative time and postoperative hematocrit drop were not significantly different. Similarly, there were no significant differences when the GJ was constructed with the surgical robot or when the attending was the primary surgeon. The prevalence of intraoperative GJ leaks, all subjected to repair, was not significantly different between the groups. During the study period, the suture material used for the inner layer of the GJ anastomosis was changed from permanent to absorbable suture. For the first 136 cases, permanent suture was used, and for the subsequent 124 cases, absorbable suture was used. The marginal ulceration rate was 7% (9/136) in the permanent suture group and 8% (10/124) in the absorbable suture group (p = 0.8, nonsignificant difference).
Of the 19 patients with marginal ulceration, 6 (32%) were seropositive for H. pylori antibody preoperatively. In contrast, only 12% of the patients without marginal ulceration were found to have preoperative H. pylori infection (88% of the patients without marginal ulceration were tested for H. pylori preoperatively). The higher rate of preoperative H. pylori infection among patients who experienced marginal ulcers was statistically significant (p = 0.02). All the patients found to have H. pylori infections were treated preoperatively with a standard 2-week course of antibiotics and proton pump inhibitors.
Overall, 68% of the patients in whom marginal ulceration developed were checked postoperatively for H. pylori, and none had positive test results. Specifically, 50% of the patients who were seropositive for H. pylori preoperatively and had marginal ulceration were rechecked for the organism postoperatively by EGD, and none showed positive test results. Suture remnants were visible in 32% of the ulcer beds on EGD (44% of the cases with permanent suture and 20% of the cases with absorbable suture used for the GJ; p = 0.3, nonsignificant difference).
Preoperative EGD was selectively performed for 36% of the patients for various clinical indications. Among the patients who did not experience ulcers, 38% had gastritis, 8% had healed ulcers from previous PUD, and 4% had Barrett’s esophagus. Of the patients in whom marginal ulceration developed, 26% underwent a preoperative EGD. This test showed gastritis in 80% of these patients. No patient who experienced marginal ulceration had preoperative PUD or Barrett’s esophagus. All the patients with gastritis diagnosed by EGD were treated with proton pump inhibitors preoperatively. The rate of gastritis shown on preoperative EGD was not significantly different between the two groups (p = 0.15).
We were able to define the nonsteroidal antiinflammatory drug (NSAID) usage among the patients who experienced marginal ulceration. Only one patient took NSAIDs postoperatively, despite a directive to avoid such medications. Another patient required NSAIDs up to the time of surgery, but did not need them postoperatively. Thus, only 2 (11%) of the 19 patients in whom marginal ulcers developed had documented NSAID use.
All the patients who experienced marginal ulceration had complete resolution of their symptoms with proton pump inhibitors and sucralfate. No reoperations were required for marginal ulcers.
Discussion
Marginal ulceration is a significant complication of Roux-en-Y gastric bypass. This phenomenon has been recognized and studied since the advent of the procedure. Several factors, including gastric acid, foreign body reaction, exogenous substances, and H. pylori infection, have been implicated as potential etiologies of this complication.
Gastric acid
It is hypothesized that peptic digestion of the unprotected jejunal mucosa leads to marginal ulceration and that this process is augmented by the secretion of gastric acid from parietal cells within the gastric pouch. Initially, large pouch size (>50 ml) was thought to predispose patients to marginal ulceration [24]. The larger parietal cell mass in the pouch was thought to create a higher volume of gastric acid, with less of this acid passed into the antrum and duodenum. Thus, it was proposed that the decrease in inhibitory feedback to antral G-cells upregulated gastrin and, thereby, gastric acid secretion [23, 24]. Indeed, reducing the size of the gastric pouch has been shown to decrease the incidence of marginal ulcers [27].
The orientation of the gastric pouch also has been hypothesized to play a role in acid secretion and the formation of marginal ulceration. The lesser curvature, with its high concentration of parietal cells, may lead to marginal ulceration if too much of the magenstrasse is included in the pouch [4, 14, 18]. Sapala et al. [31] found that creating a pouch limited to the cardia resulted in a 0.01% marginal ulceration rate at 1 year among 173 patients.
Staple line disruption, with resultant gastrogastric fistula, is yet another phenomenon that ultimately results in increased acid in the gastric pouch. Staple line dehiscence is seen primarily when the pouch is created by an undivided staple line through the proximal stomach [4, 5, 8]. Clearly, once a connection between the gastric remnant and the pouch is established, the jejunal mucosa is exposed to a greater volume of low-pH fluid. Several studies have now demonstrated that by separating the remnant stomach from the gastric pouch, as commonly performed in current bariatric surgery, the incidence of marginal ulceration can be lowered [4, 12, 21].
However, a central role for gastric acid in the development of marginal ulceration has been challenged by several studies that have found a virtual absence of acid secretion within the gastric pouch after gastric bypass [2, 21, 24, 35]. Yet, this significant decrease in acid secretion after gastric bypass may not be universal. Mason et al. [24] found that although gastric acid secretion is nearly absent in most patients after gastric bypass, 43% of their patients had a low pH within the pouch. Additionally, serum gastrin levels were found to be universally low after gastric bypass [24]. Thus, it was postulated that gastric acid secretion is primarily driven by gastrin in most obese patients, but that in patients who continue to have low gastric pH after surgery, vagal innervation may dominate acid secretion. Such patients were found to be at higher risk for marginal ulcers. Further investigations supported the findings of increased acid production [18] and prolonged duration of low gastric pH (<4) [16] after gastric bypass among patients who experienced marginal ulceration.
Thus, gastric acid seems to predispose patients to the development of marginal ulcers. This is further supported by evidence that acid suppression alone is effective in healing marginal ulcers [6, 10, 15, 16, 18, 26].
Foreign body
The foreign body (staples or suture material) used to construct the GJ has been hypothesized to cause an inflammatory reaction and lead to ulcer formation. Capella et al. [5, 6] decreased the marginal ulcer rate from 5.1% to 1.5% by switching from a stapled to a hand-sewn GJ, with absorbable suture used for the inner layer and permanent suture for the outer layer. The marginal ulceration rate further decreased to 0.4% when absorbable suture was used for both layers [6]. In a study of 3,285 patients, the marginal ulceration rate was significantly higher when the inner row of the GJ was constructed with permanent suture (2.6%) rather than absorbable suture (1.3%) [29]. We did not find a change in marginal ulceration rate when the type of suture used for the GJ was changed.
Exogenous substances
In the general population, NSAIDs have clearly been shown to cause gastric ulcers. In the context of marginal ulceration after gastric bypass, NSAIDs are believed to predispose patients to this complication [17], but a direct correlation has not been conclusively defined, especially among symptomatic patients [3]. Only 11% of our patients in whom marginal ulcers developed reported NSAID use. Smoking also may predispose patients to the development of marginal ulceration [3, 34]. Only one of our patients with marginal ulceration admitted to smoking. This patient also used NSAIDs.
Helicobacter pylori
Helicobacter pylori has been implicated as a possible causative agent in the formation of marginal ulcers after gastric bypass [7]. Findings have shown marginal ulceration to be less common among patients preoperatively screened and treated for H. pylori than among patients who were not screened, and thus not treated [33].
In our series, we found that marginal ulceration was significantly more common among patients infected with H. pylori preoperatively, even when adequately treated before gastric bypass. Furthermore, none of the patients who experienced marginal ulceration and were tested for H. pylori postoperatively had evidence of ongoing infection. Other investigators also have reported this lack of correlation between postoperative H. pylori infection and marginal ulceration [22, 34].
The actual mechanisms of H. pylori pathogenesis still are under active investigation. However, it seems clear that H. pylori incites a cytokine-mediated inflammatory response, which leads to gastritis, intestinal metaplasia, and ultimately ulcer formation [36]. Chronic gastritis and intestinal metaplasia slowly regress after H. pylori eradication, often taking more than a year to resolve [13, 20].
Our data suggest that a history of H. pylori infection may predispose to marginal ulcer formation after gastric bypass. Our mean follow-up period of 10 months is certainly sufficient to have identified the vast majority of the ulcers, which tend to occur within the first 2 to 3 months after gastric bypass and are rare (0.5%) after 6 months from surgery [16, 26, 30]. Certainly, the ideal method for screening patients to detect marginal ulceration would be routine EGD for all postoperative patients. Because this approach is impractical, we use EGD selectively on the basis of patient symptoms. This limitation, shared by other investigators who have studied marginal ulceration, may underestimate the true incidence of this postoperative complication.
Two pieces of data emerge from our study. First, we present evidence of an association between preoperative H. pylori infection and marginal ulceration. Second, there is a well-documented absence of H. pylori postoperatively among marginal ulceration patients. We thus postulate that anastomotic ulcer formation after gastric bypass may be potentiated by preoperative injury to the gastric mucosa induced by H. pylori infection, even in the absence of ongoing infection by the organism postoperatively.
References
Ali MR, Fuller WD, Choi MP, Wolfe BM (2005) Bariatric surgical outcomes. Surg Clin North Am 4: 835–852
Behrns KE, Smith CD, Sarr MG (1994) Prospective evaluation of gastric acid secretion and cobalamin absorption following gastric bypass for clinically severe obesity. Dig Dis Sci 39: 315–320
Ben-Meir A, Sonpal I, Patterson L, Schreiber H, Salomone M, Sharma K, Kumar A, Marshall JB (2005) Cigarette smoking, but not NSAID or alcohol use or comorbidities, is associated with anastomotic ulcers in Roux-en-Y gastric bypass (RYGB) patients. Surg Obes Relat Dis 1: 263
Capella JF, Capella RF (1996) Staple disruption and marginal ulceration in gastric bypass procedures for weight reduction. Obes Surg 6: 44–49
Capella JF, Capella RF (1999) Gastrogastric fistulas and marginal ulcers in gastric bypass procedures for weight reduction. Obes Surg 9: 22–27
Capella JF, Capella RF (2002) An assessment of vertical banded gastroplasty–Roux-en-Y gastric bypass for the treatment of morbid obesity. Am J Surg 183: 117–123
Cleator IGM (1996) Ulcerogenesis following gastric procedures for obesity. Obes Surg 6: 260–261
Cucchi SG, Pories WJ, MacDonald EK (1995) Gastrogastric fistulas: a complication of divided gastric bypass surgery. Ann Surg 221: 387–391
Dallal RM, Bailey LA (2006) Ulcer disease after gastric bypass surgery. Surg Obes Relat Dis 2: 455–459
Fobi MAL (1992) Marginal ulcer after gastric bypass. In: Mason EE (ed) Surgical treatment of morbid obesity. problems in general surgery, vol 9, no 2, JB Lippincott, Philadelphia pp 345–352
Fobi MAL (1993) Operations that are questionable for control of obesity. Obes Surg 3: 197–200
Fobi MAL, Lee H, Igew D (2001) Prospective comparative evaluation of stapled versus transected Silastic ring gastric bypass: six-year follow-up. Obes Surg 1: 18–24
Gisbert JP, Blanco M, Pajares JM (2000) Effect of Helicobacter pylori eradication on histological lesions of gastric mucosa: an 18-month follow-up study. Rev Clin Esp 9: 480–484
Griffen WO (1997) Stomal ulcer after gastric restrictive operations. J Am Coll Surg 185: 87–88
Gumbs AA, Duffy AJ, Bell RL (2006) Incidence and management of marginal ulceration after laparoscopic Roux-Y gastric bypass. Surg Obes Relat Dis 4: 460–463
Hedberg J, Hedenstrom H, Nilsson S, Sundbom M, Gustavsson S (2005) Role of gastric acid in stomal ulcer after gastric bypass. Obes Surg 15: 1375–1378
Higa KD, Boone KB, Ho T (2000) Complications of the laparoscopic Roux-en-Y gastric bypass: 1,040 patients: what have we learned? Obes Surg 6: 509–513
Jordan JH, Hocking MP, Rout WR, Woodward ER (1991) Marginal ulcer following gastric bypass for morbid obesity. Am Surg 57: 286–288
Kral JG (1985) Morbid obesity and related health risks. Ann Intern Med 103: 1043–1047
Kyzekova J, Mour J (1999) The effect of eradication therapy on histological changes in the gastric mucosa in patients with nonulcer dyspepsia and Helicobacter pylori infection: prospective randomized intervention study. Hepatogastroenterology 46: 2048–2056
MacLean LD, Rhode BM, Nohr C, Katz S, McLean AP (1997) Stomal ulcer after gastric bypass. J Am Coll Surg 185: 1–7
Marano BJ (2005) Endoscopy after Roux-en-Y gastric bypass: a community hospital experience. Obes Surg 15: 342–345
Mason EE (1996) Ulcerogenesis in surgery for obesity. Obes Surg 6: 180–181
Mason EE, Munns JR, Kealey GP (1976) Effect of gastric bypass on gastric secretion. Am J Surg 131: 162–168
National Institutes of Health (1991) Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med 115: 956–961
Pope GD, Goodney PP, Burchard KW (2002) Peptic ulcer/stricture after gastric bypass: a comparison of technique and acid suppression variables. Obes Surg 12: 30–33
Printen KJ, Scott D, Mason EE (1980) Stomal ulcers after gastric bypass. Arch Surg 115: 525–527
Rolls BJ (2003) The supersizing of America portion size and the obesity epidemic. Nutr Today 38: 42–53
Sacks BC, Qureshi FG, Eid GM, Collins JL, Barinas-Mitchell EJ, Schauer PR, Ramanathan RC (2006) Incidence of marginal ulcers and the use of absorbable anastomotic sutures in laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 2: 11–16
Sanyal AJ, Sugerman HJ, Kellum JM, Engle KM, Wolfe L (1992) Stomal complications of gastric bypass: incidence and outcome of therapy. Am J Gastroenterol 87: 1165–1169
Sapala JA, Wood MH, Sapala MA, Flake Jr TM (1998) Marginal ulcer after gastric bypass: a prospective 3-year study of 173 patients. Obes Surg 8: 505–516
Schauer PR, Ikramuddin S (2001) Laparoscopic surgery for morbid obesity. Surg Clin North Am 81: 1145–1179
Schirmer B, Erenoglu C, Miller A (2002) Flexible endoscopy in the management of patients undergoing Roux-en-Y gastric bypass. Obes Surg 12: 634–638
Schreiber H, Ben-Meir A, Sonpal I, Patterson L, Salomone M, Marshall JB (2005) Cigarette smoking, but not the presence of H. pylori, is associated with anastomotic ulcers in Roux-en-Y gastric bypass patients. Surg Obes Relat Dis 1: 257
Smith DC, Herkes SB, Behrns KE (1993) Gastic acid secretion and vitamin B12 absorption after vertical Roux-en-y gastric bypass for morbid obesity. Ann Surg 218: 91–96
Suerbaum S, Michetti P (2002) Helicobacter pylori infection. N Engl J Med 347: 1175–1186
Sugerman HJ, Kellum JM, Engle KM (1992) Gastric bypass for treating severe obesity. Am J Clin Nutr 55: 560–566
Wyatt HR (2003) The prevalence of obesity. Prim Care 30: 267–279
Zimmermann-Belsing T, Feldt-Rasmussen U (2004) Obesity, the new worldwide epidemic threat to general health and our complete lack of effective treatment. Endocrinology 145: 1501–1502
Acknowledgments
The authors thank Mr. William Smith for his assistance in accumulating data and Mrs. Marie Carvidi for her editorial assistance. This research was supported by a research grant from Stryker Endoscopy.
Author information
Authors and Affiliations
Corresponding author
Additional information
Submitted for oral/poster presentation at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons (SAGES), April 2007
Rights and permissions
About this article
Cite this article
Rasmussen, J.J., Fuller, W. & Ali, M.R. Marginal ulceration after laparoscopic gastric bypass: an analysis of predisposing factors in 260 patients. Surg Endosc 21, 1090–1094 (2007). https://doi.org/10.1007/s00464-007-9285-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9285-x