Abstract
Background
Five International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) surveys since 1998 have estimated the volume and type of bariatric surgery being done in constituent member countries. These reports did not include baseline demographic descriptions.
Methods
An IFSO Global Registry pilot project in 2014 demonstrated that it was possible to amalgamate large numbers of individual patient data from different local and national database systems. Here we describe demographic data from the second report for 54,490 patients from 31 countries operated in the 3 calendar years 2013–2015 and follow up data from 66,560 of 112,544 patients in 2009–2015.
Results
Most procedures (97.8%) were performed laparoscopically and 73.3% (95% CI: 73.0–73.7%, range 54.2 to 80.3%) were female. The average age was 42.0 years (95% CI 41.9–42.1, inter-quartile range 33.0–51.0 years) and the median body mass index was 43.3 kg/m2 (inter-quartile range 39.4–48.8 kg/m2). Before surgery, 22.0% patients had type 2 diabetes (inter-country variation 7.4–63.2%); 31.9% were hypertensive (15.8–92.7%); 17.6% had depression (0.0–46.3%); 27.8% took medication for musculoskeletal pain (0.0–58.9%); 18.9% had sleep apnea (0.0–63.2%); and 29.6% of patients had gastro-esophageal reflux disease (9.1–90.9%). Gastric bypass was the most prevalent operation (49.4%), followed by sleeve gastrectomy (40.7%) and gastric banding (5.5%). The 1-year total weight loss for patients with available data was 30.53% (95% CI: 30.22–30.84%) and in the cohort 2009–15 was 30.4% with a follow-up rate of 59.14%. In the 2009–2015 cohort, 64.7% of patients on treatment for diabetes preoperatively were not on treatment postoperatively.
Conclusions
There is widespread variation in access to surgery and in baseline patient characteristics in the countries submitting data to the IFSO Global Registry.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery has now been established to be safe and effective for weight loss maintenance and control of obesity-related disease as demonstrated by the Swedish Obese Subjects study, a prospective cohort control study, and by randomized control trials [1,2,3,4,5]. Despite the available evidence, only a fraction of patients who fulfill the eligibility criteria and would benefit from surgery are referred, assessed, considered for surgery, and eventually operated [6]. On a global scale, the demographic of the escalating obesity challenge has been described in multiple reports with great detail including gender and age distribution, employment status, social class, and receipt of state benefits [7].
Starting in 1998, Scopinaro, Buchwald, and Angrisani et al. have published data on the volumes of bariatric/metabolic surgery performed worldwide in the constituent countries of the International Federation for Surgery for Obesity and Metabolic Disorders (IFSO) [8,9,10,11,12]. The data were largely based on estimates and did not include baseline patient demographics or follow-up. If the uptake and acceptance of bariatric/metabolic surgery is to increase globally, it seems logical to establish detailed characterization of the operated population, to include gender distribution, age, body mass index (BMI), and disease burden. With this information, healthcare systems could estimate the overall effect of surgery and thus plan effective services. A global registry might provide a mechanism to do this.
The IFSO established in 2014 a Global Registry Pilot Project in collaboration with an international medical registry software provider [13]. The aims were to (1) establish that it was possible and feasible to combine large numbers of individual patients records from different local and national database systems; (2) demonstrate that the Dendrite Clinical Systems Ltd. software was capable of providing a robust on-line data-capture platform and a parallel system for uploading data; (3) establish that it was possible to provide meaningful analysis of these data; and (4) provide a basis for generating research questions for future investigation. A comprehensive charter of ownership was also set up regarding use and ownership of the accumulated data. This documented the aims of the project, and details of data protection and governance of the registry including access, data ownership, publication and other uses of the data, principles of operation (roles and responsibilities), data validation, and supervising authorities.
Invitations to participate were sent to 48 individual centers or national bariatric societies. In the first report, 100,092 individual operation records were submitted from 25 centers or national registries in 18 countries [13].
On the basis that the aims had been met, the IFSO Executive Council commissioned a second report and appointed an international committee to oversee data analysis, interpret, and publish the results. A synopsis of the data was presented to the IFSO World Congress in Rio de Janeiro in September 2016 [http://www.ifso2016.com]. Data were also presented as a synopsis in pdf and book form [14]. The aims of the second registry report were to (1) establish baseline demographic characteristics for patients operated in different countries, either from the respective national registries or individual units in these countries; and (2) record basic 1-year post-operative data. In this paper, we present the baseline demographic and operative data, and the basic 1-year post-operative data from the second report.
Methods
For the second report, invitations to participate were sent to all 63 constituent national society members of IFSO by Dr. N Zundel, IFSO President 2015–2016. The Dendrite Intellect Web database technology platform, a Direct Data Entry system, and an Upload-My-Data web portal were used to upload, merge, and analyze the data. Thirty-one (49%) of the invited countries responded positively and were able to contribute. Two presidents of national societies indicated that they could not submit data that year but would do so in the future.
All contributors received a copy of the IFSO Global Registry Charter. The contributors who returned their signed charter document and who had access to electronic data uploading received a unique contributor submit identifier code, a username, and password to access the specifically designed Dendrite/IFSO Upload-My Data portal accompanied by four documents: the Database Form, the File Specification Document, the Data Dictionary, and the User Manual. This information is available on rs2.e-dendrite.com/csp/PUBLIC/DocPublic/UploadMyData/IFSO2/ifso2.csp. Access to an on-line database system was provided for centers without a local database [14]. The database forms are in the supplemental files (or Dendrite website).
Data from 7 national registries were provided: India, Israel, the Netherlands, Russia, Sweden, Turkey, and the UK. Centers from 24 countries contributed data, therefore data from 31 countries are presented. It should be highlighted that in some countries only a small number of individual centers, at times as few as 1 center, provided data in the absence of national registries. Hence, data presented here may not be representative of the country. A list of the contributing centers is in the supplemental files (Fig 1).
Descriptive statistics were used for the analysis of the data. The contributors were reassured that no statistical comparison would be attempted between different units. Furthermore, as data from different countries may only provide variable representation of the population, no comparative analysis was performed between countries.
Results
A brief data set was chosen with yes/no choices for related disease (Table 1). Data from 31 countries included 142,748 operation records, 88.5% of those were in the period 2009–2015 and 42% (54,490) in the period 2013–2015 (Table 2). The individual contributions ranged from 55 records from 1 center to the national UK registry of 47,000. The baseline records were > 80% completed in 62.4%. For the preoperative characteristics, we present data for 2013–2015. For the 1-year weight loss, we present data for the 2009–2015 cohort.
The average age was 42 years (inter-quartile range (IQR): 33–51). The age reflects the variation in practice in the extremes of age, with some countries providing adolescent (and even pediatric in the case of Saudi Arabia) bariatric surgery, and in different countries a clear cutoff beyond a certain age (Fig. 2a). The average preoperative was BMI 44.7 kg m−2 (IQR: 39.4–48.8) with a wide variation ranging from 36.6 kg m−2 in Peru to 49.1 kg m−2 in Ireland (Fig. 2b). The prevalence of obesity defined as BMI of ≥ 30 kg m−2 in the same countries according to the World Health Organization is also presented in Fig. 2b [15]. The proportion of patients who were female was 73.3%, ranging from 54.2% in Brazil to 80.3% in the Netherlands.
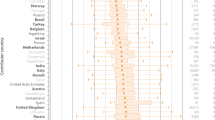
The prevalence of preoperative diabetes as reflected by the number of patients on medication for the condition was 22% (IQR: 7.4–63.2) and the wide variation among different countries can be seen on Fig. 3 [16]. The prevalence of treatment of hypertension was even higher at 31.9% (IQR: 15.8–92.7). Treatment for sleep apnea was 18.9% (IQR: 0–63.2%), depression 17.6% (IQR: 0–46.3), musculoskeletal pain 27.8% (0–58.9), and gastro-esophageal reflux disease 29.6% (9.1–90.9).
More than half (58.3%) of procedures were funded by the public health service with a wide variation between contributor countries reflecting different health systems but also the type of provider the contributing centers are. BMI and the prevalence of treatment for diabetes are presented in Fig. 4a and b
Most procedures were performed laparoscopically (97.8%). The type of primary surgery (n = 51,820) was gastric bypass in 25,594 (49.4%), sleeve gastrectomy in 21,079 (40.7%), gastric band 2865 (5.5%), duodenal switch with sleeve gastrectomy 305 (0.6%), duodenal switch 29 (0.05%), and biliopancreatic diversion 21 (0.04%). The variation between different regions can be seen in Fig. 4c This should be interpreted with caution, particularly for North America as the data are from one center performing predominantly bypass and is therefore not representative of the region.
The Obesity Surgery Mortality Risk score (OS-MRS) was used to estimate perioperative risk. The distribution between the countries where the OS-MRS could be measured is presented in Fig. 4d (n = 34,643). The highest risk populations (group B and C) were in Turkey (57.9%), Ireland (56.9%), Hong Kong (55.1), and the lowest in Peru (22.2%), the Netherlands (23.9%), and Panama (26%).
The hospital stay was 1 day after gastric banding (88.1% of patients), 2 days after gastric bypass (75.4%), and 3 days for sleeve gastrectomy (86.8%). More detailed information is provided in Fig. 5.
The 1-year total weight loss in this cohort (n = 3988) was 30.53% (95% CI: 30.22–30.84%). The follow-up of this cohort was limited due to the common practice of non-contemporaneous input of data in registries and/or lack of complete submission by the contributors (7.7%, 3988 out of 51,820 patients with 1-year weight loss data). Therefore, we report total body weight loss for the period 2009–2015 which was 30.4%. Out of 112,544 patients in this cohort, there was follow-up data available for 66,560. The average percentage total body weight loss according to initial BMI and procedure can be seen in Fig. 6a. For the same population (2009–2015), 64.7% of patients on treatment for diabetes preoperatively were not on treatment postoperatively; however, we do not report glycemic control or diabetes remission outcomes as these were not part of the dataset. There was a marked reduction in treatment of depression, hypertension, musculoskeletal pain, sleep apnea, and gastro-esophageal reflux disease (Fig. 6b).
Discussion
This is a substantial dataset of patients undergoing bariatric surgery around the world. Although there are centers from 31 countries, there are large parts of the world with no available data. For example, no data are reported from Australasia and Africa. More importantly with the exception of the seven national registries, the data reported here might not be representative of the country’s practice. Nevertheless, this is the first attempt to capture the characteristics of the population operated worldwide. The wide variation among different parts of the world is demonstrated.
We did not provide any safety data as mortality or complication rate were not in the remit of the study. If national registries become increasingly used and if data validation became the norm, perioperative morbidity and mortality will become available. Thus, it would be possible to estimate the worldwide complication and mortality rates of surgery compared to non-surgical treatments of obesity.
The 1-year weight loss and comorbidity improvement data support reports of smaller prospective studies that bariatric surgery is effective. Focusing on diabetes, glycemic control measures such as glycated hemoglobin and fasting glucose were not collected and therefore diabetes remission and glycemic control outcomes cannot be reported. The fact that 64.7% of diabetic patients are reported as being no longer diabetic is in accordance with previous reports [3, 17, 18]. Thus, the findings of this study complement the previous worldwide surveys. Future global registry reports could provide not only glycemic control data, but also cardiovascular risk and mortality.
The limitations of this registry include the incompleteness of data in some countries potentially leading to selection bias. According to the most recent IFSO estimate for the volume of surgery being done worldwide our data comprise about 4%, based on the assumption that 468,000 patients were operated in each year 2013–2015 [12]. In addition, we have not validated all of the data using other sources of information, although this has been achieved for the Swedish registry. The majority of the patients in the global registry are from two large national registries; therefore results from these countries have a substantial impact on this report. However, the data reported here represent the first attempt at obtaining a demographic characterization of bariatric surgery performed worldwide. This information adds to individual country registries, individual center series, and worldwide surveys, confirming that bariatric surgery is effective as previously reported in longitudinal series and randomized control trials.
In conclusion, there is a wide variation in the population undergoing bariatric surgery worldwide. Most of the operations are performed laparoscopically, and the most common ones are gastric bypass, sleeve gastrectomy, and gastric banding. There is a large but variable burden of associated disease. One-year weight loss data support bariatric surgery being effective in a very large combined cohort. Future reports could expand our knowledge of the obesity-related disease that is being treated by bariatric surgery worldwide.
References
Arterburn DE, Courcoulas AP. Bariatric surgery for obesity and metabolic conditions in adults. BMJ. 2014;349:g3961.
Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386:964–73.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370:2002–13.
Welbourn R, le Roux CW, Owen-Smith A, et al. Why the NHS should do more bariatric surgery; how much should we do? BMJ. 2016;353:i1472.
Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Scopinaro N. The IFSO and obesity surgery throughout the world. Obes Surg. 1998;8:3–8.
Buchwald H, Williams SE. Bariatric surgery worldwide 2003. Obes Surg. 2004;14:1157–64.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg. 2009;19(12):1605–11.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23(4):427–36.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25:1822–32.
Welbourn R, Gagner M, Naslund I, Ottosson J, Kinsman R, Walton P. First IFSO Global Registry Report 2014. Dendrite Clinical Systems Ltd., Henley-on-Thames, RG9 1AY, UK. 2014. ISBN 978-0-9568154-9-1.
Welbourn R, Dixon J, Higa K, Kinsman R, Ottosson J, Ramos A et al. Second IFSO Global Registry Report 2014. Dendrite Clinical Systems Ltd., Henley-on-Thames, RG9 1AY, UK. 2014. 2016. ISBN 978-0-9929942-1-1.
World Health Organization. Global Health Observatory data repository. apps.who.int/gho/data/node.main.A900 A?lang=en. Accessed 14 Aug 2017.
International Diabetes Federation Atlas. Seventh Edition, 2015. http://www.dmthai.org/sites/default/files/idf_atlas_2015_uk_0.pdf. Accessed 14 Aug 2017.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122:248–256.e5.
Pournaras DJ, Aasheim ET, Søvik TT, et al. Effect of the definition of type II diabetes remission in the evaluation of bariatric surgery for metabolic disorders. Br J Surg. 2012;99:100–3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding Declaration
The IFSO Global Registry Second Report was funded by the International Federation for Surgery for Obesity and Metabolic Disorders.
Conflict of Interests
Dr. Welbourn declares support for attending conferences from Ethicon Endo-Surgery, consultancy fees from Novo Nordisk, funding of a Bariatric Clinical Fellow in Musgrove Park Hospital, Taunton TA1 5DA, UK from Ethicon Endo-Surgery, outside the submitted work. Dr. Dixon declares grants from NHMRC during the conduct of the study; personal fees from Apollo Endo-surgery, Bariatric Advantage, Covidien, iNova Pharmaceuticals, Novartis, Nestle, Novo Nordisk, mdBriefcase outside the submitted work. Dr. Higa declares personal fees from Ethicon, other from Endogastric Solutions outside the submitted work. Dr. Kinsman and Dr. Walton declare grants from IFSO during the conduct of the study, other grant from IFSO outside the submitted work. Dr. Pournaras Dr. Ottosson, Dr. Ramos, Dr. van Wagensveld, Dr. Weiner, and Dr. Zundel declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Welbourn, R., Pournaras, D.J., Dixon, J. et al. Bariatric Surgery Worldwide: Baseline Demographic Description and One-Year Outcomes from the Second IFSO Global Registry Report 2013–2015. OBES SURG 28, 313–322 (2018). https://doi.org/10.1007/s11695-017-2845-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2845-9