Abstract
Background
Knowledge regarding the feasibility and safety of sleeve gastrectomy (SG) in obese liver transplant recipients is scarce. We report our experience of sleeve gastrectomy following liver transplantation (LT).
Methods
All patients who had undergone LT and subsequently underwent SG at our institution were retrospectively reviewed. Surgical outcomes, liver and kidney function tests, outcomes of obesity-related comorbidities, and excess weight loss were analyzed.
Results
Between May 2008 and February 2015, six consecutive patients underwent SG after LT. Three procedures (50%) were performed totally by laparoscopy, and three by upfront laparotomy for concomitant incisional hernia complex repair. Within the first 30 days, one complication occurred: early gastric fistula that required multiple endoscopic procedures and re-intervention, followed by death 19 months after SG due to multi-organ failure. Another patient had one late complication: chronic infection on a parietal mesh successfully controlled by mesh removal. Excess weight loss averaged 76% at 2 years with a median BMI of 28 (21–39) kg/m2. Median follow-up was 37.2 months (range 13–101 months). Median length of stay was 9 days (range: 6–81 days).
Conclusions
SG is technically feasible after LT and resulted in weight loss without adversely affecting graft function and immunosuppression. However, morbidity and mortality are high.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the World Health Organization, a body mass index (BMI) ≥ 25, ≥ 30, and ≥ 35 kg/m2 define overweight, obesity, and severe obesity, respectively. Worldwide, more than 1.9 billion adults were overweight in 2014 of whom, over 600 million met the criteria for obesity [1]. In the setting of liver transplantation, the US Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients reported that 54% of patients undergoing orthotopic liver transplant (OLT) were either overweight or obese, and 7% of patients who received liver transplant were considered severely or morbidly obese [2]. In 2025, non-alcoholic steatohepatitis (NASH) is predicted to become the main cause of liver failure requiring liver transplantation (LT) in the USA [3]. Morbid obesity has been associated with both increased mortality on the LT waitlist [4], and adverse impact on outcomes with reduced patient and graft survivals [5].
Subsequently, bariatric surgery (BS) has been proposed before, during, and after LT [6,7,8].
BS in obese LT recipient includes the followings potential specific risks: (i) technical difficulties due to adhesions in the left upper quadrant, (ii) infection and poor healing as a result of immunosuppression, and (iii) potential graft rejection due to impaired immunosuppression pharmacokinetics [8]. The purpose of the present study was to assess the feasibility and outcomes of sleeve gastrectomy (SG) in severely obese patients following previous LT.
Materials and Methods
The institutional review board approved this observational descriptive study of consecutive severely obese patients submitted from 2008 to 2015 to SG after LT.
Patients were considered candidates for SG after LT if they had a body mass index (BMI) of 35 kg/m2 or greater with weight-related comorbidities. Preoperative management of patients was standard for obese patients including a comprehensive medical evaluation and counseling by a multidisciplinary board (bariatric surgeon, endocrinologist, psychologist, and dietician) for at least 6 months, as requested by the French guidelines for bariatric surgery [9]. Decision to proceed to BS was discussed at the BS board with the participation of hepatologists and liver surgeons.
A bariatric surgeon assisted by a liver surgeon performed all cases of SG. BS was performed upfront by laparotomy in patients needing combined complex repair of LT incision hernia.
Oral calcineurin inhibitor-based immunosuppression was continued throughout the perioperative period. Thromboprophylaxis with enoxaparin for 3 weeks was started 6 h after BS. Postoperatively patients were transferred to the liver ICU for 24 h and then to the liver unit ward. Liver and kidney function tests were measured daily and liver Doppler ultrasonography was performed at day 1 and 5 days after BS.
Outcomes
Postoperative mortality and morbidity were assessed within 90 days of BS or at any time during hospitalization for surgery. Metabolic and bariatric surgery results are reported according to the American Society for Metabolic and Bariatric Surgery standards [10]. Weight loss was measured as percent of excess weight loss (%EWL) and body mass index (BMI) reduction. The %EWL was defined as the ratio between the weight lost after surgery and the overweight according to the formula: [(initial weight) − (postop weight)]/[(initial weight) − (ideal weight)], in which ideal weight is defined by the weight corresponding to a BMI of 25 kg/m2.
The outcome of the following comorbidities was assessed whenever present: diabetes mellitus (DM), hypertension (HT), dyslipidemia, obstructive sleep apnea syndrome (OSAS), and non-alcoholic fatty liver disease (NAFLD). Each comorbidity outcome was assessed as worsened, stable, or improved.
Statistical Analysis
Quantitative variables are reported as median and range. Paired t test was used as appropriate for comparisons. A p value < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS Statistics 23.0 (IBM).
Results
Study Population
Between May 2008 and February 2015, six consecutive patients underwent SG after liver transplantation. During the same period 506 LT and 659 bariatric procedures (SG, n = 275; gastric bypass, n = 341; and adjustable gastric banding, n = 43) were performed.
The main patient characteristics are reported in Table 1. All six patients had at least one obesity-related comorbidity. At BS, the median BMI was 41.9 kg/m2 (range 38–46.1 kg/m2). The median delay from LT to SG was 44 months (range: 36.0–46.1 months) and the median increase of BMI during this delay was 2 kg/m2 (range: 0.0–9.6 kg/m2).
Three procedures (50%) were performed totally by laparoscopy, and three by upfront laparotomy due to the required combined repair of LT incisional hernia, as already mentioned. No artificial grafts were needed for caval, portal, or arterial reconstruction. Median operative time was 150 min (range: 120–240 min). No intraoperative complications occurred. Median length of stay was 9 days (range: 6–81 days). Median follow-up was 37.2 months (range 13–101 months) and no patient was lost to follow-up.
Postoperative Events
Postoperative mortality occurred in one patient following the sole major complication (1/6 patients, 17%) of the series. The third patient of the cohort developed a leak from the gastric staple line, needing multiple surgical and endoscopic reoperations and a prolonged hospital stay (81 days). When the leak finally healed, the patient developed a gastroparesis, provoking a severe dysphagia to solid. Neither endoscopic exploration nor bolus swallow test ruled out any abnormality. Manometry confirmed total aperistalsis of the stomach remnant. After several weeks of parenteral nutrition, and failure of medical treatment, the SG was converted by laparotomy into a Roux-en-Y gastric bypass (RYGB). The patient developed a leak from the gastric pouch, leading progressively to multi-organ failure and death 19 months after SG and 11 months after conversion to RYGB.
Wound infection of the laparotomy incision (1/6 patients, 17%) occurred in one patient. The latter had been operated on for a ventral hernia with an intra-abdominal mesh positioning several months before SG. The infected part of the mesh was removed with a favorable outcome.
The rate of postoperative acute rejection was nil.
Long-Term Outcomes
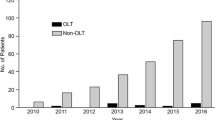
Median %EWL and BMI at 1 year were 76% (range: 25%–119%) and 29 kg/m2 (range: 21–39 kg/m2), respectively (Fig. 1). Median BMI at BS and last follow-up were 42.7 and 29.8 kg/m2 (paired t test; p = 0.007), respectively.
Liver and kidney function tests values at last follow-up were not significantly different as compared to values before sleeve gastrectomy (paired t test, Table 2). The decrease of HbA1C observed in all four diabetic patients did not reach statistical significance.
Antihypertensive medications were stopped in 2/4 patients within 1 year of SG and remained unchanged in the remaining two. Two out of three with OSAS needing upper airway stimulation before SG were weaned of the latter within 6 months of SG.
One patient underwent uneventful partial hepatectomy for recurrent hepatocellular carcinoma (HCC), 49 months after LT for HCC and 13 months after SG.
Discussion
The present series shows that SG after OLT is feasible in patients with severe obesity with significant weight loss at the 1 year follow-up.
The proportion of liver transplant recipients classified as obese has increased from 15% in the early 1990s to 33% in 2011 [11]. Despite conflicting reports [12, 13], BS has emerged as a valuable option to treat obese patients in the setting of LT [6, 14]. As shown in Table 3, BS after LT in adults has been reported so far in 37 cases to date, including the current cases, with a mortality and morbidity rate of 11 and 28%, respectively. During the study period, mortality and severe morbidity rates of SG in our center were nil. However, the mortality and morbidity following BS in the general population was 0.12 and 10%, respectively [23, 24].
In our series, patients lost nearly 56% of their excess body weight within 6 months of BS. In addition, liver graft function was preserved or improved in all patients, with no difficulty in maintaining immunosuppression, and no episodes of acute rejection. Four of the six patients were diabetic, and the dosage of HbA1c before and after SG showed improved control of diabetes after SG as shown by decreased levels of HbA1c; however, this was still not significant.
Five of the six patients with a 1 year of follow-up lost 80% of their excess body weight, but one patient did not lose weight after the SG. These results are consistent with the reported failure rates of relevant series (range: 15–25%) [25, 26].
SG might be the favored bariatric surgical technique in the setting of liver transplantation compared to gastric bypass for two main reasons: (i) SG preserves easy endoscopic access to the biliary tract [8, 27] if ever needed; and (ii) SG does not include any intestinal bypass that could impair the absorption of immunosuppressive or other medications [14, 17, 28].
Only one de novo non-alcoholic fatty liver disease (NAFLD) was discovered after biopsy examinations during post-LT follow-up (Table 4; patient 6). Vallin et al. showed that de novo and recurrent NAFLD after LT were different entities, with the latter being a more severe disease with an earlier onset [29].
Artificial grafts may be used in LT for caval, portal, or arterial reconstruction, especially when vascular grafts from the donor are not available or adequate in terms of length, size, or quality. Complications like infection and migration of these grafts in the stomach can occur and which can complicate the SG [30]. For optimal outcome, SG should be done with presence of a bariatric surgeon and a liver surgeon. In our series, no artificial or vascular grafts were used.
Major limitations of this work include the retrospective nature of the study and the small number of patients. Larger series are needed to confirm the efficacy of BS in liver transplant recipients. Due to the learning curve effect, we assume that these larger series will also show improved safety of the procedure in this setting of LT.
Multivariate analysis would be of interest to identify the risk factors of morbi-mortality. In order to establish significant results, more patients and more events are needed. Our team previously published a systematic review on bariatric surgery and LT [6]. In that paper, 56 patients were included; however, we still had to use a generalized linear mixed model framework with an underlying Poisson distribution because of the small number of patients and events. Confidence intervals were very large not very informative.
In conclusion, SG is feasible in severely obese patients after LT. It results in an improvement in obesity-related comorbidities with no impact on graft function. Larger studies are needed to improve the safety of the procedure in this high-risk population towards that seen in the general population. [8, 14,15,16,17,18,19,20,21,22].
References
World Health Organization. No Title [Internet]. Obesity and overweight. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/.)
Annual Report of the US Organ Procurement and Trans- plantation Network and the Scientific Registry of Transplant Recipients: Transplant Data 1994–2009. Department of health and human services, Health Resources and Services Adminis- tration, Healthca. Available from: https://srtr.transplant.hrsa.gov/annual_reports/2012/pdf/2012_SRTR_ADR.pdf
Thuluvath PJ. Morbid obesity with one or more other serious comorbidities should be a contraindication for liver transplantation. Liver Transpl. 2007;13(12):1627–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18044753
Schlansky B, Naugler WE, Orloff SL, et al. Higher mortality and survival benefit in obese patients awaiting liver transplantation. Transplantation. 2016;100(12):2648–55. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27575690
Conzen KD, Vachharajani N, Collins KM, et al. Morbid obesity in liver transplant recipients adversely affects longterm graft and patient survival in a single-institution analysis. HPB (Oxford). 2015;17(3):251–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25322849
Lazzati A, Iannelli A, Schneck A-S, et al. Bariatric surgery and liver transplantation: a systematic review a new frontier for bariatric surgery. Obes Surg. 2015;25(1):134–42. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25337867%5Cn http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed13&NEWS=N&AN=25337867
Nesher E, Mor E, Shlomai A, et al. Simultaneous liver transplantation and sleeve gastrectomy: prohibitive combination or a necessity? Obes Surg. 2017;27:3–6. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s11695-017-2634-5
Lin MYC, Tavakol MM, Sarin A, et al. Safety and feasibility of sleeve gastrectomy in morbidly obese patients following liver transplantation. Surg Endosc. 2013;27(1):81–5.
Laville M, Romon M, Chavrier G, et al. Recommendations regarding obesity surgery. Obes Surg. 2005;15(10):1476–80. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16354530
American Society for Metabolic & Bariatric Surgery. Metabolic and Bariatric Surgery: Fact Sheet. 2013;24–7. Available from: https://asmbs.org/wp/uploads/2014/05/Metabolic+Bariatric-Surgery.pdf
Singhal A, Wilson GC, Wima K, et al. Impact of recipient morbid obesity on outcomes after liver transplantation. Transpl Int. 2015;28(2):148–55.
Perez-Protto SE, Quintini C, Reynolds LF, et al. Comparable graft and patient survival in lean and obese liver transplant recipients. Liver Transpl. 2013;19(8):907–15.
Lamattina JC, Foley DP, Fernandez LA, et al. Complications associated with liver transplantation in the obese recipient. Clin Transpl. 2012;26(6):910–8.
Elli EF, Gonzalez-Heredia R, Sanchez-Johnsen L, et al. Sleeve gastrectomy surgery in obese patients post-organ transplantation. Surg Obes Relat Dis. 2015. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26823089
A. Duchini MB. Roux-en-Y gastric bypass for recurrent nonalcoholic steatohepatitis in liver transplant recipients with morbid obesity. Transplantation. 2001;72(1):156–71.
Tichansky DS, Madan AK. Laparoscopic Roux-en-Y gastric bypass is safe and feasible after orthotopic liver transplantation. Obes Surg. 15(10):1481–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16354531
Butte JM, Devaud N, Jarufe NP, et al. Sleeve gastrectomy as treatment for severe obesity after orthotopic liver transplantation. Obes Surg. 2007;17(11):1517–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18219781
Gentileschi P, Venza M, Benavoli D, et al. Intragastric balloon followed by biliopancreatic diversion in a liver transplant recipient: a case report. Obes Surg. 2009;19(10):1460–3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19506982
Elli EF, Masrur MA, Giulianotti PC. Robotic sleeve gastrectomy after liver transplantation. Surg Obes Relat Dis. 9(1):e20–2. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22365186
Al-Nowaylati A-R, Al-Haddad BJS, Dorman RB, et al. Gastric bypass after liver transplantation. Liver Transpl. 2013;19(12):1324–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24039124
Pajecki D, Cesconetto DM, Macacari R, et al. Bariatric surgery (sleeve gastrectomy) after liver transplantation: case report. Arq Bras Cir Dig. 2014;27 Suppl 1:81–3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25409975
Khoraki J, Katz MG, Funk LM, et al. Feasibility and outcomes of laparoscopic sleeve gastrectomy after solid organ transplantation. Surg Obes Relat Dis. 2015;12(1):75–83. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26048513
Lazzati A, Audureau E, Hemery F, et al. Reduction in early mortality outcomes after bariatric surgery in France between 2007 and 2012: a nationwide study of 133,000 obese patients. Surg (United States). 2016;159(2):467–74. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26376758
Germanova D, Loi P, van Vyve E, et al. Previous bariatric surgery increases postoperative morbidity after sleeve gastrectomy for morbid obesity. Acta Chir Belg. 113(4):254–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24224433
Sánchez-Santos R, Masdevall C, Baltasar A, et al. Short- and mid-term outcomes of sleeve gastrectomy for morbid obesity: the experience of the Spanish National Registry. Obes Surg. 2009;19(9):1203–10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19572113
Felberbauer FX, Langer F, Shakeri-Manesch S, et al. Laparoscopic sleeve gastrectomy as an isolated bariatric procedure: intermediate-term results from a large series in three Austrian centers. Obes Surg. 2008;18(7):814–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18392898
Sherman S, Shaked A, Cryer HM, et al. Endoscopic management of biliary fistulas complicating liver transplantation and other hepatobiliary operations. Ann Surg 1993;218(2):167–75. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8342996
Heimbach JK, Watt KDS, Poterucha JJ, et al. Combined liver transplantation and gastric sleeve resection for patients with medically complicated obesity and end-stage liver disease. Am J Transplant. 2013;13(2):363–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23137119
Vallin M, Guillaud O, Boillot O, et al. Recurrent or de novo nonalcoholic fatty liver disease after liver transplantation: natural history based on liver biopsy analysis. Liver Transpl. 2014;20(9):1064–71. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24961607
Esposito F, Lim C, Salloum C, et al. Intra-gastric migration of a mesenterico-portal polytetrafluoroethylene (PTFE) jump graft after liver transplantation. Liver Transpl. 2017; Available from: http://www.ncbi.nlm.nih.gov/pubmed/28236364
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Funding
None.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
For this type of study, formal consent is not required.
Additional information
Michael Osseis and Andrea Lazzati are co-first authors
Rights and permissions
About this article
Cite this article
Osseis, M., Lazzati, A., Salloum, C. et al. Sleeve Gastrectomy After Liver Transplantation: Feasibility and Outcomes. OBES SURG 28, 242–248 (2018). https://doi.org/10.1007/s11695-017-2843-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2843-y