Abstract
Background
Compared to healthy individuals, obese have significantly higher systolic and diastolic blood pressure, mean arterial pressure, heart rate, and cardiac output. The aim of this study was to evaluate cardiovascular hemodynamic changes before and 3 months after bariatric surgery.
Methods
Patients scheduled for bariatric surgery between the 29th of September 2016 and 24th of March 2016 were included and compared with 24 healthy individuals. Hemodynamic measurements were performed preoperatively and 3 months after surgery, using the Nexfin® non-invasive continuous hemodynamic monitoring device (Edwards Lifesciences/BMEYE B.V., Amsterdam, the Netherlands).
Results
Eighty subjects were included in this study, respectively, 56 obese patients scheduled for bariatric surgery and 24 healthy individuals. Baseline hemodynamic measurements showed significant differences in cardiac output (6.5 ± 1.6 versus 5.7 ± 1.6 l/min, p = 0.046), mean arterial pressure (107 ± 19 versus 89 ± 11 mmHg, p = 0.001), systolic (134 ± 24 versus 116 ± 18 mmHg, p = 0.001) and diastolic blood pressure (89 ± 17 versus 74 ± 10 mmHg, p = 0.001), and heart rate (87 ± 12 versus 76 ± 14 bpm, p = 0.02) between obese and healthy subjects. Three months after surgery, significant changes occurred in mean arterial pressure (89 ± 17 mmHg, p = 0.001), systolic (117 ± 24 mmHg, p = 0.001) and diastolic blood pressure (71 ± 15 mmHg, p = 0.001), stroke volume (82.2 ± 22.4 ml, p = 0.03), and heart rate (79 ± 17 bpm, p = 0.02)
Conclusions
Three months after bariatric surgery, significant improvements occur in hemodynamic variables except cardiac output and cardiac index, in the patient group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a recognized risk factor for cardiac dysfunction, atherosclerosis, and cardiovascular disease [1, 2]. When combined with hypertension, dyslipidaemia, and type 2 diabetes mellitus, it is known as “metabolic syndrome,” which in itself is an independent predictor of cardiac dysfunction and cardiovascular disease [1, 3]. Increasing evidence from large population-based studies (such as the Framingham Heart Study) and cardiac imaging trials show that long-term obesity can lead to structural changes in cardiac structure, such as left ventricular (LV) dilatation, hypertrophy, and even heart failure [1, 4]. Adipose tissue itself contributes to the circulating volume and must increase cardiac output [5].
The literature suggests that weight loss is able to improve cardiac structure and function and decrease cardiovascular risk (due to reverse remodeling) [6, 7]. Aggarwal et al. [6] summarized the beneficial effects of bariatric procedures on cardiac functional imaging endpoints, but short-term hemodynamic changes have not been studied extensively. Namely the presence of left ventricular hypertrophy (LVH) and hypertension is a prerequisite for cardiac remodeling after bariatric surgery, and in this review, by Aggarwal et al. [6], mostly cardiac structure changes were evaluated, without looking at the short-term hemodynamic changes after bariatric surgery.
The aim of the present study was to evaluate the cardiovascular hemodynamic changes before and 3 months after bariatric surgery. It was hypothesized that bariatric surgery (irrespective of the type of surgical procedure) gives a decrease in cardiac output and in systolic and diastolic blood pressure.
Methods
This study was approved by the Medical Ethics Committee of the Catharina Hospital in Eindhoven, The Netherlands, and adheres the principles of the declaration of Helsinki. Informed consent was obtained from all patients included. This study was conducted according to the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) statement [8].
Patient Population
A multidisciplinary team screened all included patients preoperatively, consisting of a physician assistant, a psychologist, a nutritionist, and a surgeon. Patients were eligible for surgery if they had a BMI of 40 kg/m2 or higher, or a BMI between 35 and 40 kg/m2 with significant comorbidities, with serious attempts to lose weight in the past. Comorbidities were considered significant when medication had to be used, or if continuous positive airway pressure (CPAP) had to be used in case of obstructive sleep apnea (OSAS). Patients with pre-existing cardiac and/or pulmonary and/or kidney diseases were excluded from this study.
The subjects in this study were divided into two groups. Group A of morbidly obese patients scheduled for bariatric surgery that were measured preoperatively and 3 months after bariatric surgery. Group B was a control group of, healthy, health professionals recruited from the research team.
Nexfin® Hemodynamic Monitoring Device
The Nexfin® device (Edwards Lifesciences/BMEYE B.V., Amsterdam, the Netherlands) is based on the volume clamp method first described by Penaz and the Physiocal criteria of Wesseling and provides a reconstructed continuous brachial arterial BP that are used to derive stroke volume [9–14].
Procedure and Data Collection
All hemodynamic measurements were obtained before, and only the patient’s measurements were repeated 3 months after bariatric surgery. Patients were asked to relax for 10 min in a comfortable chair, and any form of disturbance was prevented. After that, each study participant was asked neither to speak nor to move during the measurement. Appropriate cuff size was determined for both the finger and the arm in each participant. The Nexfin® finger cuff was attached to the mid-phalanx of the third digit of the patients left hand. Data of interest were anthropometric variables and comorbidities, hemodynamic variables (systolic and diastolic blood pressure, cardiac output, cardiac index, stroke volume, and heart rate). Secondly, operative details and evolution of weight and comorbidities were recorded, in terms of remission of type 2 diabetes, hypertension, hypercholesterolemia, sleep apnea, and osteoarthritis.
Primary endpoint of the study was the change in cardiac output, cardiac index, and systolic and diastolic pressure 3 months after bariatric surgery. Secondary endpoints were other hemodynamic parameters such as stroke volume and heart rate.
Statistical Analysis
Our hypothesis was that bariatric surgery gives a decrease in cardiac output and in systolic and diastolic blood pressure. In current literature, it is seen that bariatric surgery gives a mean reduction of 20% in systolic and diastolic blood pressure [3, 15].
Using a two-sided 5% significance level and a power of 90%, a power analysis indicated a sample of 50 patients. Taking into account a dropout rate of 10%, we have included 56 patients.
Continuous variables were shown as mean ± standard deviation (SD) and categorical variables as frequency with percentages. The Shapiro-Wilk test was used to test each variable for normality. Student’s t test for independent groups or the Mann-Whitney U test was used to compare the hemodynamic variables in the preoperative period, depending on the normality or non-normality of the data distribution. To determine whether the hemodynamic variables 3 months reach normal values, these follow-up values were compared with the baseline values of group B (the health professionals), assuming that these measurements would not change in 3 months. In all tests, values of p < 0.05 were considered statistically significant. Statistical Package for Social Sciences (SPSS, Chicago, IL, USA Version 20.0) was used to prepare the database and for statistical analysis.
Results
A total of 80 subjects were included in this study, respectively, 54 patients in group A and 24 healthy individuals in group B. Three months after surgery, follow-up data was available of 51 patients in group A. Three patients were unable to attend the follow-up visits at our clinic; one was admitted in a hospital because of a cerebral infarction and two patients were lost to follow-up. Table 1 gives an overview of the characteristics of each study group. A significant difference was found between group A and group B in terms of weight, waist circumference, and body mass index (BMI).
Weight Loss and Resolution of Comorbidities
Table 1 gives an overview of the weight loss profiles in group A after 3 months, the group of patients that underwent bariatric surgery. In total, 29 patients (53.7%) had a Roux-en-Y gastric bypass (RYGB); 25 (46.3%) underwent a sleeve gastrectomy (SG). In terms of resolution of comorbidities after 3 months, 15 patients (12.7%) had partial remission and 3 patients (2.5%) had complete remission of hypertension. Hypercholesterolemia resolved partially in 5 patients (4.2%) and completely in 6 patients (5.1%). Obstructive sleep apnea syndrome (OSAS) resolved partially in 7 patients (5.9%) and completely in 2 patients (1.7%). The remission of type 2 diabetes (T2DM) was partial in eight patients (6.8%) and complete in three patients (2.5%).
Baseline Cardiovascular Hemodynamic Variables
Table 2 gives an overview of the baseline hemodynamic variables between groups A and B. Between groups A and B, no significant differences were found in stroke volume (SV) and cardiac index (CI)
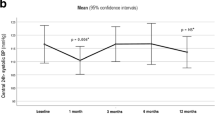
Effect of Weight Loss on Cardiovascular Hemodynamic Variables
Follow-up data of 51 patients was available (in group A). Table 3 gives an overview of the changes in cardiovascular hemodynamic variables. There were no differences between postoperative and preoperative cardiac output (CO) and cardiac index (CI) (p values, respectively, 0.082 and 0.970). Compared to group B, the postoperative hemodynamics of group A did not differ significantly from that of the healthy individuals: p = 0.586 (systolic blood pressure), 0.678 (diastolic blood pressure), 0.778 (mean arterial pressure), 0.335 (cardiac output), 0.246 (cardiac index), 0.890 (stroke volume), and 0.145 (heart rate), respectively.
We did a subgroup analysis to determine if there is a relationship between the type of bariatric surgery and the postoperative changes in cardiovascular hemodynamics. No significant differences were found between patients who underwent an SG or a RYGB of revisional surgery.
Discussion
The present study assessed the effects of bariatric surgery on cardiovascular hemodynamics 3 months after bariatric surgery. We have found that compared to healthy individuals, obese patients prior to bariatric surgery have significantly higher systolic and diastolic blood pressure, mean arterial pressure, heart rate, and cardiac output. Three months after bariatric surgery, significant improvements occur in all hemodynamic variables except cardiac output and cardiac index. Secondly, assuming that hemodynamic measurements of healthy individuals do not change over the course of 3 months, we do not see a significant difference in postoperative hemodynamics compared to healthy individuals that might be a clue that there is a normalization of hemodynamic profile after 3 months.
With respect to hemodynamic changes after bariatric surgery, conflicting results are reported in current literature. Several studies report a significant decrease in systolic and diastolic blood pressure in the first weeks after bariatric surgery, but also over longer postoperative period [16–23]. A few reports only show a significant decrease in either mean arterial blood pressure [24, 25], a long-term significant decrease in systolic blood pressure [26–29], or a significant decrease in diastolic blood pressure [30–32]. In contrast to these positive results, others show no significant changes in blood pressure after bariatric surgery [25, 27, 32–41]. This may be explained by presence of hypertension and/or a high left ventricular mass (LVM) as postulated by Mukerji et al. [42] and Alpert et al. [43]. Furthermore, a few studies found a significant short- and long-term decrease in heart rate after bariatric surgery [16, 21, 23, 25, 28–32, 35, 36, 44], while others found no differences [24, 33, 34, 37–39, 41, 42, 45]. The most intriguing fact of these results is that there must be an intrinsic morphological factor that makes the difference and explains us why these conflicting results exist. In current literature, cardiac remodeling after bariatric surgery is seen mostly in patients with hypertension, LVH, or both [43]. In our opinion, pre-existing hypertension or LVH might be prerequisite for reverse remodeling after bariatric surgery and thus the explanation for the conflicting results in current literature.
Regarding cardiac output, we hypothesized that, due to volume decrease as result of weight loss, the cardiac output would decrease 3 months after surgery. Our data suggest that a slight decrease in cardiac output occurs, although significance was not reached (p = 0.082). Moreover, in our patient population, the heart rate decreased and stroke volume increased 3 months after bariatric surgery significantly. However, there was a decreasing trend in cardiac output seen in our study, although not significant. This observation is in line with current literature, because in most of the studies, a significant decrease after 6–24 months and even after 10 years in terms of cardiac output was seen [21, 25, 28, 32, 41, 44]. These changes might indicate an improvement in relative volume overload, which can be the start of normalization of cardiac remodeling. However, the degree of remodeling in relationship with the time postoperative is not known.
The findings of cardiovascular changes after bariatric surgery are noticeable [6] and may represent a supra-physiological effect of metabolic/bariatric surgical procedures [1]. There might be a combination of weight-dependent (e.g., weight loss) and also weight-independent mechanisms (inotropic hormones, like GLP-1) that induce cardiac remodeling. This includes that there is a possibility of direct gut hormonal inotropic action on the myocardium through an enterocardiac axis [1, 6]. The classical hemodynamic weight-dependent effect of bariatric surgery is no longer thought to be the only one responsible for reverse remodeling seen after bariatric surgery, as the beneficial effects can be independent from changes in blood pressure [15, 30].
Manipulation of enteric gut hormones has been shown to have beneficial effects on cardiovascular function through the enterocardiac axis [1, 46]. Hormones such as secretin, glucagon, and vasoactive intestinal peptide act as inotropes by activating cardiac membrane adenylate cyclase, which is a key enzyme in cardiac cellular energy physiology [47]. Although these mechanisms are not fully understood, it is thought that the energy metabolism of the heart is enhanced through intermediaries of TCA cycle, cardiorenal protectivity, and caloric restriction [48].
Limitations
There are some limitations that need to be addressed. Firstly, our sample size was calculated using the difference in systolic and diastolic blood pressure, and therefore, we might have been slightly underpowered to detect a difference in cardiac output between the preoperative and the postoperative measurements. Secondly, our sample size was not suited to determine the influence of remission of comorbidities on cardiovascular hemodynamics. Finally, this study is the first to assess hemodynamic changes in bariatric patients, and since this is a pilot study, we had a short follow-up. Also, to further substantiate the findings and generalizability of the device, there should be a comparison with echocardiography findings. And if so, a control group should also be matched according to gender, age, BMI, and body surface that are to avoid bias and heterogeneity among the group of patients.
Conclusion
In summary, the aim of this study was to assess the cardiovascular and hemodynamic changes 3 months after bariatric surgery. We have found that obese patients prior to bariatric surgery have increased systolic, diastolic, and mean arterial pressure; heart rate; and cardiac output that all normalized within 3 months after bariatric surgery except cardiac output. This suggests that bariatric surgery can have beneficial effects for cardiovascular hemodynamics in the early postoperative phase.
Authors’ contributions
Initial idea and design of the study: SP, BL, SN, RB, MB.
Drafting and finalizing manuscript: SP, BL, SN, RB, MB.
Final approval: SP, BL, SN, RB, MB.
References
Ashrafian H, le Roux CW, Darzi A, et al. Effects of bariatric surgery on cardiovascular function. Circulation. 2008;118(20):2091–102. Epub 2008/11/13 doi:10.1161/circulationaha.107.721027.
Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the global burden of disease study 2013. Lancet (London, England). 2014;384(9945):766–81. Epub 2014/06/02 doi:10.1016/s0140-6736(14)60460-8.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37. Epub 2004/10/14 doi:10.1001/jama.292.14.1724.
Kasper EK, Hruban RH, Baughman KL. Cardiomyopathy of obesity: a clinicopathologic evaluation of 43 obese patients with heart failure. Am J Cardiol. 1992;70(9):921–4. Epub 1992/10/01
Adams JP, Murphy PG. Obesity in anaesthesia and intensive care. Br J Anaesth. 2000;85(1):91–108. Epub 2000/08/06
Aggarwal R, Harling L, Efthimiou E, et al. The effects of bariatric surgery on cardiac structure and function: a systematic review of cardiac imaging outcomes. Obes Surg. 2015; Epub 2015/09/04 doi:10.1007/s11695-015-1866-5.
Pritchett AM, Deswal A, Aguilar D, et al. Lifestyle modification with diet and exercise in obese patients with heart failure - a pilot study. Journal of obesity & weight loss therapy. 2012;2(2):1–8. Epub 2012/11/06 doi:10.4172/2165-7904.1000118.
von Elm E, Altman DG, Egger M, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ (Clinical research ed). 2007;335(7624):806–8. Epub 2007/10/20 doi:10.1136/bmj.39335.541782.AD.
Gizdulich P, Aschero G, Guerissi M, et al. Effects of hydrostatic pressure of finger pressure measured with Finapres. Homeostasis. 1995;36:120–9.
Gizdulich P, Imholz BP, van den Meiracker AH, et al. Finapres tracking of systolic pressure and baroreflex sensitivity improved by waveform filtering. J Hypertens. 1996;14(2):243–50. Epub 1996/02/01
Gizdulich P, Prentza A, Wesseling KH. Models of brachial to finger pulse wave distortion and pressure decrement. Cardiovasc Res. 1997;33(3):698–705. Epub 1997/03/01
Wesseling KH. A century of noninvasive arterial pressure measurement: from Marey to Penaz and Finapres. Homeostasis. 1995;36:2–3.
Wesseling KH, De Wit B, Van der Hoeven GMA, et al. Physiocal, calibrating finger vascular physiology for Finapres. Homeostasis. 1995;36:67–82.
Westerhof BE, Guelen I, Parati G, et al. Variable day/night bias in 24-h non-invasive finger pressure against intrabrachial artery pressure is removed by waveform filtering and level correction. J Hypertens. 2002;20(10):1981–6. Epub 2002/10/03
Vest AR, Heneghan HM, Agarwal S, et al. Bariatric surgery and cardiovascular outcomes: a systematic review. Heart. 2012;98(24):1763–77. Epub 2012/10/19 doi:10.1136/heartjnl-2012-301778.
Hsuan CF, Huang CK, Lin JW, et al. The effect of surgical weight reduction on left ventricular structure and function in severe obesity. Obesity (Silver Spring, Md). 2010;18(6):1188–93. Epub 2010/03/20 doi:10.1038/oby.2010.42.
Iancu ME, Copaescu C, Serban M, et al. Favorable changes in arterial elasticity, left ventricular mass, and diastolic function after significant weight loss following laparoscopic sleeve gastrectomy in obese individuals. Obes Surg. 2014;24(3):364–70. Epub 2013/10/22 doi:10.1007/s11695-013-1097-6.
Cunha Lde C, da Cunha CL, de Souza AM, et al. Evolutive echocardiographic study of the structural and functional heart alterations in obese individuals after bariatric surgery. Arq Bras Cardiol. 2006;87(5):615–22. Epub 2007/01/16
Karason K, Wallentin I, Larsson B, et al. Effects of obesity and weight loss on left ventricular mass and relative wall thickness: survey and intervention study. BMJ (Clinical research ed). 1997;315(7113):912–6.
Kokkinos A, Alexiadou K, Liaskos C, et al. Improvement in cardiovascular indices after roux-en-Y gastric bypass or sleeve gastrectomy for morbid obesity. Obes Surg. 2013;23(1):31–8. Epub 2012/08/28 doi:10.1007/s11695-012-0743-8.
Luaces M, Cachofeiro V, Garcia-Munoz-Najar A, et al. Anatomical and functional alterations of the heart in morbid obesity. Changes after bariatric surgery. Revista espanola de cardiologia (English ed). 2012;65(1):14–21. Epub 2011/10/22 doi:10.1016/j.recesp.2011.06.018.
Martin J, Bergeron S, Pibarot P, et al. Impact of bariatric surgery on N-terminal fragment of the prohormone brain natriuretic peptide and left ventricular diastolic function. The Canadian journal of cardiology. 2013;29(8):969–75. Epub 2013/02/06 doi:10.1016/j.cjca.2012.11.010.
Willens HJ, Chakko SC, Byers P, et al. Effects of weight loss after gastric bypass on right and left ventricular function assessed by tissue Doppler imaging. Am J Cardiol. 2005;95(12):1521–4. Epub 2005/06/14 doi:10.1016/j.amjcard.2005.02.029.
Alpert MA, Terry BE, Kelly DL. Effect of weight loss on cardiac chamber size, wall thickness and left ventricular function in morbid obesity. Am J Cardiol. 1985;55(6):783–6.
Di Bello V, Santini F, Di Cori A, et al. Effects of bariatric surgery on early myocardial alterations in adult severely obese subjects. Cardiology. 2008;109(4):241–8. Epub 2007/09/18 doi:10.1159/000107787.
Cavarretta E, Casella G, Cali B, et al. Cardiac remodeling in obese patients after laparoscopic sleeve gastrectomy. World J Surg. 2013;37(3):565–72. Epub 2012/12/21 doi:10.1007/s00268-012-1874-8.
Ikonomidis I, Mazarakis A, Papadopoulos C, et al. Weight loss after bariatric surgery improves aortic elastic properties and left ventricular function in individuals with morbid obesity: a 3-year follow-up study. J Hypertens. 2007;25(2):439–47. Epub 2007/01/11 doi:10.1097/HJH.0b013e3280115bfb.
Owan T, Avelar E, Morley K, et al. Favorable changes in cardiac geometry and function following gastric bypass surgery: 2-year follow-up in the Utah obesity study. J Am Coll Cardiol. 2011;57(6):732–9. Epub 2011/02/05 doi:10.1016/j.jacc.2010.10.017.
Valezi AC, Machado VH. Morphofunctional evaluation of the heart of obese patients before and after bariatric surgery. Obes Surg. 2011;21(11):1693–7. Epub 2011/05/06 doi:10.1007/s11695-011-0431-0.
Garza CA, Pellikka PA, Somers VK, et al. Structural and functional changes in left and right ventricles after major weight loss following bariatric surgery for morbid obesity. Am J Cardiol. 2010;105(4):550–6. Epub 2010/02/16 doi:10.1016/j.amjcard.2009.09.057.
Jhaveri RR, Pond KK, Hauser TH, et al. Cardiac remodeling after substantial weight loss: a prospective cardiac magnetic resonance study after bariatric surgery. Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery. 2009;5(6):648–52. Epub 2009/10/17 doi:10.1016/j.soard.2009.01.011.
Kardassis D, Bech-Hanssen O, Schonander M, et al. Impact of body composition, fat distribution and sustained weight loss on cardiac function in obesity. Int J Cardiol. 2012;159(2):128–33. Epub 2011/03/04 doi:10.1016/j.ijcard.2011.02.036.
Koshino Y, Villarraga HR, Somers VK, et al. Changes in myocardial mechanics in patients with obesity following major weight loss after bariatric surgery. Obesity (Silver Spring, Md). 2013;21(6):1111–8. Epub 2013/08/06 doi:10.1002/oby.20168.
Kanoupakis E, Michaloudis D, Fraidakis O, et al. Left ventricular function and cardiopulmonary performance following surgical treatment of morbid obesity. Obes Surg. 2001;11(5):552–8. Epub 2001/10/12 doi:10.1381/09608920160556715.
Leichman JG, Aguilar D, King TM, et al. Improvements in systemic metabolism, anthropometrics, and left ventricular geometry 3 months after bariatric surgery. Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery. 2006;2(6):592–9. Epub 2006/12/02 doi:10.1016/j.soard.2006.09.005.
Leichman JG, Wilson EB, Scarborough T, et al. Dramatic reversal of derangements in muscle metabolism and left ventricular function after bariatric surgery. Am J Med 2008;121(11):966–73. Epub 2008/10/29. doi: 10.1016/j.amjmed.2008.06.033.
Maniscalco M, Arciello A, Zedda A, et al. Right ventricular performance in severe obesity. Effect of weight loss. Eur J Clin Investig. 2007;37(4):270–5. Epub 2007/03/22 doi:10.1111/j.1365-2362.2007.01783.x.
Algahim MF, Lux TR, Leichman JG, et al. Progressive regression of left ventricular hypertrophy two years after bariatric surgery. Am J Med. 2010;123(6):549–55. Epub 2010/06/24 doi:10.1016/j.amjmed.2009.11.020.
Alpert MA, Lambert CR, Terry BE, et al. Effect of weight loss on left ventricular diastolic filling in morbid obesity. Am J Cardiol. 1995;76(16):1198–201. Epub 1995/12/01
Dzenkeviciute V, Petrulioniene Z, Sapoka V, et al. The effect of weight loss on the cardiac structure and function after laparoscopic adjustable gastric banding surgery in morbidly obese individuals. Obes Surg. 2014;24(11):1961–8. Epub 2014/05/29 doi:10.1007/s11695-014-1294-y.
Rider OJ, Francis JM, Ali MK, et al. Beneficial cardiovascular effects of bariatric surgical and dietary weight loss in obesity. J Am Coll Cardiol. 2009;54(8):718–26. Epub 2009/08/15 doi:10.1016/j.jacc.2009.02.086.
Mukerji R, Petruc M, Fresen JL, et al. Effect of weight loss after bariatric surgery on left ventricular mass and ventricular repolarization in normotensive morbidly obese patients. Am J Cardiol. 2012;110(3):415–9. Epub 2012/04/28 doi:10.1016/j.amjcard.2012.03.045.
Alpert MA, Nusair MB, Mukerji R, et al. Effect of weight loss on ventricular repolarization in normotensive severely obese patients with and without heart failure. The American journal of the medical sciences. 2015;349(1):17–23. Epub 2014/09/24 doi:10.1097/maj.0000000000000342.
Karason K, Wallentin I, Larsson B, et al. Effects of obesity and weight loss on cardiac function and valvular performance. Obes Res. 1998;6(6):422–9. Epub 1998/12/09
Lin CH, Kurup S, Herrero P, et al. Myocardial oxygen consumption change predicts left ventricular relaxation improvement in obese humans after weight loss. Obesity (Silver Spring, Md). 2011;19(9):1804–12. Epub 2011/07/09 doi:10.1038/oby.2011.186.
Ashrafian H, Athanasiou T, le Roux CW. Heart remodelling and obesity: the complexities and variation of cardiac geometry. Heart. 2011;97(3):171–2. Epub 2010/12/30 doi:10.1136/hrt.2010.207092.
Chatelain P, Robberecht P, de Neef P, et al. Low responsiveness of cardiac adenylate cyclase activity to peptide hormones in spontaneously hypertensive rats. FEBS Lett. 1979;107(1):86–90. Epub 1979/11/01
Fenske W, Athanasiou T, Harling L, et al. Obesity-related cardiorenal disease: the benefits of bariatric surgery. Nat Rev Nephrol. 2013;9(9):539–51. Epub 2013/08/07 doi:10.1038/nrneph.2013.145.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Funding
None.
Ethical Approval
“All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Animal Rights
This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Pouwels, S., Lascaris, B., Nienhuijs, S.W. et al. Short-Term Changes in Cardiovascular Hemodynamics in Response to Bariatric Surgery and Weight Loss Using the Nexfin® Non-invasive Continuous Monitoring Device: a Pilot Study. OBES SURG 27, 1835–1841 (2017). https://doi.org/10.1007/s11695-017-2564-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2564-2