Abstract
Background
Postoperative pain and analgesia present challenges in bariatric surgery patients. Multimodal analgesia may provide better efficacy, less complications and expedite fast-track bariatric surgical care. There are no studies of the broader topic of perioperative analgesia and the overall impact. This study highlights the impact of multimodal intraoperative analgesia on fast-track bariatric surgery.
Methods
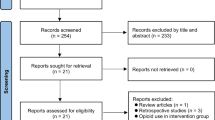
This observational study examined the perioperative outcome data of 412 consecutive laparoscopic bariatric surgery patients over a 6-year period. Perioperative outcome and variables were analysed and compared between different intraoperative analgesia types.
Results
Mean BMI was 49, mean age was 42 and male:female ratio was 1:4. About 82% of patients received multimodal intraoperative analgesia, comprising various combinations of bupivacaine infiltration and intravenous acetaminophen, morphine, tramadol, parecoxib or diclofenac. Morphine was administered in 83% of patients and tramadol in 17%. Multimodal intraoperative analgesia provided better postoperative analgesia, shorter postanaesthesia care unit (PACU) duration, lower postoperative opioid requirement, less postoperative vomiting, earlier postoperative oral intake, earlier ambulation and shorter hospital stay compared to unimodal intraoperative morphine analgesia (p = 0.0001). Multimodal analgesia comprising tramadol + acetaminophen + diclofenac provided better postoperative analgesia, shorter PACU duration, lower postoperative opioid requirement, earlier ambulation, shorter hospital stay and less postoperative hypopnoea compared to patients who received morphine (p = 0.0001).
Conclusions
Multimodal intraoperative analgesia provides better postoperative analgesia, less complications and better perioperative outcomes and facilitates fast-track bariatric surgical care. Tramadol is suitable, efficacious and safe and associated with the best perioperative outcomes in bariatric surgery patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic bariatric surgery is an effective therapy for morbid or complicated obesity, and the fast-track approach is becoming popular [1, 2]. However, there are serious perioperative challenges and factors that may hamper the perioperative outcome or recovery of bariatric surgery patients [3, 4]. Postoperative pain may be significant and has negative impact on recovery, respiration, haemodynamics, mentation, ambulation, bowel function and length of hospital stay. Also, opioid analgesia in obese patients is associated with serious adverse effects such as hypopnoea, hypoxaemia, drowsiness, ileus, vomiting, delayed ambulation and mortality [5, 6]. These complications are compounded by pre-existing obstructive sleep apnoea (OSA), cardiorespiratory insufficiency, psychiatric disorder and chronic opioid use which may be present in obese patients [7–9]. Thus, optimal perioperative, non-opioid, multimodal analgesia may expedite fast-track bariatric surgery. Few small retrospective studies of postoperative analgesia in bariatric surgery have been published [10–13]. However, there are no studies of the broader topic of perioperative analgesia and the overall impact. This large prospective study examined the overall impact of perioperative analgesia on fast-track bariatric surgical care.
Methods
This prospective observational study was approved and registered by the research department of Central Manchester University Hospital, Manchester, UK. Perioperative patient outcome data were recorded from January 2007 to January 2013. Consecutive patients underwent laparoscopic Roux-en-Y gastric bypass (LRYGB) under general anaesthesia. LRYGB was performed by two experienced surgeons, who are contemporaries and use similar surgical techniques. Surgery involved five trocar sites (three 5-mm and two 12-mm), hand-sewn gastrojejunal anastomosis and suture of all trocar sites. No concurrent or other surgery was performed. Operative time was similar for the patients, with mean duration of 100 min and median duration of 95 min.
Balanced general anaesthesia, including prophylactic anti-emetic therapy, was provided by three experienced anaesthesiologists. Supplemental intraoperative analgesia was administered based on the clinical decision and preference of each anaesthesiologist. All patients received surgical site infiltration with bupivacaine + epinephrine at the start and end of surgery. In the postanaesthesia care unit (PACU), analgesia consisted of intravenous (IV) morphine patient-controlled analgesia (PCA). On the surgical ward, analgesia comprised IV acetaminophen 1 g 6-hourly regularly and morphine PCA.
General data collected included patients’ gender, age, body mass index (BMI), comorbidities, obstructive sleep apnoea (OSA) diagnosis, American Society of Anesthesiologist (ASA) physical status, perioperative monitoring, surgery duration, perioperative complications, PACU duration, intensive care unit duration and length of hospital stay. Specific perioperative data collected included intraoperative analgesic, numeric pain score at PACU and 24 h, opioid analgesia requirement at PACU and 24 h, postoperative nausea/vomiting (PONV) and time to sustain oral drinks. Opioid requirement was measured by the dose, demand and duration of PCA used. Pain was categorized based on numeric pain score: 0 = no pain, 1–3 = mild pain, 4–6 = moderate pain and 7–10 = severe pain. Obesity was categorized based on BMI: severe obesity = 36–39.9, morbid obesity = 40–49.9 and super obesity is ≥50.
Data were analysed using SPSS® version 20 (IBM Corp., Armonk, NY, USA) and included descriptive statistics. Bivariate analysis was performed using the Student’s t test. Differences between groups were compared using the Pearson’s chi-square test or the Fisher’s exact test as appropriate. p value <0.05 was considered statistically significant.
A total of 412 consecutive patients were studied over a 6-year period. The BMI and gender distribution is shown in Table 1 with BMI range of 38–80, mean of 49 (±7), median of 48 and male:female ratio of 1:4.
All the patients were contemporaneous adults from a homogeneous population. The age range was 18–64 years, mean age was 42 (±9) years and median age was 42 years. The age distribution is shown in Table 2.
Results
Approximately 82% of patients received multimodal intraoperative analgesia, comprising IV opioid, acetaminophen, with or without non-steroidal anti-inflammatory drug (NSAID). The opioid administered in 83% of patients was morphine and tramadol in 17%. About 48.5% received morphine 0.1 mg/kg up to maximum of 20 mg + acetaminophen 2 g + parecoxib 40 mg; 17.2% received morphine 0.1 mg/kg + acetaminophen 2 g; 17% received tramadol 1.5 mg/kg up to maximum of 200 mg + acetaminophen 2 g + diclofenac 75 mg; and 17.2% received morphine 0.1 mg/kg (Table 3).
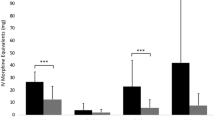
Postoperative Pain & Duration in PACU
Pain assessment in PACU showed that 4% had severe pain, 7% had moderate pain and 63% had mild pain (Table 4). However, 26% had no pain; this group comprised all patients who received tramadol + acetaminophen + diclofenac (65% of pain-free patients) and some patients who received morphine + acetaminophen + parecoxib (35% of pain-free patients). In the PACU, 26% of patients did not use any analgesia; this group comprised all the patients who received tramadol + acetaminophen + diclofenac (65%) and some patients who received morphine + acetaminophen + parecoxib (35%). Multimodal intraoperative analgesia provided lower PACU pain scores compared to unimodal intraoperative morphine analgesia (p = 0.0001). Multimodal analgesia comprising tramadol + acetaminophen + diclofenac provided lower PACU pain scores than other multimodal analgesia regimens (p = 0.0001).
PACU duration was categorized as short ≤50 min, medium = 51-100 min, long = 101–150 min and longest ≥ 151 min. PACU duration varied with intraoperative analgesia type, as shown in Table 5. Approximately 67% of patients spent short duration in PACU; this group mainly comprised patients who received multimodal analgesia, and they had shorter PACU duration than patients who received unimodal morphine analgesia (p = 0.01). Multimodal intraoperative analgesia comprising tramadol + acetaminophen + diclofenac was associated with shorter PACU duration compared to other analgesia types (p = 0.001).
Postoperative Pain and Analgesia Requirement at 24 h
Patients had lower pain scores at 24 h compared to PACU (p = 0.001). Pain assessment at 24 h showed that 1.5% had severe pain, 5.6% had moderate pain, 68.9% had mild pain and 24% had no pain (Table 6). The pain-free group comprised all the patients who received tramadol + acetaminophen + diclofenac (74% of pain-free patients) and some patients who received morphine + acetaminophen + parecoxib (26% of pain-free patients). Patients who received multimodal intraoperative analgesia had lower pain scores at 24 h compared to patients who received unimodal morphine analgesia (p = 0.002). Analgesia usage at 24 h showed that 24% did not use the PCA which was provided, 73% discontinued PCA on the first postoperative day and 3% discontinued PCA on the second day. Patients who did not use PCA comprised those who received tramadol + acetaminophen + diclofenac (74%) and some patients who received morphine + acetaminophen + parecoxib (26%). Patients who received multimodal intraoperative triple analgesia had lower pain scores at 24 h and shorter use of PCA compared to other patients (0.002).
Postoperative Oral Intake and PONV
PONV occurred in 19.2% of patients and varied with intraoperative analgesia type (Table 7). Patients who received unimodal intraoperative morphine analgesia comprised 33% of PONV cases. Multimodal intraoperative analgesia was associated with lower PONV rates compared to unimodal morphine analgesia (p = 0.001).
About 90% of patients had sustained oral drinks postoperatively on the day of surgery (day 0), and this varied with intraoperative analgesia type (Table 8). Patients who received multimodal intraoperative triple analgesia had earlier and better sustained postoperative oral drinks than other patients (0.004).
Postoperative Respiratory Complications
About 1.7% of patients had early postoperative hypopnoea which required respiratory support with mask-CPAP (continuous positive airway pressure); and 0.4% of patients required supplemental nasal oxygen after 24 h (Table 9). There was no significant association between postoperative respiratory dysfunction and intraoperative analgesia type (p = 0.9). Half of the patients with respiratory dysfunction were successfully treated with single dose of IV doxapram 75–100 mg, which enabled prompt recovery and discharge. Compared to patients who received intraoperative tramadol, patients who received intraoperative morphine had significantly higher rates of postoperative doxapram therapy (p = 0.04).
Length of Hospital Stay
Majority of patients (59%) were discharged home at 24 h. Length of hospital stay was associated with intraoperative analgesia type (Table 10). Multimodal intraoperative analgesia comprising tramadol + acetaminophen + diclofenac was associated with earlier ambulation and shorter hospital stay than other analgesia types (p = 0.01).
Discussion
Postoperative pain and analgesia are associated with challenges in bariatric surgery patients [3, 6, 8, 9]. Multimodal analgesia has better efficacy and less complications [11–14]. About 82% of patients in our study received multimodal intraoperative analgesia, which enhanced their overall good perioperative outcome. It was associated with better postoperative analgesia, shorter PACU duration and lower postoperative opioid requirement. This confirms that multimodal analgesia is beneficial and essential in bariatric surgery patients and corroborates other studies [11–14]. Our study demonstrated that multimodal analgesia is associated with less PONV, earlier postoperative oral intake, earlier ambulation and shorter hospital stay, and these are highly essential factors for fast-track or enhanced recovery bariatric surgical care. Our study also highlights the economic benefits of multimodal analgesia with shorter PACU duration, lower postoperative opioid requirement, earlier ambulation and shorter hospital stay.
Multimodal analgesia involves the simultaneous use of different analgesics that act via different physiologic processes to produce effective synergistic analgesia with less complications. In our study, it involved various combinations of intraoperative bupivacaine infiltration and IV acetaminophen, morphine, tramadol, parecoxib or diclofenac. Bupivacaine is a local anaesthetic which temporarily blocks neurotransmission, thereby providing analgesia for 4–8 h. Every patient in our study received bupivacaine infiltration, which contributed to multimodal analgesia, and this corroborates other studies [10, 15, 16].
Morphine is an efficacious opioid analgesic but is associated with significant adverse effects including airway or respiratory compromise, which may be severe in bariatric patients [3, 6, 9, 11, 12]. About 83% of our patients received intraoperative morphine, which provided good analgesia especially as part of multimodal analgesia, but was associated with postoperative hypopnoea. Our study confirms that morphine-related hypopnoea may be significant in bariatric patients but can be treated with the analeptic doxapram, and this corroborates a previous study [9]. Postoperative morphine was administered in the form of PCA, which afforded smaller doses and less complications, and contributed to lower pain scores at 24 h.
Tramadol is a synthetic analgesic with opioid, noradrenergic and serotoninergic effects. Its opioid and non-opioid analgesic effects are synergistic, thereby producing effective analgesia and minimal serious side-effects [17]. About 17% of our patients received intraoperative tramadol, and they had better postoperative analgesia, shorter PACU duration, less postoperative opioid requirement, earlier ambulation, shorter hospital stay, less postoperative hypopnoea and less doxapram requirement compared to patients who received morphine. These are very positive and essential perioperative outcome measures in bariatric patients. Our study is the first to highlight that tramadol analgesia is most suitable, efficacious, safe and associated with the best perioperative outcomes in bariatric patients. The main side-effect of tramadol is vomiting, but our study showed that this can be effectively prevented by pre-emptive multimodal anti-emetic therapy [17].
Acetaminophen is an analgesic with opioid-sparing activity but has rare adverse effects [11–13, 18]. It is an essential component of multimodal perioperative analgesia and was used in every case of multimodal analgesia in our study. Our study confirms that multimodal analgesia involving acetaminophen, reduces opioid requirement and side-effects but without acetaminophen-related adverse effects as indicated in other studies [11–13, 18].
Diclofenac and parecoxib are non-steroidal anti-inflammatory drugs (NSAID) and opioid-sparing analgesics with few adverse effects [12, 16, 19–21]. Two thirds of patients in our study received NSAID, which enhanced multimodal analgesia. Our study confirms that multimodal analgesia involving NSAID, reduces opioid requirement and side-effects but without NSAID-related adverse effect as shown in other studies [12, 16, 19–21].
Our study is a reliable prospective observational clinical research with good sample size and valid results. However, it is limited by the time-consuming consecutive sample of patients. A larger sample size may probably reveal more perioperative complications. Further larger studies would be interesting, and should focus on pain-related and analgesia-related perioperative complications in bariatric surgery patients.
Conclusion
Postoperative pain and analgesia pose peculiar challenges in bariatric surgery patients. However, multimodal intraoperative analgesia is a good foundation towards optimal postoperative analgesia. Multimodal intraoperative analgesia provides better postoperative analgesia, less complications and better perioperative outcomes and facilitates fast-track perioperative care. Tramadol is suitable, efficacious, safe and associated with the best perioperative outcomes in bariatric surgery patients.
References
Bamgbade OA, Adeogun BO, Abbas K. Fast-track laparoscopic gastric bypass surgery: outcomes and lessons from a bariatric surgery service in the United Kingdom. Obes Surg. 2012;22(3):398–402.
Dogan K, Kraaij L, Aarts EO, et al. Fast-track bariatric surgery improves perioperative care and logistics compared to conventional care. Obes Surg. 2015;25(1):28–35.
Bamgbade OA, Rutter TW, Nafiu OO, et al. Postoperative complications in obese and nonobese patients. World J Surg. 2007;31(3):556–60.
Lemanu DP, Srinivasa S, Singh PP, et al. Optimizing perioperative care in bariatric surgery patients. Obes Surg. 2012;22(6):979–90.
Bamgbade OA, Alfa JA. Dexmedetomidine anaesthesia for patients with obstructive sleep apnoea undergoing bariatric surgery. Eur J Anaesthesiol. 2009;26(2):176–7.
Lloret-Linares C, Lopes A, Declèves X, et al. Challenges in the optimisation of post-operative pain management with opioids in obese patients: a literature review. Obes Surg. 2013;23(9):1458–75.
Bamgbade OA, Chung AS, Khalaf WM, et al. Survey of perioperative care of adults with obstructive sleep apnoea. Eur J Anaesthesiol. 2009;26(8):706–8.
Weingarten TN, Sprung J, Flores A, et al. Opioid requirements after laparoscopic bariatric surgery. Obes Surg. 2011;21(9):1407–12.
Bamgbade OA. Advantages of doxapram for post-anaesthesia recovery and outcomes in bariatric surgery patients with obstructive sleep apnoea. Eur J Anaesthesiol. 2011;28(5):387–8.
Moncada R, Martinaitis L, Landecho M, et al. Does preincisional infiltration with bupivacaine reduce postoperative pain in laparoscopic bariatric surgery? Obes Surg. 2016;26(2):282–8.
Song K, Melroy MJ, Whipple OC. Optimizing multimodal analgesia with intravenous acetaminophen and opioids in postoperative bariatric patients. Pharmacotherapy. 2014;34(Suppl 1):14S–21S.
Ziemann-Gimmel P, Hensel P, Koppman J, et al. Multimodal analgesia reduces narcotic requirements and antiemetic rescue medication in laparoscopic Roux-en-Y gastric bypass surgery. Surg Obes Relat Dis. 2013;9(6):975–80.
Gonzalez AM, Romero RJ, Ojeda-Vaz MM, et al. Intravenous acetaminophen in bariatric surgery: effects on opioid requirements. J Surg Res. 2015;195(1):99–104.
Lam KK, Mui WL. Multimodal analgesia model to achieve low postoperative opioid requirement following bariatric surgery. Hong Kong Med J. 2016;22(5):428–34.
Ruiz-Tovar J, Muñoz JL, Gonzalez J, et al. Postoperative pain after laparoscopic sleeve gastrectomy: comparison of three analgesic schemes (isolated intravenous analgesia, epidural analgesia associated with intravenous analgesia and port-sites infiltration with bupivacaine associated with intravenous analgesia). Surg Endosc. 2017;31(1):231–6.
Schumann R. Anaesthesia for bariatric surgery. Best Pract Res Clin Anaesth. 2011;25(1):83–93.
Lehmann KA. Tramadol in acute pain. Drugs. 1997;53(Suppl 2):25–33.
Saurabh S, Smith JK, Pedersen M, et al. Scheduled intravenous acetaminophen reduces postoperative narcotic analgesic demand & requirement after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2015;11(2):424–30.
El-Shobary H, Christou N, Backman SB, et al. Effect of laparoscopic versus open gastric bypass surgery on postoperative pain and bowel function. Obes Surg. 2006;16(4):437–42.
Govindarajan R, Ghosh B, Sathyamoorthy MK, et al. Efficacy of ketorolac in lieu of narcotics in the operative management of laparoscopic surgery for morbid obesity. Surg Obes Relat Dis. 2005;1(6):530–5. discussion 535-536
Kamelgard JI, Kim KA, Atlas G. Combined preemptive and preventive analgesia in morbidly obese patients undergoing open gastric bypass: a pilot study. Surg Obes Relat Dis. 2005;1(1):12–6.
Acknowledgements
This study was approved and registered by the research department of Central Manchester University Hospital, Manchester, UK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Institutional support is acknowledged, but there was no conflict of interest or financial involvement regarding any of the authors. The first author has no conflict of interest. The second author has no conflict of interest. The third author has no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human Rights
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Bamgbade, O.A., Oluwole, O. & Khaw, R.R. Perioperative Analgesia for Fast-Track Laparoscopic Bariatric Surgery. OBES SURG 27, 1828–1834 (2017). https://doi.org/10.1007/s11695-017-2562-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2562-4