Abstract
Background
The feasibility of a side-to-side jejunoileal anastomosis (SJA) to control type 2 diabetes mellitus (T2DM) was studied in non-obese diabetic Goto–Kakizaki (GK) rats.
Methods
Seventeen 14-week-old male GK rats were divided into three groups: SJA bypassing 60 % of the small bowel length, sham-operated jejunoileal bypass (Sham group), and control animals. Rats were observed for 10 weeks after surgery. Fasting blood glucose (FBG) levels and oral glucose tolerance test (OGTT) were measured before and after the procedure.
Results
Animals with SJA exhibited normalization of FBG levels from the 1st and up to the 10th postoperative week when the experiment terminated. OGTT compared with sham-operated and control groups was also significantly better at 3 and 8 weeks postoperatively.
Conclusions
A simple SJA, diverting the food and biliopancreatic secretion to the distal small bowel, was able to normalize both FBG levels and OGTT in a non-obese diabetic rat model.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical treatment of type 2 diabetes mellitus has been discussed during the Diabetes Surgery Summit Consensus conference in Rome. It was agreed that bariatric procedures are able to induce long-term remission of type 2 diabetes mellitus (T2DM) in morbidly obese patients [1] and that best results are obtained from those operations that are diverting food and biliopancreatic secretions to the distal small bowel, such as the gastric bypass [2] and the biliopancreatic diversion [3]. At this historical meeting, the need of new metabolic procedures focused on the management of diabetes was also stressed [4]. Since then, a number of new operations have been developed and utilized in obese and non-obese diabetic patients, under strict ethical considerations [5–7]. Such operations are still considered investigational and should be very cautiously applied on diabetic patients.
For enhancing weight loss in morbidly obese patients, the addition of a side-to-side jejunoileal anastomosis to sleeve gastrectomy has previously been described from our group [8]. The very successful results in diabetic remission, observed following this procedure in morbidly obese diabetic patients, lead us to the assumption that diverting and accelerating the food transmission into the distal small bowel with a simple jejunoileal anastomosis, in non-obese diabetic patients where weight loss is not the main goal, will act therapeutically by stimulating the L cells of the ileum for incretins production. Therefore, side-to-side jejunoileal anastomosis (SJA) was performed in Goto–Kakizaki (GK) rats in order to determine whether this food-diverting procedure is able to induce diabetes control in a non-obese animal model and establish a suitable experimental setting for further studies of the mechanism/s for diabetes control.
Experimental Materials and Methods
Animals and Diets
Nine to 10 week-old male diabetic, normolipidemic GK rats were purchased from “Charles River” Research Models and Services (Boston, USA). All animals were housed in individual cages under standard conditions (constant ambient temperature of 22 °C and humidity of 60 % in a 12-h light/dark cycle) in the animal house, Heraklion University Hospital, with free access to water. Animals were fed with a 2 % fat and 16.5 % protein rat chow diet (Kounker, Athens, Greece) before operation. The animal experiment in this study was approved by the Ethics Committee of the Medical School, University of Crete, and received permission from Heraklion Regional Veterinary Service. All applicable institutional and/or national guidelines for the care and use of animals were followed.
Experimental Design
Rats were allowed 4 weeks for acclimation before the experiment. After that, 17 rats randomly underwent one of the following procedures: SJA, 11 animals; sham side-to-side jejunoileal anastomosis (SSJA): 4 animals; or no intervention (controls): 2 animals. Weight, fasting glucose, cholesterol, triglycerides, and oral glucose tolerance test (OGTT) were measured at intervals according to the experimental schedule.
The operative times (time from the beginning of the midline abdominal incision to the end of suturing of the abdominal incision) of SJA and SSJA groups were accurately recorded. Moreover, the time of first postoperative defecation (an indicator of postoperative recovery time) and all postoperative complications were extensively recorded.
Surgical Techniques
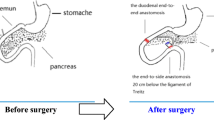
Before operations, rats were fasted overnight for 12 h. Rats were anesthetized with ketamine hydrochloride 50 mg/ml (Molteni Farmaceutical, Firenze, Italy) during the surgery. SJA procedure (Fig. 1) involved (1) a 4-cm midline abdominal incision, (2) measurement of the length of the entire small intestine from the Treitz ligament to the ileocecal valve, (3) estimation of the length of small bowel equal to 20 % of its entire length, (4) identification of a point distal to the Treitz ligament at a distance equal with 20 % of the total bowel length, (5) identification of a point proximal to the Ileocecal valve at a distance equal with 20 % of the total bowel length, (6) side-to-side anastomosis between jejunum and ileum at the measured points distal to the Treitz and proximal to the ileocecal valve using 6–0 polydioxanone monofilament absorbable sutures (PDS; Johnson and Johnson, USA), (7) closure of the abdominal incision using 4–0 polyglycolic acid absorbable sutures (Safil Braun, Tuttlingen Germany), and (8) closure of the skin incision with subcuticular suture with the same suturing material.
Sham operations were performed by the same abdominal incisions and same jejunoileal anastomosis. Thereafter, the anastomosis was taken down with restoration of the small bowel continuity using 6–0 PDS sutures.
Rats had free access to water 2 h after surgery as well as free access to food 24 h postoperatively. Food intake was not limited. Both groups were fed the same perioperative diet. Weight was measured every 7 days until the 10th week when the study was terminated.
Biochemical Tests
Blood glucose, cholesterol, and triglycerides were measured using a quantitative instrument (Accutrend Plus, Roche Diagnostic, Mannheim, Germany). Before operation and every week postoperatively, from the 1st until the 10th when the experiment was terminated, blood samples were collected after 12 h overnight fast from the tail’s vein of conscious rats, for measuring of serum glucose levels. Cholesterol and triglyceride levels were measured before operation and at the third and the eighth postoperative weeks. OGTT was performed preoperatively and at 3 and 8 weeks after surgery. After an overnight fast, rats were administrated with 1 g/kg glucose by oral gavage and blood glucose levels were measured before, 30, 60, and 120 min after the oral gavage.
Statistical Analysis
All statistical analyses were performed with SPSS 17.0. Data was expressed as median and range. All p values are two-tailed. Because of the small animal numbers in the three groups, data were compared using non-parametric tests for different population. Mann–Whitney U tests were used for comparisons between groups and Wilcoxon paired test for intra-group comparisons. p < 0.05 was considered statistically significant.
Results
Operation Time, Postoperative Recovery Time, and Postoperative Complications
All operations were successful. However, compared with SJA, the operation time 47.5 min (range 25–60 min) vs 89.5 min (range 45–105 min) of SSJA was longer (p < 0.01). There was no significant (NS) differences in postoperative recovery time for SJA, 2 days (range 1–3 days) vs SSJA, 2 days (range 1–2 days) (p = 0.9). One SJA rat died from intestinal obstruction, due to torsion of the anastomosis along the longitudinal axis, at day 32 after the operation. Neither deaths nor complications were observed in the sham-operated and control groups.
Small Bowel Lengths
At 14 week, the measured average intestinal length of SJA animals from Treitz ligament to the ileocecal valve was 89 cm (range 70–118 cm) and for SSJA animals 84 cm (range 65–95 cm) (p = 0.57 NS).
Weight and Postoperative Weight Loss
At week 0, the median weight for the three groups was as follows: SJA 358 g (range 354–366 g), SSJA 355.5 g (range 345–360 g), and controls 360 g (range 355–365 g). The p values for the differences between groups were SJA vs Sham SJA p = 0.32, SJA vs controls p = 0.9, and SSJA vs controls p = 0.36, all NS.
Animals in SJA group experienced loss of weight from the first and up to 4 weeks after the operation. The median %TWL observed at that time point was 7.2 %. The weight of the rats in this group was stabilized thereafter but remained reduced comparing with the pre-operative values (p < 0.001) until the end of the experiment (Fig. 2).
Glucose Metabolism
Glucose
Animals in the control group and those in SJA and SSJA groups have no statistically different fasting glucose levels before the procedures. SJA: median 213.5 mg/dl (range 181–260), controls: median 308 mg/dl (range 280–336), and Sham: median 235 mg/dl (range 219–248). SJA vs Sham p = 0.4 NS, SJA vs controls p = 0.062 NS, and Sham vs controls p = 0.074 NS.
However, compared with sham-operated rats and controls, the fasting glucose levels were significantly lower in the SJA group (p < 0.01) from the 1st postoperative week and continued to be within normal range up to the 10th week when the experiment was terminated (Fig. 3).
Fasting serum glucose levels in SJA and SSJA animals before and after surgery and in the control group. Fasting serum glucose levels in SJA animals were significantly reduced (p < 0.01) during the whole post-operative period (7–70 days). Animals in Sham and control groups had no significant changes in fasting serum glucose levels
OGTT
Prior to the procedures, no statistical difference in OGTT was found among all experimental groups. At 120 min following administration of 1 g/kg glucose by oral gavage, the median plasma glucose levels were 301.5 mg/dl (range 261–480 mg/dl) for SJA, 409 mg/dl (range 327–439 mg/dl) for Sham group, and 378 mg/dl (range 300–457 mg/dl) for the control group. SJA vs Sham p = 0.076 NS, SJA vs control p = 0.052 NS, and Sham vs control p = 1.00 NS.
However, all rats in the side-to-side jejunoileal bypass group showed a significant improvement in glucose tolerance test at 120 min following administration of 1 g/kg glucose by oral gavage at 3 and 8 weeks postoperatively [273.5 (57–382) mg/dl; p = 0.02 and 95.5 (70–241) mg/dl; p = 0.005, respectively]. On the contrary, no significant changes were observed either in Sham [414 (188–510) mg/dl; p = 0.72 NS and 414 (188–510) mg/dl; p = 0.07 NS, respectively] or in the control [383 (346–420) mg/dl; p = 0.66 NS and 457.5 (400–515) mg/dl; p = 0.18 NS, respectively] groups (Fig. 4).
Oral glucose tolerance test, after administration of 1 g/kg glucose by oral gavage. The SJA group had a significant reduction of serum glucose levels 120 min after the gavage, at 21 days (p < 0.05) and 56 days (p < 0.01) post-operatively. In Sham and control groups, no significant changes were observed
Cholesterol and Triglycerides Levels
Serum cholesterol and triglycerides levels had no difference prior to surgery among all experimental groups. No significant differences in those parameters were observed following SJA or Sham procedures.
Discussion
This experiment study on a non-obese diabetic rat model showed that by diverting food and biliopancreatic secretion to the distal small bowel, by a simple jejunoileal anastomosis, glucose homeostasis is restored. Many pathophysiological mechanisms may be contributing to diabetes remission observed in this non-obese rat model. It is noticeable that none of the animals in this study developed diarrhea or other symptoms and signs of malabsorption, following this procedure. However, even without sleeve gastrectomy, simple jejunoileal anastomosis resulted in minimal weight loss. In the animal model following bypass of 60 % of the small bowel length, %TWL of 7.2 % were observed the first 4 postoperative weeks, followed by weight stabilization.
Nevertheless, the weight loss seen postoperatively in the animals can be explained by the fast transmission of food in the distal small bowel and the release of incretins which are known to result into satiety signals and therefore in reduction of calorie intake [9–11]. To test this hypothesis, further studies are in progress in our institution.
Although there is no question that durable weight loss improves insulin sensitivity which contributes to diabetes control [12], the weight loss observed in the SJA animals cannot fully explain the rapid remission of diabetes. Other mechanisms are very likely to be responsible for diabetes control, following side-to-side jejunoileal bypass. Our previous studies showed a positive effect in glucose homeostasis following operation with fast transmission of the food into the distal gut, such as the sleeve gastrectomy [9, 13]. The present study suggests that the effective improvement of T2DM at early stage after the SJA is mediated by rapid improvement in insulin sensitivity independent of weight loss [4, 8, 14]. It can be speculated that the GLP-1 and PYY released from the gut is the possible mechanism for diabetes control, apart from the weight loss that occurred postoperatively [9, 10].
Four possible anti-diabetic theories have been developed to explain the postoperative diabetes remission: (a) the weight loss hypothesis [12], (b) the ghrelin hypothesis [15], (c) the foregut hypothesis [16], and (d) the hindgut hypothesis [17].
Weight loss was observed in our study in the SJA animals. Although the loss of weight was not extensive and up to 7.2 % in rats, this may play a role in diabetes remission. Nevertheless, it has been proven that weight loss after surgery plays an important role in the long-term improvement of glucose homeostasis [10, 12]. However, control of glucose homeostasis was evident from the early postoperative period and before substantial weight loss in our patients and in the experimental animals, suggesting that other mechanisms are significantly contributing in diabetic control [9, 18, 19].
The stomach was not altered with this operation; therefore, the ghrelin theory cannot be confirmed from this study. Our findings do not support the foregut hypothesis, since the proximal jejunum remained intact and food was getting in contact with the bowel mucosa.
Our findings might well be explained by the hindgut hypothesis, from the rapid delivery of nutrients to the distal bowel, where the vast majority of the L cells which are producing incretines such as GLP-1 and PYY [9, 18, 19].
Those enteropeptides are considered as extremely important parameters for long-term remission of diabetes by reducing appetite, improving insulin sensitivity, inhibiting pancreatic β-cells apoptosis, and stimulating proliferation and differentiation of insulin secreting β-cells. Additionally, GLP-1 inhibits gastric secretion and motility. This delays and protracts carbohydrate absorption and contributes to a satiating effect [20, 21]. Thus, GLP-1 is now being used in the clinic to improve glucose tolerance and control T2DM [20].
Finally, following SJA in rats, cholesterol and triglyceride levels remained unchanged until postoperative day 56. Longer follow-up period is required to investigate if any change in lipids profile will be statistically evidenced in this normolipidemic animal model. As shown in dyslipidemic diabetic patients, a period of several years is necessary following control of the disease, to normalize the lipid profile [22].
We used Goto–Kakizaki rats, a non-obese effective and economical diabetic experimental model [21, 23], in order to investigate the safety of SJA and its effectiveness on diabetes control. To our knowledge, studies on the effects of this novel operation in animals or in non-morbidly obese diabetic patients have not been reported.
This procedure diverts food and biliopancreatic secretion to the distal gut bypassing a significant part of the small intestine. Although there is no blind bowel loop after SJA, the possibility of unpleasant pathophysiological consequences should not be overlooked or underestimated. Micronutrient and macronutrient deficiencies particularly for iron, zinc, vitamins B and D, calcium, and albumins can be manifested in the early or late postoperative period [24, 25]. Bile salt diversion may lead to malabsorption and diarrhea, improper balance of intestinal bacteria, and alteration of microbiota [26, 27]. The possibility of small bowel bacteria overgrowth syndrome due to the anatomical disturbance of the gut should also kept in mind [28, 29]. This experimental study was not designed to investigate the above possible side effects. In fact, during the 10 weeks postoperative period of animal’s observation, none of the rats developed any suspicious sign or symptom such as diarrhea, loss of appetite, edema, abdominal distension, etc.
One animal died from intestinal obstruction in 32nd postoperative day. Although in the rats no mesenteric defect management to prevent this complication was undertaken, if this operation would be implemented in humans, closure of the mesenteric defect below the distal loop is absolutely necessary, as we have learned from the implementation of this procedure, with sleeve gastrectomy, in morbidly obese patients.
This experimental research is an interventional before and after study and has a limitation. The comparisons with the sham group and the control group are simply indicative and confirmatory of the main goal which is largely the outcome after the intervention. Therefore, the results of the comparison among the three different groups must interpret with caution because of the small-sized groups.
In conclusion, simple side-to-side jejunoileal anastomosis, bypassing a large part of the mid small bowel for T2DM control, is reported for the first time in experimental animals. Experimental results and preliminary data from the implementation of this new procedure are encouraging. Further studies are in progress in our institution in diabetic rats and diabetic patients with BMI 25–35 kg/m2, in order to further evaluate the safeness and effectiveness of this novel procedure.
References
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370(21):2002–13.
De Sa VC, Ferraz AA, Campos JM, et al. Gastric bypass in the treatment of type 2 diabetes in patients with a BMI of 30 to 35 kg/m2. Obes Surg. 2011;21(3):283–7.
Scopinaro N, Papadia F, Marinari G, et al. Long-term control of type 2 diabetes mellitus and the other major components of the metabolic syndrome after biliopancreatic diversion in patients with BMI < 35 kg/m2. Obes Surg. 2007;17(2):185–92.
Rubino F, Kaplan LM, Schauer PR, et al. The Diabetes Surgery Summit Consensus conference recommendations for the evaluation and use of gastrointestinal surgery to treat type 2 diabetes mellitus. Ann Surg. 2010;251(3):399–405.
Cohen RV, Schiavon CA, Pinheiro JS, et al. Duodenal-jejunal bypass for the treatment of type 2 diabetes in patients with body mass index of 22–34 kg/m2: a report of 2 cases. Surg Obes Relat Dis. 2007;3(2):195–7.
De Paula AL, Stival AR, Halpern A, et al. Improvement in insulin sensitivity and β-cell function following ileal interposition with sleeve gastrectomy in type 2 diabetic patients: potential mechanisms. J Gastrointest Surg. 2011;15(8):1344–53.
Santoro S, Castro LC, Velhote MC, et al. Sleeve gastrectomy with transit bipartition: a potent for metabolic syndrome and obesity. Ann Surg. 2012;256(1):104–10.
Melissas J, Peppe A, Askoxilakis J, et al. Sleeve gastrectomy plus side-to-side jejunoileal anastomosis for the treatment of morbid obesity and metabolic diseases: a promising operation. Obes Surg. 2012;22(7):1104–9.
Dimitriadis E, Daskalakis M, Kampa M, et al. Alterations in gut hormones after laparoscopic sleeve gastrectomy: a prospective clinical and laboratory investigational study. Ann Surg. 2013;257(4):647–54.
Peterli R, Wölnerhanssen B, Peters T, et al. Improvement in glucose metabolism after bariatric surgery: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: a prospective randomized trial. Ann Surg. 2009;250(2):234–41.
De Silva A, Bloom SR. Gut hormones and appetite control: a focus on PYY and GLP-1 as therapeutic targets in obesity. Gut Liver. 2012;6(1):10–20.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248–56.
Melissas J, Daskalakis M, Koukouraki S, Dimitriadis E, et al. Sleeve gastrectomy—a “food limiting” operation. Obes Surg. 2008;18(10):1251–6.
Melissas J, Leventi A, Klinaki I, et al. Alterations of global gastrointestinal motility after sleeve gastrectomy: a prospective study. Ann Surg. 2013;258(6):976–82.
Bohdjalian A, Langer FB, Shakeri-Leidenmühler S, et al. Sleeve gastrectomy as sole and definite bariatric procedure: 5-year results for weight loss and ghrelin. Obes Surg. 2010;20(5):535–40.
Rubino F, Forgione A, Cummings DE, et al. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology type 2 diabetes. Ann Surg. 2006;244(5):741–9.
Mingrone G. Role of the incretin system in the remission of type 2 diabetes following bariatric surgery. Nutr Metab Cardiovasc Dis. 2008;18(8):574–9.
Bikman BT, Zheng D, Pories WJ, et al. Mechanism for improved insulin sensitivity after gastric bypass surgery. J Clin Endocrinol Metab. 2008;93(12):4656–63.
Chambers AP, Jessen L, Ryan KK, et al. Weight-independent changes in blood glucose homeostasis after gastric bypass or vertical sleeve gastrectomy in rats. Gastroenterology. 2011;141(3):950–8.
Amori RE, Lau J, Pittas AG. Efficacy and safety of incretin therapy in type 2 diabetes: systematic review and meta-analysis. JAMA. 2007;298(2):194–206.
Sun D, Liu S, Zhang G, et al. Type 2 diabetes control in a nonobese rat model using sleeve gastrectomy with duodenal-jejunal bypass (SGDJB). Obes Surg. 2012;22(12):1865–73.
Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–59.
Akash MS, Rehman K, Chen S. Goto–Kakizaki rats: its suitability as non-obese diabetic animal model for spontaneous type 2 diabetes mellitus. Curr Diabetes Rev. 2013;9(5):387–96.
Stein J, Stier C, Raab H, et al. Review article: The nutritional and pharmacological consequences of obesity surgery. Aliment Pharmacol Ther. 2014;40(6):582–609.
Topart P, Becouam G, Salle A, et al. Biliopancreatic diversion requires multiple vitamin and micronutrient adjustments within 2 years of surgery. Surg Obes Relat Dis. 2014;10(5):936–41.
Penney NC, Kinross JM, Newton RC, Purkayastha S. The role of bile acids in reducing the metabolic complications of obesity after bariatric surgery: a systematic review. Int J Obes (Lond) 2015 Jun 17 doi: 10.1038/ijo.2015.115
Damms-Machado A, Mitra S, Schollenberger AE, Kramer KM, Meile T, Konigsrainer A et al. Effect of surgical and dietary weight loss therapy for obesity in gut microbiota composition and nutrient absorption. Biomed Res Int 2015:806248 doi: 10.1155/2015/806248
Lakhani SV, Shah HN, Alexander K, et al. Small intestinal bacterial overgrowth and thiamine deficiency after Roux-en-Y gastric bypass in obese patients. Nutr Res. 2008;28(5):293–8.
Ishida RK, Faintuch J, Paula AM, et al. Microbial flora of the stomach after gastric bypass for morbid obesity. Obes Surg. 2007;17(6):752–8.
Conflict of Interest
The authors declare that they have no competing interests.
Compliance with Ethical Standards
All applicable institutional and/or national guidelines for the care and use of animals were followed. This article does not contain any studies with human participants.
Informed Consent
Informed consent is not applicable in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
John Melissas and Drakos Peirasmakis contributed equally to this work.
Rights and permissions
About this article
Cite this article
Melissas, J., Peirasmakis, D., Lamprou, V. et al. Is a Simple Food-Diverting Operation the Solution for Type 2 Diabetes Treatment? Experimental Study in a Non-Obese Rat Model. OBES SURG 26, 1010–1015 (2016). https://doi.org/10.1007/s11695-015-1871-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1871-8