Abstract
Introduction
Most papers discussing specifics of reoperative surgery after laparoscopic Roux-en-Y gastric bypass (LRYGB) are over 10 years old.
Methods
A retrospective analysis of patients undergoing reoperative surgery within 30 days of LRYGB.
Results
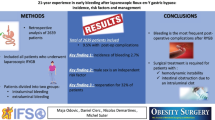
Over a 5-year period, 52 out of 1769 (2.9 %) patients underwent reoperation within 30 days of the index LRYGB. The 30-day reoperative surgery rate was 2.5 % for primary and 7.1 % for revisional LRYGB. The most common indications for reoperation included bleeding (n = 16), followed by bowel obstruction (n = 14), leak (n = 14), and diagnostic exploration for tachycardia and abdominal pain (n = 4). Forty-nine (94 %) reoperations were started laparoscopically and six (12 %) required conversion to laparotomy. The most common sources of bleeding were the mesenteric vessels (n = 6); the most common cause of obstruction was adhesion (n = 5), and the most common site of leak was the gastric pouch and gastrojejunal anastomosis (n = 9). Twenty (38 %) patients developed further complications that led to a third surgery in nine (17 %) patients. There were no significant differences as far cause for reoperation noted between patients undergoing primary surgery versus revisional surgery. The 90-day readmission and mortality rates were 29 % and zero, respectively.
Conclusion
Type of complications is comparable, and number of complications requiring early surgical reintervention following primary or revisional LRYGB is low. Increasing proportion of patients requiring early reoperation will have undergone a revisional surgery. The majority of these reoperations are accomplished laparoscopically. Bleeding continues to be the most common cause for early reoperation. Although associated with significant morbidity, mortalityis rare in this patient population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent studies have shown markedly improved safety and outcomes after bariatric surgery comparable to other common general surgical procedures [1]. Morbidity and mortality after bariatric surgery in large population-based studies are noted to be less than 10 % and less than 1 %, respectively [2, 3]. This has been a result of increasing surgical experience, improving technology, development of centers of excellence, and better supportive care [1, 3, 4]. The increasing adoption of laparoscopic bariatric surgery has also shown several advantages over the open approach including enhanced recovery, shorter length of hospital stay (LOS), and diminished risk of wound infections and incisional hernia [5]. Nonetheless, surgical complications following laparoscopic bariatric surgery may warrant reoperation during the initial hospitalization.
Morbidity and mortality after bariatric surgery increases more than 10-fold in patients requiring return to operating room for complications after initial surgery [6]. Rate of return to the operating room after bariatric surgery has varied from 2.3 % in patients undergoing laparoscopic Roux-en-Y gastric bypass (LRYGB) and laparoscopic adjustable gastric banding (LAGB) in a study from the American College of Surgeons-National Surgical Quality Improvement Program (ACS-NSQIP) to 2.6 % in the Longitudinal Assessment of Bariatric Surgery (LABS) consortium [6, 7]. While the 30-day reoperative rate due to postoperative complications is well published, most papers discussing specifics of reoperative surgery are over 10 years old [8]. Since then, there have been multiple changes to the management paradigm for strictures and leaks with increased use of stents and other nonoperative management strategies [9, 10]. Additionally, these studies have not included data regarding patients undergoing revisional bariatric surgery.
With this in mind, we queried our database to study patients undergoing reoperative surgery for management of early complications of LRYGB. The aim of this study was to assess the outcomes after early reoperations and compare this to available data.
Methods
A prospectively maintained database of all patients undergoing LRYGB over a 5-year period from January 2008 to December 2012 was reviewed with institutional review board approval. Among them, patients required reoperation within 30 days of the index LRYGB were identified.
The patient charts were reviewed, and the data collected included patient demographics, the interval between the primary operation and the development of postoperative complications requiring reoperation, details regarding operative intervention including findings on reoperation, postoperative complications after second surgery including need for third operative intervention, and short-term outcomes includingmorbidity and mortality after reoperation.
At our institution, all patients underwent standardized LRYGB and perioperative management according to the established pathways. In brief, the side-to-side stapled jejunojejunostomy was completed using a 60-mm linear stapler. The common opening (enterotomy) was closed using either a stapled or hand-sewn technique according to surgeon preference. The Roux limb was placed in the antecolic, antegastric position, and the gastrojejunostomy was completed using a linear or circular stapler. The mesenteric defects were closed with nonabsorbable suture. Intraoperative endoscopy was used to assess the gastrojejunostomy for leakage and intraluminal bleeding.
Statistical analysis was performed using STATA (version 12.0, College Station, Texas). Differences between the mean values were evaluated using the Wilcoxon rank-sum test. Bivariate associations were evaluated using chi-squared tests for pairs of ordinal variables. All tests were two-tailed, and the results with P less than 0.05 were considered statistically significant.
Results
Over a 5-year period, five surgeons performed 1769 LRYGB cases. Of these, 52 (2.9 %) patients underwent reoperation within 30 days of the index LRYGB. Table 1 describes the preoperative variables in patients undergoing reoperative surgery. Of the 52 patients, 40 (77 %) were females. The mean age for the entire population was 49.5 years with a range of 24 to 68 years. The preoperative body mass index (BMI) ranged from 27 to 65 with a mean of 46 kg/m2. Three patients with BMI less than 35 kg/m2 all underwent revisional bariatric surgery. Two of these patients had previous gastric bands and had presented with prolapse. One patient with a previous open vertical banded gastroplasty had developed gastric outlet obstruction.
Of the 52 patients, 40 (77 %) patients had primary LRYGB and 12 (23 %) had revisional LRYGB. Among the revisional surgeries, majority were conversions of LAGB to LRYGB (n = 7), followed by conversion of vertical banded gastroplasty (n = 4) and laparoscopic sleeve gastrectomy (n = 1) to LRYGB. Thus, the 30-day reoperative surgery rate for primary LRYGB was 2.5 % compared to 7.1 % for revisional surgery.
Indications for early reoperation included bleeding (n = 16, 31 %), followed by bowel obstruction (n = 14, 27 %), leak (n = 14, 27 %), diagnostic exploration for tachycardia and abdominal pain (n = 4, 7.6 %), and abscess without leak (n = 1, 1.9 %). Two patients (3.8 %) were taken to the operating room for acute cholecystitis and one (1.9 %) for complicated ovarian cyst within the 30-day period. There were no significant differences noted between the group of patients undergoing primary surgery versus those undergoing revisional surgery.
Table 2 describes the operative and postoperative course of patients undergoing reoperative surgery. Of the total surgeries, 49 (94 %) were started laparoscopically and three surgeries were planned as open procedures. Of the 49 started laparoscopically, six (12 %) required conversion to open procedure. Overall, there were no intraoperative complication. The mean operative time is 105 ± 48 min. The mean days to reoperation was 6.3 ± 7. Based on the most common causes of reoperation, the shortest time to reoperation was for bleeding (1.9 days), followed by leak (5 days) and obstruction (8.6 days). Table 3 presents the intraoperative findings of these patients. For patients undergoing surgery related to bleeding, the most common sources of bleeding were the mesenteric vessels (n = 6), gastric staple lines (n = 4), and splenic injuries (n = 3). Forty percent of the bleeding on exploration was old clots not requiring active interventions whereas 60 % of patients were noted to have active bleeding requiring intervention. None of the patients who developed bleeding requiring reoperation while on enoxaparin bridging for various medical indications were found to have a surgical bleed. One patient developed a grade 4 splenic laceration from a fall at home 5 days postoperatively. This patient underwent an open splenectomy. None of the patient underwent an open splenectomy. None of the patients were noted to have bleeding at the gastrojejunostomy site; thus, there was no relationship of bleeding to type of gastrojejunostomy anastomosis, linear versus circular. Threshold to take patients back to the operating room for bleeding was variable. All patients had hemodynamic instability, and most patients had received blood transfusions prior to reoperation. All patients at our institution are routinely placed on 40 mg of enoxaparin twice a day for DVT prophylaxis.
The most common cause of obstruction was adhesion (n = 5), followed by kink or narrowing at the jejunojejunostomy (n = 3), and intraluminal clot (n = 2). Two patients requiring reoperation due to obstruction required revision of the jejunojejunal anastomosis.
In patients undergoing reoperative surgery for leak, the site of leak was the gastric pouch and gastrojejunal anastomosis (n = 9), gastric remnant (n = 1), and jejunojejunal anastomosis (n = 1). In 50 % of patients undergoing reoperative surgery for leak, only wide drainage was used, 35 % required resection, repair, or revision along with drainage, and 14 % of the patients were treated with endoscopic stenting and surgical drainage.
The average post-reoperation LOS was 10.4 ± 9.9 days with the shortest for bleeding and longest for leaks. Twenty (38.5 %) patients developed further complications after reoperative surgery including urinary (n = 5) and pulmonary (n = 4) complications, and intra-abdominal collections (n = 3). A third surgery was required in nine (17 %) patients. Of these, four patients originally had leak, three had bleeding, and two had obstruction. These nine patients had a length of stay of 25 days compared to 7.5 days for patients not undergoing a third reoperation (P < 0.001). The 90-day readmission and mortality rates of the entire cohort were 29 % and zero, respectively (Table 2).
Discussion
The outcomes as well as complications after bariatric surgery have improved constantly as surgeons have gained increasing experience in performing these technically demanding operations [11]. However, as the patients get more challenging technically and medically and the number of revisional procedures increases, surgical complications continue to exist. Return to the operating room for immediate complications of surgery is associated with significant morbidity and mortality [6].
There is relatively little published data regarding early reoperations after gastric bypass surgery. We analyzed our database for patients returning to the operating room and found important differences from existing and past literature. Our reoperation rate of 2.9 % is higher than recently published data from the ACS-NSQIP (2.3 %), but the latter study included patients undergoing LAGB, a procedure known to have a significantly decreased postoperative complication rate. Comparing our rate to a paper published in 2003 (13.8 %) [12], a significantly lower rate in our series exists despite the high percentage of revisional surgery in our series. This might reflect the significantly improved safety of laparoscopic bariatric surgery as well the acceptance and use of newer nonoperative techniques to manage postoperative complications.
A majority of the reoperations were a direct complication of LRYGB, with bleeding being the cause in 31 % of patients followed by bowel obstruction and leak. Our negative reexploration rate was 7.7 %. Based on our data, a majority of these surgeries can be accomplished laparoscopically. Patients who underwent an open reexploration had severe small bowel distention related to either ileus or bowel obstruction. Seventeen percent of our patients underwent a third exploration.
As would be expected, bleeding has the shortest interval from index surgery to reoperation, followed by leak and obstruction. Patients with leak had the longest length of hospital stay followed by obstruction and bleeding. Unlike other series, we did not have any short-term mortality in patients undergoing reoperative surgery. As was seen in previous studies, a majority of the patients undergoing reoperation for obstruction did not require revision of the anastomosis [13]. Internal hernia following LRYGB was not among the causes of bowel obstruction in this series. Majority of patients undergoing reoperation for leaks did not undergo revision or resection of the anastomosis.
There is expected to be an increasing number of revisional bariatric surgeries in the coming years [14]. Multiple studies have documented the increased risk of postoperative morbidity after revisional bariatric surgery [15–18]. There is also data suggesting higher reoperative rate for complications in patients undergoing revisional surgery [19]. In our data, about 23 % of all patients that underwent reoperation within 30 days had undergone a revisional bariatric surgery. Thus, although there does exist an increased risk of postoperative complications requiring reoperation after revisional bariatric surgery compared to primary LRYGB, the type of complications remains comparable. Additionally, although none of the differences noted were significant, we did note a higher percent of anastomotic leaks and bowel obstruction in our revisional group, while this group had a lower percent of patients with bleeding requiring reoperation. Thus, while revisional surgery may carry a possible higher risk of anastomotic leak and bowel obstruction, the risk of surgical bleed requiring reoperation is not increased compared to primary surgery.
A limitation of our study apart from the retrospective nature of this analysis includes the lack of long-term reoperative rates in our population. Although a majority of immediate technical complications are manifested in the first 30 days after surgery, bowel obstruction related to internal hernias as well gastrojejunostomy complications including strictures and marginal ulceration can manifest in the long term and may be associated with significant mortality and morbidity. Also, our readmission rate may underrepresent the actual rate due to patients presenting to outside hospitals for complications not requiring operative management. Additionally, complications that were managed nonoperatively like significant bleeding not requiring operative management, strictures managed nonoperatively, deep vein thrombosis, and pulmonary emboli were not analyzed during the course of this study.
In conclusion, results of this study indicate that complications requiring early surgical reintervention following LRYGB in morbidly obese patients is decreasing. Increasing proportion of patients requiring return to the operating room will have undergone a revisional surgery. Bleeding continues to be the most common cause for requiring reoperation within a 30-day period. Although associated with significant morbidity, mortality is low in this patient population. Additionally, when complications are identified and treated promptly, majority of these reoperations can be accomplished laparoscopically.
References
Pories WJ. Bariatric surgery: risks and rewards. J Clin Endocrinol Metab. 2008;93:S89–96.
Saunders JK, Ballantyne GH, Belsley S, et al. 30-Day readmission rates at a high volume bariatric surgery center: laparoscopic adjustable gastric banding, laparoscopic gastric bypass, and vertical banded gastroplasty-Roux-En-Y gastric bypass. Obes Surg. 2007;17:1171–7.
Smith BR, Schauer P, Nguyen NT. Surgical approaches to the treatment of obesity: bariatric surgery. Med Clin N Am. 2011;95:1009–30.
O’Brien PE. Bariatric surgery: mechanisms, indications and outcomes. J Gastroenterol Hepatol. 2010;25:1358–65.
Masoomi H, Nguyen NT, Stamos MJ, et al. Overview of outcomes of laparoscopic and open Roux-En-Y gastric bypass in the United States. Surg Technol Int. 2012;22:72–6.
Nandipati K, Lin E, Husain F, et al. Factors predicting the increased risk for return to the operating room in bariatric patients: a NSQIP database study. Surg Endosc. 2013;27:1172–7.
Flum DR, Belle SH, King WC, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361:445–54.
Papasavas PK, O’Mara MS, Quinlin RF, et al. Laparoscopic Reoperation for early complications of laparoscopic gastric bypass. Obes Surg. 2002;12:559–63.
Brolin RE, Lin JM. Treatment of gastric leaks after Roux-En-Y gastric bypass: a paradigm shift. Surg Obes Relat Dis. 2013;9:229–33.
Victorzon M, Victorzon S, Peromaa-Haavisto P. Fibrin glue and stents in the treatment of gastrojejunal leaks after laparoscopic gastric bypass: a case series and review of the literature. Obes Surg. 2013;23:1692–7.
Schauer P, Ikramuddin S, Hamad G, et al. The learning curve for laparoscopic Roux-En-Y gastric bypass is 100 cases. Surg Endosc. 2003;17:212–5.
Papasavas PK, Caushaj PF, McCormick JT, et al. Laparoscopic management of complications following laparoscopic Roux-En-Y gastric bypass for morbid obesity. Surg Endosc. 2003;17:610–4.
Shimizu H, Maia M, Kroh M, et al. Surgical Management of early small bowel obstruction after laparoscopic Roux-En-Y gastric bypass. Surg Obes Relat Dis. 2013;9:718–24.
Spyropoulos C, Kehagias I, Panagiotopoulos S, et al. Revisional bariatric surgery: 13-year experience from a tertiary institution. Arch Surg. 2010;145:173–7.
Germanova D, Loi P, van Vyve E, et al. Previous bariatric surgery increases postoperative morbidity after sleeve gastrectomy for morbid obesity. Acta Chir Belg. 2013;113:254–7.
Himpens J, Coromina L, Verbrugghe A, et al. Outcomes of revisional procedures for insufficient weight loss or weight regain after Roux-En-Y gastric bypass. Obes Surg. 2012;22:1746–54.
Nesset EM, Kendrick ML, Houghton SG, et al. A two-decade spectrum of revisional bariatric surgery at a tertiary referral center. Surg Obes Relat Dis. 2007;3:25–30. discussion 30.
Stefanidis D, Malireddy K, Kuwada T, et al. Revisional bariatric surgery: perioperative morbidity is determined by type of procedure. Surg Endosc. 2013;27(12):4504–10.
Moon RC, Teixeira AF, Jawad MA. Conversion of failed laparoscopic Adjustable gastric banding: sleeve gastrectomy or Roux-En-Y gastric bypass? Surg Obes Relat Dis. 2013;9(6):901–7.
Conflict of Interest
No conflict of interest to disclose.
Ethical Approval
For this type of study, formal consent is not required.
Informed Consent
Does not apply
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Augustin, T., Aminian, A., Romero-Talamás, H. et al. Reoperative Surgery for Management of Early Complications After Gastric Bypass. OBES SURG 26, 345–349 (2016). https://doi.org/10.1007/s11695-015-1767-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1767-7