Abstract
Associations of BMI with body composition and health outcomes may differ between Asian and European populations. Asian populations have also been shown to have an elevated risk of type 2 diabetes, hypertension, and hyperlipidemia at a relatively low level of BMI. New surgical indication for Asian patients should be discussed by the expert of this field. Forty-four bariatric experts in Asia-Pacific and other regions were chosen to have a voting privilege for IFSO-APC Consensus at the 2nd IFSO-APC Congress. A computerized audience-response voting system was used to analyze the agreement with the sentence of the consensus. Of all delegates, 95% agreed with the necessity of the establishment of IFSO-APC consensus statements, and 98% agreed with the necessity of a new indication for Asian patients.
IFSO-APC Consensus statements 2011
-
Bariatric surgery should be considered for the treatment of obesity for acceptable Asian candidates with BMI ≥ 35 with or without co-morbidities
-
Bariatric/GI metabolic surgery should be considered for the treatment of T2DM or metabolic syndrome for patients who are inadequately controlled by lifestyle alternations and medical treatment for acceptable Asian candidates with BMI ≥ 30
-
The surgical approach may be considered as a non-primary alternative to treat inadequately controlled T2DM, or metabolic syndrome, for suitable Asian candidates with BMI ≥ 27.5.
Other eight sentences are agreed with by majority of the voting delegates to form IFSO-APC consensus statements. This will help to make safe and wholesome the progress of bariatric and metabolic surgery in Asia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past few decades, there had been a dramatic increase in the prevalence of obesity in many countries. The World Health Organization (WHO) estimates that more than 1 billion adults worldwide are overweight; of these, at least 300 million are obese [1]. Obesity is associated with multiple chronic diseases including type 2 diabetes, hypertension, coronary heart disease, stroke, and several cancers [2].
Definitions of overweight (BMI >25) and obesity (BMI >30) are based essentially on criteria derived from studies that involved populations of European origin. The validity of these criteria in Asian populations has yet to be determined. It has been suggested that the associations of BMI with body composition and health outcomes may differ between Asian and European populations [3]. Studies have shown that for a given BMI, Asians generally have a higher percentage of body fat than do Europeans [3]. Asian populations have also been shown to have an elevated risk of type 2 diabetes, hypertension, and hyperlipidemia at a relatively low level of BMI. On the basis of these observations, it has been proposed that the BMI cutoff points for overweight and obesity should be lower for Asian populations than they are for European populations (suggested cutoff points for Asian, >23 for overweight and >27.5 for obesity) [3].
Method
Generation of IFSO-APC consensus statement: Forty-four bariatric experts from Asia-Pacific and other regions were chosen to have voting privileges for the IFSO-APC consensus at the 2nd IFSO-APC congress on 24th February, 2011, in Rusutsu, Hokkaido, Japan (Table 1).
All voting delegates represented their respective societies or countries. The IFSO-APC consensus is based on the antecedent statements and guidelines regarding bariatric and metabolic surgery mainly in the Asia-Pacific region, including the NIH statement [4], Obesity Surgery Society of India (OSSI), Japan Society of Surgery for Obesity and Metabolic Disorder (JSSO), Asian Consensus Meeting of Metabolic Surgery (ACMOMS) [5], Obesity Surgery Society of Australia and New Zealand (OSSANZ), Asian Pacific Metabolic and Bariatric Surgery Society (APMBSS) [6], Diabetes Surgery Summit (DSS) [7], and Asian Diabetes Surgery Summit (ADSS) (Table 2).
These statements and guidelines were used to establish the consensus of IFSO-APC. Before voting on the consensus, representatives of each society presented their statements or guidelines. Tables 3, 4, 5, 6, 7, 8, 9, and 10 described the comparisons among each of the statements or guidelines.
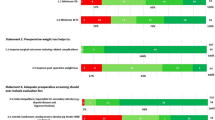
A computerized audience-response voting system was used to analyze agreement or disagreement with the wording of each of the consensuses. “Consensus” was established with the agreement of over 75% of delegates and a “Viewpoint” was recognized with an agreement from 66.6% to 75%.
Results
Of all delegates, 95% agreed with the necessity of establishment of the IFSO-APC consensus statement, and 98% agreed with the necessity of a new indication for Asian patients.
IFSO-APC Consensus Statements 2011
-
1.
Bariatric surgery should be considered for the treatment of obesity for acceptable Asian candidates with BMI ≥ 35 with or without co-morbidities.
Agree 75% consensus
-
2.
Bariatric/GI metabolic surgery should be considered for the treatment of T2DM or metabolic syndrome for patients who are inadequately controlled by lifestyle alternations and medical treatment for acceptable Asian candidates with BMI ≥ 30.
Agree 76.7% consensus
-
3.
The surgical approach may be considered as a non-primary alternative to treat inadequately controlled T2DM, or metabolic syndrome, for suitable Asian candidates with BMI ≥ 27.5.
Agree 67.5% viewpoint
-
4.
Any surgery for T2DM, or metabolic syndrome, for Asian patients with a BMI ≤ 27.5 should be strictly performed only under clinical study protocol with an informed consent from the patient and prior approval from the ethics committee.
Agree 88.1% consensus
-
5.
IFSO-APC generally recommends procedures below for bariatric/GI metabolic surgery for Asian, currently
–Gastric bypass, sleeve gastrectomy, gastric banding, BPD/DS
Agree 95.3% consensus
-
6.
Although novel GI surgical procedures show promising results for Asians other than the four mentioned previously, these should currently be used only in the context of IRB approval.
Agree 97.6% consensus
-
7.
Bariatric/GI metabolic surgery is generally recommended for patients within the ages of >18 and <65.
Under special circumstances, in consideration with a physician or a pediatrician, bariatric/GI metabolic surgery may be used in elderly or adolescent patients.
Agree 92.7% consensus
-
8.
All surgeons who perform bariatric/GI metabolic surgery are properly credentialed and provide a quality bariatric surgical service in accordance with both the required level of skill and experience and the capability of the health service.
Agree 100% consensus
-
9.
Surgical treatment of obesity and metabolic disorder needs a multidisciplinary approach with a team, which includes surgeons, physicians, psychiatrists, dieticians, counselors, and others as needed.
Agree 95% consensus
-
10.
Clinical study should be organized by highly experienced bariatric surgeons, with experience in over 100 cases of bariatric surgery.
Agree 80% consensus
-
11.
This IFSO-APC consensus shows respect for the statements and guidelines of individual societies in Asia-Pacific countries. It does not deny the statement and guideline of each society.
Agree 90% consensus
Discussion
IFSO is the federation of societies of bariatric and metabolic surgery in each individual country and region. IFSO also consists of four chapters: the European chapter, North American Chapter—which is known as American Society of Metabolic and Bariatric Surgery (ASMBS)—South American chapter and Asia-Pacific chapter. The Asia-Pacific region has approximately 60% of the world population and more than 60% of the world’s population with diabetes will come from Asia.
The Asia-Pacific chapter is the newest chapter; the first congress of IFSO-APC was held in 2009 in Cairns, Australia. The 2nd IFSO-APC congress was held in conjunction with the Japan Society of Surgery for Obesity and metabolic disorder (JSSO) meeting in 2011 at Rusutsu, Japan.
As previous guidelines and statements suggested that the action cutoff point for Asian obesity was different from Caucasian populations and the indication for bariatric surgery for Asian populations should be also different. IFSO-APC consensus statements were established with the purpose of considering Asian ethnicity, to perform bariatric/metabolic surgery safely, and to conduct its clinical trials safely according to Asian particularities.
Particularity of Obesity and Diabetes in Asia
In most Asian countries, the prevalence of overweight and obesity has increased many times over in the past few decades, with the magnitude varying between countries [8–10]. Southeast Asia and the Western Pacific region are currently facing an epidemic of diseases associated with obesity such as diabetes and CVD. India has the highest number of people with diabetes in the world and China occupies the second position [11].
The obesity pandemic has been restricted to developed, high-income countries until a few decades ago, but recently it has penetrated even the poorest of nations. Asia has undergone considerable socioeconomic transition in the last three decades, which has resulted in increased availability of food, better transport facilities, and better health care facilities. The changing trend was seen first in urban populations and in the recent years, with an improving socioeconomic scenario in the rural areas, the changes were seen even among urbanizing rural populations. The recent epidemiological data among urban and semi-urban southern Indian populations illustrates the changing scenario [12]. In addition, reduced physical activity at work due to mechanization, improved motorized transport and preferences for viewing television and video games to outdoor games during leisure time, have resulted in a positive energy balance in most Asian countries [13].
In parallel with the increase in adult obesity, obesity in children is also increasing. Childhood obesity has reached more than 25% in many developing countries. The etiological factors for childhood obesity include genetic, metabolic, and behavioral components. An imbalanced energy intake versus energy expenditure due to consumption of energy-dense food and increase in sedentary habits has mainly contributed to the increase in childhood obesity, both in developed and developing countries [14].
Asian populations generally have a lower BMI than many other ethnic groups, but the association between BMI and glucose intolerance is as strong as in any other population [15]. The risk of diabetes (odds ratio) was significant for urban Indian populations with a BMI of >23 kg/m2 [16]. This has been confirmed by studies from other parts of India [17], by studies in migrant Indians and in other Asian populations [18]. According to the WHO recommendations, a BMI of 18.5–22 kg/m2 is considered healthy for Asian populations [19]. Insulin resistance is one of the major etiological factors for diabetes and the risk association between obesity and diabetes is mediated through insulin resistance.
Many Asian populations have a higher total and central adiposity for a given body weight when compared with matched Caucasian populations. A higher prevalence of metabolic syndrome in south Asians is mostly attributed to the higher prevalence of central adiposity.
The IDF criteria for metabolic syndrome recommends use of ethnic specific thresholds for waist circumference, which includes ≥90 cm in men, and ≥80 cm in women of Asian origin [20]. The Japanese population is an exception.
It has also been noted that for a given BMI, Asians have higher body fat percentage compared with Caucasians [21, 22]. Higher insulin resistance and an increased risk of diabetes may be partially attributed to this feature. The differences in anthropometric characteristics are evident even in Asian children who are shown to have higher body fat percentage at lower levels of body weight [23, 24] and also a tendency for abdominal obesity [25].
In the cohorts of East Asians [26], including Chinese, Japanese, and South Koreans, the lowest risk of death was seen among persons with a BMI in the range of 22.6 to 27.5. The risk was elevated among persons with BMI levels either higher or lower than that range—by a factor of up to 1.5 among those with a BMI of more than 35.0 and by a factor of 2.8 among those with a BMI of 15.0 or less. A similar U-shaped association was seen between BMI and the risks of death from cancer, cardiovascular diseases, and from other causes.
A WHO expert consultation concluded in 2004 that Asians generally have a higher percentage of body fat than Caucasian people of the same age, sex, and BMI. Also, the proportion of Asians with risk factors for type 2 diabetes and cardiovascular disease is substantial even below the existing WHO BMI cutoff point of 25 kg/m2. Thus, WHO cut-off points did not provide an adequate basis for taking action on risks related to overweight and obesity in many populations in Asia. WHO recommended for many Asian populations additional trigger points for public health action that were identified as 23 kg/m2 or higher, representing increased risk, and 27.5 kg/m2 or higher as representing high risk. The suggested categories are as follows: less than 18.5 kg/m2 underweight; 18.5–23 kg/m2 increasing but acceptable risk; 23–27.5 kg/m2 increased risk; and 27.5 kg/m2 or higher high risk [3].
The International Diabetes Federation predicts that by 2025 there will be 380 million people worldwide with type 2 diabetes, up from 240 million in 2007 [27]. Asia is expected to feel the brunt of this increase. Asia is the world’s most populous region and accounts for 60% of the global diabetes population [28]. Rates of diabetes and impaired glucose tolerance will grow in every country, particularly those with lower and middle-income, which account for 80% of all afflicted [29]. Asia also stands out because diabetes is predominant among the young to middle-aged.
Changing Asian economies and nutritional behavior makes the increase in diabetes cases even more prevalent. In China, the prevalence of diabetes increased from 1% in 1980 to 5.5% in 2001 [30], with much higher rates in urban areas such as Shanghai [31]. Nearly 10% of Chinese adults residing in affluent regions such as Hong Kong and Taiwan have diabetes [32]. Among individuals with diabetes, two thirds in mainland China and one-half in Hong Kong and Taiwan remain undiagnosed.
In urban Indian adults, diabetes prevalence increased from 3% in the early 1970s to 12% in 2000, with a narrowing rural–urban gradient [33]. In 2006, the rate of type 2 diabetes in rural South India was 9.2%, compared with an increase from 13.9% in 2000 to 18.6% in 2006 in urban South India [34].
Asians have a greater risk of developing type 2 diabetes at a lower BMI than Europeans [35], which explains why diabetes rates match, or even exceed, those in the West, despite overweight and obesity being more common there [4].
Susceptibility to abdominal obesity, low muscle mass, and greater insulin resistance are prevalent in Asia, especially South Asia [36–40]. Waist circumference measurement is, therefore, helpful for measuring obesity-related type 2 diabetes risk, especially when a BMI is within a normal range [41]. Greater type 2 diabetes risk among Asians caused by increased abdominal and visceral adiposity for a given BMI is supported by data [42].
In Asian populations, the amount of visceral fat (including mesenteric fat) and fatty liver was significantly associated with subclinical atherosclerosis [43]. In addition, increased waist circumference has been associated with substantially increased risk of developing diabetes [44] as well as increased risk of cardiovascular and all-cause mortality, independent of BMI [45–47].
Japanese researchers first discovered in the 1980s that lower early insulin response could be used independently to predict diabetes at all stages of glucose intolerance [48, 49]. Early and late-phase insulin response was lower among Japanese. Even a minor increase in BMI among Japanese men with normal glucose tolerance led to a reduction in beta cell function disproportionate to that in insulin sensitivity [50]. Chinese patients showed similar results, with a sample of type 2 diabetes patients where 50% were at normal weight levels and had low BMI correlating with low levels of fasting plasma C-peptide and high glycated hemoglobin levels [51]. Visceral fat areas and reduced incremental insulin response were found in a survey of Japanese Americans to be independent predictors of diabetes [52]. These findings show that among Asians when there is insufficient beta cell response to increasing insulin resistance causes a loss of glycemic control and greater risk of diabetes among Asians, even with only comparatively minor increases in weight.
A comparison of responses to a 75-g carbohydrate load between thin, healthy people matched for age, BMI, waist circumference, birth weight, and diet showed that Asians have higher levels of postprandial glycemia and lower insulin sensitivity than Caucasians, suggesting increased genetic susceptibility to insulin resistance and diabetes [53]. Asian patients with diabetes continue to exhibit high risk for renal complications [54]. In observational studies as well as clinical trials, Asian patients with diabetes were more likely to develop end-stage renal disease (ESRD) than their Caucasian counterparts. In a 25-year prospective survey, 60% of young Japanese patients with type 2 diabetes diagnosed before age 35 became blind or had developed ESRD at a mean age of 50 [55].
Furthermore, the International Diabetes Federation position statement in 2011 March [56] also concluded surgery should be considered as an alternative treatment option in Asian patients with a BMI between 27.5 and 32.5 kg⁄m2 when diabetes cannot be adequately controlled by optimal medical regimen, especially in the presence of other major cardiovascular disease risk factors.
Commentary on IFSO-APC Consensus Statement
Regarding the consensus nos. 1, 2, and 3, the indications of bariatric and metabolic surgery for Asians were argued and decided according to the Asian ethnicity.
Consensus no. 4 is for the BMI definition of a clinical trial for lower BMI patients. Patients with BMI less than 27.5 are categorized as “increased risk,” not “high risk” for Asian [3]. Surgery for this level of patient should be strictly under the protocol of the clinical trial.
Consensus no. 5 defined the generally recommended procedures in Asia. They are as same as the ones ASMBS recommended in 2004 [57] and 2007 [58].
Consensus no. 6 is for the novel procedures. Sleeve gastrectomy with duodenal jejunal bypass [59], ileal interposition with sleeve gastrectomy [60], and others [61] are performed in Asian and have revealed good results but still there is not enough evidence. The novel procedures should be performed only as clinical trials in Asia.
Consensus no. 7 is for the age limitations. Surgeries for adolescent and elderly patients are still not generally recommended. But they will be accepted only under special circumstances.
Consensus nos. 8 and 9 defined the importance of the surgeon’s credentials and a multidisciplinary approach.
Consensus no. 10 is for the safety of clinical trials. Mortality and morbidity during clinical trials should be avoided rather than be seen as a usual practice. Because adverse events in the clinical trial phase will ruin the progress of metabolic surgery in our region, only highly experienced bariatric surgeons should perform the surgery as a clinical trial.
Regarding consensus no. 11, as IFSO is the federation of countries, so that IFSO-APC statements do not deny current statements of each society and country. We hope the IFSO-APC statement will be the foundation of new statements or guidelines in each society and country.
The IFSO-APC consensus statement should be updated according to the upcoming new evidence for bariatric and metabolic surgery. It will be checked and modified at an IFSO-APC congress that will be held every 2 years.
These results indicate progress within the Asian region is different from other continents, and the IFSO-APC will play a significant role in the progression of metabolic surgery, not only in Asia, but throughout the entire world
References
Abelson P, Kennedy D. The obesity epidemic. Science. 2004;304:1413.
Haslam DW, James WP. Obesity. Lancet. 2005;366:1197–209.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
NIH conference. Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med. 1991;115(12):956–61.
Lakdawara M, Bhasker A, Asian Consensus meeting on Metabolic Surgery (ACMOMS), Report: Asian Consensus Meeting on Metabolic Surgery. Recommendations for the use of Bariatric and Gastrointestinal Metabolic Surgery for Treatment of Obesity and Type II Diabetes Mellitus in the Asian Population: August 9th and 10th, 2008, Trivandrum, India. Obes Surg. 2010;20(7):929–36.
Lee WJ, Wang W. Bariatric surgery: Asia-Pacific perspective. Obes Surg. 2005;15:751–7.
Rubino F, Kaplan LM, Schauer PR, et al. The Diabetes Surgery Summit consensus conference: recommendations for the evaluation and use of gastrointestinal surgery to treat type 2 diabetes mellitus. Ann Surg. 2010;251(3):399–405.
Yoon KH, Lee JH, Kim JW, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368(9548):1681–8.
Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999–2008. J Am Med Assoc. 2010;303(3):235–41.
Griffiths PL, Bentley ME. The nutrition transition is underway in India. J Nutr. 2001;131(10):2692–700.
International Diabetes Federation, Diabetes Atlas, 4th edition, 2009.
Ramachandran A, Snehalatha C, Vijay V. Temporal changes in prevalence of type 2 diabetes and impaired glucose tolerance in urban southern India. Diabetes Res Clin Pract. 2002;58(1):55–60.
Parizkova J, Chin MK, Chia M, et al. An international perspective on obesity, health and physical activity: current trends and challenges in China and Asia. J of Exerc Sci and Fit. 2007;5(1):7–23.
World Health Organization, “Report of a joint WHO/FAO Expert. Consultation. Diet, nutrition and the prevention of chronic diseases,” WHO technical report series No. 916, http://whqlibdoc.who.int/trs/who TRS 916.pdf.
Ramachandran A, Snehalatha C, Kapur A, et al. High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia. 2001;44(9):1094–101.
Snehalatha C, Viswanathan V, Ramachandran A. Cut-off values for normal anthropometric variables in Asian Indian adults. Diabetes Care. 2003;26(5):1380–4.
Misra A, Pandey RM, Devi JR, et al. High prevalence of diabetes, obesity and dyslipidaemia in urban slum population in northern India. Int J Obes. 2001;25(11):1722–9.
Chandalia M, Abate N, Garg A, et al. Relationship between generalized and upper body obesity to insulin resistance in Asian Indian men. J Clin Endocrinol Metabol. 1999;84(7):2329–35.
Report of WHO Consultation, “Obesity: preventing and managing the global epidemic,” World Health Organization—Technical Report Series, no. 894, pp. 1–253, 2000.
Alberti KGMM, Zimmet P, Shaw J, et al. Metabolic syndrome—a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006;23(5):469–80.
Ramachandran A, Snehalatha C. Current scenario of diabetes in India. J Diabetes. 2009;1:18–28.
Raji A, Seely EW, Arky RA, et al. Body fat distribution and insulin resistance in healthy Asian Indians and Caucasians. J Clin Endocrinol Metabol. 2001;86(11):5366–71.
Yajnik CS, Lubree HG, Rege SS, et al. Adiposity and hyperinsulinemia in Indians are present at birth. J Clin Endocrinol Metabol. 2002;87(12):5575–80.
Gill T. Young people with diabetes and obesity in Asia: a growing epidemic. Diabetes Voice. 2007;52:20–2.
Ramachandran A, Snehalatha C, Yamuna A, et al. Insulin resistance and clustering of cardiometabolic risk factors in urban teenagers in Southern India. Diabetes Care. 2007;30(7):1828–33.
Zheng W, McLerran DF, Rolland B, et al. Association between body mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364(8):719–29.
Wild S, Roglic G, Green A, et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–53.
International Diabetes Federation. Diabetes Atlas. 3rd ed. Brussels: International Diabetes Federation; 2006.
Chan JCN, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009;301(20):2129–40.
Gu D, Reynolds K, Duan X, et al. Prevalence of diabetes and impaired fasting glucose in the Chinese adult population: International Collaborative Study of Cardiovascular Disease in Asia (InterASIA). Diabetologia. 2003;46(9):1190–8.
Jia WP, Pang C, Chen L, et al. Epidemiological characteristics of diabetes mellitus and impaired glucose regulation in a Chinese adult population: the Shanghai Diabetes Studies, a cross-sectional 3-year follow-up study in Shanghai urban communities. Diabetologia. 2007;50(2):286–92.
Wong KC, Wang Z. Prevalence of type 2 diabetes mellitus of Chinese populations in Mainland China, Hong Kong, and Taiwan. Diabetes Res Clin Pract. 2006;73(2):126–34.
Ramachandran A. Epidemiology of diabetes in India—three decades of research. J Assoc Physicians India. 2005;53:34–8.
Ramachandran A, Mary S, Yamuna A, et al. High prevalence of diabetes and cardiovascular risk factors associated with urbanization in India. Diabetes Care. 2008;31(5):893–8.
Huxley R, James WP, Barzi F, et al. Obesity in Asia Collaboration. Ethnic comparisons of the cross-sectional relationships between measures of body size with diabetes and hypertension. Obes Rev. 2008;9 suppl 1:53–61.
Aekplakorn W, Bunnag P, Woodward M, et al. A risk score for predicting incident diabetes in the Thai population. Diabetes Care. 2006;29(8):1872–7.
Ma RCW, Ko GT, Chan JC. Health hazards of obesity—an overview. In: Williams G, Frubeck G, editors. Obesity: Science to Practice. Hoboken: John Wiley & Sons; 2009. p. 215–36.
Nakagami T, Qiao Q, Carstensen B, et al. Age, body mass index and type 2 diabetes—associations modified by ethnicity. Diabetologia. 2003;46(8):1063–70.
Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002;3(3):141–6.
Reynolds K, Gu D, Whelton PK, et al. Prevalence and risk factors of overweight and obesity in China. Obesity (Silver Spring). 2007;15(1):10–8.
Balkau B, Deanfield JE, Despres JP, et al. International Day for the Evaluation of Abdominal Obesity (IDEA): a study of waist circumference, cardio- vascular disease, and diabetes mellitus in 168,000 primary care patients in 63 countries. Circulation. 2007;116(17):1942–51.
Lear SA, Humphries KH, Kohli S, et al. Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M-CHAT). Am J Clin Nutr. 2007;86(2):353–9.
Liu KH, Chan Y, Chan W, et al. Mesenteric fat thickness is an independent determinant of metabolic syndrome and identifies subjects with increased carotid intimamedia thickness. Diabetes Care. 2006;29(2):379–84.
Cheung BM, Wat NM, Man YB, et al. Development of diabetes in Chinese with the metabolic syndrome: a 6-year prospective study. Diabetes Care. 2007;30(6):1430–6.
Mak KH, Ma S, Heng D, et al. Impact of sex, metabolic syndrome, and diabetes mellitus on cardiovascular events. Am J Cardiol. 2007;100(2):227–33.
Thomas GN, Schooling CM, McGhee SM, et al. Metabolic syndrome increases all-cause and vascular mortality: the Hong Kong Cardiovascular Risk Factor Study. Clin Endocrinol (Oxf). 2007;66(5):666–71.
Zhang X, Shu XO, Yang G, et al. Abdominal adiposity and mortality in Chinese women. Arch Intern Med. 2007;167(9):886–92.
Kadowaki T, Miyake Y, Hagura R, et al. Risk factors for worsening to diabetes in subjects with impaired glucose tolerance. Diabetologia. 1984;26(1):44–9.
Fukushima M, Usami M, Ikeda M, et al. Insulin secretion and insulin sensitivity at different stages of glucose tolerance: a cross-sectional study of Japanese type 2 diabetes. Metabolism. 2004;53(7):831–5.
Kuroe A, Fukushima M, Usami M, et al. Impaired beta-cell function and insulin sensitivity in Japanese subjects with normal glucose tolerance. Diabetes Res Clin Pract. 2003;59(1):71–7.
Chan WB, Tong PCY, Chow CC, et al. The associations of body mass index, C peptide and metabolic status in Chinese type 2 diabetic patients. Diabet Med. 2004;21(4):349–53.
Boyko EJ, Fujimoto WY, Leonetti DL, et al. Visceral adiposity and risk of type 2 diabetes: a prospective study among Japanese Americans. Diabetes Care. 2000;23(4):465–71.
Veena SR, Geetha S, Leary SD, et al. Relationships of maternal and paternal birthweights to features of the metabolic syndrome in adult offspring: an inter-generational study in South India. Diabetologia. 2007;50(1):43–54.
Karter AJ, Ferrara A, Liu J, et al. Ethnic disparities in diabetic complications in an insured population. JAMA. 2002;287(19):2519–27.
Yokoyama H, Okudaira M, Otani T, et al. High incidence of diabetic nephropathy in early onset Japanese NIDDM patients: risk analysis. Diabetes Care. 1998;21(7):1080–5.
Dixon JB, Zimmet P, Alberti KG, et al. Bariatric surgery: an IDF statement for obese Type 2 diabetes. Diabet Med. 2011;28(6):628–42.
2004 ASBS Consensus Conference on Surgery for Severe Obesity. Surg Obes Relat Dis. 2005;1(3):297–381.
Clinical Issues Committee of the American Society for Metabolic and Bariatric Surgery. Updated position statement on sleeve gastrectomy as a bariatric procedure. Surg Obes Relat Dis. 2010;6(1):1–5.
Kasama K, Seki Y, Tagaya N, et al. Laparoscopic sleeve gastrectomy with duodenojejunal bypass: technique and preliminary results. Obes Surg. 2009;19(10):1341–5.
Kumar KV, Ugale S, Gupta N, et al. Ileal interposition with sleeve gastrectomy for control of type 2 diabetes. Diabetes Technol Ther. 2009;11(12):785–9.
Huang CK, Lo CH, Shabbir A, et al. Novel bariatric technology: laparoscopic adjustable gastric banded plication: technique and preliminary results. Surg Obes Relat Dis. 2011;8:41–5.
Acknowledgment
The authors would like to thank Karl Miller (Austria), Ken Loi, Leon Cohen (Austlaria), Joel Faintuch, Nilton Kawahara (Brazil), Shashank Shah, Surendra Ugale, Ramen Goel, Sanjay Borude, Praveen Raj, Jayashree Todkar (India), Barlian Sutedja (Indonesia), Masayuki Ohta, Susumu Inamine (Japan), Hong Chan Lee, Kyung Yul Hur, Sang Kuon Lee, Sang Moon Han (Korea), Chin Kin Fah (Malaysia), Hildegardes C Dineros (Philippine), Sultan Al Temyatt (Saudi Arabia), Davide Lomanto, Jimmy So, Shanker Pasupathy (Singapore), Weu Wang, Chih-Kun Huang (Taiwan), Suthep Udomsawaengsup, Paisal Pongchairerks, Apichai Chaiyaroj (Thailand), Alper Celic (Turkey), Michel Gagner (Canada), and Sayeed Ikramuddin (USA)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kasama, K., Mui, W., Lee, W.J. et al. IFSO-APC Consensus Statements 2011. OBES SURG 22, 677–684 (2012). https://doi.org/10.1007/s11695-012-0610-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-012-0610-7