Abstract
Background
Obesity is associated with nutritional deficiencies. Bariatric surgery could worsen these deficiencies. Fewer nutritional deficiencies would be seen after sleeve gastrectomy compared to the Roux-en-Y gastric bypass, but sleeve gastrectomy would also cause further deterioration of the deficiencies. The aim of this study was to determine the amount of pre-operative nutrient deficiencies in sleeve gastrectomy patients and assess the evolution of the nutritional status during the first post-operative year.
Methods
Four hundred seven sleeve gastrectomy patients were assigned to a standardized follow-up program. Data of interest were weight loss, pre-operative nutrient status and evolution of nutrient deficiencies during the first post-operative year. Deficiencies were supplemented when found.
Results
Two hundred patients completed blood withdrawal pre-operatively and in the first post-operative year. pre-operatively, 5 % of the patients were anemic, 7 % had low serum ferritin and 24 % had low folic acid. Hypovitaminosis D was present in 81 %. Vitamin A had excessive levels in 72 %. One year post-operatively, mean excess weight loss was 70 %. Anemia was found in 6 %. Low-ferritin levels were found in 8 % of the patients. Folate deficiency decreased significantly and hypovitaminosis D was still found in 36 %.
Conclusions
In this study, a considerable amount of patients suffered from a deficient micronutrient status pre-operatively. One year after surgery, micronutrient deficiencies persisted or were found de novo in a considerable amount of patients, despite significant weight loss and supplementation. Significant reductions were seen only for folate and vitamin D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past years, the sleeve gastrectomy (SG) has become accepted as a stand-alone treatment modality for morbid obesity [1]. Early results of the SG show the safety and effectiveness of this procedure in terms of weight loss and remission of comorbidities [2–5]. Although long-term results of the SG are scarce, this technique seems to be a promising procedure [4, 5]. Obesity is associated with nutritional deficiencies. Several studies reported a high prevalence of deficient nutrient status prior to bariatric surgery [6–10]. After bariatric surgery, these micronutrient deficiencies increase or occur de novo, and they may be threatening when left unattended [11–13]. A recent prospective study concluded that fewer deficiencies are seen after SG compared to the Roux-en-Y gastric bypass (RYGB) [14]. Other recent studies show additional deterioration of the existing deficiencies after sleeve gastrectomy [9, 15–17]. The aim of this study was to determine the amount of pre-operative nutrient deficiencies in bariatric patients who underwent SG and assess the evolution of the nutritional status during the first post-operative year.
Materials and Methods
Between April 2010 and September 2011, 407 sleeve gastrectomies were performed by three bariatric surgeons at the Catharina Hospital in Eindhoven, the Netherlands. All patients were restricted to a liquid diet in the first 3 post-operative weeks. They were also instructed to take multivitamin tablets on a daily basis, containing the vitamins A (retinol), B1 (thiamine), B2, B3, B5, B6 (pyridoxine), B8, B12 (cobalamin) and folate (vitamin B11), and also the vitamins C, D3, E and K and the minerals chrome, iron, magnesium, selenium and zinc in concentrations between 100 and 200 % of the recommended daily intake. Furthermore, dalteparin 5000 IU injections were addressed to all patients for 5 weeks to prevent thrombosis. A proton pump inhibitor (PPI) was prescribed for at least 3 months to prevent ulceration of the gastric staple line and to reduce the risk of staple line leakage, as the staple line is exposed to higher pressure and secretion of gastric acids is only slightly decreased, leading to higher risk of gastro-esophageal reflux disease [18]. All patients were assigned to a standard follow-up program consisting of four visits to the outpatient clinic at 6 weeks, 3 months, 6 months and 1 year post-operatively and annual consultation until the fifth post-operative year. Standard laboratory evaluation, consisting of a complete blood count, mean cell volume (MCV) and mineral and vitamin status, was performed for pre-operative assessment, at 6 and 12 months after surgery and annually until the fifth post-operative year.
Nutrient deficiencies were diagnosed by blood analysis. Laboratory values were regarded as deficient when they did not meet the reference values determined by our clinical laboratory (see Table 2). Nutrient deficiencies were scored as de novo when they were newly diagnosed post-operatively. There was anemia in case of reduced haemoglobin and haematocrit values according to local laboratory reference values. Deficiencies that were found either pre-operatively or post-operatively were supplemented. In case of iron levels <10 μmol/L and ferritin concentrations <20 μg/L, ferrofumarate 200 mg was prescribed once or twice daily in combination with 500 mg vitamin C once per day. When deficient levels of calcium were found pre-operatively, 1000 mg calcium citrate was supplemented once a day in combination with 800 IU vitamin D. pre-operative vitamin D levels <50 nmol/L were restored by supplementation of 1 mL vitamin D liquid (50,000 IU/mL) weekly during the first 4 weeks and monthly afterwards. In case of folate deficiency, 5 mg folic acid daily was prescribed for 3 months. Vitamin B12 levels <140 pmol/L were corrected by injecting 2 mL of hydroxocobalamine 500 μg/mL once per 2 weeks in the first 2 months and once per 3 months afterwards. Vitamin B1 levels <70 nmol/L were restored by supplementation of 50–100 mg thiamine daily for a period of 3 months. All laboratory values were evaluated after 12 months of treatment.
For this study, only those patients who completed a pre-operative blood test and at least one blood withdrawal during the first post-operative year were included. Patients who did not complete blood testing or those who had a revision to RYGB were excluded from the study. Data were analyzed retrospectively using a prospectively collected database. Data of interest were weight loss, pre-operative nutrient status and evolution of nutrient deficiencies during the first post-operative year.
Statistics
Excess weight loss (EWL) was calculated using the formula %EWL = weight loss (kg) / excess weight (kg). Excess weight was based on the patients’ ideal weight with a BMI of 25 kg/m2. IBM® Statistical Package for the Social Sciences® (SPSS®) 18.0 was used for processing. The normality of distribution was checked using the skewness and kurtosis calculation, showing normal distribution when values were between −1.00 and 1.00. In case of normal distribution, mean values and ± SD were given; median values and range were given for non-normally distributed data. For calculation of nominal data, the chi-square test was used. For trend analysis of the deficiencies, the McNemar test was used. A P value <0.05 was regarded as statistically significant.
Results
Two hundred patients completed pre-operative blood withdrawal and blood sampling in the first post-operative year. Their mean age was 43 years. Seventy-one per cent of the patients were female. The mean pre-operative BMI in this group was 46 kg/m2. Table 1 shows the baseline characteristics. pre-operatively, ten patients were anemic. Of them, 20 % had microcytic anemia and 20 % had low-ferritin levels. There was no difference in distribution of anemia between both sexes (8.5 vs 3.5 %, P = 0.145 X 2 test). Low serum iron was present in high rates (38 %). Low-ferritin levels were present in 7 % of the patients and all were female. The mean serum concentration was 78.51 μg/L. Decreased levels of serum folate were found in 24 % of the patients. At pre-operative evaluation, a disturbed vitamin status was seen frequently. Remarkably, vitamin A and B6 levels were elevated in a high number of patients (72 and 21 %, respectively). The mean serum concentration of vitamin A was even 2.62 2 μmol/L. A vitamin B12 deficiency was found in 23 patients (11.5 %) and low levels of vitamin B1 were present in 5.5 %. Hypovitaminosis D was present in a great majority of the patients (81 %), and 55 % of them even had a severe deficiency (<30 nmol/L). The mean pre-operative serum concentration of vitamin D was 36.13 nmol/L. In 29 % of the patients with low vitamin D, elevated levels of parathyroid hormone (PTH) were found at assessment, and serum calcium levels corrected for albumin were between acceptable values. In patients with normal serum vitamin D concentration, 5.3 % had elevated PTH levels. The mean pre-operative laboratory values are listed in Table 2.
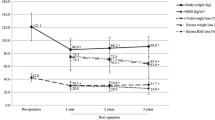
One year post-operatively, a mean excess weight loss of 69.8 % was achieved and the mean BMI decreased significantly from 46.2 to 32.7 kg/m2 (see Table 3).
Twelve months after surgery, laboratory results were assessed (see Table 4). post-operative anemia was found in 6.5 % of the patients. The number of patients with low serum iron decreased significantly to 37 patients (18.5 %). The number of patients with low-ferritin levels increased from 14 to 16 patients (8.0 %). Still, all were female. Their mean serum ferritin concentration increased from 78.51 μg/L pre-operatively to 112.14 μg/L 1 year after surgery. Low levels of folate were recovered significantly in 35 patients, and post-operatively, 25 patients had folate deficiency. Table 5 shows the evolution of the most common deficiencies.
Although the presence of hypervitaminosis A had significantly decreased, excess of vitamin A was still found in over half the patients. The mean serum concentration decreased to 2.32 μmol/L, which is still excessive. The number of patients with hypervitaminosis B6 had even doubled (47.5 %). Vitamin B12 was still deficient in 11.5 % of the patients. Deficiency of vitamin B1 was more frequent 1 year after surgery (9.0 vs 5.5 %). In the meantime, vitamin D deficiency had disappeared in over half the cases, and the mean serum concentration increased to 58.11 nmol/L. Recovery of elevated PTH levels occurred in more than one third (37 %) of the affected patients. Still, the corrected calcium level remained within the normal range. Elevated levels of PTH were found in 12.5 % of the patients with a normal serum vitamin D concentration 1 year post-operatively.
Discussion
This study shows that in the morbidly obese, micronutrient deficiencies are frequently found pre-operatively. Deficiencies can be attributed to a non-varied, high-calorie and high-fat diet. Previous studies already showed the importance of pre- and post-operative assessment of the nutritional status of patients undergoing a bariatric intervention [6–8, 10]. Few studies reported on the nutritional status before and after sleeve gastrectomy [9, 14–16]. All recommend adequate supplementation based on laboratory values.
Anemia is a condition that can be caused by micronutrient deficiencies. Anemia was determined based on low-haemoglobin and -haematocrit levels. Pre-operatively, anemia was found in 5 % of the patients, and 20 % of them had an iron deficiency with low serum ferritin levels. A recent study reporting pre- and post-operative deficiencies in laparoscopic RYGB candidates found 7.9 % pre-operative anemia [19]. Other studies found anemia rates between 12 and 22 % [10, 20–22]. The number of anemic patients doubled post-operatively. Literature describes iron deficiency rates varying between 17 and 44 % [10, 23, 24]. Serum iron levels alone are a poor marker for iron deficiency. Serum ferritin is more specific [24–26]. We found low-ferritin levels in 7 % of the patients before surgery. One year after the SG, the number of affected patients had not significantly changed—iron deficiency persisted in the pre-operatively affected patients. However, the mean serum ferritin concentration increased significantly. This could be the result of supplementation. By resecting the fundus during the SG procedure and by administration of proton pump inhibitors after surgery, the production of HCl is reduced, which may reduce the iron uptake, as Fe3+ conversion to Fe2+ is diminished. The uptake of haem iron is also disrupted and iron-rich red meat is less well tolerated after stomach reduction. These factors could also contribute to a disturbed iron status. The findings implicate that pre-operative supplementation was not sufficient. A disturbed bone metabolism with secondary hyperparathyroidism was found in more than one fifth of the patients pre-operatively. However, calcium levels were between normal values. The prevalence of pre-operative hypovitaminosis D was considerably high (81 %). These high rates have been reported in other studies [17, 27–29]. Hypovitaminosis D is associated with malnutrition and with less exposure to sunlight due to reduced physical activity. Several studies have shown that there is increased uptake of vitamin D in adipose tissue, reducing the serum concentrations of this vitamin [30, 31]. Twelve months after surgery, the number of patients with vitamin D deficiency had decreased significantly. This might be related to the loss of adipose tissue after surgery, and serum levels may also have risen because of adequate supplementation of vitamin D. Although the duodenum and jejunum are not bypassed and uptake of vitamin D is not disturbed, almost one fifth of the patients developed a deficiency newly during the first post-operative year. This could be caused by accelerated food passage, a topic that should be further investigated. Adequate monitoring and supplementation of this vitamin is highly recommended. Remarkably, in a considerable number of patients, vitamin A and vitamin B6 were found in excessive serum concentrations prior to surgery. The number of patients with hypervitaminosis B6 had doubled in the first post-operative year. This might be the effect of multivitamin supplementation, as the prescribed multivitamins contained pyridoxine. Severe excessive serum concentrations of vitamin B6 can cause neurologic symptoms. These symptoms were not reported in this cohort, and in none of the patients, toxic serum levels of vitamin B6 were found. Excessive levels of vitamin A can cause nausea, vomiting, headaches and altered mental status, and also anemia, hepatotoxia and osteoporosis in case of chronic elevated serum levels. Moreover, hypervitaminosis A has a strong teratogenic effect. Vitamin A Intoxication has been described from a level of >100 μg/dL (>3.49 μmol/L) [32], but there are no data on long-term effects of elevated vitamin A levels. None of the patients in our cohort reported signals of intoxication. Vitamin B1 (thiamine) deficiency was present in 5.5 % of the patients at assessment. This prevalence is lower than earlier studies have reported [20, 33]. After surgery, de novo hypovitaminosis B1 was found in 8 % of the patients. Chronic deficiency of thiamine can cause neurological disorders [34, 35]. The deficiency can be caused by a non-varied diet or by chronic alcohol abuse. Moreover, major surgery increases vitamin requirements. After bariatric surgery, thiamine levels must be monitored as rapid weight loss and loss of distributional area after bariatric surgery can cause severe deficiencies. Vitamin B12 (cobalamin) is present in fish, meat and dairy products. It plays a vital role in DNA synthesis and in neurologic functioning and is absorbed in the terminal ileum when bound to intrinsic factor (IF) [7]. The glycoprotein IF is produced in the parietal cells in the antrum of the stomach and in the duodenum. These parts are bypassed after the RYGB, but are preserved after the sleeve gastrectomy. Therefore, cobalamin deficiencies are expected to be less common after sleeve gastrectomy. However, by resecting two thirds of the stomach during SG, a considerable reduction in the number of parietal cells occurs, and less IF might be produced [7, 35]. Literature reports deficiency rates between 3 and 18 % pre-operatively, supporting our findings [6, 7, 20, 36]. After sleeve gastrectomy, a vitamin B12 deficiency was newly diagnosed in 8.0 % of the patients. Frequently, vitamin B12 deficiency is accompanied by low levels of serum folate and they can cause hyperhomocysteinemia, creating a risk factor for atherosclerosis. Low levels of serum folate were already present in a quarter of the patients pre-operatively. This deficiency is mainly associated with reduced intake of folate-rich food, such as lettuce and vegetables [36]. Adequate multivitamin intake might have contributed to the resolution of the deficiency in half of the affected patients. Deficient serum levels of the minerals magnesium and zinc were found in a small amount of patients. Zinc levels were adequate in all patients pre-operatively. Zinc plays a role in the immune system and in wound healing and it plays a key role in the synthesis of insulin. Deficiency of zinc can be associated with hair loss. Deficiency of zinc was newly diagnosed in 5 % of the patients post-operatively. This is lower than the prevalence reported in other studies [6, 37]. Magnesium deficiency can cause neurological and cardiovascular complaints. Magnesium is considered a key factor in the development of the metabolic syndrome [38, 39]. The unvaried high-calorie diet of the obese patients often does not contain adequate amounts of magnesium. We found a magnesium deficiency in 2 % of the patients pre-operatively. After surgery, levels rose in three of them, but deficient levels were diagnosed newly in five patients.
This study has some limitations. First of all, more than half of the cohort did not complete the pre- and post-operative blood withdrawal. This is a large drop-out; however, 200 patients were still analyzed. It is difficult to distinguish between the remission in deficiencies based on supplementation and remission based on weight loss after the sleeve gastrectomy. We only asked patients whether they were compliant towards taking their multivitamins. We did not further assess the patients’ compliance, which could be a major factor in remission of the nutrient deficiencies. Neither did we check the patients’ dietary intake at 12 months post-operatively. This may also have an important influence on the post-operative micronutrient status. At last, the supplements were dosed based on the local protocol. The optimal dose for the micronutrient supplements in the bariatric patient should be subject to further investigation, as this might also be an influence on the patients’ micronutrient status.
Conclusions
In this study, the pre- and post-operative nutrient statuses of 200 morbidly obese patients undergoing a sleeve gastrectomy were analyzed. A considerable amount of patients suffered from a deficient micronutrient status pre-operatively. One year after surgery, micronutrient deficiencies persisted or were found de novo in a considerable amount of patients, despite significant weight loss and supplementation. Only for folate and vitamin D were significant deficiency reductions seen. The questions whether pre-operative supplementation was inadequate and what was the direct effect of the sleeve gastrectomy remain. Another point of interest is the patients’ compliance of supplement intake and this should be subject to further research. At last, the optimal duration of supplementation and the optimal dosage should be determined for adequate treatment of the nutrient deficiencies.
References
Aasheim ET, Hofso D, Hjelmesaeth J, et al. Vitamin status in morbidly obese patients: a cross-sectional study. Am J Clin Nutr. 2008;87:362–9.
Boza C, Salinas J, Salgado N, et al. Laparoscopic sleeve gastrectomy as a stand-alone procedure for morbid obesity: report of 1,000 cases and 3-year follow-up. Obes Surg. 2012;22:866–71.
Brethauer SA, Hammel JP, Schauer PR. Systematic review of sleeve gastrectomy as staging and primary bariatric procedure. Surg Obes Relat Dis. 2009;5:469–75.
Deitel M, Gagner M, Erickson AL, et al. Third international summit: current status of sleeve gastrectomy. Surg Obes Relat Dis. 2011;7:749–59.
Shi X, Karmali S, Sharma AM, et al. A review of laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg. 2010;20:1171–7.
Ernst B, Thurnheer M, Schmid SM, et al. Evidence for the necessity to systematically assess micronutrient status prior to bariatric surgery. Obes Surg. 2009;19:66–73.
Kaidar-Person O, Person B, Szomstein S, et al. Nutritional deficiencies in morbidly obese patients: a new form of malnutrition? Part A: vitamins. Obes Surg. 2008;18:870–6.
Kaidar-Person O, Person B, Szomstein S, et al. Nutritional deficiencies in morbidly obese patients: a new form of malnutrition? Part B: minerals. Obes Surg. 2008;18:1028–34.
Damms-Machado A, Friedrich A, Kramer KM, et al. Pre- and postoperative nutritional deficiencies in obese patients undergoing laparoscopic sleeve gastrectomy. Obes Surg. 2012;22:881–9.
Schweiger C, Weiss R, Berry E, et al. Nutritional deficiencies in bariatric surgery candidates. Obes Surg. 2010;20:193–7.
Davies DJ, Baxter JM, Baxter JN. Nutritional deficiencies after bariatric surgery. Obes Surg. 2007;17:1150–8.
Malinowski SS. Nutritional and metabolic complications of bariatric surgery. Am J Med Sci. 2006;331:219–25.
Toh SY, Zarshenas N, Jorgensen J. Prevalence of nutrient deficiencies in bariatric patients. Nutrition. 2009;25:1150–6.
Gehrer S, Kern B, Peters T, et al. Fewer nutrient deficiencies after laparoscopic sleeve gastrectomy (LSG) than after laparoscopic Roux-Y-gastric bypass (LRYGB)-a prospective study. Obes Surg. 2010;20:447–53.
Aarts EO, Janssen IM, Berends FJ. The gastric sleeve: losing weight as fast as micronutrients? Obes Surg. 2011;21:207–11.
Pech N, Meyer F, Lippert H, et al. Complications, reoperations, and nutrient deficiencies two years after sleeve gastrectomy. J Obes. 2012;2012:828737.
Ruiz-Tovar J, Oller I, Tomas A, et al. Mid-term effects of sleeve gastrectomy on calcium metabolism parameters, vitamin D and parathormone (PTH) in morbid obese women. Obes Surg. 2012;22:797–801.
Chiu S, Birch DW, Shi X, et al. Effect of sleeve gastrectomy on gastroesophageal reflux disease: a systematic review. Surg Obes Relat Dis. 2011;7:510–5.
Aarts EO, van Wageningen B, Janssen IM, et al. Prevalence of anemia and related deficiencies in the first year following laparoscopic gastric bypass for morbid obesity. J Obes. 2012;2012:193705. doi:10.1155/2012/193705.
Flancbaum L, Belsley S, Drake V, et al. Preoperative nutritional status of patients undergoing Roux-en-Y gastric bypass for morbid obesity. J Gastrointest Surg. 2006;10:1033–7.
Muñoz M, Botella-Romero F, Gómez-Ramírez S, et al. Iron deficiency and anaemia in bariatric surgical patients: causes, diagnosis and prope management. Nutr Hosp. 2009;24(6):640–54.
von Drygalski A, Andris DA, Nuttleman PR, et al. Anemia after bariatric surgery cannot be explained by iron deficiency alone: results of a large cohort study. Surg Obes Relat Dis. 2011;7(2):151–6. doi:10.1016/j.soard.2010.04.008.
Vargas-Ruiz AG, Hernandez-Rivera G, Herrera MF. Prevalence of iron, folate, and vitamin B12 deficiency anemia after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2008;18:288–93.
Ten Broeke R, Bravenboer B, Smulders FJ. Iron deficiency before and after bariatric surgery: the need for iron supplementation. Neth J Med. 2013;71(8):412–7.
Hakeam HA, O'Regan PJ, Salem AM, et al. Impact of laparoscopic sleeve gastrectomy on iron indices: 1 year follow-up. Obes Surg. 2009;19:1491–6.
Mittinty MN, Golley RK, Smithers LG, et al. A preference based measure of complementary feeding quality: application to the avon longitudinal study of parents and children. PLoS One. 2013;8(10):e76111. doi:10.1371/journal.pone.0076111.
Carlin AM, Rao DS, Yager KM, et al. Effect of gastric bypass surgery on vitamin D nutritional status. Surg Obes Relat Dis. 2006;2:638–42.
Ybarra J, Sanchez-Hernandez J, Gich I, et al. Unchanged hypovitaminosis D and secondary hyperparathyroidism in morbid obesity after bariatric surgery. Obes Surg. 2005;15:330–5.
Ybarra J, Sanchez-Hernandez J, Perez A. Hypovitaminosis D and morbid obesity. Nurs Clin N Am. 2007;42:19–27.
Blum M, Dolnikowski G, Seyoum E, et al. Vitamin D(3) in fat tissue. Endocrine. 2008;33:90–4.
Holick MF. Vitamin D, deficiency. N Engl J Med. 2007;357:266–81.
Grune T, Lietz G, Palou A, et al. Beta-carotene is an important vitamin A source for humans. J Nutr. 2010;140(12):2268S–85S. doi:10.3945/jn.109.119024.
Carrodeguas L, Kaidar-Person O, Szomstein S, et al. Preoperative thiamine deficiency in obese population undergoing laparoscopic bariatric surgery. Surg Obes Relat Dis. 2005;1:517–22.
Mason ME, Jalagani H, Vinik AI. Metabolic complications of bariatric surgery: diagnosis and management issues. Gastroenterol Clin N Am. 2005;34:25–33.
Singh S, Kumar A. Wernicke encephalopathy after obesity surgery: a systematic review. Neurology. 2007;68:807–11.
Allen LH. Causes of vitamin B12 and folate deficiency. Food Nutr Bull. 2008;29:S20–34.
Madan AK, Orth WS, Tichansky DS, et al. Vitamin and trace mineral levels after laparoscopic gastric bypass. Obes Surg. 2006;16:603–6.
Barbagallo M, Dominguez LJ, Resnick LM. Magnesium metabolism in hypertension and type 2 diabetes mellitus. Am J Ther. 2007;14:375–85.
Barbagallo M, Dominguez LJ. Magnesium metabolism in type 2 diabetes mellitus, metabolic syndrome and insulin resistance. Arch Biochem Biophys. 2007;458:40–7.
Conflicts of Interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Rutte, P.W.J., Aarts, E.O., Smulders, J.F. et al. Nutrient Deficiencies Before and After Sleeve Gastrectomy. OBES SURG 24, 1639–1646 (2014). https://doi.org/10.1007/s11695-014-1225-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1225-y