Abstract
Background
Laparoscopic Nissen fundoplication is an effective treatment for gastroesophageal reflux disease (GERD). However, there is no consensus for the surgical treatment of GERD in morbidly obese patients.
Methods
Twenty-five morbidly obese patients with GERD underwent our novel procedure, laparoscopic Nissen fundoplication with gastric plication (LNFGP), and were monitored for 6 to 18 months. Operative complication, weight loss, and GERD symptoms were monitored.
Results
The study subjects consisted seven males and 18 females. The average age was 38.2 years (from 18 to 58), and the mean BMI was 37.9 kg/m2 (from 31.5 to 56.4). The mean operative time was 145.6 min (from 105 to 190). All procedures were performed via laparoscopic surgery. Two patients (8 %) displayed a major 30-day perioperative complication. The first patient had an acute leak on the second postoperative day. The patient received a laparoscopic revision sleeve gastrectomy and was discharged 5 days later after an uneventful recovery. Another patient developed an intra-abdominal abscess 3 weeks after surgery and received laparoscopic drainage and a revision sleeve gastrectomy. Upon follow-up, only four (16 %) patients experienced occasional acid regurgitation symptoms; however, no anti-acid medication was required. A significant decrease in the prevalence of erosive esophagitis (80 vs. 17 %) after LNFGP was observed. The mean weight loss was 9.7, 14.1, 17.9, and 18.1 % at 1, 3, 6 and 12 months, respectively. The mean BMI decreased to 30.8 kg/m2 1 year post surgery with a mean body weight loss of 25 kg.
Conclusions
LNFGP appears to be an acceptable treatment option for treating GERD in morbidly obese patients who refuse Roux-en-Y gastric bypass. However, further study is indicated to verify this novel procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroesophageal reflux disease (GERD) is a common clinical problem of the alimentary tract [1]. In the USA, 7 % of the adult experiences at least one episodes of reflux every day [2]. Laparoscopic Nissen fundoplication is an effective treatment for patients with severe GERD and has a sustained long-term benefit [3, 4]. Because obesity is a key risk factor for GERD, the increasing prevalence of obesity worldwide has coincided with an increasing prevalence of GERD [5]. Weight reduction is also recommended for managing GERD among obese patients [6]. Among various obesity treatments, bariatric surgery is a viable option for the treatment of severe obesity in comparison with conservative methods, resulting in long-lasting weight loss, an improved quality of life, and the resolution of obesity-related comorbidities as well as a decrease in overall mortality [7, 8]. However, laparoscopic Nissen fundoplication may be an obstacle for the application of bariatric surgery to treat morbidly obese patients with GERD [9–11]. In the present study, we report a novel technique involving both laparoscopic Nissen fundoplication and gastric plication (LNFGP) to combine the weight loss effect with the anti-reflux effect.
Patients and Methods
Eligibility
The study was conducted in the Department of Surgery of the Min-Sheng General Hospital, National Taiwan University. Prior approval for conducting the study was obtained from the ethics committee of the hospital. A total of 25 morbidly obese Asian subjects with GERD (male/female, 7/18; age 38.2 ± 8.0; mean BMI, 37.9 ± 5.9 kg/m2) who received laparoscopic Nissen fundoplication in addition to greater curvature side gastric plication for treating GERD and accompanying obesity were evaluated. All patients who were referred for the surgical treatment of GERD or morbid obesity were evaluated by a gastrointestinal physician. A thorough assessment was performed for those patients with GERD symptoms.
The inclusion criteria were the following: patients aged 18 to 60 years who had a history of GERD for more than 6 months and a BMI above 32 kg/m2 [12]. This study was approved by the Min-Sheng General Hospital Institutional Review Board. All patients were required to provide a written informed consent before undergoing surgery. All the patients were prospectively recruited and followed up according to the study protocol.
Surgical Technique
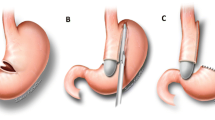
The procedure was performed in the French position using with a standard five-port laparoscopic technique. The greater curvature was mobilized from the omentum starting from 3 cm proximal to the pylorus to the angle of His. The bilateral crus muscles were then dissected out, and the hiatal hernia was exposed. The hernia was closed using 1–0 silk suture. Subsequently, the fundus was wrapped around the esophagus using a 36 F orogastric calibration tube in situ to complete the standard Nissen fundoplication [13]. We then performed the greater curvature side plication using 4–5 interrupted 1–0 silk sutures to correct the shape of gastric plication. A continuous seromuscular suture was then performed using nonabsorbable sutures (2–0 Ethibond Endo-Surgery, Cincinnati, Ohio) from the first interrupted suture at the fundus below the Nissen wrap to the distal antrum to create a single-layer and double loop plication [14]. The calibration tube was removed after completing the LNFGP procedure (Fig 1), and all the trocar wounds were closed. A proton pump inhibitor was administered for 1 day postoperatively. No nasogastric tube was left. The patients were allowed to drink water the next day and discharged later if they did not exhibit vomiting or specific discomfort. During follow-up, the gastrografin study conducted on the second postoperative days indicated a Nissen fundoplication at the proximal stomach and a sleeve-like appearance of the plicated stomach (Fig 2). The endoscopic study conducted during the fourth postoperative month indicated an imbricated greater curvature side and thigh esophagogastric junction (Fig 3).
Measurement of Reflux Symptoms
The frequency and severity of GERD symptoms were assessed by the Gastrointestinal Quality-of-Life Index (GIQLI), a 36-item questionnaire [15] and the items were scored on a 5-point scale (0–4). The maximum score is 144. During analysis, the results of the questionnaire are divided into four domains: physical status (seven items), psychological emotions (six items), social functioning (four items), and specific symptoms (19 items). The specific items for GERD on the GIQLI were divided into three symptoms; heartburn, regurgitation, and dyspepsia with a score between 0 and 4 for each symptom (from the worst to the best option). The GIQLI was evaluated preoperative and 6 to 12 months after surgery for all the patients. The presence of GERD symptoms was defined as typical heartburn and/or acid regurgitation occurring at least once per week over the most recent 3 months.
Classification of Erosive Esophagitis
All patients received preoperative endoscopic evaluation. The diagnosis and classification of esophagitis was based on the Los Angeles (LA) classification [16]. According to this system, esophagitis was classified into grade A (one or more mucosal break less than 5 mm in length that do not extend between the tops of two mucosal folds), grade B (one or more mucosal breaks greater than 5 mm in length, that do not extend between the tops of two mucosa folds), grade C (one or more continuous mucosal breaks between the tops of two or more mucosal folds involving <75 % of the esophageal circumference), and grade D (one or more mucosal breaks that involve at least 75 % of the esophageal circumference).
A hiatal hernia was diagnosed in the presence of a diaphragmatic indentation that was at least 2 cm distal to the Z-line and the proximal margins of the gastric mucosal folds [17]. The endoscopic evaluation was repeated at 6 to 12 months after surgery for all the patients.
Statistical Analysis
Continuous variables were expressed as mean (standard deviation). The descriptive results of the categorical variables were expressed as percentages (%) of the subjects affected. Changes in clinical characteristics, symptoms scores, and EE grade were compared preoperatively and postoperatively. The categorical variables were compared using McNemar’s test, whereas the continuous variables were compared using a paired t test or Wilcoxon signed-rank test, as appropriate. A two-sided P value of 0.05 was considered statistically significant. All statistical analyses were performed using SPSS version 12.01 (SPSS Inc, Chicago, Illinois) for Windows.
Results
Patient Demographics
We analyzed a total of 25 consecutive patients (18 women and seven men), with a mean age of 38.2 ± 7.8 years (from 18 to 58) and a mean BMI of 37.4 ± 5.1 kg/m2 (from 31.5 to 56.4). The subjects’ characteristics are shown in Table 1. All the patients were experiencing GERD symptoms before surgery. The mean operative time was 145.6 ± 23.5 minutes (from 105 to 190). All procedures were performed by laparoscopic surgery. No intraoperative complication developed. The mean postoperative hospitalization stay was 1.4 ± 1.5 days. Two patients (8 %) experienced a major 30 days perioperative complication. The first patient had an acute leak on the second postoperative day and received a laparoscopic revision sleeve gastrectomy (Fig 4). The patient recovered uneventfully and was discharged 5 days later. The second patient returned to the emergency room 21 days after surgery because of an abscess in left subphrenic space. The patient required laparoscopic drainage and received a revision sleeve gastrectomy (Fig 5).
Change of Clinical Characteristics After LNFGP
The mean BMI at 1, 3, 6 and 12 months after surgery were 34.4, 34.1, 31.5 and 30.8, respectively. The mean postoperative weight loss was 9.7, 14.1, 18.0, and 17.0 % at 1, 3, 6 and 12 months, respectively. The percentage of excess postoperative weight loss was 23.6, 34.2, 45.5, and 46.7 % at 1, 3, 6 and 12 months, respectively. The actual mean weight loss was 24.6 kg. The remission of obesity related comorbidities was also high. One patient received revision surgery at 10 months after surgery because of inadequate weight loss. She received a laparoscopic revision sleeve gastrectomy first but converted to a Roux-en-Y gastric bypass 3 days later when a leakage developed. The patient was discharged 1 week later after an uneventful recovery.
Change of GERD Symptoms After LNFGP
During follow-up, only four (16 %) patients had occasional acid regurgitation symptoms after surgery; however, no anti-acid medication was needed. Following LNFGP, the median GIQLI increased significantly, especially improving in symptoms of regurgitation and heart burn (Table 2). However, patients experienced more abdominal fullness or dyspepsia symptom after surgery. After surgery, only five (20 %) patients experienced erosive esophagitis, and all cases were grade A. Before surgery, 20 patients (80 %) experienced erosive esophagitis, including 10 (40 %) with grade A, six (24 %) with grade B, and four patients (16 %) with grade C according to the LA classification (Table 2).
Discussions
Morbid obesity is commonly associated with GERD partly because of the increased intraabdominal pressure that accompanies obesity [5, 6]. Although laparoscopic Nissen fundoplication is a standard approach and an excellent option for treating intractable GERD, this procedure has no effect on weight loss and the resolution of obesity related comorbidities. Recently, several studies have proposed that laparoscopic Roux-en-Y gastric bypass is a more effective weight reduction procedure than Nissen fundoplication for morbidly obese GERD patients [18, 19]. However, gastric bypass surgery yields significant long-term complications and side-effects, such as gastrointestinal bleeding, ileus, and nutritional deficiencies [20–23]. In addition, life-long oral supplements are also indicated for gastric bypass patients. Because of these side effects, not every morbidly obese GERD patient can accept gastric bypass surgery instead of Nissen fundoplication for the treatment of GERD.
For other bariatric procedures, laparoscopic sleeve gastrectomy (LSG) is the most commonly performed bariatric surgery in Asia to date [24]. However, LSG is notorious for an increase in reflux incidence and is not recommended for morbidly obese GERD patients [25]. Similar controversy also existed for laparoscopic adjustable gastric banding. Thus, the appropriate surgical treatment for morbidly obese GERD patients is still controversial.
Nissen fundoplication had been reported to associate with a significant weight loss of 3.9 kg (mean BMI decrease from 27.6 to 26.0) [26]. We also observed a similar average weight reduction of 4 kg in our patient. However, this degree of weight loss is far less than effective for morbidly obese patients. Recently, Khazzaka and Sarkis reported a novel technique of fundoplication combined with mediogastric plication in 16 patients with a mass index of 32–35 kg/m2. The excess weight loss was 10 ± 4 kg (58 %) 1 year after the procedure [27]. In this study, we use greater curvature side plication instead of mediogastric plication and the excess weight loss was 24.6 ± 9 kg (46.7 %). The weight loss was two times higher using greater curvature side plication than using mediogastric plication (24.6 vs. 10 kg). In a previous study, Brethauer discovered that greater curvature side plication was more effective than mediogastric plication, which is consistent with our finding [28]. There was no serious complication in Khassaka’s study using mediogastric plication; however, 8 % of patients who underwent greater curvature side plication experienced a major complication in this study.
Laparoscopic gastric greater curvature side plication (LGGCP) is a new restrictive technique that was first reported in 1981 by Wilkinson [29] but did not garner much attention. Recently, this technique regained interest after Talepour and Amoi reported their long-term results [30, 31]. Skrekas recently proposed a double plication technique instead of single plication which may eliminate prolonged nausea and vomiting after LGGCP [14]. LNFGP has also been adapted for salvaging failed bariatric surgery, such as a dilated sleeve gastrectomy, pouch dilatation after gastric bypass, or inadequate weight loss after gastric banding [32]. The combination of current bariatric surgery with LGGCP has also been reported, for example, banded gastric plication [33]. LNFGP is the first combination of an anti-reflux procedure with a bariatric procedure. Our preliminary data indicates that this combination is feasible and may be an option for the treatment for obese GERD patients.
The advantages of this novel procedure of adding greater curvature side gastric plication to laparoscopic Nissen fundoplication is the treatment of both obesity and GERD. The benefits of LNFGP that mostly influenced the patients’ decision-making were the lack of side-effects from gastric bypass surgery, preserving the efficacy of Nissen fundoplication and a comparable weight loss effect with sleeve gastrectomy. The major disadvantage of LNFGP is a high major 30-day complication rate (8 %) in this study. The high complication rate may be attributed to a small case number and a higher complication in the learning curve of a new laparoscopic procedure. We have learned to avoid a whole layer suture during the surgery and educate the patient to avoid excess vomiting during the early postoperative period.
There were some limitations in this study. The first was the lack of long-term data in durability of gastric plication. According to our short-term follow-up after LNFGP, we consider its anti-reflex and weight loss effect to be satisfied and expect that this procedure would be more readily accepted by patients who hesitate to undergo a procedure that requires life-long change in eating and behavior, long-term medical follow-up, and vitamin supplementation. However, we need long-term data before accepting this novel procedure as a standard treatment. In addition, laparoscopic Roux-en-Y gastric bypass may still be considered as a better procedure for obese GERD patients with a hiatal hernia >3 cm or long-segment Barrett’s esophagus, because a high recurrence rate after fundoplication may be expected in this group of patients [34]. Another limitation of this study is the lack of objective pH monitoring data preoperatively and postoperatively.
In conclusion, LNFGP is a novel, technically feasible combination procedure of fundoplication and bariatric surgery that results in a good anti-reflux effect and acceptable weight loss during short-term follow-up. However, this procedure should be performed under an investigation setting under IRB approval at this moment, and long-term follow-up is necessary to confirm our findings.
References
Dent J, El-Serag HB, Wallander MA, et al. Epidemiology of gastro-esophageal reflux disease: a systematic review. Gut. 2005;54:710–7.
Hinder RA, Libbey JS, Gorecki P, et al. Antireflux surgery: Indications, preoperative evaluation, and outcome. Gastroenterol Clin North Am. 1999;28:987–1005.
Bammer T, Hinder RA, Klaus A, et al. Five- to eight year outcome of the first laparoscopic Nissen fundopications. J Gastroitest Surg. 2001;5:42–8.
Dallemagne B, Perretta S. Twenty years of laparoscopic fundoplicaion for GERD. World J Surg. 2011;35:1428–35.
Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005;143:199–211.
De Groot NL, Burgerhart JS, Meeberg PC VDe, et al. Systematic review: the effects of conservative and surgical treatment for obesity on gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2009;30:1091–102.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Sjostrom L, Narbro K, Sjostrom D, et al. Effect of bariatric surgery on mortality in Swedish obese subjects. NEJM. 2007;357:741–52.
Antanavicius G, Leslie D, Torres-Vilalobos G, et al. Distal esophageal erosion after laparoscopic adjustable gastric band placement with Nissen fundoplication takedown. Obes Surg. 2008;18:1350–3.
Stefanidis D, Navarro F, Augenstein VA, et al. Laparoscopic fundoplication takedown with conversion to Rou-en-Y Gastric bypass leads to excellent reflux control and quality of life after fundoplication failure. Surg Endosc. 2012;26:3521–7.
Makris KL, Lee T, Mitrral K. Roux-en-Y reconstruction for failed fundoplication. J Gastrointest Surg. 2009;13:2226–32.
Lee WJ, Wang W. Bariatric surgery: Asia-Pacific perspective. Obes Surg. 2005;15:751–7.
Espasch E, Williams JL, Wood-Dauphinee S. Gastrointestinal quality of life index: development validation and application of new instrument. Br J Surg. 1995;82:216–22.
Skrekas G, Antiochos K, Stafyla VK. Laparoscopic gastric greater curvature plication: results and complications in a series of 135 patients. Obes Surg. 2011;21:1657–63.
Lai IR, Lee YC, Lee WJ, et al. Comparison of open and laparoscopic antireflux surgery for the treatment of gastroesophageal reflux disease in Taiwanese. J Formos Med Assoc. 2002;101:547–51.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of esophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–80.
Johnson DA, Younes Z, Hogan WJ. Endoscopic assessment of hiatal hernia repair. Gastrointest Endosc. 2000;52:650–9.
Varela JE, Hinojosa MW, Nguyen NT. Laparoscopic fundoplication compared with laparoscopic gastric bypass in morbidly obese patients with gastroesophageal reflux disease. Surg Obes Related Dis. 2009;5:139–43.
Braghetto I, Korn O, Csendes A, et al. Laparoscopic treatment of obese patients with gastroesophageal reflux disease and Barrett’s esophagus: a prospective study. Obes Surg. 2012;22:764–72.
EL-Hayek K, Timratana P, Shimizu H, et al. marginal ulcer after Roux-en-Y Gastric bypass: what we really learned? Sur Endosc. 2012;26:2789–96.
Paroz A, Calmes JM, Giusti V. Internal hernia after laparoscopic Roux-en-Y Gastric bypass for morbid obesity: a continuous challenge in bariatric surgery. Obes Surg. 2006;16:1482–7.
Gasteyger C, Suter M, Gaillard RC, et al. Nutritional deficiencies after Roux-en-Y gastric bypass for morbid obesity often cannot be prevented by standard multivitamin supplementation. Am J Clin Nutr. 2008;87:1128–33.
Lee WJ, Ser KH, Lee YC, et al. Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg. 2012;22:1827–34.
Lomanto D, Lee WJ, Goel R, et al. Bariatric surgery in Asia in the last 5 years (2005–2009) 2012;22:502–506.
Ser KH, Lee WJ, Lee YC, et al. Experience in laparoscopic sleeve gastrectomy for morbidly obese Taiwanese: stapler-line reinforcement is important for preventing leakage. Surg Endosc. 2010;24:2253–9.
Neumayer C, Ciovica R, Gadenstatter M, et al. Significant weight loss after laparoscopic Nissen fundoplication. Surg Endosc. 2005;19:15–20.
Khazzaka A, Sarkis R. Fundoplication combined with mediogastric plication. Surg Obes Related Dis. 2013;9:398–404.
Brethauer SA, Harris JL, Kroh M, et al. Laparoscopic gastric plication for treatment of severe obesity. Surg Obes Relat Dis. 2011;7:15–22.
Wilkinson LH, Peloso OA. Gastric (reservoir) reduction for morbid obesity. Arch Surg. 1981;116:602–5.
Talebpour M, Amoli B. Laparoscopic total gastric plication in morbid obesity. J Laparoendoscopic Adv Surg Techn. 2007;17:793–8.
Niazi M, Maleki AR, Talebpour M. Short-term outcomes of laparoscopic gastric placation in morbidly obese patients: importance of postoperative follow-up. Obes Surg. 2013;23:87–92.
Huang CK, Asim S, Lo CH. Augmenting weight loss after laparoscopic adjustable gastric banding by laparoscopic gastric plication. Surg Obes Related Dis. 2011;7:235–6.
Huang CK, Lo CH, Shabbir A, et al. Novel bariatric technology: laparoscopic adjustable gastric banded plication: technique and preliminary results. Surg Obes Related Dis. 2012;8:41–7.
Miholic J, Hafez J, Lenglinger J, et al. Hiatal hernia, Barrett’s esophagus, and long-term symptom control after laparoscopic fundoplication for gastroesophageal reflux. Surg Endosc. 2012;26:3225–31.
Conflict of Interest
All authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, WJ., Han, ML., Ser, KH. et al. Laparoscopic Nissen Fundoplication with Gastric Plication as a Potential Treatment of Morbidly Obese Patients with GERD, First Experience and Results. OBES SURG 24, 1447–1452 (2014). https://doi.org/10.1007/s11695-014-1223-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1223-0