Abstract
Background
Redo fundoplication has acceptable outcomes in patients with failed previous fundoplications. However, a subset of patients require Roux-en-Y (RNY) reconstruction for symptom relief.
Aim
The aim of this study was to demonstrate safety and efficacy of RNY reconstruction for failed fundoplications.
Method
Retrospective review of data on patients who underwent short-limb RNY gastrojejunostomy (GJ) or esophagojejunostomy (EJ) between the years 2005 and 2007 was performed.
Results
Twenty-two patients underwent RNY reconstructions. Fourteen (64%) patients had one, six (27%) patients had two, and 2 (9%) patients had three previous anti-reflux procedures. RNY GJ was performed in 18 patients and EJ in four patients. Gastrectomy was performed in 13 of these patients. Seven patients (32%) had ten major or minor complications within the 30-day postoperative period, without any mortality observed. At a mean follow-up of 23 months, completed in 21 of these patients (95%), the average heartburn score was 0.38 (range, 0–2). The average regurgitation score was 0.23 (range, 0 to2) and the average dysphagia score was 0.7 (range, 0–2). The mean postoperative BMI was 25.4 compared to a preoperative BMI of 31.
Conclusion
RNY reconstruction with GJ or EJ for failed anti-reflux procedures is a safe, valid surgical option in difficult situations, where a redo fundoplication is either non-feasible or expected to fail. However, it is associated with higher morbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The lower esophageal sphincter complex acts as a physiologic barrier, preventing continuous reflux from the high-pressure stomach into the low-pressure esophagus. Gastroesophageal reflux disease (GERD), which affects nearly 20% of the population in the USA, is a result of this barrier dysfunction. Surgical fundoplication re-creates a barrier between the stomach and the esophagus, restoring near-normal physiology. With the advent of minimally invasive surgery, laparoscopic anti-reflux procedures have gained widespread acceptance. Excellent long-term results have been reported with greater than 90% patient satisfaction on a 5- to 10-year follow-up.1–4
Postoperatively, recurrence of previous symptoms or emergence of new undesirable symptoms should be considered surgical failure and has been reported in 2–30% of patients.3,5–10 A subset of these patients require reoperative intervention, which may include redo fundoplication, esophagogastric resection, and/or diversion of the gastric reservoir.
Gastrectomy with Roux-en-Y (RNY) reconstruction has been used as an antireflux procedure before.11,12 The RNY gastric bypass (with the distal stomach left in situ) has also been shown to be an effective surgical treatment for GERD in obese patients13–17 as well as in patients with scleroderma.18
The role of RNY for primary and reoperative treatment of GERD continues to evolve. We present our initial experience with RNY gastrojejunostomy (GJ) and esophagojejunostomy (EJ) for previously failed fundoplications.
Materials and Methods
Data Collection
All patients undergoing primary and reoperative antireflux surgery at the Creighton University Medical Center (CUMC) were entered into a prospectively maintained database. After approval from the Institutional Review Board, the database was queried to retrieve patients who underwent RNY GJ or EJ as reoperative intervention after previous antireflux surgery.
All of the patients had undergone an extensive preoperative workup, consisting of upper endoscopy, barium swallow, manometry, 24-h pH monitoring, and gastric emptying study.
Data regarding presenting symptoms, previous procedures, preoperative work-up, operative findings, postoperative course, and complications were collected. Attempt was made to contact all patients at least 1 year after surgery. A standard questionnaire (Table 1) used at our center pertaining to foregut symptoms, use of antireflux medications, and patient satisfaction was administered. The data was entered into an Excel database (Microsoft Excel ®) and analyzed.
Surgical Technique
Our operative approach consisted of two steps. The first step was to dismantle the previous fundoplication and repair the recurrent hiatal hernia, if present. The second step was to perform an EJ or GJ, depending on the primary pathology. In patients with undilatable esophageal stricture or significant intraoperative damage to the gastroesophageal junction (GEJ), an EJ was performed. Otherwise, a small gastric pouch (70–100 cc) was created using linear staplers. In some patients, a larger gastric pouch was left in place with recreation of a fundoplication above the GJ. Early in our series, we performed open procedures and resected the distal stomach. However, with growing experience, we performed more laparoscopic procedures and preferred to leave the distal stomach in situ. Gastrointestinal tract continuity was reestablished in all patients with a short (60-cm long) RNY alimentary limb to prevent bile reflux. The biliary limb was 20 cm long. Schematic representation of the postoperative anatomy is shown in Fig. 1.
Results
Demographics
Thirty-five patients underwent RNY GJ or EJ for failed antireflux surgery from January 2005 to October 2007 by the senior author (SKM) at the CUMC. Twenty-two patients (14 female and eight male) with at least 1 year follow-up are included in this study. Their mean age is 55 years (range, 34–78 years) and preoperative mean body mass index (BMI) was 31 (range 20–49). A total of 32 antireflux procedures had previously been performed on these 22 patients with a mean of 1.45 per patient (range, 1–3; Table 2).
Preoperative Assessment
The primary presenting symptom for reoperative surgery was heartburn in seven patients (32%), dysphagia in seven (32%), and chest pain in four (18%). Three (14%) presented with epigastric complaints and one (5%) with combined chest pain and dyspnea from an acutely herniated intrathoracic stomach. The preoperative findings are shown in Table 3.
In the majority of cases, the preoperative anatomical deformity was confirmed by the intraoperative findings. However, in one case, a tight GEJ due to scarring was identified during the operation, whereas a prolapsing gastric polypoid lesion was preoperatively thought to be the cause of symptoms (dysphagia).
Procedures and Postoperative Care
Fourteen of the 22 operations were done via laparotomy, four laparoscopically, two were converted to open, and two procedures were completed with a combined abdominal and thoracic approach. Four of the patients had EJ reconstruction, while 18 had GJ, of which five had a larger gastric pouch with a recreated fundoplication. In 13 patients, the distal stomach was resected, and in nine, it was left in situ. The types of the procedures performed are summarized in Table 4, and the postoperative anatomy is demonstrated in Fig. 1.
The diet was advanced in a stepwise fashion from clear liquids to full liquids and then to six small meals daily. The patients were not placed on bariatric diet, but they were counseled by a dietician and instructed on dumping syndrome symptoms with high-sugar food consumption. Most patients had a temporary gastrostomy or jejunostomy tube placed at the time of surgery, especially if the procedure was done via laparotomy. Tube feeds were administered if prolonged nothing by mouth status was required. Discharge criteria included diet tolerance, adequate bowel function, and satisfactory pain control.
Perioperative Morbidity and Mortality
There was no in-hospital or 30-day mortality. Ten complications occurred in seven (32%) patients (Table 5) within the 30-day postoperative period. The mean hospital stay was 10 days (range, 4–46). The majority of the patients remained in the hospital for less than 10 days. Only five patients were hospitalized for more than 10 days because of complications.
One-Year Outcomes
The follow-up, performed via telephone interviews, was completed in 21 out of the 22 patients (95%) and consisted of at least a 12-month postoperative period. The mean follow-up was 23 months (range, 12–44).
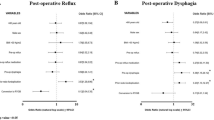
The average heartburn score was 0.38 (range, 0–2). The average dysphagia score was 0.7 (range, 0–2), the average regurgitation score was 0.23, all chest pain scores were 0, and the average nausea score was 0.42 (Table 6). Two patients complained of diarrhea and three of abdominal pain.
Three (14%) patients remained on proton pump inhibitors for reflux, of which one graded his subsequent reflux symptoms as 0 and two as 2. Three (14%) different patients required continuation of metoclopramide for intermittent nausea.
The mean satisfaction level reported was eight on a scale from 1 to 10. Eleven patients (52%) rated their satisfaction level as 9–10, seven patients (33%) as 7–8, and three patients as 6 or less. Twenty patients (95%) would recommend their procedure to a friend if needed.
The mean postoperative BMI of the 21 patients followed-up was 25.4. As shown in Fig. 2, most of the weight loss was observed in patients with a BMI of greater than 30. The patients with a BMI of 30 or less essentially maintained their weight. No patient was postoperatively found to have a BMI of less than 20.
Discussion
Reoperations for previously failed antireflux procedures have increasingly become common with an estimated doubling of their occurrence over the last decade.4 They are technically more challenging due to obscured anatomy and scarring, resulting in a higher incidence of hollow viscus perforations and vagal injury. Other factors, such as short esophagus3 and delayed gastric emptying, further compound the complexity of the procedure. These anatomical and physiological factors account for a higher morbidity and a lower success rate of reoperative fundoplicatons compared to primary surgery.19,20 A morbidity of 4–40% and a mortality rate of 0–4.9% have been reported.3,19–21
Traditional antireflux surgery aims to restore the incompetent barrier between the gastric reservoir and the esophagus. An alternative surgical approach is the removal or redirection of the gastric reservoir. This option appears especially attractive in situations where a redo fundoplication would be expected to have a high failure rate. RNY diversion has been used as a valid antireflux surgical option for many years.11,12
Csendes et al. have reported excellent outcomes with RNY reconstruction as a primary anti-reflux procedure both after antrectomy and vagotomy22 and after duodenal switch and vagotomy.23 Signs of regression of Barrett’s metaplasia were demonstrated in these patients. Given their radical nature, widespread application of these procedures as primary surgical treatment for GERD has not gained acceptance.24
Many studies13–17 have demonstrated the effectiveness of weight-loss-directed RNY gastric bypass in the treatment of GERD in obese patients. This is a particularly difficult group of patients to treat, in which poorer outcomes have been reported with fundoplications.25,26 Additionally, in the obese patients with previously failed antireflux procedures, conversion to a RNY gastric bypass has been shown to be feasible with significant subsequent reduction of reflux symptoms.27,28
Williams et al.29 reported better outcomes for patients undergoing RNY GJ as compared to those undergoing redo fundoplications, even though preoperatively, they had more esophageal changes and greater number of previous procedures. They showed improved symptom control and decreased need for further operative interventions, though they experienced significantly higher complication rate. In our series, we show similar symptom resolution and high patient satisfaction with RNY reconstructions.
A recent study demonstrated the safety and efficacy of near-EJ with RNY reconstruction for recurrent GERD, although significant morbidity was reported.30 Most of the procedures were completed laparoscopically. The characteristic feature of this procedure was an extremely small pouch of 5–10 ml capacity, with the intention to maximally reduce the amount of acid-producing stomach remaining connected to the esophagus. A gastrostomy tube was placed in the distal stomach.
The indications for RNY as a treatment option for failed antireflux surgery have not been clearly defined. Situations where a redo fundoplication would be expected to have a high failure rate should bring RNY into consideration. These situations include obesity (where not only fundoplication has higher failure rate, but weight loss is also desirable), short esophagus (since Collis gastroplasty with fundoplication has poorer results than a straight forward fundoplication), delayed gastric emptying, history of multiple failed fundoplications, injured or scarred fundus, and very poor esophageal motility (where a fundoplication may result in disabling dysphagia).
A short-limb RNY GJ to a small gastric pouch is an attractive alternative to a redo fundoplication. Occasionally, patients with an undilatable distal esophageal stricture (either primary peptic or secondary to previous operation) or patients who sustain significant damage to the GEJ during the dismantling of the previous fundoplication, will require resection of the distal esophagus and proximal stomach with RNY EJ.
The answer to the question of whether the distal gastric remnant should be left in situ or resected is not clear. Obvious concerns about leaving the distal stomach include retained antrum syndrome and possible bleeding from gastroduodenal ulcerations. However, the major advantage of leaving the distal stomach in place is its availability for a possible gastric pull-up if the patient needs an esophageal resection in the future. This is particularly important in patients with Barrett’s esophagus or poor esophageal motility. In our study, we found no difference in patient symptom resolution and satisfaction, either with or without distal gastric resection.
There are three important technical differences between RNY reconstruction for failed fundoplications and the bariatric procedure. First, we leave a larger gastric pouch (70–100 cc) to allow improved meal size. Although we do not have objective data to compare patient satisfaction between different pouch sizes, our patients report high satisfaction without recurrent GERD symptoms. There is always a concern with bleeding from the GJ anastomosis, and more recently, we have started fashioning our pouch in a vertical fashion with little or no fundus included. Second, we create a large GJ to allow rapid transit of food out of the gastric pouch, preventing regurgitation into the esophagus. Third, we measure the biliary limb to be about 20 cm long, with a 60-cm-long alimentary limb, in order to limit the malabsorption associated with the usual bariatric procedure. As a result of these modifications, the majority of the patients maintain a healthy BMI, with the more obese ones losing a significant amount of weight (although not to the extent of a bariatric procedure). We anticipate that with short-limb reconstructions, patients will have decreased nutritional problems. We are in the process of obtaining nutritional parameters for our patients to objectively assess this.
Morbidity is not negligible with RNY procedures as has previously been reported by Williams and Awais.29,30 However, in our view, this can be considered a safe surgical approach in the context of reoperative surgery on patients who have undergone multiple previous operations. Significant adhesions are encountered and the gastric blood supply can be compromised by the previous operations. Sound surgical technique and experience with these reoperative interventions can mitigate the complication rate. High patient satisfaction and symptom resolution is attained with the RNY procedures in this difficult-to-treat group of patients with incapacitating symptoms.
The conclusions that can be drawn are limited by the retrospective nature of our study and the relatively small number of patients included in this initial reporting of our experience. The heterogeneity of the procedures performed may be considered confounding; however, the common underlying physiologic antireflux effect of the RNY reconstruction is of great importance. Longer follow-up, beyond the minimum duration of 1 year reported in our study, will also be needed to validate the initial results of patient satisfaction.
Conclusion
RNY reconstruction with GJ or EJ for failed antireflux procedures is a safe, valid surgical option in difficult situations, where a redo fundoplication is either non-feasible or expected to fail.
References
Horgan S, Pohl D, Bogetti D, Eubanks T, Pellegrini C. Failed antireflux surgery; what have we learned from reoperations? Arch Surg 1999;134:809–817.
Bais JE, Horbach JM, Masclee AA, Smout AJ, Terpstra JL, Gooszen HG. Surgical treatment for recurrent gastro-oesophageal reflux disease after failed antireflux surgery. Br J Surg 2000;87:243–249.
Iqbal A, Awad Z, Simkins J, Shah R, Haider M, Salinas V, Turaga K, Karu A, Mittal SK, Filipi CJ. Repair of 104 failed anti-reflux operations. Ann Surg 2006;244:42–51.
Ohnmacht GA, Deschamps C, Cassivi SD, Nichols FC 3rd, Allen MS, Schleck CD, Pairolero PC. Failed antireflux surgery: results after reoperation. Ann Thorac Surg 2006;81:2050–2054.
DeMeester TR, Bonavina L, Albertucci M. Nissen fundoplication for gastroesophageal reflux disease: evaluation of primary repair in 100 consecutive patients. Ann Surg 1986;204:9–20.
Shirazi SS, Schulze K, Soper RT. Long-term follow-up for treatment of complicated chronic reflux esophagitis. Arch Surg 1987;122:548–552.
Stirling MC, Orringer MB. Surgical treatment after the failed antireflux operation. J Thorac Cardiovasc Surg 1986;92:667–672.
Hunter JG, Trus TL, Branum GD, Waring JP, Wood WC. A physiologic approach to laparoscopic fundoplication for gastroesophageal reflux disease. Ann Surg 1996;223:673–685.
Jamieson GG, Watson DI, Britten-Jones R, Mitchell PC, Anvari M. Laparoscopic Nissen fundoplication. Ann Surg 1994;220:137–145.
Peters JH, Heimbucher J, Kauer WK, Incarbone R, Bremner CG, DeMeester TR. Clinical and physiologic comparison of laparoscopic and open Nissen fundoplication. J Am Coll Surg 1995;180:385–393.
Washer GF, Gear MWL, Dowling BL, Gillison EW, Royston CM, Spencer J. Randomized prospective trial of Roux-en-Y duodenal diversion versus fundoplication for severe reflux oesophagitis. Br J Surg 1984;71:181–184.
Salo JA, Lempinen M, Kivilaakso E. Partial gastrectomy with Roux-en-Y reconstruction in the treatment of persistent or recurrent oesophagitis after Nissen fundoplication. Br J Surg 1985;72:623–625.
Smith SC, Edwards CB, Goodman GN. Symptomatic and clinical improvement in morbidly obese patients with gastroesophageal disease following Roux-en-Y gastric bypass. Obes Surg 1997;7(6):479–484.
Frezza EE, Ikramuddin S, Gourash W, Rakitt T, Kingston A, Luketich J, Schauer P. Symptomatic improvement in gastroesophageal reflux disease (GERD) following laparoscopic Roux-en-Y gastric bypass. Surg Endosc 2002;16:1027–1031.
Perry Y, Courcoulas AP, Fernando HC, Buenaventura PO, McCaughan JS, Luketich JD. Laparoscopic Roux-en-Y gastric bypass for recalcitrant gastroesophageal reflux disease in morbidly obese patients. JSLS 2004;8(1):19–23.
Patterson EJ, Davis DG, Khajanchee Y, Swanström LL. Comparison of objective outcomes following laparoscopic Nissen fundoplication versus laparoscopic gastric bypass in the morbidly obese with heartburn. Surg Endosc 2003;17(10):1561–1565.
Nelson LG, Gonzalez R, Haines K, Gallagher SF, Murr MM. Amelioration of gastroesophageal reflux symptoms following Roux-en-Y gastric bypass for clinically significant obesity. Am Surg 2005;71(11):950–953.
Kent MS, Luketich JD, Irshad K, Awais O, Alvelo-Rivera M, Churilla P, Fernando HC, Landreneau RJ. Comparison of surgical approaches to recalcitrant gastroesophageal reflux disease in the patient with scleroderma. Ann Thorac Surg 2007;84:1710–1716.
DePaula AL, Hashiba K, Baffuto M, Machado CA. Laparoscopic reoperations after failed and complicated antireflux operations. Surg Endosc 1995;9:681–686.
Siewert JR, Isolauri J, Feussner H. Reoperation following failed fundoplication. World J Surg 1989;13:791–796.
Hiebert CA, O’Mara CS. The Belsey operation for hiatal hernia: a twenty year experience. Am J Surg 1979;137:532–535.
Csendes A, Bragheto I, Burdiles P, Smok G, Henriquez A, Parada F. Regression of intestinal metaplasia to cardiac or fundic mucosa in patients with Barrett’s esophagus submitted to vagotomy, partial gastrectomy and duodenal diversion. A prospective study of 78 patients with more than 5 years of follow up. Surgery 2006;139(1):46–53.
Csendes A, Braghetto I, Burdiles P, Díaz JC, Maluenda F, Korn O. A new physiologic approach for the surgical treatment of patients with Barrett’s esophagus: technical considerations and results in 65 patients. Ann Surg 1997;226(2):123–133.
Lillemoe K. A new approach for the surgical treatment of Barrett’s esophagus. Ann Surg 1997;226(2):121–122.
Morgenthal CB, Lin E, Shane MD, Hunter JG, Smith CD. Who will fail laparoscopic Nissen fundoplication? Preoperative prediction of long-term outcomes. Surg Endosc 2007;21:1978–1984.
Perez AR, Moncure AC, Rattner DW. Obesity adversely affects the outcome of antireflux operations. Surg Endosc 2001;15:986–989.
Raftopoulos I, Awais O, Courcoulas AP, Luketich JD. Laparoscopic gastric bypass after antireflux surgery for the treatment of gastroesophageal reflux in morbidly obese patients: initial experience. Obes Surg 2004;14(10):1373–1380.
Houghton SG, Nelson LG, Swain JM, Nesset EM, Kendrick ML, Thompson GB, Murr MM, Nichols FC, Sarr MG, et al. Is Roux-en-Y gastric bypass safe after previous antireflux surgery? Technical feasibility and postoperative symptom assessment. Surg Obes Relat Dis 2005;1(5):475–480.
Williams VA, Watson TJ, Gellersen O, Feuerlein S, Molena D, Sillin LF, Jones C, Peters JH. Gastrectomy as a remedial operation for failed fundoplication. J Gastrointest Surg 2007;11:29–35.
Awais O, Luketich JD, Tam J, Irshad K, Schuchert MJ, Landreneau RJ, Pennathur A. Roux-en-Y near esophagojejunostomy for intractable gastroesophageal reflux after antireflux surgery. Ann Thorac Surg 2008;85:1954–1961.
Acknowledgements
We thank Aikaterini A. Nella, MD for the medical illustration and Janese Gerhardt, RN for the follow-up data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Makris, K.I., Lee, T. & Mittal, S.K. Roux-en-Y Reconstruction for Failed Fundoplication. J Gastrointest Surg 13, 2226–2232 (2009). https://doi.org/10.1007/s11605-009-0994-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-009-0994-4